Abstract
Background
Arrhythmogenic right ventricular cardiomyopathy (ARVC) or arrhythmogenic cardiomyopathy is a rare inherited disease with incomplete penetrance and an environmental component. Although a rare disease, ARVC is a common cause of sudden cardiac death in young adults. Data on the different stages of ARVC remains scarce. The purpose of this study is to describe the initial presentation and cardiac phenotype of definite and non-definite ARVC for patients seen at a tertiary service.
Methods
This is a single centre, observational cohort study of patients with definite and non-definite ARVC seen at the Inherited Cardiac Conditions services at University Hospital Birmingham (UHB) in the period 2010–2021. Patients were identified by interrogation of digital health records, medical history, imaging and by examining 12-lead electrocardiograms (ECG).
Result
The records of 1451 patients were reviewed; of those, 165 patients were at risk of ARVC (mean age 41 ± 17 years, 56% male). 60 patients fulfilled task force criteria for definite ARVC diagnosis (n = 40, 67% males), and 38 (72%) of them carried a known pathogenic variant. The remaining 105 patients (50% males) were non-definite, and of these 45 (62%) carried a known pathogenic variant. Patients in the definite group were more symptomatic, with palpitations (57% vs. 17%), syncope (35% vs. 6%) and shortness of breath (28% vs. 5%, p < 0.001). T-wave inversion in V1-V3 and epsilon waves were observed only in the definite group. Both PR interval and QRS duration were longer in the definite (170 ± 34 ms and 100 ± 19 ms, p < 0.001) compared to (149 ± 25 and 91 ± 14 ms, p = 0.005). Patients with definite ARVC had significantly larger RV end diastolic areas and significantly reduced biventricular function (RVEDA = 27 ± 10 cm2, RVFAC = 37 ± 11% and EF = 56 ± 12%) compared to the non-definite group (RVEDA = 18 ± 4 cm2, RVFAC 49 ± 6% and LVEF 64 ± 7%, p < 0.001). Sustained ventricular tachycardia (VT) occurred more frequently in the definite group compared to the non-definite group (27% vs. 2%, p < 0.001). Ventricular fibrillation was observed in the definite group only (8 of 60 patients, 13%).
Conclusion
Our study showed differences between definite and non-definite ARVC patients in terms of clinical, electrophysiological and imaging features. Major adverse cardiac events occurred more commonly in the definite group, but also were observed in non-definite ARVC. This single centre observational cohort study forms a basis for further prospective multicentre interventional studies.
Similar content being viewed by others
Introduction
Arrhythmogenic right ventricular (RV) dysplasia/cardiomyopathy (ARVC) is a rare inherited non-ischemic cardiomyopathy characterised by fibrotic replacement of cardiac myocytes [1]. It is linked to a high incidence of ventricular arrhythmia (VA) and sudden cardiac death (SCD), particularly in young and athletic people [2]. ARVC has an estimated prevalence of 1 in 1000 to 1 in 2000 individuals [3]. Classically, it is considered an inherited disease with an autosomal dominant pattern; nevertheless, incomplete penetrance, variable expressivity and age at manifestation have been described [4]. In patients with classical ARVC, a pathogenic variant in the desmosomal genes desmoplakin (DSP), plakoglobin (JUP), plakophilin-2 (PKP2), desmocollin-2 (DSC2) and desmoglein-2 (DSG2) accounts for over 50% of cases [5]. Less common pathogenic variants in the extra-desmosomal genes, including desmin (DES), sodium voltage-gated channel alpha subunit (SCN5A), phospholamban (PLN), transmembrane protein 43 (TMEM43), N-cadherin (CDH2) and alpha-T-catenin (CTNNA3), have also been reported [6].
The first clinical description of ARVC by Marcus et al. [7] noted a series of 24 patients presenting with T-wave inversion in the right precordial electrocardiogram (ECG) leads, dilatation of the right ventricle (RV) and dysplasia associated with ventricular tachycardia (VT) of left bundle branch block configuration. In 1994, the first ARVC Task Force criteria (TFC) for diagnosis based on histological, arrhythmia, structural, ECG and familial features of the disease were published. In 2010, these criteria were modified to include quantitative parameters, particularly from imaging [8], leading to increased specificity for the diagnosis. However, sensitivity was still lacking, particularly for early stages of the disease [9]. New insights from post-mortem studies, genotype–phenotype correlation studies and myocardial tissue characterisation by cardiovascular magnetic resonance imaging (CMR) have led to a broader understanding of the disease. Recent modifications have been made to the classification of ARVC as ‘arrhythmogenic cardiomyopathy’, with recognition of biventricular and predominant left ventricular phenotypes. Because of the rarity of the condition and sudden death as a frequent first manifestation, phenotypic data on cohorts referred for assessment for ARVC are still scarce. Therefore, the purpose of this study is to describe the initial presentation and natural history of patients with ARVC referred to a tertiary care centre and to investigate the difference in cardiac phenotypes in definite and non-definite ARVC.
