Abstract
Background
Inflammation and cardiometabolic risk factors can be involved in developing type 2 diabetes mellitus (T2DM). This study aimed to investigate and compare the association between a pro-inflammatory diet and cardiometabolic risk factors in patients with T2DM and non-T2DM cases.
Methods
In this cross-sectional population-based study, considering the baseline data of the Ravansar Non-Communicable Disease (RaNCD) cohort, patients with T2DM (n = 785) and non-T2DM cases (n = 8254) were included. The dietary inflammatory index (DII) was calculated using a food frequency questionnaire (FFQ) and was classified into four groups (quartiles) with lowest to highest scores. Logistic regression analysis was conducted to determine the association between DII and cardiometabolic risk factors in both groups.
Results
The participants were 9,039 (4140 men and 4889 women) with a mean age of 47.4 ± 8.2 years; the mean body mass index (BMI) and DII were 27.49 ± 4.63 kg/m2 and − 2.49 ± 1.59, respectively. After adjustment for confounding factors, we found that DII can increase the risk of T2DM by 61% (95% CI 1.27 to 2.05, P < 0.001). A comparison of two groups revealed that the association of DII, obesity/overweight and dyslipidemia were also significant in both diabetic (P < 0.05) and non-diabetic cases (P < 0.05). However, no significant association was found between DII, MetS, and hypertension in either of the groups. The association between DII and cardiovascular diseases (CVDs) was only significant in diabetic patients (1.65; 95%CI: 1.02 to 2.65, P = 0.04) and T2DM showed an interaction with the association between DII and CVDs.
Conclusion
Inflammatory potential of diet may increase the risk of T2DM. Although it can increase the risk of some cardiometabolic risk factors in both diabetic and non-diabetic cases, its effects were greater among patients with T2DM. However, further prospective studies are required to confirm these associations.
Similar content being viewed by others
Introduction
Dietary patterns are one of the main determinants of chronic systemic inflammation which can be resulted in an increasing level of pro-inflammatory cytokines including tumour necrosis factor α (TNF-α), high sensitivity C-reactive protein (hs-CRP), and interleukin 6 (IL-6) [1,2,3]. The Western dietary pattern, characterized by high consumption of high-fat dairy products, refined grains as well as red and processed meat, has been associated with a higher level of inflammation and an increased risk of inflammation-related diseases [4, 5]. However, a diet rich in whole grains, fruits and green vegetables, such as the Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diet, has been linked with lower concentrations of inflammation markers [6, 7]. Such healthy dietary patterns contain anti-inflammatory nutrients including vitamin C, beta-carotene, n-3 PUFAs, and dietary fibers, which were shown to induce a balance between anti-inflammatory and pro-inflammatory parameters and lower the risks of various chronic diseases [8].
Dietary Inflammatory Index (DII) has been developed, as a population-based dietary score, to specifically reflect the inflammatory potential of dietary factors and to classify the individuals’ diets into the most pro- and anti-inflammatory ones. This index measures the effects of diet on various inflammatory biomarkers by considering the pro- or anti-inflammatory properties of its components, including different macro- and micronutrients and specific food items [9]. An inverse association was reported between DII and other indices which showed healthy dietary patterns such as healthy eating index (HEI) and alternate healthy eating index (AHEI). It is also suggested that DII can be considered a useful tool to examine the healthy eating of adults [10].
Prior evidence also is accumulating on the role of DII in different chronic diseases, which indicated that DII scores are associated with an increased risk of CVDs, obesity, and T2DM [11]. However, there are limited population-based studies, particularly on diabetes. Asadi et al. reported that there was no significant link between the DII and CVDs, stable angina, and myocardial infarction in Mashhad population [12]. In another study by Denova-Gutiérrez et al., the risk of T2DM was 3 times greater in a Mexican population with high scores of DII, compared with those with the lowest scores [13]. Laouali et al. also found that a higher DII score is associated with a higher risk (23%) of T2DM in French adults [14].
Despite the growing interest in the link between inflammatory biomarkers and inflammation-related chronic diseases, the association of the DII and intermediate risk factors of cardiometabolic disorders is insufficiently investigated, particularly in Iranian patients with T2DM. This is particularly important due to differences in dietary habits, genetics, and race and their interactions in various populations, thus, examining the association between DII and cardiometabolic risk factors is likely to be different. Accordingly, the current study aimed to explore and compare the association of DII with cardiometabolic risk factors in both diabetic and non-diabetic populations.
