Abstract
Background
Neutrophils and high-density lipoprotein cholesterol (HDL-c) play critical roles in the pathogenesis of acute myocardial infarction. We aimed to investigate the value of neutrophils count to high-density lipoprotein cholesterol ratio (NHR) in predicting occurrence of in-hospital adverse events in ST-segment elevation myocardial infarction (STEMI) patients treated with primary percutaneous coronary intervention (PPCI).
Methods
We retrospectively analyzed 532 patients who had been diagnosed with acute STEMI and treated with PPCI. Demographic and clinical data, admission laboratory parameters and NHR values were recorded. Major adverse cardiac events (MACE) were defined as stent thrombosis, cardiac rupture, cardiac arrest, ventricular aneurysm, malignant arrhythmia and cardiac death. Based on the receiver operating characteristic (ROC) analysis, all patients were divided into 2 groups based on the cut-off NHR value (NHR ≤ 11.28, NHR > 11.28). Cox regression analyses and the Kaplan–Meier survival curve were used to assess the prognostic ability of NHR in in-hospital MACE.
Results
MACE was observed in 72 patients (13.5%) during in-hospital follow-up. NHR was significantly higher in MACE group compared to MACE-free group (10.93 [6.26–13.97] vs. 8.13 [5.89–11.16]; P = 0.001). The incidence of in-hospital MACE was significantly higher in the NHR > 11.28 group than in NHR ≤ 11.28 group (24.8% vs. 9.6%; P < 0.001). In multivariable Cox regression analyses, ALT, Killip III-IV and increased NHR (hazard ratio, 2.211; 95% confidence interval,1.092–4.479; P = 0.027) were identified as independent predictive factors of occurrence of in-hospital MACE. Higher NHR group had worse cumulative survival compared with the lower group.
Conclusions
NHR value on admission, which is an easily calculated and universally available maker, may be useful in in-hospital risk classification of STEMI patients undergoing PPCI.
Similar content being viewed by others
Introduction
Acute myocardial infarction (AMI) is a major cause of global morbidity and mortality. Despite the improvements in reperfusion strategies, the outcome of patients with AMI remains unsatisfactory. Early risk stratification and timely interventions are significant in improving the prognosis of these patients.
Atherosclerosis and atherosclerotic plaque rupture are the main causes of STEMI. Atherosclerosis is characterized by inflammation and abnormal lipid metabolism and may cause plaque rupture in patients with certain risk factors [1,2,3,4]. Also, previous study showed that baseline inflammation status was an important factor in stent restenosis in STMI patient [5]. Neutrophils play an important role in innate immunity and atherosclerosis, particularly, the inflammatory responses in the pathogenesis of atherosclerosis [6]. In contrast, high-density lipoprotein cholesterol (HDL-c) has been associated with anti-inflammatory, antioxidant and antithrombotic effects [7]. Previous studies indicated that HDL-c was strongly associated with neutrophils in the pathogenesis of atherosclerosis, suggesting that HDL-c may regulate the function of activated neutrophils [8]. Activated neutrophils also affected the composition and function of HDL-c [9]. In a recent study, neutrophils count to high-density lipoprotein ratio (NHR) was identified as a novel factor in predicting poor long-term clinical outcomes in elderly patients with AMI [10]. However, the short-term prognostic ability of NHR has not been studied in ST-segment elevation myocardial infarction (STEMI) patients. Therefore, the present study aimed to investigate the association between NHR levels on admission with in-hospital major adverse cardiac events (MACE) in STEMI patients underwent primary percutaneous coronary intervention (PPCI).
Materials and methods
Study population
We retrospectively reviewed 561 STEMI patients underwent PPCI at the First Affiliated Hospital of Chongqing Medical University between September 2016 and December 2018. Participants enrolled in the study fulfilled the following criteria: (1) visited the hospital within 12 h of onset of acute myocardial ischemic symptoms and (2) ST-segment elevation of greater than or equal to 1 mm in at least 2 consecutive leads. Patients with previous myocardial infraction, a history of coronary revascularization (either coronary artery bypass graft (CABG) or PCI), active infection (including COPD and asthma), clinical evidence of cancer, chemotherapy, receiving steroid therapy for autoimmune disease, hematological proliferative disorders and patients without a laboratory data on complete blood count and cholesterol levels on admission were excluded from this study. Finally, 532 patients were included in the study (Fig. 1).