Methods
Study design
This is a single centre, observational, cross-sectional cohort study conducted at the Inherited Cardiac Conditions (ICC) service at University Hospital Birmingham (UHB). This is a highly specialised clinic to which patients with a suspected inherited cardiac condition are referred, often following aborted or sudden cardiac death either in the individual or in a close relative (Fig. 1). The scope of the clinic was set up by the NHS Commissioning Board to include the following four disease categories: (1) arrhythmia syndromes caused by variants in the proteins involved in generating action potential, for example, Brugada syndrome, long QT syndrome and short QT syndrome; (2) cardiomyopathies caused mainly by variants in the proteins involved in myocardial contraction, for example, hypertrophic cardiomyopathy, dilated cardiomyopathy and ARVC; (3) inherited arteriopathies, for example, Loeys–Dietz syndrome and Marfan syndrome; and (4) muscular dystrophies. The ICC clinic at UHB focuses on arrhythmia syndromes and cardiomyopathies with a joint board, with additional hypertrophic cardiomyopathy clinics and with separate arteriopathy and muscular dystrophy services. The aim of the service is to provide timely diagnosis, proactive care and a smooth transition from paediatric to adult care. The ICC functions as a multidisciplinary service, with a core consisting of cardiologists, clinical geneticists and counsellors, ICC nurse specialists and experienced echocardiographers. Diagnostic tools include echocardiography, CMR, exercise testing, signal-averaged ECGs (SAECG), and genetic testing.
Study population
Adult patients aged 18 and older were included consecutively based on referral to the clinic with suspected ARVC or a positive family history [10]. Patients were excluded if they had a history or current evidence of ischaemia, hypertension or valve disease as the most likely cause of heart disease and cardiovascular complication (Table 1). Final diagnostic categorisation into definite and non-definite categories was carried out following discussion by a multidisciplinary team with the ICC clinicians, including specialists in genetics, cardiac electrophysiology and cardiovascular imaging all experienced in ARVC. All patients with suspected and confirmed ARVC were identified by interrogation of digital health records and were classified into two groups, ‘definite’ and ‘non-definite according to the 2010 TFC [8]. A definite ARVC diagnosis was made when two major criteria or one major and two minor criteria or four minor criteria from different categories were met. A non-definite ARVC diagnosis was made when one major and one minor criteria or three minor criteria from different categories were met or when one major or two minor criteria from different categories were met. Major adverse events were recorded from first attendance and medication, biomarkers and SAECG were included as close to the first attendance as feasible from the clinical records.
As exercise has been described as an aggravating factor for ARVC, proportions of different levels of physical activity (competitive and non-competitive exercise) were compared between definite and non-definite groups, as defined by Maron et al. [11].
Electrocardiography
12-lead ECGs were performed in all cases upon entry to the ICC clinic. Each 12-lead ECG was assessed for the presence of repolarisation and depolarisation criteria, per the 2010 TFC. Signal-averaged ECGs were performed routinely at baseline to assess the presence or absence of late potentials. Premature ventricular complex count was measured by 24-h Holter monitoring upon entry to the ICC clinic and was considered abnormal if it was > 500/24 h, as described by 2010 TFC.
Echocardiography
Transthoracic echocardiography (TTE) was performed by experienced echocardiographers accredited by the British Society of Echocardiography (BSE). All available TTE images were re-analysed and re-measured offline by a single independent operator (AA) blinded to demographic, clinical and diagnostic data for conventional parameters, including atrial and ventricular size and function per the most recent requirements of the published BSE guidelines using IntelliSpace Cardiovascular technology (ISCV; Philips, the Netherlands) [12].
