Abstract
Background
Postoperative atrial fibrillation (POAF) is the most common arrhythmia after cardiac surgery, and its occurrence is closely related to inflammation. This paper intends to apply meta-analysis to investigate the effect of glucocorticoids on POAF.
Methods
PubMed, Embase, Web of Science, and Cochrane Library were searched using the internationally recognized systematic evaluation and retrieval strategy. Two review authors independently selected relevant studies and extracted data based on the Cochrane handbook for systematic reviews of interventions approach. Stata 17 was used for data analysis. In the subgroup analysis, we grouped the participant data according to differences in glucocorticoids dose and type of surgery. At the same time, we also conducted a meta-analysis on the possible infection and gastrointestinal injury caused by glucocorticoids use.
Results
27 studies and 14,442 patients were finally included. Results from the random-effects model indicated that the incidence of POAF was lower in glucocorticoid group (RR 0.80, 95% CI 0.71–0.92, P = 0.001). According to the subgroup analysis result, low doses of glucocorticoids reduced the incidence of POAF (RR 0.81, 95% CI 0.71–0.92, P = 0.001). The effect of high doses glucocorticoids on the POAF was not statistically significant (RR 0.81, 95% CI 0.56–1.19, P = 0.286). In the coronary artery bypass grafting (CABG) subgroup, the glucocorticoids reduced the incidence of POAF (RR 0.71, 95% CI 0.58–0.87, P = 0.001). In the CABG OR Valvular Surgery group, the effect of glucocorticoids on POAF was not statistically significant (RR 0.88, 95% CI 0.75–1.03, P = 0.108). 15 studies documented postoperative complications of infection, two studies were excluded from the system because the end point event was 0, and meta-analysis showed no increased risk of infection from glucocorticoid use (RR 0.85, 95% CI 0.68–1.06, P = 0.158). Eight studies documented the effects of glucocorticoids on gastrointestinal diseases, and meta-analysis showed no differences between the two groups (RR 1.12, 95% CI 0.83–1.50, P = 0.450).
Conclusion
The use of glucocorticoids can reduce the incidence of POAF. The subgroup analysis result showed that low-dose glucocorticoids were more effective than high-dose glucocorticoids in inhibiting POAF. The use of glucocorticoids in CABG alone can better inhibit the occurrence of POAF. The effects of glucocorticoids on infection and gastrointestinal injury were not statistically significant.
Review registration: PROSPERO, CRD42022304521.
Similar content being viewed by others
Introduction
POAF is the most common arrhythmia after CABG and valve surgery, with an overall incidence of 20% to 40% and a higher incidence of approximately 30% to 50% in valve surgery [1]. POAF is closely relevant to stroke, hospital stay time, and the cost of treatment [2, 3]. The pathological mechanism of POAF is very complex, and it is related to many factors. At present, the study about POAF is increasing rapidly, but no clear conclusion has been reached. Relevant research found that the main influencing factors are structure and electrical reconstruction. Furthermore, an increased adrenergic tone and changes in metabolic milieus are also possible mechanisms of POAF [4].
Data suggests that inflammation might lead to the POAF [5]. Trauma, ischemia/reperfusion, and cardiopulmonary bypass during cardiac surgery can induce systemic inflammation; this inflammatory response is closely related to the occurrence of POAF [6,7,8,9]. Glucocorticoids can inhibit inflammation and, as a result, may decrease the POAF risk. The effects of glucocorticoids on POAF have been researched widely in many countries. According to previous study result, glucocorticoids reduce postoperative C-reactive protein (CRP) levels, leukocytes, and other inflammatory markers; but the conclusions of these studies are controversial [10, 11]. Thus, we conducted this meta-analysis to investigate the effect of glucocorticoids on POAF.
Methods
Literature search strategy and criteria
PubMed, Embase, and Cochrane Library were searched based on internationally recognized systematic evaluation and retrieval strategy. Retrieval of data began from the establishment of the database through December 2021. The search terms were as follows: “Postoperative atrial fibrillation”, “POAF”, “Cardiac surgery”, “CABG”, “Cardiac valve surgery”, “atrial fibrillation”, “AF”, “Glucocorticoids”, “Glucocorticoid”, “Steroid”, “Corticosteroid” and other individual drug names. Articles were also identified by referring to the references of each study to supplement the data.
Inclusion and exclusion criteria
Inclusion criteria: (1) randomized controlled trial (RCT) with glucocorticoids treatment and placebo control; (2) all patients required surgical treatment and had no atrial fibrillation before surgery, where the types of procedures included were CABG, cardiac valve surgery, and CABG combined with valve surgery; (3) published literature.