Baseline data included age, sex, systolic blood pressure (SBP) and diastolic blood pressure (DBP) on admission, smoking, hypertension, diabetes, myocardial injury markers, blood routine test, aminopherase, renal function indexes, blood lipids, high-sensitivity C-reactive protein (hs-CRP), fasting plasma glucose (FPG), HbA1c, Gensini score, NHR, Killip classification, left ventricular ejection fraction (LVEF), MACE and time of outcome events. On admission, all patients received a 12-lead electrocardiogram (ECG), routine blood test and analysis of myocardial injury markers. Other blood samples were drawn on the first day of admission. NHR was calculated as neutrophils count (×109/L) to high-density lipoprotein cholesterol (mmol/L) ratio.
Hypertension was defined as use of antihypertensive drugs or SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg. While diabetes mellitus (DM) was regarded as use of antidiabetic drugs or FPG levels of greater than 7.0 mmol/L. Smoking status was assessed base on tobacco use at the time of admission. MACEs were defined as stent thrombosis, cardiac rupture, cardiac arrest, ventricular aneurysm, malignant arrhythmia and cardiac death. Cardiac rupture was diagnosed when the following criteria were fulfilled: sudden circulatory collapse and a sudden increase in pericardial effusion evident in the echocardiograms [11]. Malignant arrhythmia, including non-sustained or sustained ventricular tachycardia (VT), ventricular fibrillation (VF) and complete atrioventricular block, were recorded using ECG or cardiac monitoring. When patients experienced recurrent MACE, only the first event was considered in the analysis.
Angiotensin-converting enzyme inhibitor (ACEI) or Angiotensin receptor blocker (ARB), β-blocker and statin were administered to all patients unless there were contraindication. Patients took clopidogrel 75 mg daily or ticagrelor 90 mg twice a day and aspirin 100 mg daily after PPCI.
This study was conducted in accordance with the “Declaration of Helsinki” and approved by the institutional ethics committee (approval No. 2018-035). This study was registered on clinicaltrials.gov (approval No. NCT03527940).
Statistical analyses
NHR was analyzed as a continuous variable and a grouped variable. The continuous variables were represented as mean ± standard deviation (SD), or median (interquartile range) based on the normality of their distribution as evaluated using the Kolmogorov–Smirnov test. The categorical variables were expressed as frequencies and percentages. The continuous variable between the two groups was compared using an independent sample t test or Mann–Whitney U test as appropriate. Comparisons between the categorical variables were evaluated using the Chi-Square test. Kendall’s tau-b correlation analysis was used for assessing the correlation between NHR and Killip classification, SBP. The receiver operating characteristic (ROC) curve was constructed to determine the cut-off NHR value for predicting in-hospital MACE. Univariate and multivariate Cox regression analyses were performed to identify the independent predictors of in-hospital MACE. Variables which were included into multivariable Cox regression model were statistically significant in the univariate Cox regression model. NHR was used as a grouped variable in Cox regression models. The effect of NHR on survival during hospitalization were analyzed using the Kaplan–Meier method and compared using log-rank tests. All statistical analyses were performed using SPSS Statistics software version 22.0. A two-tailed P value < 0.05 was considered to be statistically significant for all described analyses.
Results
Baseline characteristic
Of 532 participants, 72 (13.53%) patients experienced MACE, including 8 patients (1.50%) who died during hospital stay. The baseline and clinical characteristics of the patient were shown in Table 1. Patients who were MACE-free were younger than patients who suffered from MACE. Neutrophils count was higher and HDL-c was lower in the MACE group compared with the MACE-free group. NHR in the MACE group was significantly higher than that in MACE-free group (10.93 [6.26–13.97] vs. 8.13 [5.89–11.16]; P = 0.001). The MACE group had a worse heart function compared with the MACE-free group, as shown by a lower LVEF and a higher proportion of patients with Killip class III and IV, as well as significantly lower SBP and DBP in the MACE group.
The age, WBC, neutrophil count, monocyte count, ALT, AST, creatinine, hs-CRP and FPG were higher in the MACE group compared with the MACE-free, but there was no significant difference in the other parameters between the two groups.