Cardiac magnetic resonance imaging
Left and right ventricular volumes and mass and left and right atrial volumes were acquired in line with standard CMR (1.5 T Avanto; Siemens Healthcare, Erlangen, Germany) protocols [13]. Late gadolinium enhancement (LGE) imaging was performed 7–10 min after 0.15 mmol/kg of gadolinium-based contrast agent administration (Gadovist Bayer Healthcare). Analysis of the right and left ventricular volume and ejection fraction were performed using cvi42® (version 5.3.6 Circle Cardiovascular Imaging, Canada) by a single independent operator (AA) blinded to the demographic, clinical and diagnostic data for conventional parameters. For ventricular volume analysis, the endocardial border was detected with the largest and smallest cavity volumes defined as end diastole and end systole, respectively. The endocardial border was defined as the boundary between blood pool and myocardium, with papillary muscles excluded from ventricular volume.
Genetics
Genetic testing was performed with either next-generation sequencing or whole genome targeted panel. The panel of genes included Plakophilin-2 (PKP2), desmoglein-2 (DSG2) plakoglobin (JUP), desmoplakin (DSP), desmocollin-2 (DSC2), N-cadherin (CDH2), phospholamban (PLN), transmembrane protein 43 (TMEM43), desmin (DES) and lamin A (LMNA). Genetic testing was performed for family members only after identification of a pathogenic variant in the proband and in clinically screened family members of a deceased proband who expressed an ARVC phenotype.
Statistical analysis
Continuous variables are presented as means and standard deviations; the unpaired t-test was used for statistical comparison between definite and non-definite ARVC groups. Additionally, categorical variables are expressed as a frequency with percentage of the total population, having been compared statistically using a Fisher’s exact test or a Chi-squared test. For non-normally distributed variables, a Mann–Whitney U Test was used. A two-sided p value with statistical significance defined as < 0.05 was used. All statistical tests were performed using IBM SPSS 27.
Results
A total of 1451 new patients were referred to the ICC clinic in the period 2010–2021 for confirmed or suspected arrhythmia syndromes and differential diagnosis of ARVC. Of those, 1105 patients were excluded with another diagnosis; the most common categories were the following: long QT syndrome: n = 355; hypertrophic cardiomyopathy (HCM): n = 338; dilated cardiomyopathy (DCM): n = 140; Brugada syndrome: n = 121 and catecholaminergic polymorphic ventricular tachycardia (CPVT): n = 31.
There were also disparate other conditions diagnosed in this subspecialised clinic which were seen in low numbers (as these patients were more often diagnosed and seen in other highly specialised tertiary care clinics), including: peripartum cardiomyopathy: n = 3; restrictive cardiomyopathy: n = 1; LV non-compaction cardiomyopathy: n = 7; congenital heart disease: n = 10; Fabry disease: n = 1; Wolf Parkinson White syndrome (WPWS): n = 5, coronary artery disease: n = 10; familial hypercholesterolemia: n = 2; familial lone AF: n = 7; family history of SCD due to known aetiology-other than ARVC: n = 41 and patients or family members below age 18: n = 33).
346 patients were assessed for the presence of major and minor ARVC criteria as per the 2010 TFC, and 181 patients were excluded (those patients who did not meet either definite or non-definite ARVC diagnosis n = 28; ARVC excluded based on genetic testing that was negative for the family member of a proband with confirmed pathogenic variant: n = 14; patients aged under 18 years screened for ARVC: n = 26; incomplete data: n = 19; Idiopathic VF/VT: n = 34; and family history of SCD due to unknown aetiology with normal investigations: n = 60. A definite diagnosis of ARVC was made for 60 patients, and non-definite disease was diagnosed in 105 patients (Fig. 1).
Clinical characteristics
Overall, average age at presentation was 41 ± 17 years, and 56% of patients were male (n = 92). The majority of those referred to the clinic following a possible or confirmed diagnosis of ARVC in a first-degree relative (n = 118 (72%)) or a second-degree relative (n = 21 (13%)). Some patients were diagnosed ‘de novo’ following a major adverse cardiovascular event, including sustained VT (n = 18 (11%)) and VF (n = 8 (5%)). The most common presentations were palpitations (n = 52 (32%)) and syncope (n = 27 (16%)). Of the total population, 29 (19%) patients had a history of competitive exercise.