Methods
Study design
This cross-sectional study was designed according to the baseline data of the Ravansar Non-Communicable Disease (RaNCD) cohort study, which was conducted in Ravansar, Iran [15]. RaNCD study is a part of the Prospective Epidemiological Research Studies in IRAN (PERSIAN) cohort study, carried out in different cities with the coordination of the Ministry of Health and Medical Education in Iran [16]. Further details of the RaNCD study have been explained elsewhere [15].
Inclusion and exclusion criteria
Participants who met the following criteria were included: (i) capacity to cooperate with the project team, (ii) age range between 35 and 65 years old, (iii) being the residence of Ravansar for at least 1 year, with a minimum of nine months per year being in the city, and the possibility of staying in Ravansar during the next years, and (iv) having Iranian nationality. Of 10,047 participants in the RaNCD cohort study, 9039 men and women including patients with T2DM (n = 785), and non-diabetic ones (n = 8254) were included. The flowchart of sampling is provided in Fig. 1.
Ethics approval
All eligible individuals signed written informed consent at baseline. The present study was conducted in accordance with the Declaration of Helsinki and was registered with the Department of Research and Technology after getting approval from the Ethics Committee of Kermanshah University of Medical Sciences (KUMS.REC.1394.318).
Data collection and measurements
All details of data collection and assessments are available in the RaNCD protocol [15]. Briefly, demographic characteristics and other information were assessed face-to-face using the digital questionnaire. The socio-economic status (SES) was created, using 18 items (including education level, residence place housing and welfare amenities) by principal component analysis (PCA) method. Finally, the SES was categorized from the lowest to the highest in three groups. Individuals, who never smoked, were defined as non-smokers and current smokers were those who reported smoking a minimum of 100 cigarettes. And, former smokers were those who had given up smoking with a history of at least 100 cigarettes throughout their lifetime [17]. Physical activity was assessed using the standard RaNCD cohort questionnaire [22 questions] and was classified into three levels: low, medium and high according to MET/hour per day [18]. We used the BSM 370 (Biospace Co, Seoul, Korea) to measure the height (precision: 0.1 cm) and Bio-Impedance Analyzer BIA (Inbody 770, Inbody Co, Seoul, Korea) to measure the body weight (precision: 0.5 kg). Other anthropometric indices were also measured including BMI, visceral fat area (VFA), Waist to Hip Ratio (WtHR) and Waist Circumference (WC).
Visceral adipose index (VAI) was calculated based on specific formulas for men and women [19] by the following formula:
Biochemical measurements were also done by collecting participants’ blood samples. We asked them to be fasted overnight for at least 8–12 h. Glucose levels and lipid profile were measured by enzymatic methods after sample collections After taking the blood samples, we kept the serum samples in a freezer at − 72 °C for further measurements.
Assessment of dietary intake
A 118-item food frequency questionnaire (FFQ) was used to examine dietary intake. The validity of this questionnaire was examined earlier [20]. Details of the assessment were explained elsewhere [15]. Briefly, a face-to-face interview was conducted to fill out the questionnaire. Frequency and the amount of food items consumed, including local foods, during the past year were asked to estimate the participants’ dietary intake.
Assessment of DII
Using FFQ, DII was calculated. Shivappa et al. found that 45 foods items were linked with at least one of the inflammatory parameters such as C-reactive protein (CRP), Interleukin- 6 (IL-6), Interleukin-1b (IL-1b), Tumor Necrosis Factor-a (TNF-a) or anti-inflammatory markers including Interleukin-4 (IL-4) and Interleukin-10 (IL-10) [9, 21].
The method for calculation of DII has been published in the previous study [9, 21]. Briefly, the DII score was obtained using 31 food items (out of 45 items introduced for DII), extracted from FFQ by Shivappa criteria [9]. Food items with anti-inflammatory characteristics obtained a score of + 1, and pro-inflammatory ones received a score of − 1. The scores for those with no effect on the levels of inflammatory markers were 0. The greater positive DII scores show more pro-inflammatory diets, and higher negative scores point to a more anti-inflammatory dietary pattern. Generally, the total score for DII can be ranged between − 8.87 (the greatest anti-inflammatory score) and + 7.98 (the highest pro-inflammatory score).