Prognostic ability of NHR for in-hospital outcomes
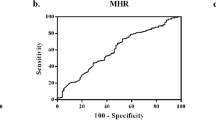
The area under the curve (AUC) of NHR for predicting in-hospital MACE was 0.617 (P = 0.0029, 95% confidence interval [CI]: 0.574–0.658) and the optimal cut-off point was observed at 11.28 with a sensitivity of 47.22% and a specificity of 77.61% (Fig. 2). According to the cut-off value, all patients were grouped into 2 groups based on the cut-off value (the higher group NHR > 11.28, the lower group NHR ≤ 11.28). Baseline characteristics of two groups were showed in Table 2. The incidence of MACE was higher in NHR > 11.28 group compared with NHR ≤ 11.28 group, while HDL-c levels were higher and neutrophils count lower in NHR ≤ 11.28 group. The NHR > 11.28 group had a higher proportion of patients with Killip class III and IV. Patients in NHR > 11.28 group had higher smoking proportion, MYO, CK-MB, WBC, RBC, hemoglobin, platelet count, lymphocyte count, monocyte count, aminotransferase, creatinine, UA, TG, FPG and HbA1c as well as significantly lower age, SBP, TC and LDL-c than the NHR ≤ 11.28 group. There were no significant differences in all the other parameters between the two groups.
The ROC curve of NHR for predicting in-hospital MACE. The cutoff value of was NHR > 11.28 with a sensitivity of 47.22% and a specificity of 77.61%, respectively. AUC, Area under the curve; MACE, major adverse cardiac events; NHR, neutrophils count to high-density lipoprotein cholesterol ratio; ROC, receiver operating characteristic; 95% CI, 95% confidence interval
NHR was significantly associated with Killip class III-IV (r = 0.089, P = 0.012) and SBP (r = -0.078, P = 0.029).
Univariate and multivariate Cox regression analyses
In the univariate Cox regression analyses, age, BP on admission, WBC, neutrophils count, aminotransferase, UA, hs-CRP, FPG, LVEF, Killip III-IV and NHR were associated with a high risk of in-hospital MACE. However, in multivariate regression analyses, only ALT (HR: 1.017, 95% CI: 1.008–1.026, P < 0.001), Killip III-IV (HR: 5.745, 95% CI: 2.795–11.807, P < 0.001) and NHR (HR: 2.211, 95% CI: 1.092–4.479, P = 0.027) were found to be independent predictors of in-hospital MACE after adjustment for other confounding variables (Table 3).
Survival analysis
The Kaplan–Meier curve were plotted base on the event free survival data from the in-hospital follow-up. As showed in Fig. 3, patients in the NHR > 11.28 group had a worse clinical outcome than patients in the NHR ≤ 11.28 group.
Discussion
The main finding of the study were that ALT, presence of Killip class III-IV and NHR value was independently associated with in-hospital MACE in STEMI patients treated with PPCI. In addition, increased NHR was significantly associated with worse Killip classification. To the best of our knowledge, this was the first study focused on the prognostic value of NHR in predicting MACE in STEMI patients.
Inflammation plays a critical role in formation of atherosclerosis. In the presence of serval risk factors, inflammation may lead plaque rupture, which is the main cause of STEMI. Also, inflammation is correlated with adverse event and life threating complications in these patients. Various inflammatory indexes, such as blood platelet count, CRP, neutrophil to lymphocyte ratio, and so on, have been investigated in patients with cardiovascular disease and demonstrated to be short or long term prognostic factors [12,13,14]. In the current study, admission WBC, neutrophil count, monocyte count, hs-CRP level were significantly higher in the MACE group compared with the MACE-free.
Neutrophils, as a component of immune cell, have attracted the attention of researchers in the past decade, emerging studies have suggested that neutrophils play an important role in different stages of atherosclerosis, including atherogenesis, plaque destabilization, plaque erosion, as well as repair processes in myocardial infarction[15,16,17]. When arterial plaque ruptured, neutrophils and platelets aggregated rapidly at the lesion site, where the neutrophils may induce and amplify platelet activation and blood coagulation [18,19,20].Neutrophil extracellular trap, a protein synthesized by neutrophils, has been considered to be a key component of pathological thrombi and drive cardiovascular disease [21, 22]. Neutrophil-derived micro-vesicles represented another mechanism by which neutrophils amplify inflammatory processes [23]. In addition, Clinical studies have shown that the increase in neutrophils was independently correlated with the infarct size, left cardiac function and adverse events in patients with AMI [24, 25].