The baseline demographic characteristics of those with ARVC are summarised in Table 2, sub-divided according to definite and non-definite ARVC diagnosis. Patients in the definite group were more symptomatic compared to those in the non-definite, with palpitations (57% vs. 17%), syncope (35% vs. 6%) and shortness of breath (28% vs. 5%, p < 0.001). History of participation in competitive sports was more common in the definite group (32%) compared to the non-definite group (11%, p = 0.001). Major adverse cardiac events were more common in the definite group compared to the non-definite group in terms of aborted VF (13% vs. 0%) and sustained VT (27% vs. 2%, p < 0.001).
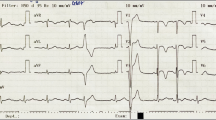
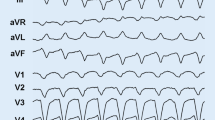
Electrocardiographic evaluation
12-lead ECG, SAECG and 24-h Holter data from the definite and non-definite ARVC groups are summarised in Table 3. T-wave inversion (TWI) in leads V1–V3 detected by 12-lead ECG was observed in 36 (60%) patients in the definite group. Epsilon waves were observed only in the definite group (n = 14, 23%), while no patient in the non-definite group demonstrated a major ECG depolarisation criterion (p < 0.001). There were no significant differences between the definite and non-definite groups regarding the 12-lead ECGs in terms of P and QRS axes, but both PR interval and QRS duration were longer in the definite group (170 ± 34 ms and 100 ± 19 ms) compared to non-definite group (149 ± 25, p < 0.001 and 91 ± 14 ms p = 0.005).). Patients in the definite group were more likely to have BBB compared to those in the non-definite (23% vs. 5%, p < 0.001).
Imaging evaluation
Imaging characteristics derived from echocardiography and CMR are summarised in Table 4. At presentation, RV function in the group with definite ARVC was worse by fractional area change (FAC) on echocardiography compared to the non-definite ARVC group (37 ± 11% vs. 49 ± 6%, p < 0.001) and right ventricular ejection fraction (RVEF) on CMR (39 ± 15% vs. 56 ± 7%, p < 0.001). Likewise, RV size was larger in the definite group compared to the non-definite group based on both imaging modality. Late enhancement was more common in those with definite ARVC compared to those with non-definite ARVC, although detectable in 5 (13%) of the patients in the non-definite ARVC group (p < 0.001), (Fig. 2). (Additional file 1: Figs. S1, S2 and S3) illustrate imaging and ECG features taken from one patient with definite and one patient with non-definite ARVC.
Genetics
Genetic data are summarised in Table 5. Genetic testing was performed in 127 patients out of 165, and a pathogenic variant was identified in 83 (66%). The most common pathogenic variant was PKP2, which occurred in 50 (39%) patients, followed by DSP in 26 (20%) patients. Of those, 7 (6%) patients showed a double variant along with PKP2 and DSP. Around 4 (7%) patients with double variants were in the definite ARVC stage, while 3 (4%) were in the non-definite ARVC stage.
No known pathogenic variant was detected in 41 (32%) of the patients. DSC2 variants were detected in 3 (2%) patients and DSG2 variants in 4 (3%). Patients in the non-definite group were more likely to harbour a DSP variant (p = 0.027).
As 32 (30) patients did not undergo genetic testing we repeated the analysis after excluding the untested patients from the non-definite group and the results presented in the supplementary did not show significant differences from the result presented in the manuscript (Additional file 1: Table S1, S2 and S3).
Discussion
This is a single centre snapshot of the clinical presentation, demographic, electrical, imaging and genetic characteristics of a cohort of patients referred for ICC assessment for suspected ARVC in the West Midlands region of the United Kingdom. In contrast to prior studies that have mostly focused on the definite group alone, a particular attribute of this study is to present characteristics of both patients with definite ARVC and patients with non-definite ARVC.
Among 165 subjects hitherto screened, a definite ARVC diagnosis was made according to the 2010 TFC for 60 patients and a non-definite ARVC diagnosis was made for 105 patients. As would be expected from a predominant autosomal inherited disease, there was near equivalence in terms of sex in the whole population described here (56% male), but there was a male preponderance in the definite group (67% male). In the original paper by Marcus et al., a male to female ratio of 2.7:1 was described in a study of 24 patients [7]. Likewise, in a study of 149 index patients, there was significant male predominance in both ARVC patients with a confirmed pathogenetic variant (71% male) and those without (80% male), [14]. This finding of male predominance is not to be expected based on the inheritance of this condition. It could however be caused by a more active lifestyle, as 9 (23%) males reported high intensity sports-physical, and by male sex hormone facilitating disease phenotype [15]. The higher diagnosis rate of definite ARVC in males could also reflect a lack of sensitivity of the imaging criteria, even when indexed to body surface area for women. Echocardiography cut-off values are based not only on absolute values but also values indexed to body surface area for size that are the same in men and women; yet, even indexed dimensions are frequently smaller in women.