Definitions of T2DM, CVDs, metabolic syndrome (MetS) and other metabolic disorders
Fasting blood sugar (FBS) levels equal to or higher than 126 mg/dL and/or treatment with anti-diabetic medications were considered for the diagnosis of T2DM. Participants with a history of and/or treatment for one or more types of heart diseases such as stroke, myocardial infarction (MI), coronary artery disease, and/or taking CVDs medications were categorized as patients with CVDs. Participants with systolic blood pressure (SBP) of equal to or greater than 140 mmHg and/or diastolic blood pressure (DBP) of equal to or greater than 90 mmHg and/or those with a current use of antihypertensive drugs were classified as patients with hypertension [22]. Dyslipidemia was also defined as serum levels of TC ≥ 240 mg/dl and/or LDL-C ≥ 160 mg/dL and/or TG ≥ 200 mg/dL and/or HDL- C < 40 mg/dL or a history of taking medications for dyslipidemia [23]. Subjects with BMI equal to or greater than 25 kg/m2 were also considered as subjects with overweight/obesity. Moreover, International Diabetes Federation (IDF) criteria were also considered to identify subjects with the MetS [21, 24].
Statistical analysis
Personal characteristics and other assessments across the quartiles of the DII score were reported as Mean ± Standard Deviation (SD) for continuous variables, and qualitative variables were provided by percentages. The normality of the data was checked using the Kolmogorov–Smirnov test. Comparison of baseline characteristics between the two groups of with and without T2DM was performed using t-test and chi-square test. To compare DII quartiles, the one-way ANOVA test was applied. Crude and adjusted logistic regression models were applied to assess the association (odd ratio) between DII quartiles and cardiometabolic risk factors with odds of T2DM. Estimates with a 95% confidence interval and a P-value lower than 0.05 were reported as significant. In the adjusted model, age, sex, energy intake, physical activity, smoking, and SES were taken into the account. All analyses in the current study were performed using Stata version 14.2 software (Stata Corp, College Station, TX, USA).
Results
Characteristics of the study population
Out of 10,047 participants in the RaNCD cohort study, 9,039 individuals including T2DM (n = 785) and non-T2DM cases (n = 8254) were considered for the present study. Baseline characteristics of participants are presented in Table 1. Mean age of the study population was 47.4 ± 8.2 years old and around 46% of them were men with or without diabetes. There were significant differences in terms of smoking, sleep duration, and physical activity levels between diabetic and non-diabetic cases (P-values for all < 0.05). However, no considerable differences were found in socioeconomic status (SES) between the two groups (P = 0.06).
The total mean DII score was − 2.49 ± 1.59. As indicated in Table 1, this score among non-T2DM cases was significantly fewer (with more anti-inflammatory levels) than those with T2DM (mean − 2.50 vs. − 2.37, P = 0.022). Regarding anthropometric indices, significant differences were found between the two groups. BMI, WC, WHR as well as VAI in patients with T2DM were greater than in non-diabetic ones (p-values < 0.01 for all). Moreover, percentages of subjects with metabolic disorders such as hypertension, dyslipidemia, and CVDs in diabetic patients were higher than non-T2DM ones (P-values < 0.01 for all), as expected.
Characteristics of participants in DII categories
In Table 2, the characteristics of all participants, regardless of the diabetic status of participants, are indicated. Based on the findings, mean DII ranged from − 4 to − 0.1 (Quartile 1 to Quartile 4) and most individuals (n = 2391) adhered to anti-inflammatory diets. In addition, most percentage (about 35%) of subjects with low SES had the most anti-inflammatory diet. Regarding the level of physical activity, no significant differences were found between the quartiles of DII (P = 0.13).
There were significant differences in BMI, WHR and VFA across quartiles of DII score. Compared with those in the lowest quartile, participants in the highest quartile of DII score had greater BMI (P < 0.001), WHR (P < 0.001), and VFA (P = 0.003). Regarding their dietary intake, subjects with the most pro-inflammatory diets consumed greater total energy (P < 0.001) compared to those with the most anti-inflammatory diet (Table 3). The intake of all nutrients and food groups except carbohydrates (P = 0.98) and fat (P = 0.12) were significantly different across the categories of the DII score (Table 3).