Exclusion criteria: (1) age less than 18 years; (2) cardiovascular risk factors were not considered as primary or secondary endpoints; (3) the full text of the study is not available.
Quality assessment and data extraction
This meta-analysis was reported per the Preferred reporting items for systematic reviews and Meta-Analyses (PRISMA) guidelines.
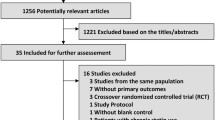
The data collected in this study were screened and extracted by 2 researchers (Zhongzheng Zhou and Xin He) in strict accordance with the exclusion criteria according to the established retrieval strategy. The Cochrane risk-of-bias assessment tool (RoB 2) was used to evaluate literature bias [12]. Figure 1 shows the flowchart of the literature retrieval (Additional file 1).
Statistical treatment
In this study, the correlation of glucocorticoids and POAF risk was evaluated by indexes of relative risk (RR) and 95% confidence interval (CI). The RR was used to evaluated glucocorticoids group and placebo group, the glucocorticoids group refers to the use of glucocorticoids before or after surgery, while placebo group refers to the use of an equal dose of saline as placebo. Both Cochran’s Q test and I2 index were applied to measure the heterogeneity, where heterogeneity was quantified by I2, the range of which is 0 to 100% (judge criteria I2 = 0–25%, no; I2 = 25–50%, low; I2 = 50–75%, moderate; I2 = 75–100%, high heterogeneity). In the comprehensive effect study, the random effect model was selected, and subgroup analysis was conducted according to different doses. On this basis, the possible sources of heterogeneity were discussed. The possibility of publication bias was evaluated by Egger test method [13]. The sensitivity is determined by excluding one study at a time, and then the impact of a single study on the overall research results is analyzed. The judgment basis of statistical difference was set as P < 0.05. Stata 17 software was used for data analysis.
In addition, two subgroup analyses were conducted, the first subgroup research was conducted based on the dose of glucocorticoids. Patients who were administered dexamethasone doses lower or equal to 100 mg were placed in the low-dose group, and patients who were administered dexamethasone doses higher than 100 mg were classified into high-dose group (where different types of glucocorticoids are converted to equivalent doses of dexamethasone). Previous studies indicated that 100 mg dexamethasone might achieve a balance between efficacy and safety, so we used the 100 mg dose as the standard for subgroup analysis [39]. Second, we divided them into CABG group and CABG OR Valvular surgery group for subgroup analysis according to different surgical types, where the CABG group refers to patients who underwent CABG alone, and the CABG OR Valvular surgery group refers to patients who had valve surgery or CABG combined with valve surgery.
Results
Literature search
The literature search process is depicted in Fig. 1. 3743 studies were identified by searching each database according to the search keywords. The titles, abstracts, and full texts of the initially detected literature were read, and 27 studies were included based on above criteria [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40].
Study characteristics
Across the included studies, 14,442 patients were enrolled. Table 1 shows the basic feature and quality assessment results of the selected studies. The regions involved in these studies mainly include the EU, Asia and USA Interventions in the trial group included dexamethasone, methylprednisolone, and hydrocortisone. Figure 2 summarizes the results of quality assessment of each study according to the Cochrane risk-of-bias assessment tool (RoB 2).
Correlation between glucocorticoids and POAF
A total of 27 studies evaluated the influence of glucocorticoids on POAF; in total, there were 7260 cases in glucocorticoids group and 7182 cases in control group. According to the result of Fig. 3, incidence of POAF in glucocorticoid group is lower (RR 0.80, 95% CI 0.71–0.92, P = 0.001). In certain range, low doses glucocorticoids can reduce the POAF risk (RR 0.81, 95% CI 0.71–0.92, P = 0.001). The risk of POAF was not significantly different between the high-dose glucocorticoids group and the placebo group (RR 0.81, 95% CI 0.56–1.19, P = 0.286). In the CABG subgroup, the glucocorticoids reduced the POAF risk (RR 0.71, 95% CI 0.58–0.87, P = 0.001). In the CABG OR Valvular Surgery group, the effect of glucocorticoids on POAF was not statistically significant (RR 0.88, 95% CI 0.75–1.03, P = 0.108) (see Table 2).