Among individuals with ARVC, a history of exercise has been linked to disease progression and poor outcomes. Variant carriers who exercised for longer periods of time were previously shown to have a higher risk of VA events [16]. 32% of our definite group exercised regularly and had suffered more potentially life-threatening arrhythmias at presentation compared to the non-definite ARVC group. This is consistent with lower penetrance in patients who exercise less. In patients with definite ARVC, the same result was found; athletes with confirmed ARVC had a greater risk of VA at a younger age and more often received an implantable cardioverter-defibrillator [17]. Although patients in the definite ARVC group were more likely to experience severe arrhythmia and to show structural involvement, two patients (2%) in the non-definite group experienced sustained VT. This suggests that severe arrhythmia may occur at any stage of the disease, even in the absence of myocardial structural changes, making risk stratification challenging for those patients.
5 patients (13%) with non-definite ARVC diagnosis were found to have LGE in one or both ventricles (Table 4) (Fig. 2). Of those, three patients showed enhancement in the mid-anterior wall of the LV. In line with this, it has been reported that the subtricuspid/peritricuspid area and the LV inferolateral wall may be the most affected areas in the early stages of ARVC, and that the finding of LGE in ARVC patients is a predictor of all cause mortality and major adverse cardiovascular events [18]. Although LGE was not included in the 2010 TFC, our finding suggests the diagnostic utility of CMR-LGE to define those with non-definite ARVC disease.
Genetic family screening identifies individuals at risk of developing ARVC [19]. However, the current standard methods for screening do not identify all non-definite patients at risk of severe arrhythmia and may miss early structural involvement. Newer imaging techniques, such as deformation imaging by echocardiography, CMR-LGE and exercise echocardiography, could detect early structural involvement and identify those patients at risk, as several studies suggest. A study conducted by Leren et al. [19] aimed at investigating early arrhythmic markers in early ARVC. Of 73 patients with early ARVC, arrhythmic events occurred in 15 (21%). Those with arrhythmic events showed longer RV mechanical dispersion (RVMD), larger RV basal diameter and abnormal SAECG. These findings were replicated, with shorter RVMD in asymptomatic variant carriers compared with ARVC patients with arrhythmia. Importantly, biventricular strain was reduced, and MD was more pronounced in asymptomatic variant carriers compared to controls [20].
Limitations
Despite the fact that participants were recruited from a regional institution servicing a varied multi-ethnic community in the Midlands, the data were acquired from a single centre, which may restrict the generalisability of our findings. As not all our non-definite ARVC patients underwent genetic testing, our results could be confounded by the inclusion of untested first-degree relatives who might not have true ARVC. Larger non-definite ARVC cohorts are needed to confirm our results. Finally, cardiac magnetic resonance, SAECG, 24-h Holter monitoring and blood tests were not performed for all patients.
Conclusion
The findings of this study showed differences in clinical, electrical and imaging phenotype between definite and non-definite ARVC patients. Major adverse events were more common in definite ARVC patients but also occurred in non-definite ARVC. This single centre observational cohort study forms a basis for further prospective multicentre interventional studies.
Availability of data and materials
The anonymised datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ARVC:
-
Arrhythmogenic right ventricular cardiomyopathy
- VA:
-
Ventricular arrhythmias
- SCD:
-
Sudden cardiac death
- CMR:
-
Cardiovascular magnetic resonance
- ECG:
-
Electrocardiogram
- ICD:
-
Implantable cardioverter-defibrillator
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
- RV:
-
Right ventricle
- SCD:
-
Sudden cardiac death
- TFC:
-
Task force criteria
References
Zghaib T, Te Riele ASJM, James CA, Rastegar N, Murray B, Tichnell C, et al. Left ventricular fibro-fatty replacement in arrhythmogenic right ventricular dysplasia/cardiomyopathy: prevalence, patterns, and association with arrhythmias. J Cardiovasc Magn Reson. 2021. https://doi.org/10.1186/s12968-020-00702-3.