The association between DII and the risk of T2DM
Logistic regression analysis revealed that the risk of T2DM in subjects who consumed the most pro-inflammatory diet was 28% (95% CI: (1.03 to 1.57)) greater than in those with the most anti-inflammatory ones. After adjustment for confounding factors including age, sex, energy intake, BMI, physical activity, and dyslipidemia, the risk reached 61% (95% CI 1.27–2.05).
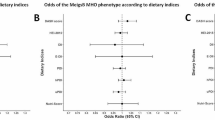
The association between DII and cardiometabolic risk factors
The risk of cardiometabolic disorders in both crude and adjusted models was compared between patients with T2DM and non-T2DM cases and provided in Table 4. In diabetic individuals, the odds of obesity and overweight in the fourth quartile of DII were significantly higher than in the first quartile (Adjusted OR 2.11; 95% CI 1.18, 3.78, P = 0.01), and in non-diabetic individuals, was significantly 52% higher in the fourth quartile than in the first quartile (Adjusted OR: 1.52; 95% CI 1.32, 1.76, P < 0.001). Regarding dyslipidemia, the odds in the fourth quartile of DII were significantly 58% higher than the first one among patients with diabetes (Adjusted OR: 1.58: 95% CI 1.01, 2.50, P = 0.04), and in non-diabetic cases, was 20% greater in the fourth quartile compared to the reference group (Adjusted OR: 1.20: 95% CI 1.05, 1.38, P = 0.007). As indicated in Table 4, the association between MetS and DII was significant only in non-diabetic cases (Adjusted OR: 1.18; 95% CI: 1.01, 1.36, P = 0.02).
The association between DII and an atherogenic index (TG/HDL-C) for both groups is shown in Fig. 2. In both diabetic and non-diabetic cases, direct associations were found between DII and TG/HDL-C. However, the association among diabetic patients was greater than in non-diabetic ones.
Discussion
In the current population-based study, the possible link between the inflammatory potential of diet and risk of cardiometabolic parameters was investigated in both patients with T2DM and the non-diabetic population. Our results demonstrated that participants with the greatest adherence to a pro-inflammatory diet had a higher risk of T2DM versus those with the lowest adherence, even after adjusting for potentially confounding variables. Comparing diabetic and non-diabetic participants, the DII score was also significantly associated with the risk of various intermediate-risk factors of cardiometabolic disorders including obesity/overweight and dyslipidemia among both T2DM and non-T2DM cases. But regarding MetS, a significant association was observed only in non-diabetic cases. Observing these results among both T2DM and non-T2DM cases may support the roles pro-inflammatory diets can have regardless of the health status of participants. However, it should be considered that these dietary factors’ effects in patients with T2DM were greater than non-diabetic ones.
Overall, previous research has reported that the DII score was associated with several inflammatory processes including obesity [21], CVDs [25] and various cancers [26]. In the current study, we compared DII scores among both healthy and diabetic participants. Interestingly, it has been observed that T2DM patients had more pro-inflammatory dietary intakes than non-T2DM cases, such that, mean DII scores were -2.37 and -2.50 among T2DM and non-T2DM cases, respectively.