A total of 15 studies documented postoperative complications of infection. However, two studies were excluded from the system because the end point event was 0, and meta-analysis showed no increased risk of infection from glucocorticoid use (RR 0.85, 95% CI 0.68–1.06, P = 0.158) (see Fig. 4). And 8 studies documented the effects of glucocorticoids on gastrointestinal diseases, and meta-analysis showed no differences between the glucocorticoid and the control group (RR 1.12, 95% CI 0.83–1.50, P = 0.450) (see Fig. 5).
Publication bias evaluation and sensitivity analysis
In the research process, publication bias were evaluated based on Egger’s test, and the relevant result is shown in Fig. 6. The results of Egger's test were close to the critical value, suggesting that there might be publication bias in the analysis results (P = 0.050). Sensitivity analysis was conducted on the three study endpoints. We used the leave-one-out analysis method for sensitivity analysis. The vertical axis represents the study type, and the horizontal axis represents the combined results after excluding a certain study. Sensitivity analysis results showed that excluding any study, the combined results of the remaining studies would not affect the end point outcome, proving that the conclusion was stable (see Fig. 7).
Discussion
Meta-analysis was used to judge the effect of glucocorticoids use on POAF. The results showed a lower POAF risk in glucocorticoids group, while subgroup analysis showed that low-dose glucocorticoids decreased the incidence of POAF compared to high-dose glucocorticoids. Previous studies on the influence of glucocorticoids on POAF were controversial; some previous studies have yielded positive results, while others have been negative. Past studies included small sample sizes, Van Osch's study was a single-center substudy of the DECS study [38], and the SIRS study [39] was a large controlled trial. Their results suggest that glucocorticoids have no correlation with the incidence of POAF. But the controlled experiment conducted by Al-Shawabkeh in 2016 suggested that glucocorticoids reduced the incidence of that [40]. Therefore, we included patients with all types of surgery for this meta-analysis.
POAF usually occurs during the initial 4 days after cardiac surgery; it is closely related to the type of surgery, with an incidence about (20–30%) in CABG surgery, (30–50%) in valvular surgery and a higher incidence in valvular combined coronary artery bypass surgery (60–80%) [41, 42]. Some school found that the occurrence of POAF is closely related to the prolongation of postoperative hospital stay and the increases in treatment cost [43, 44]. POAF is usually self-limited, and most of cases return to normal on their own within 24 h of onset [45]; although some patients will relapse within 2 days of the first attack [46]. The pathogenesis of POAF is mainly related to local inflammatory reaction [47, 48], adrenergic activation [49], electrolyte disturbances [50], atrial stimulation [51] and prolonged mechanical ventilation [42]. Among them, the inflammatory response is considered to be the most important pathogenesis of POAF [52]. The concentrations of CRP [53], number of white blood cells in POAF patients are higher than those in patients with sinus rhythm [54, 55]; the increase of these inflammatory indicators is closely related to the occurrence of POAF [56, 57]. Glucocorticoids can effectively reduce inflammatory reactions [58], thus reducing the incidence of POAF.
The anti-inflammatory mechanism of glucocorticoids is mainly through inhibiting the activity of immunomodulatory transcription factors such as NF-KB,AP-1, which is dose-dependent. The higher the dose, the stronger the inhibition effect [59]. But in our study, it was found that compared to the high-dose glucocorticoids, low-dose glucocorticoids were more effective in inhibiting the occurrence of POAF. There are a few possible causes for this observation. First, high doses of glucocorticoids cause high expression of calcium regulator mRNA, which can shorten the action potential refractory period and induce arrhythmia. Oakley analyzed the signal pathways related to dysregulated genes, and the results showed that the mechanism of glucocorticoids on POAF might be as follows: improving the expression of voltage-gated L-type calcium channel (LTCC), sarcoplasmic/endoplasmic reticulum calcium adenosine triphosphatase 2 (SERCA2), sodium/calcium exchanger 1 (NCX1) and RyR2 genes, this result has important reference value for the pathological study of POAF [60, 61]; this abnormal expression may contribute to the development of arrhythmias. Second, glucocorticoids can activate the renin–angiotensin–aldosterone system (RASS) system, leading to increased blood pressure, rapid heart rate [62, 63]. High doses of glucocorticoids over-activate the RASS system and the sympathetic nervous system, increasing the risk of arrhythmias. Third, intravenous methylprednisolone alters myocardial cell stimulation thresholds and sodium metabolism. These changes may lead to the variation of electrolyte shifts in the membranes of the heart muscle, result in arrhythmias [64, 65]. Fourth, the use of high doses of glucocorticoids can induce insulin resistance, which may prevent glucose from entering cardiac muscle cells, aggravate an ischemic injury, and induce arrhythmias [49].Low-doses of glucocorticoids are less likely to cause these adverse reactions and may have a better control effect on POAF. We investigated the influence of glucocorticoids on AF after different types of surgery, glucocorticoids reduced the incidence of POAF in CABG group, but the effect of glucocorticoids in combined group was not statistically significant. We hypothesized that this may be due to the lower incidence of POAF and the lower inflammatory response in CABG alone.