Cadrin-Tourigny J, Bosman LP, Wang W, Tadros R, Bhonsale A, Bourfiss M, et al. Sudden cardiac death prediction in arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythmia Electrophysiol. 2021;14(1):30–40. https://doi.org/10.1161/CIRCEP.120.008509.
Wallace R, Calkins H. Risk stratification in arrhythmogenic right ventricular cardiomyopathy. Arrhythmia Electrophysiol Rev. 2021;10(1):26–32.
Leone MP, Palumbo P, Saenen J, Mastroianno S, Castellana S, Amico C, et al. Phenotypic variability of a pathogenic PKP2 mutation in an Italian family affected by arrhythmogenic cardiomyopathy and juvenile sudden death: considerations from molecular autopsy to sport restriction. Front Cardiovasc Med. 2021. https://doi.org/10.3389/fcvm.2021.635141/full.
Elliott PM, Anastasakis A, Asimaki A, Basso C, Bauce B, Brooke MA, et al. Definition and treatment of arrhythmogenic cardiomyopathy: an updated expert panel report. Eur J Heart Fail. 2019;21(8):955–64. https://doi.org/10.1002/ejhf.1534.
van Lint FHM, Murray B, Tichnell C, Zwart R, Amat N, Lekanne Deprez RH, et al. Arrhythmogenic right ventricular cardiomyopathy-associated desmosomal variants are rarely De Novo. Circ Genomic Precis Med. 2019;12(8):337–44. https://doi.org/10.1161/CIRCGEN.119.002467.
Marcus FI, Fontaine GH, Guiraudon G, Frank R, Laurenceau JL, Malergue C, et al. Right ventricular dysplasia: a report of 24 adult cases. Ann Noninvasive Electrocardiol. 1999;4(1):97–111. https://doi.org/10.1111/j.1542-474X.1999.tb00372.x.
Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2010;121(13):1533–41. https://doi.org/10.1161/CIRCULATIONAHA.108.840827.
Gandjbakhch E, Redheuil A, Pousset F, Charron P, Frank R. Clinical diagnosis, imaging, and genetics of arrhythmogenic right ventricular cardiomyopathy/dysplasia. J Am Coll Cardiol. 2018;72(7):784–804.
Priori SG, Blomstrom-Lundqvist C, Mazzanti A, Bloma N, Borggrefe M, Camm J, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the Europea. Eur Heart J. 2015;36(41):2793–2867l.
Maron BJ, Chaitman BR, Ackerman MJ, Bayés de Luna A, Corrado D, Crosson JE, et al. Recommendations for physical activity and recreational sports participation for young patients with genetic cardiovascular diseases. Circulation. 2004;109(22):2807–16. https://doi.org/10.1161/01.CIR.0000128363.85581.E1.
Robinson S, Rana B, Oxborough D, Steeds R, Monaghan M, Stout M, et al. A practical guideline for performing a comprehensive transthoracic echocardiogram in adults: the British society of echocardiography minimum dataset. Echo Res Pract. 2020;7(4):G59-93. https://doi.org/10.1530/ERP-20-0026.
Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance (CMR) protocols 2013 update. J Cardiovasc Magn Reson. 2013;15(1):91. https://doi.org/10.1186/1532-429X-15-91.
Cox MGPJ, Van Der Zwaag PA, Van Der Werf C, Van Der Smagt JJ, Noorman M, Bhuiyan ZA, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy: pathogenic desmosome mutations in index-patients predict outcome of family screening: Dutch arrhythmogenic right ventricular dysplasia/cardiomyopathy genotype-phenotype follow-up study. Circulation. 2011;123(23):2690–700.
Akdis D, Saguner AM, Shah K, Wei C, Medeiros-Domingo A, Von Eckardstein A, et al. Sex hormones affect outcome in arrhythmogenic right ventricular cardiomyopathy/dysplasia: Froma stemcell derived cardiomyocyte-based model to clinical biomarkers of disease outcome. Eur Heart J. 2017;38(19):1498–508.
James CA, Bhonsale A, Tichnell C, Murray B, Russell SD, Tandri H, et al. Exercise increases age-related penetrance and arrhythmic risk in arrhythmogenic right ventricular dysplasia/cardiomyopathy–associated desmosomal mutation carriers. J Am Coll Cardiol. 2013;62(14):1290–7.