HDL-c is a well-known antioxidant, anti-inflammatory, antiapoptotic, antithrombotic, anti-atherosclerotic agent that also has reverse-cholesterol transport effects [26]. Reduced HDL-c is common in patients with AMI and is associated with the severe coronary artery disease. Clinical studies showed HDL-c was negatively correlated with the risk of coronary heart disease, and lower levels of HDL-c were an independent predictor of adverse cardiovascular events [27]. In our study, admission HDL-c levels were lower in the MACE group but did not show statistical significance and it did not correlate with in-hospital MACE in multivariate analysis.
Recent studies on HDL-c have focused on its immunomodulatory effects [28]. Neutrophils can be activated in hyperlipidemia. HDL-c has been shown to stimulate the biogenesis of microRNA-223-3p which regulates neutrophil development, hyperactivity and recruitment during infection [29]. Another study indicated that HDL may contribute to the neutrophil activation by decreasing neutrophil membrane lipid rafts [30]. In in vitro and in vivo studies of myocardial ischemia/reperfusion injury, HDL-c administration prior to ischemia or reperfusion had a multidimensional protective effect on cardiac function, and involved the ability of HDL-c to restrict endothelial permeability, as well as promote vasodilation and neovascularization in coronary endothelial cells [31, 32].
As mentioned above, NHR was considered as a valuable biomarker of inflammatory status and may be a predictor for adverse cardiovascular events in myocardial infarction patient. A recent clinical study on elderly patients with AMI by Huang et al. [10] reported that high NHR was a predictor of the long-term clinical outcomes including mortality and recurrence of myocardial infraction, and was superior to pre-existing biomarker called monocyte to High-density Lipoprotein Cholesterol ratio (MHR) and low-density Lipoprotein Cholesterol to High-density Lipoprotein Cholesterol ratio (LDL-C/HDL-C). The present study was conducted to further verify the short-term prognostic value of NHR in STEMI patients. In the study, NHR was higher in patients with in-hospital MACE than those patients who were MACE-free. ROC curve analysis revealed that NHR greater than 11.28 as a cutoff value for in-hospital MACE. A high NHR value was independently associated with increased incidence of in-hospital MACE in STEMI patients treated with PPCI. Patients with NHR greater than 11.28 groups had a 2.211 (95% CI: 1.092–4.479)-fold increased risk of occurrence of in-hospital MACE, compared with NHR less than 11.28.
Interestingly, patients with increased NHR in our study were associated with worse Killip classification and SBP, which indicated that NHR may be a new biomarker of cardiac function. This funding was consistent with a previous report which suggested that excessive infiltration or delayed regression of neutrophils aggravated myocardium injury via the abundant release of inflammatory mediators and proteinases [33].
There were some limitations in this study. First, the retrospective design of the study set a limit to the convincement of our study. The second limitation was this research was based in a single center and the study population size was small, so multicenter and large-scale studies are needed to verify this conclusion.
In conclusion, NHR is an easily calculated and universally available marker that may be useful in in-hospital risk classification of STEMI patients undergoing PPCI. Given the interactions and significant roles played by neutrophils and HDL-c in the pathogenesis of atherosclerosis and myocardial infraction, strategies aimed at reducing the NHR have potential therapeutic effects for STEMI patients undergoing PPCI.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMI:
-
Acute myocardial infarction
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blocker
- AUC:
-
Area under the curve
- CABG:
-
Coronary artery bypass graft
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- ECG:
-
Electrocardiogram
- FPG:
-
Fasting plasma glucose
- hs-CRP:
-
High-sensitivity C-reactive protein
- HDL-c:
-
High-density lipoprotein cholesterol
- LDL-C/HDL-C:
-
Low-density lipoprotein cholesterol to high-density lipoprotein cholesterol ratio
- LVEF:
-
Left ventricular ejection fraction
- MACE:
-
Major adverse cardiac events
- MHR:
-
Monocyte to high-density lipoprotein cholesterol ratio
- NHR:
-
Neutrophils count to high-density lipoprotein cholesterol ratio
- PPCI:
-
Primary percutaneous coronary intervention
- ROC:
-
Receiver operating characteristic
- SD:
-
Standard deviation
- STEMI:
-
ST-segment elevation myocardial infarction
- SBP:
-
Systolic blood pressure
- VT:
-
Ventricular tachycardia
- VF:
-
Ventricular fibrillation
References
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–95.
Forrester JS. Prevention of plaque rupture: a new paradigm of therapy. Ann Intern Med. 2002;137(10):823–33.