The main side effects of glucocorticoids are gastrointestinal bleeding and an high risk of infection, which limits the application of glucocorticoids in heart surgery. We also conducted a meta-analysis of these risks, 12,126 cases were enrolled in 15 studies to assess the effects of glucocorticoids on infections including mediastinal, pulmonary, digestive and urinary tract infections, suggesting that glucocorticoids use did not lead to an higher risk of infection. Besides, a total of 11,155 patients were enrolled in 8 studies to assess the effect of glucocorticoids on gastrointestinal injury, including postoperative gastrointestinal bleeding, vomiting, gastrointestinal ulceration, or gastrointestinal dysfunction, meta-analysis results suggested that the effect of glucocorticoids on gastrointestinal injury was not significant. The present results seem to be at variance with our past consensus, and we speculate that this may be due to the shorter duration of glucocorticoid use in all studies and the smaller single dose, which needs to be confirmed in more and larger controlled trials. In addition to increased risk of infection and gastrointestinal damage, the use of glucocorticoids may cause abnormal glucose tolerance, electrolyte disorder, abnormal fat metabolism, osteoporosis, slow wound healing, nervous system abnormalities, and even lead to thromboembolism. When the drug is stopped for a long time, it can also lead to withdrawal reaction, adrenal cortical dysfunction, hypotension, and even shock. These side effects also limit the further use of glucocorticoids.
Limitations
Firstly, the heterogeneity of the primary end points was too high. Subgroup analysis was conducted, but our grouping criteria were established in advance. In the second subgroup analysis, we found a significant reduction in heterogeneity in the CABG group, in the CABG OR Valvular Surgery group, the heterogeneity was significantly higher than that in the CABG group due to the inclusion of patients undergoing combined surgery. And in valve surgery, different valve lesions have different effects on cardiac function. Therefore, we believe that the differences in surgical methods are the main reason for the heterogeneity. In future trials, we plan to conduct more rigorous surgical classification to reduce heterogeneity. Due to the differences in drug sensitivity among the included population and the large differences in the dose of glucocorticoids used in each subgroup, this may be another factor leading to the generation of heterogeneity. We analyzed and discussed the source of heterogeneity in Limitations and finally choose to use random effect model to synthesize heterogeneity, and we cautiously recommend the final conclusion. Secondly, there was a lack of recent large clinical studies.
Conclusions
The results of this study showed that glucocorticoids were beneficial in reducing the effect of POAF, and low-dose glucocorticoids could reduce the incidence of POAF. However, heterogeneity of overall study and subgroup analysis was high, so we held a cautious recommendation. Our study also did not find that glucocorticoids use increased the risk of infection and gastrointestinal injury.
Availability of data and materials
We declare that the data supporting the conclusions of this article are fully described within the article.
Abbreviations
- POAF:
-
Postoperative atrial fibrillation
- CRP:
-
C-reactive protein
- CABG:
-
Coronary artery bypass graft
- RCT:
-
Randomized controlled trial
- PRISMA:
-
The Preferred reporting items for systematic reviews and Meta-Analyses
- CI:
-
Confidence interval
- RR:
-
Relative risk
- LTCC:
-
L-type calcium Channel
- SERCA2:
-
Sarcoplasmic/endoplasmic reticulum calcium adenosine triphosphatase 2
- NCX1:
-
Sodium/calcium exchanger 1
- RASS:
-
Renin–angiotensin–aldosterone system
- RoB 2:
-
Cochrane risk-of-bias assessment tool (RoB 2)
References
Bessissow A, Khan J, Devereaux PJ, Alvarez-Garcia J, Alonso-Coello P. Postoperative atrial fibrillation in non-cardiac and cardiac surgery: an overview. J Thromb Haemost. 2015;13(Suppl 1):S304–12. https://doi.org/10.1111/jth.12974.
Almassi GH, Schowalter T, Nicolosi AC, Aggarwal A, Moritz TE, Henderson WG, et al. Atrial fibrillation after cardiac surgery: a major morbid event? Ann Surg. 1997;226(4):501–11; discussion 511–3. https://doi.org/10.1097/00000658-199710000-00011.