As diabetic patients are at a higher risk of CVDs than healthy individuals, it is essential to examine potentially modifiable risk factors for CVDs in such a population and compare them with healthy individuals [4,5,6]. Dietary indicators are among the most important and potentially modifiable of these risk factors [10,11,12]. One of the most interesting factors that have received great attention in recent years is the inflammatory potential of diet, which has been quantified by the DII score [18]. Using the DII score to characterize the associations between dietary inflammatory potential and CVDs is of immense importance leading us to conduct food-based novel strategies to prevent and control CVDs. Up to now, there were several studies demonstrating well-established links between DII score and CVDs risk factors [27, 28]. In line with our observations, several, but not all investigations in different populations have reported that a greater pro-inflammatory diet is linked to a higher risk of CVDs risk factors. For instance, in a prospective population-based study among 3726 French participants, a significant association was demonstrated between a higher DII score and an elevated risk of metabolic syndrome, as well as blood pressure, triglycerides which are all among the main risk factors of CVDs [27]. A higher DII score was also reported to be prospectively linked with myocardial infarction (MI) occurrence among the French population [28]. Moreover, no significant relationship was shown between DII score and metabolic syndrome risk in a Mediterranean prospective study in which 6851 participants were followed for 8.3 years [29]. However, Vissers et al. conducted a cohort study on Australian women in the range of 50–55 years and reported no significant relationships between higher DII scores and CVD events including ischemic heart disease, MI, cerebrovascular disease, and Stroke [30]. These contradictory findings could be due to the various characteristics of the examined population such as their age, BMI, socioeconomic status, health status, disease background, race, the mean score of DII and more importantly their dietary habits and lifestyle. Thus, evaluating the links between DII score and various risk factors of CVDs in different population settings is of high importance as these variables have an impact on both DII score and its relationship with cardiovascular health. Another study among 7,216 men (55–80 years old) and women (60–80 years old) conducted by Garcia-Arellano et al. has also reported that a higher DII score was associated with an increased odds of atherosclerosis [31]. Moreover, a large analysis of data obtained in seven countries reported that the DII score was positively correlated with an increased risk of CVDs-related mortality [32]. However, among the prior investigations, only one clinical trial study was carried out on participants with diagnosed diabetes. In this trial which was conducted on 2568 patients, aged 50–75 years, DII score was significantly associated with the CVDs risk factors profile [33]. Our study findings have confirmed these observations and suggested that the inflammatory potential of diet could have detrimental effects even among diabetic patients who have metabolic features associated with insulin resistance. However, insignificant findings in other prior investigations which could be due to different variables including the number of foods used to calculate the DII score, the duration of follow-up, and the definition of cases, provide the necessity that further studies are required in this area to clarify this issue.
The potential mechanisms through which the inflammatory potential of diet might influence CVDs have not been fully elucidated. However, one of the plausible mechanisms could be due to the effects of a pro-inflammatory diet on insulin resistance leading to increased systemic inflammation, which subsequently plays a common pathway for CVDs [34, 35]. Indeed, pro-inflammatory dietary factors increased the expression of some inflammatory cytokines such as IL-1 and TNF-α. These inflammatory markers will in return interfere with insulin signaling and cause insulin resistance [36, 37]. Then, due to the vital roles of insulin in activating nitric oxide, which is a potent vasodilator and antiatherogenic agent, any impairments in insulin signaling such as insulin resistance may lead to hypertension and subsequently CVDs [38, 39]. Cytokines have been also shown to cause attraction and migration of inflammatory cells into vascular tissue and increase the expression of various cell adhesion molecules, which in turn, mediate the adhesion of white blood cells to the vascular endothelium [40]. Moreover, the process of up-regulation of atherogenic gene expression, caused by various dietary inflammatory factors, has been reported to enhance the risks of CVDs [41, 42].
The current study has several limitations that should be addressed. One of the main limitations of the present study was the impossibility of inferring a causal association between DII score and CVDs risk factors due to the observational type of our study. As another limitation of the present study, we were not able to control the confounding effects of genetic and biological differences on the results, since a homogeneous population with a high sample size was used as a control group. Some other confounders, including unmeasured or unknown variables that can affect statistical analysis, have not been controlled in the current study. Although we used a validated FFQ, all 45 items for the DII score were not considered in calculating the total score, and a measurement error was also unavoidable due to using the FFQ for the nutritional assessment of participants. The current study, however, was the only study aimed to determine the association of DII scores with CVDs among a large sample size of Kurdish adults, which could be considered the first strength of our study. High quality of data collection, population-based study, and adjustment for several potential confounders to reach an independent association between DII score and CVDs risk factors are among other strengths of the present study.
Conclusion
Inflammatory potential of diet can increase the risk of T2DM by 61%. Although it can increase the risk of some cardiometabolic risk factors in both diabetic and non-diabetic cases, its effects in patients with T2DM were greater than in non-diabetic ones. Accordingly, providing healthy dietary recommendations and a personalized diet full of anti-inflammatory food items and the least pro-inflammatory foodstuffs such as Mediterranean and DASH diets can be helpful for patients with T2DM to prevent diabetes complications. However, further studies, with a prospective design, are required to confirm these observations.
Availability of data and materials
Data are available from the corresponding author upon reasonable request due to privacy or other restrictions.