Bartels ED, Christoffersen C, Lindholm MW, Nielsen LB. Altered metabolism of LDL in the arterial wall precedes atherosclerosis regression. Circ Res. 2015;117(11):933–42.
Ganjali S, Gotto AM Jr, Ruscica M, Atkin SL, Butler AE, Banach M, Sahebkar A. Monocyte-to-HDL-cholesterol ratio as a prognostic marker in cardiovascular diseases. J Cell Physiol. 2018;233(12):9237–46.
Rencuzogullari I, Karabag Y, Cagdas M, Karakoyun S, Seyis S, Gursoy MO, Yesin M, Artac I, Ilis D, Tanboga IH. Assessment of the relationship between preprocedural C-reactive protein/albumin ratio and stent restenosis in patients with ST-segment elevation myocardial infarction. Rev Port Cardiol (Engl Ed). 2019;38(4):269–77.
Murphy AJ, Woollard KJ, Suhartoyo A, Stirzaker RA, Shaw J, Sviridov D, Chin-Dusting JP. Neutrophil activation is attenuated by high-density lipoprotein and apolipoprotein A-I in in vitro and in vivo models of inflammation. Arterioscler Thromb Vasc Biol. 2011;31(6):1333–41.
Karabacak M, Kahraman F, Sert M, Celik E, Adali MK, Varol E. Increased plasma monocyte chemoattractant protein-1 levels in patients with isolated low high-density lipoprotein cholesterol. Scand J Clin Lab Invest. 2015;75(4):327–32.
Curcic S, Holzer M, Frei R, Pasterk L, Schicho R, Heinemann A, Marsche G. Neutrophil effector responses are suppressed by secretory phospholipase A2 modified HDL. Biochim Biophys Acta. 2015;1851(2):184–93.
Cogny A, Atger V, Paul JL, Soni T, Moatti N. High-density lipoprotein 3 physicochemical modifications induced by interaction with human polymorphonuclear leucocytes affect their ability to remove cholesterol from cells. Biochem J. 1996;314(Pt 1):285–92.
Huang JB, Chen YS, Ji HY, Xie WM, Jiang J, Ran LS, Zhang CT, Quan XQ. Neutrophil to high-density lipoprotein ratio has a superior prognostic value in elderly patients with acute myocardial infarction: a comparison study. Lipids Health Dis. 2020;19(1):59.
Nakatsuchi Y, Minamino T, Fujii K, Negoro S. Clinicopathological characterization of cardiac free wall rupture in patients with acute myocardial infarction: difference between early and late phase rupture. Int J Cardiol. 1994;47(1 Suppl):S33-38.
Nikolsky E, Grines CL, Cox DA, Garcia E, Tcheng JE, Sadeghi M, Mehran R, Lansky AJ, Na Y, Stone GW. Impact of baseline platelet count in patients undergoing primary percutaneous coronary intervention in acute myocardial infarction (from the CADILLAC trial). Am J Cardiol. 2007;99(8):1055–61.
Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102(6):653–7.
Makrygiannis SS, Ampartzidou OS, Zairis MN, Patsourakos NG, Pitsavos C, Tousoulis D, Prekates AA, Foussas SG, Cokkinos DV. Prognostic usefulness of serial C-reactive protein measurements in ST-elevation acute myocardial infarction. Am J Cardiol. 2013;111(1):26–30.
Silvestre-Roig C, Braster Q, Ortega-Gomez A, Soehnlein O. Neutrophils as regulators of cardiovascular inflammation. Nat Rev Cardiol. 2020;17(6):327–40.
Drechsler M, Megens RT, van Zandvoort M, Weber C, Soehnlein O. Hyperlipidemia-triggered neutrophilia promotes early atherosclerosis. Circulation. 2010;122(18):1837–45.
Ionita MG, van den Borne P, Catanzariti LM, Moll FL, de Vries JP, Pasterkamp G, Vink A, de Kleijn DP. High neutrophil numbers in human carotid atherosclerotic plaques are associated with characteristics of rupture-prone lesions. Arterioscler Thromb Vasc Biol. 2010;30(9):1842–8.
Swystun LL, Liaw PC. The role of leukocytes in thrombosis. Blood. 2016;128(6):753–62.
Pircher J, Czermak T, Ehrlich A, Eberle C, Gaitzsch E, Margraf A, Grommes J, Saha P, Titova A, Ishikawa-Ankerhold H, et al. Cathelicidins prime platelets to mediate arterial thrombosis and tissue inflammation. Nat Commun. 2018;9(1):1523.