Hakala T, Pitkänen O, Hippeläinen M. Feasibility of predicting the risk of atrial fibrillation after coronary artery bypass surgery with logistic regression model. Scand J Surg. 2002;91(4):339–44. https://doi.org/10.1177/145749690209100406.
Anselmi A, Possati G, Gaudino M. Postoperative inflammatory reaction and atrial fibrillation: simple correlation or causation? Ann Thorac Surg. 2009;88(1):326–33. https://doi.org/10.1016/j.athoracsur.2009.01.031.
Shingu Y, Kubota S, Wakasa S, Ooka T, Tachibana T, Matsui Y. Postoperative atrial fibrillation: mechanism, prevention, and future perspective. Surg Today. 2012;42(9):819–24. https://doi.org/10.1007/s00595-012-0199-4.
Fillinger MP, Rassias AJ, Guyre PM, Sanders JH, Beach M, Pahl J, et al. Glucocorticoid effects on the inflammatory and clinical responses to cardiac surgery. J Cardiothorac Vasc Anesth. 2002;16(2):163–9. https://doi.org/10.1053/jcan.2002.31057.
Marik PE, Fromm R. The efficacy and dosage effect of corticosteroids for the prevention of atrial fibrillation after cardiac surgery: a systematic review. J Crit Care. 2009;24(3):458–63. https://doi.org/10.1016/j.jcrc.2008.10.016.
Jakubová M, Mitro P, Stančák B, Sabol F, Kolesár A, Cisarik P, et al. The occurrence of postoperative atrial fibrillation according to different surgical settings in cardiac surgery patients. Interact Cardiovasc Thorac Surg. 2012;15(6):1007–12. https://doi.org/10.1093/icvts/ivs361.
Dieleman JM, de Wit GA, Nierich AP, Rosseel PM, van der Maaten JM, Hofland J, et al. Long-term outcomes and cost effectiveness of high-dose dexamethasone for cardiac surgery: a randomised trial. Anaesthesia. 2017;72(6):704–13. https://doi.org/10.1111/anae.13853.
Jansen NJ, van Oeveren W, van den Broek L, Oudemans-van Straaten HM, Stoutenbeek CP, Joen MC, et al. Inhibition by dexamethasone of the reperfusion phenomena in cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1991;102(4):515–25.
El Azab SR, Rosseel PM, de Lange JJ, Groeneveld AB, van Strik R, van Wijk EM, et al. Dexamethasone decreases the pro- to anti-inflammatory cytokine ratio during cardiac surgery. Br J Anaesth. 2002;88(4):496–501. https://doi.org/10.1093/bja/88.4.496.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. https://doi.org/10.1136/bmj.l4898.
Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018;74(3):785–94. https://doi.org/10.1111/biom.12817.
Chaney MA, Nikolov MP, Blakeman B, et al. Pulmonary effects of methylprednisolone in patients undergoing coronary artery bypass grafting and early tracheal extubation. Anesth Analg. 1998;87(1):27–33.
Schurr UP, Zünd G, Hoerstrup SP, et al. Preoperative administration of steroids: influence on adhesion molecules and cytokines after cardiopulmonary bypass. Ann Thorac Surg. 2001;72(4):1316–20.
Yared JP, Starr NJ, Torres FK, Bashour CA, Bourdakos G, Piedmonte M, et al. Effects of single dose, postinduction dexamethasone on recovery after cardiac surgery. Ann Thorac Surg. 2000;69(5):1420–4. https://doi.org/10.1016/s0003-4975(00)01180-2.
Fillinger MP, Rassias AJ, Guyre PM, et al. Glucocorticoid effects on the inflammatory and clinical responses to cardiac surgery. J Cardiothorac Vasc Anesth. 2002;16(2):163–9.
Halvorsen P, Ræder J, White PF, Almdahl SM, Nordstrand K, Saatvedt K, et al. The effect of dexamethasone on side effects after coronary revascularization procedures. Anesth Analg. 2003;96(6):1578–83. https://doi.org/10.1213/01.ANE.0000063922.90966.3A.
Oliver WC Jr, Nuttall GA, Orszulak TA, et al. Hemofiltration but not steroids results in earlier tracheal extubation following cardiopulmonary bypass: a prospective, randomized double-blind trial. Anesthesiology. 2004;101(2):327–39.
Prasongsukarn K, Abel JG, Jamieson WR, Cheung A, Russell JA, Walley KR, et al. The effects of steroids on the occurrence of postoperative atrial fibrillation after coronary artery bypass grafting surgery: a prospective randomized trial. J Thorac Cardiovasc Surg. 2005;130(1):93–8. https://doi.org/10.1016/j.jtcvs.2004.09.014.