Abbreviations
- BMI:
-
Body mass index
- DII:
-
Dietary inflammatory index
- WHR:
-
Waist hip ratio
- WC:
-
Waist circumference
- VFA:
-
Visceral fat area
- TG:
-
Triglycerides
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- T-C:
-
Total cholesterol
- CVDs:
-
Cardiovascular diseases
- VAI:
-
Visceral adiposity index
- FBS:
-
Fasting blood sugar
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- RaNCD:
-
Ravansar non-communicable diseases
- MI:
-
Myocardial infarction
- CRP:
-
C-reactive protein
- TNF-α:
-
Tumor necrosis factor alpha, high sensitivity
- IL-6:
-
Interleukin 6
- IL-4:
-
Interleukin 4
- IL-10:
-
Interleukin 10
- MI:
-
Myocardial infarction
- DASH:
-
Dietary approaches to stop hypertension
- HEI:
-
Healthy eating index
- AHEI:
-
Alternate healthy eating index
- T2DM:
-
Type 2 diabetes mellitus
- SES:
-
Socio-economic status
References
Smidowicz A, Regula J. Effect of nutritional status and dietary patterns on human serum C-reactive protein and interleukin-6 concentrations. Adv Nutr. 2015;6(6):738–47.
Phillips CM, Chen L-W, Heude B, Bernard JY, Harvey NC, Duijts L, et al. Dietary inflammatory index and non-communicable disease risk: a narrative review. Nutrients. 2019;11(8):1873.
Corley J, Shivappa N, Hébert JR, Starr J, Deary I. Associations between dietary inflammatory index scores and inflammatory biomarkers among older adults in the Lothian birth cohort 1936 study. J Nutr Health Aging. 2019;23(7):628–36.
Lainampetch J, Panprathip P, Phosat C, Chumpathat N, Prangthip P, Soonthornworasiri N, et al. Association of tumor necrosis factor alpha, interleukin 6, and C-reactive protein with the risk of developing type 2 diabetes: a retrospective cohort study of rural thais. J Diabet Res; 2019.
Naja F, Shivappa N, Nasreddine L, Kharroubi S, Itani L, Hwalla N, et al. Role of inflammation in the association between the western dietary pattern and metabolic syndrome among Lebanese adults. Int J Food Sci Nutr. 2017;68(8):997–1004.
Tsigalou C, Konstantinidis T, Paraschaki A, Stavropoulou E, Voidarou C, Bezirtzoglou E. Mediterranean diet as a tool to combat inflammation and chronic diseases: an overview. Biomedicines. 2020;8(7):201.
Lin P-H, Vliet SV, Lin C-Y, Svetkey L, Tyson C, Scialla J. Impact of the DASH Diet on Intestinal Permeability and Inflammation Markers. Curr Dev Nutrit. 2020;4(2):542.
Montefusco L, D’Addio F, Loretelli C, Nasr MB, Garziano M, Rossi A, et al. Anti-inflammatory effects of diet and caloric restriction in metabolic syndrome. J Endocrinol Invest 2021; pp. 1–9.
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. 2014;17(8):1689–96.
Asadi Z, Ghaffarian Zirak R, Yaghooti Khorasani M, Saedi M, Parizadeh SM, Jafarzadeh-Esfehani R, et al. Dietary inflammatory index is associated with healthy eating index, alternative healthy eating index, and dietary patterns among Iranian adults. J Clin Lab Anal. 2020;34(12): e23523.
Hariharan R, Odjidja EN, Scott D, Shivappa N, Hébert JR, Hodge A, et al. The dietary inflammatory index, obesity, type 2 diabetes, and cardiovascular risk factors and diseases. Obes Rev. 2022;23(1): e13349.
Asadi Z, Yaghooti-Khorasani M, Ghazizadeh H, Sadabadi F, Mosa-Farkhany E, Darroudi S, et al. Association between dietary inflammatory index and risk of cardiovascular disease in the Mashhad stroke and heart atherosclerotic disorder study population. IUBMB Life. 2020;72(4):706–15.
Denova-Gutiérrez E, Muñoz-Aguirre P, Shivappa N, Hébert JR, Tolentino-Mayo L, Batis C, et al. Dietary inflammatory index and type 2 diabetes mellitus in adults: the diabetes mellitus survey of Mexico City. Nutrients. 2018;10(4):385.