Gasperetti A, Dello Russo A, Busana M, Dessanai M, Pizzamiglio F, Saguner AM, et al. Novel risk calculator performance in athletes with arrhythmogenic right ventricular cardiomyopathy. Hear Rhythm. 2020;17(8):1251–9. https://doi.org/10.1016/j.hrthm.2020.03.007.
Liu Y, Yu J, Liu J, Wu B, Cui Q, Shen W, et al. Prognostic value of late gadolinium enhancement in arrhythmogenic right ventricular cardiomyopathy: a meta-analysis. Clin Radiol. 2021;76(8):628.e9-628.e15.
Marcus FI, Edson S, Towbin JA. Genetics of arrhythmogenic right ventricular cardiomyopathy. J Am Coll Cardiol. 2013;61(19):1945–8. https://doi.org/10.1016/j.jacc.2013.01.073.
Sarvari SI, Haugaa KH, Anfinsen O-G, Leren TP, Smiseth OA, Kongsgaard E, et al. Right ventricular mechanical dispersion is related to malignant arrhythmias: a study of patients with arrhythmogenic right ventricular cardiomyopathy and subclinical right ventricular dysfunction. Eur Heart J. 2011;32(9):1089–96. https://doi.org/10.1093/eurheartj/ehr069.
Acknowledgements
The authors would like to acknowledge the work of the cardiac physiologists at UHB, the cardiac radiographers at UHB CMR service, the ICC clinic nurses, James Hudson for reviewing the statistical methods and Dr Winnie Chua for expert advice on methods.
Funding
Partially funded by EU Horizon 2020 MAESTRIA (grant agreement number 965286) to LF and EU Horizon 2020 CATCH ME (grant agreement number 633196) to LF. The Institute of Cardiovascular Sciences received an Accelerator Award by the British Heart Foundation (AA/18/2/34218). AA’s PhD stipend is funded by the Royal Embassy of Saudi Arabia Cultural Bureau. RS acknowledges partial funding from the NIHR West Midlands Senior Clinical Scholarship. Disclosures: LF received institutional research grants for basic, translational and clinical research projects from the European Union, the British Heart Foundation, the Medical Research Council (UK), National Institute of Health Research, DZHK, DFG and several biomedical companies. LF is listed as inventor of two patents held by the University of Birmingham (Atrial Fibrillation Therapy WO 2015140571, Markers for Atrial Fibrillation WO 2016012783).
Author information
Authors and Affiliations
Contributions
AA conducted the background research and review, drafted the manuscript and collected the data. TK and SB collected data. RS and LF planned the study, reviewed patient files, supervised AA, SB and TK and wrote the manuscript. HC, BE, MK and LCS critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All experimental protocols were approved by the local clinical governance committee (audit number: Clinical Audit Registration and Management system by Birmingham’s Children’s Hospital Clinical Audit and Effectiveness Lead/University Hospital’s Birmingham, ((CARMS)-16044, 17734) and conformed to the Good Clinical Practice guidelines. The local clinical governance committee has the authority to approve and waive the ethical approval and informed consent. All methods were performed in accordance with the relevant guidelines and regulations. As this observational study was performed as part of an audit ((CARMS)-16044, 17734) in patients receiving standard NHS care, the clinical audit committee by Birmingham’s Children’s Hospital Clinical Audit and Effectiveness Lead/University Hospital’s Birmingham thereby waived the need of informed consent. From 2020, patients have given Human Biomaterial Resource Centre (HBRC), a Human Tissue Authority (HTA) licensed human sample biorepository operated by the University of Birmingham informed consent to provide blood samples and clinical data (study title: Heartbeat Matrix Pilot: Accelerating targeted treatments for patients with inherited heart diseases. REC reference: 20/LO/0184 IRAS project ID: 269251, REC name: London—West London & GTAC Research Ethics Committee).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests to the work in this submission.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Represents clinical, electrical and imaging data after excludig untested non-definite ARVC patients.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Aljehani, A., Kew, T., Baig, S. et al. Characterisation of patients referred to a tertiary-level inherited cardiac condition clinic with suspected arrhythmogenic right ventricular cardiomyopathy (ARVC). BMC Cardiovasc Disord 23, 14 (2023). https://doi.org/10.1186/s12872-022-03021-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-03021-w