Sano T, Morita S, Masuda M, et al. Minor infection encouraged by steroid administration during cardiac surgery. Asian Cardiovasc Thorac Ann. 2006;14(6):505–10.
Enc Y, Karaca P, Ayoglu U, et al. The acute cardioprotective effect of glucocorticoid in myocardial ischemia-reperfusion injury occurring during cardiopulmonary bypass. Heart Vessels. 2006;21(3):152–6.
Whitlock RP, Young E, Noora J, et al. Pulse low dose steroids attenuate post-cardiopulmonary bypass SIRS. SIRS I J Surg Res. 2006;132(2):188–94.
Halonen J, Halonen P, Järvinen O, Taskinen P, Auvinen T, Tarkka M, et al. Corticosteroids for the prevention of atrial fibrillation after cardiac surgery: a randomized controlled trial. JAMA. 2007;297(14):1562–7. https://doi.org/10.1001/jama.297.14.1562.
Yared JP, Bakri MH, Erzurum SC, Moravec CS, Laskowski DM, Van Wagoner DR, et al. Effect of dexamethasone on atrial fibrillation after cardiac surgery: prospective, randomized, double-blind, placebo-controlled trial. J Cardiothorac Vasc Anesth. 2007;21(1):68–75. https://doi.org/10.1053/j.jvca.2005.10.014.
Sobieski MA 2nd, Graham JD, Pappas PS, et al. Reducing the effects of the systemic inflammatory response to cardiopulmonary bypass: can single dose steroids blunt systemic inflammatory response syndrome? ASAIO J. 2008;54(2):203–6.
Amr YM, Elmistekawy E, El-Serogy H. Effects of dexamethasone on pulmonary and renal functions in patients undergoing CABG with cardiopulmonary bypass. Semin Cardiothorac Vasc Anesth. 2009;13(4):231–7.
Weis F, Beiras-Fernandez A, Schelling G, et al. Stress doses of hydrocortisone in high-risk patients undergoing cardiac surgery: effects on interleukin-6 to interleukin-10 ratio and early outcome. Crit Care Med. 2009;37(5):1685–90.
Mauermann WJ, Nuttall GA, Cook DJ, Hanson AC, Schroeder DR, Oliver WC. Hemofiltration during cardiopulmonary bypass does not decrease the incidence of atrial fibrillation after cardiac surgery. Anesth Analg. 2010;110(2):329–34. https://doi.org/10.1213/ANE.0b013e3181c76bd3.
Vukovic PM, Maravic-Stojkovic VR, Peric MS, et al. Steroids and statins: an old and a new anti-inflammatory strategy compared. Perfusion. 2011;26(1):31–7.
Murphy GS, Sherwani SS, Szokol JW, et al. Small-dose dexamethasone improves quality of recovery scores after elective cardiac surgery: a randomized, double-blind, placebo-controlled study. J Cardiothorac Vasc Anesth. 2011;25(6):950–60.
Mirhosseini SJ, Forouzannia SK, Sayegh AH, Sanatkar M. Effect of prophylactic low dose of methylprednisolone on postoperative new atrial fibrillation and early complications in patients with severe LV dysfunction undergoing elective off-pump coronary artery bypass surgery. Acta Med Iran. 2011;49(5):288–92.
Kilger E, Heyn J, Beiras-Fernandez A, et al. Stress doses of hydrocortisone reduce systemic inflammatory response in patients undergoing cardiac surgery without cardiopulmonary bypass. Minerva Anestesiol. 2011;77(3):268–74.
Dieleman JM, Nierich AP, Rosseel PM, et al. Intraoperative high-dose dexamethasone for cardiac surgery: a randomized controlled trial. JAMA. 2012;308(17):1761–7.
Abbaszadeh M, Khan ZH, Mehrani F, et al. Perioperative intravenous corticosteroids reduce incidence of atrial fibrillation following cardiac surgery: a randomized study. Rev Bras Cir Cardiovasc. 2012;27(1):18–23.
Suezawa T, Aoki A, Kotani M, Tago M, Kobayashi O, Hirasaki A, et al. Clinical benefits of methylprednisolone in off-pump coronary artery bypass surgery. Gen Thorac Cardiovasc Surg. 2013;61(8):455–9. https://doi.org/10.1007/s11748-013-0206-8.