Laouali N, Mancini FR, Hajji-Louati M, El Fatouhi D, Balkau B, Boutron-Ruault M-C, et al. Dietary inflammatory index and type 2 diabetes risk in a prospective cohort of 70,991 women followed for 20 years: the mediating role of BMI. Diabetologia. 2019;62(12):2222–32.
Pasdar Y, Najafi F, Moradinazar M, Shakiba E, Karim H, Hamzeh B, et al. Cohort profile: Ravansar non-communicable disease cohort study: the first cohort study in a Kurdish population. Int J Epidemiol. 2019;48(3):682–3.
Eghtesad S, Mohammadi Z, Shayanrad A, Faramarzi E, Joukar F, Hamzeh B, et al. The PERSIAN cohort: providing the evidence needed for healthcare reform. Arch Iran Med. 2017;20(11):691–5.
Rezaei S, Hajizadeh M, Pasdar Y, Moradinazar M, Hamzeh B, Najafi F. Association of smoking with general and abdominal obesity: evidence from a cohort study in west of Iran. J Res Health Sci. 2018;18(1):401.
Karyani AK, Matin BK, Soltani S, Rezaei S, Soofi M, Salimi Y, et al. Socioeconomic gradient in physical activity: findings from the PERSIAN cohort study. BMC Public Health. 2019;19(1):1–11.
Baveicy K, Mostafaei S, Darbandi M, Hamzeh B, Najafi F, Pasdar Y. Predicting metabolic syndrome by visceral adiposity index, body roundness index and a body shape index in adults: a cross-sectional study from the Iranian RaNCD Cohort Data. Diabetes Metabol Synd Obe Target Therapy. 2020;13:879.
Moradi S, Pasdar Y, Hamzeh B, Najafi F, Nachvak SM, Mostafai R, et al. Comparison of 3 nutritional questionnaires to determine energy intake accuracy in Iranian adults. Clin Nutrit Res. 2018;7(3):213–22.
Abdollahzad H, Pasdar Y, Nachvak SM, Rezaeian S, Saber A, Nazari R. The relationship between the dietary inflammatory index and metabolic syndrome in ravansar cohort study. Diabet Metabol Synd and Obesit Target Therapy. 2020;13:477.
Rajati F, Hamzeh B, Pasdar Y, Safari R, Moradinazar M, Shakiba E, et al. Prevalence, awareness, treatment, and control of hypertension and their determinants: Results from the first cohort of non-communicable diseases in a Kurdish settlement. Sci Rep. 2019;9(1):1–10.
Rezaei M, Fakhri N, Pasdar Y, Moradinazar M, Najafi F. Modeling the risk factors for dyslipidemia and blood lipid indices: Ravansar cohort study. Lipids Health Dis. 2020;19(1):1–8.
Alberti KGM, Zimmet P, Shaw J. The metabolic syndrome—a new worldwide definition. The Lancet. 2005;366(9491):1059–62.
Moradinazar M, Samadi M, Hamzeh B, Najafi F, Karimi S, Faraji F, et al. Association of Dietary Inflammatory Index with cardiovascular disease in Kurdish adults: results of a prospective study on Ravansar non-communicable diseases. BMC Cardiovasc Disord. 2020;20(1):1–8.
Fowler ME, Akinyemiju TF. Meta-analysis of the association between dietary inflammatory index (DII) and cancer outcomes. Int J Cancer. 2017;141(11):2215–27.
Neufcourt L, Assmann K, Fezeu L, Touvier M, Graffouillère L, Shivappa N, et al. Prospective association between the dietary inflammatory index and metabolic syndrome: findings from the SU. VI. MAX study. Nutrit Metabol Cardiovasc Dis. 2015;25(11):988–96.
Neufcourt L, Assmann KE, Fezeu LK, Touvier M, Graffouillere L, Shivappa N, et al. Prospective association between the dietary inflammatory index and cardiovascular diseases in the SUpplémentation en VItamines et Minéraux AntioXydants (SU VI MAX) cohort. J Am Heart Assoc. 2016;5(3):e002735.
Pimenta AM, Toledo E, Rodriguez-Diez MC, Gea A, Lopez-Iracheta R, Shivappa N, et al. Dietary indexes, food patterns and incidence of metabolic syndrome in a Mediterranean cohort: The SUN project. Clin Nutr. 2015;34(3):508–14.