Rotzius P, Thams S, Soehnlein O, Kenne E, Tseng CN, Bjorkstrom NK, Malmberg KJ, Lindbom L, Eriksson EE. Distinct infiltration of neutrophils in lesion shoulders in ApoE-/- mice. Am J Pathol. 2010;177(1):493–500.
Doring Y, Soehnlein O, Weber C. Neutrophil extracellular traps in atherosclerosis and atherothrombosis. Circ Res. 2017;120(4):736–43.
Fousert E, Toes R, Desai J. Neutrophil extracellular traps (NETs) take the central stage in driving autoimmune responses. Cells. 2020;9(4):915.
Bonaventura A, Montecucco F, Dallegri F, Carbone F, Luscher TF, Camici GG, Liberale L. Novel findings in neutrophil biology and their impact on cardiovascular disease. Cardiovasc Res. 2019;115(8):1266–85.
Tamura A, Watanabe T, Nasu M. Association between neutrophil counts on admission and left ventricular function in patients successfully treated with primary coronary angioplasty for first anterior wall acute myocardial infarction. Am J Cardiol. 2001;88(6):678–80.
Husser O, Bodi V, Sanchis J, Nunez J, Mainar L, Chorro FJ, Lopez-Lereu MP, Monmeneu JV, Chaustre F, Forteza MJ, et al. White blood cell subtypes after STEMI: temporal evolution, association with cardiovascular magnetic resonance–derived infarct size and impact on outcome. Inflammation. 2011;34(2):73–84.
Ganjali S, Momtazi AA, Banach M, Kovanen PT, Stein EA, Sahebkar A. HDL abnormalities in familial hypercholesterolemia: focus on biological functions. Prog Lipid Res. 2017;67:16–26.
Acharjee S, Roe MT, Amsterdam EA, Holmes DN, Boden WE. Relation of admission high-density lipoprotein cholesterol level and in-hospital mortality in patients with acute non-ST segment elevation myocardial infarction (from the National Cardiovascular Data Registry). Am J Cardiol. 2013;112(8):1057–62.
Trakaki A, Marsche G. Current understanding of the immunomodulatory activities of high-density lipoproteins. Biomedicines. 2021;9(6):587.
Cuesta Torres LF, Zhu W, Ohrling G, Larsson R, Patel M, Wiese CB, Rye KA, Vickers KC, Tabet F. High-density lipoproteins induce miR-223-3p biogenesis and export from myeloid cells: Role of scavenger receptor BI-mediated lipid transfer. Atherosclerosis. 2019;286:20–9.
Murphy AJ, Westerterp M, Yvan-Charvet L, Tall AR. Anti-atherogenic mechanisms of high density lipoprotein: effects on myeloid cells. Biochim Biophys Acta. 2012;1821(3):513–21.
Gomaraschi M, Calabresi L, Franceschini G. Protective effects of HDL against ischemia/reperfusion injury. Front Pharmacol. 2016;7:2.
Murphy AJ, Woollard KJ, Hoang A, Mukhamedova N, Stirzaker RA, McCormick SP, Remaley AT, Sviridov D, Chin-Dusting J. High-density lipoprotein reduces the human monocyte inflammatory response. Arterioscler Thromb Vasc Biol. 2008;28(11):2071–7.
Ma Y, Yabluchanskiy A, Lindsey ML. Neutrophil roles in left ventricular remodeling following myocardial infarction. Fibrogenesis Tissue Repair. 2013;6(1):11.
Acknowledgements
Not applicable.
Funding
This research was funded by Chongqing Science and Technology Commission, key Project (2019 ZLXM003); Chongqing Science and Technology Commission, Youth Project (2018QNXM024).
Author information
Authors and Affiliations
Contributions
Material preparation, data collection and analysis were performed by DJ, YC, HT, PG and QD. The manuscript was written by YC and DJ. QD designed the study and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the "Declaration of Helsinki" and approved by the ethics committee of the first affiliated hospital of Chongqing Medical University (approval No. 2018-035).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y., Jiang, D., Tao, H. et al. Neutrophils to high-density lipoprotein cholesterol ratio as a new prognostic marker in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a retrospective study. BMC Cardiovasc Disord 22, 434 (2022). https://doi.org/10.1186/s12872-022-02870-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02870-9