Jacob KA, Dieleman JM, Nathoe HM, et al. The effects of intraoperative dexamethasone on left atrial function and postoperative atrial fibrillation in cardiac surgical patients. Neth Heart J. 2015;23(3):168–73.
Van Osch D, Dieleman JM, van Dijk D, Jacob KA, Kluin J, Doevendans PA, et al; DExamethasone for Cardiac Surgery (DECS) study group; DExamethasone for Cardiac Surgery DECS study group. Dexamethasone for the prevention of postoperative atrial fibrillation. Int J Cardiol. 2015;182:431–7. https://doi.org/10.1016/j.ijcard.2014.12.094.
Whitlock RP, Devereaux PJ, Teoh KH, Lamy A, Vincent J, Pogue J, et al. SIRS Investigators. Methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;386(10000):1243–1253. https://doi.org/10.1016/S0140-6736(15)00273-1.
Al-Shawabkeh Z, Al-Nawaesah K, Anzeh RA, et al. Use of short-term steroids in the prophylaxis of atrial fibrillation after cardiac surgery. J Saudi Heart Assoc. 2017;29(1):23–9.
Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol. 2008;51(8):793–801. https://doi.org/10.1016/j.jacc.2007.10.043.
Helgadottir S, Sigurdsson MI, Ingvarsdottir IL, Arnar DO, Gudbjartsson T. Atrial fibrillation following cardiac surgery: risk analysis and long-term survival. J Cardiothorac Surg. 2012;7:87. https://doi.org/10.1186/1749-8090-7-87.
Aranki SF, Shaw DP, Adams DH, Rizzo RJ, Couper GS, VanderVliet M, et al. Predictors of atrial fibrillation after coronary artery surgery. Current trends and impact on hospital resources. Circulation. 1996;94(3):390–7. https://doi.org/10.1161/01.cir.94.3.390.
Hravnak M, Hoffman LA, Saul MI, Zullo TG, Whitman GR. Resource utilization related to atrial fibrillation after coronary artery bypass grafting. Am J Crit Care. 2002;11(3):228–38.
Auer J, Weber T, Berent R, Ng CK, Lamm G, Eber B. Risk factors of postoperative atrial fibrillation after cardiac surgery. J Card Surg. 2005;20(5):425–31. https://doi.org/10.1111/j.1540-8191.2005.2004123.x.
Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. Investigators of the Ischemia Research and Education Foundation; Multicenter Study of Perioperative Ischemia Research Group. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291(14):1720–9. https://doi.org/10.1001/jama.291.14.1720.
Ishii Y, Schuessler RB, Gaynor SL, Yamada K, Fu AS, Boineau JP, et al. Inflammation of atrium after cardiac surgery is associated with inhomogeneity of atrial conduction and atrial fibrillation. Circulation. 2005;111(22):2881–8. https://doi.org/10.1161/CIRCULATIONAHA.104.475194.
Gaudino M, Andreotti F, Zamparelli R, Di Castelnuovo A, Nasso G, Burzotta F, et al. The -174G/C interleukin-6 polymorphism influences postoperative interleukin-6 levels and postoperative atrial fibrillation Is atrial fibrillation an inflammatory complication? Circulation. 2003;108(Suppl 1):II195–9. https://doi.org/10.1161/01.cir.0000087441.48566.0d.
Hogue CW Jr, Domitrovich PP, Stein PK, Despotis GD, Re L, Schuessler RB, Kleiger RE, et al. RR interval dynamics before atrial fibrillation in patients after coronary artery bypass graft surgery. Circulation. 1998;98(5):429–34. https://doi.org/10.1161/01.cir.98.5.429.
Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. Investigators of the Ischemia Research and Education Foundation; Multicenter Study of Perioperative Ischemia Research Group. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291(14):1720–9. doi: https://doi.org/10.1001/jama.291.14.1720.
Funk M, Richards SB, Desjardins J, Bebon C, Wilcox H. Incidence, timing, symptoms, and risk factors for atrial fibrillation after cardiac surgery. Am J Crit Care. 2003;12(5):424–33; quiz 434–5.
Dimmer C, Tavernier R, Gjorgov N, Van Nooten G, Clement DL, Jordaens L. Variations of autonomic tone preceding onset of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol. 1998;82(1):22–5. https://doi.org/10.1016/s0002-9149(98)00231-8.
Bruins P, te Velthuis H, Yazdanbakhsh AP, Jansen PG, van Hardevelt FW, de Beaumont EM, et al. Activation of the complement system during and after cardiopulmonary bypass surgery: postsurgery activation involves C-reactive protein and is associated with postoperative arrhythmia. Circulation. 1997;96(10):3542–8. https://doi.org/10.1161/01.cir.96.10.3542.