Vissers LE, Waller MA, van der Schouw YT, Hebert JR, Shivappa N, Schoenaker DA, et al. The relationship between the dietary inflammatory index and risk of total cardiovascular disease, ischemic heart disease and cerebrovascular disease: findings from an Australian population-based prospective cohort study of women. Atherosclerosis. 2016;253:164–70.
Garcia-Arellano A, Ramallal R, Ruiz-Canela M, Salas-Salvadó J, Corella D, Shivappa N, et al. Dietary inflammatory index and incidence of cardiovascular disease in the PREDIMED study. Nutrients. 2015;7(6):4124–38.
Puddu PE, Shivappa N, Menotti A, Hébert JR, Tolonen H, Kafatos A, et al. Energy-adjusted Dietary Inflammatory Index scores predict long-term cardiovascular disease mortality and other causes of death in an ecological analysis of the Seven Countries Study. Eur J Prevent Cardiol. 2020:2047487320903866.
Vitale M, Calabrese I, Massimino E, Shivappa N, Hebert JR, Auciello S, et al. Dietary inflammatory index score, glucose control and cardiovascular risk factors profile in people with type 2 diabetes. Int J Food Sci Nutr. 2021;72(4):529–36.
Greenfield JR, Campbell LV. Relationship between inflammation, insulin resistance and type 2 diabetes:’cause or effect’? Curr Diabetes Rev. 2006;2(2):195–211.
Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuñiga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):1–14.
Chen L, Chen R, Wang H, Liang F. Mechanisms linking inflammation to insulin resistance. Int J Endocrinol. 2015;2015.
Wieser V, Moschen AR, Tilg H. Inflammation, cytokines and insulin resistance: a clinical perspective. Arch Immunol Ther Exp. 2013;61(2):119–25.
Dandona P, Chaudhuri A, Ghanim H, Mohanty P. Insulin as an anti-inflammatory and antiatherogenic modulator. J Am Coll Cardiol. 2009;53(5S):S14–20.
Bauer V, Sotníková R. Nitric oxide—the endothelium-derived relaxing factor and its role in endothelial functions. Gen Physiol Biophys. 2010;29(4):319.
Hallahan D, Kuchibhotla J, Wyble C. Cell adhesion molecules mediate radiation-induced leukocyte adhesion to the vascular endothelium. Can Res. 1996;56(22):5150–5.
Ng MK, Quinn CM, McCrohon JA, Nakhla S, Jessup W, Handelsman DJ, et al. Androgens up-regulate atherosclerosis-related genes in macrophages from males but not females: molecular insights into gender differences in atherosclerosis. J Am Coll Cardiol. 2003;42(7):1306–13.
Spady DK, Kearney DM, Hobbs HH. Polyunsaturated fatty acids up-regulate hepatic scavenger receptor B1 (SR-BI) expression and HDL cholesteryl ester uptake in the hamster. J Lipid Res. 1999;40(8):1384–94.
Acknowledgements
The authors thank the PERSIAN cohort Study collaborators and of Kermanshah University of Medical Sciences. The Iranian Ministry of Health and Medical Education has contributed to the funding used in the PERSIAN Cohort through Grant No 700/534.
Funding
This study was supported by the Kermanshah University of Medical Sciences, Kermanshah, Iran (Grant Number 92472).
Author information
Authors and Affiliations
Contributions
NN and YP designed the study. MD and FN conducted data analyses. JASH and MHA interpreted the results. NN and FN supervised the whole project. NN and MHA drafted the manuscript, and all authors revised it critically for important intellectual content and have read and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Ethics Committee of Kermanshah University of Medical Sciences approved the study (KUMS.REC.1394.318). All methods were carried out in accordance with relevant guidelines and regulations. All the participants were provided oral and written informed consent.
Competing interests
Authors declared no competing interests.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Namazi, N., Anjom-Shoae, J., Najafi, F. et al. Pro-inflammatory diet, cardio-metabolic risk factors and risk of type 2 diabetes: A cross-sectional analysis using data from RaNCD cohort study. BMC Cardiovasc Disord 23, 5 (2023). https://doi.org/10.1186/s12872-022-03023-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-03023-8