Lamm G, Auer J, Weber T, Berent R, Ng C, Eber B. Postoperative white blood cell count predicts atrial fibrillation after cardiac surgery. J Cardiothorac Vasc Anesth. 2006;20(1):51–6. https://doi.org/10.1053/j.jvca.2005.03.026.
Ishida K, Kimura F, Imamaki M, Ishida A, Shimura H, Kohno H, et al. Relation of inflammatory cytokines to atrial fibrillation after off-pump coronary artery bypass grafting. Eur J Cardiothorac Surg. 2006;29(4):501–5. https://doi.org/10.1016/j.ejcts.2005.12.028.
Hak Ł, Myśliwska J, Wieckiewicz J, Szyndler K, Siebert J, Rogowski J. Interleukin-2 as a predictor of early postoperative atrial fibrillation after cardiopulmonary bypass graft (CABG). J Interferon Cytokine Res. 2009;29(6):327–32. https://doi.org/10.1089/jir.2008.0082.2906.
Bruins P, te Velthuis H, Eerenberg-Belmer AJ, Yazdanbakhsh AP, de Beaumont EM, Eijsman L, et al. Heparin-protamine complexes and C-reactive protein induce activation of the classical complement pathway: studies in patients undergoing cardiac surgery and in vitro. Thromb Haemost. 2000;84(2):237–43.
Patti G, Chello M, Candura D, Pasceri V, D’Ambrosio A, Covino E, Di Sciascio G. Randomized trial of atorvastatin for reduction of postoperative atrial fibrillation in patients undergoing cardiac surgery: results of the ARMYDA-3 (Atorvastatin for Reduction of MYocardial Dysrhythmia After cardiac surgery) study. Circulation. 2006;114(14):1455–61. https://doi.org/10.1161/CIRCULATIONAHA.106.621763.
Coutinho AE, Chapman KE. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol. 2011;335(1):2–13. https://doi.org/10.1016/j.mce.2010.04.005.
Oakley RH, Cruz-Topete D, He B, Foley JF, Myers PH, Xu X, et al. Cardiomyocyte glucocorticoid and mineralocorticoid receptors directly and antagonistically regulate heart disease in mice. Sci Signal. 2019;12(577):eaau9685. https://doi.org/10.1126/scisignal.aau9685.
Cruz-Topete D, Oakley RH, Carroll NG, He B, Myers PH, Xu X, et al. Deletion of the cardiomyocyte glucocorticoid receptor leads to sexually dimorphic changes in cardiac gene expression and progression to heart failure. J Am Heart Assoc. 2019;8(15):e011012. https://doi.org/10.1161/JAHA.118.011012.
Yang S, Zhang L. Glucocorticoids and vascular reactivity. Curr Vasc Pharmacol. 2004;2(1):1–12. https://doi.org/10.2174/1570161043476483.
Sato A, Suzuki H, Nakazato Y, Shibata H, Inagami T, Saruta T. Increased expression of vascular angiotensin II type 1A receptor gene in glucocorticoid-induced hypertension. J Hypertens. 1994;12(5):511–6.
Kumari R, Uppal SS. First report of supraventricular tachycardia after intravenous pulse methylprednisolone therapy, with a brief review of the literature. Rheumatol Int. 2005;26(1):70–3. https://doi.org/10.1007/s00296-005-0589-7.
Moretti R, Torre P, Antonello RM, Zorzon M, Cazzato G. Recurrent atrial fibrillation associated with pulse administration of high doses of methylprednysolone: a possible prophylactic treatment. Eur J Neurol. 2000;7(1):130. https://doi.org/10.1046/j.1468-1331.2000.00026.x.
Acknowledgements
None.
Funding
This work was supported by The Scientific Research Institution Performance Incentive and Guidance Special Project of Chongqing (cstc2019jxj1130010).
Author information
Authors and Affiliations
Contributions
ZZ and YL designed the methods and carried out the statistical analyses. ZZ, XH and YL made substantial contributions to the acquisition and analysis of the data and to the interpretation of data. All the authors contributed to the data extraction, drafted the article, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Literature retrieval Method.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, Z., Long, Y., He, X. et al. Effects of different doses of glucocorticoids on postoperative atrial fibrillation: a meta-analysis. BMC Cardiovasc Disord 23, 16 (2023). https://doi.org/10.1186/s12872-022-03001-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-03001-0