Abstract
Background
Hypoxemia after cardiopulmonary bypass (CPB) is the quantifiable manifestation of pulmonary dysfunction. This retrospective study was designed to investigate the risk factors for post-cardiopulmonary bypass hypoxaemia and the features of hypoxaemia and pulmonary complications in paediatric congenital heart disease surgery involving CPB.
Methods
Data including demographics, preoperative pulmonary or cardiac parameters, and intraoperative interventions were retrospectively collected from 318 paediatric patients who underwent radical surgery with CPB for congenital heart disease. Among them, the factors that were significant by univariate analysis were screened for multivariate Cox regression. The lowest ratio of arterial oxygen tension and the inspiratory oxygen fraction (PaO2/FiO2), hypoxaemia (PaO2/FiO2 ≤ 300) insult time, duration of hypoxaemia, extubation time, and pulmonary complications were also analysed postoperatively.
Results
The morbidity of post-cardiopulmonary bypass hypoxaemia was 48.4% (154/318). Months (6 < months ≤ 12, 12 < months ≤ 36 and 36 < months compared with 0 ≤ months ≤ 6: HR 0.582, 95% CI 0.388–0.873; HR 0.398, 95% CI 0.251–0.632; HR 0.336, 95% CI 0.197–0.574, respectively; p < 0.01), preoperative intracardiac right-to-left shunting (HR 1.729, 95% CI 1.200–2.493, p = 0.003) and intraoperative pleural cavity entry (HR 1.582, 95% CI 1.128–2.219, p = 0.008) were identified as independent risk factors for the development of post-cardiopulmonary bypass hypoxaemia. Most hypoxaemia cases (83.8%, 129/154) occurred within 2 h, and the rate of moderate hypoxaemia (100 < PaO2/FiO2 ≤ 200) was 60.4% (93/154).
Conclusion
The morbidity of post-cardiopulmonary bypass hypoxaemia in paediatric congenital heart disease surgery was considerably high. Most hypoxaemia cases were moderate and occurred in the early period after CPB. Scrupulous management should be employed for younger infants or children with preoperative intracardiac right-to-left shunting or intraoperative pleural cavity entry.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Postoperative pulmonary dysfunction is a well-known cause of mobility and mortality after cardiac surgery with cardiopulmonary bypass (CPB) [1,2,3]. Although technologies involving CPB have improved, the incidence of various lung dysfunctions in patients undergoing cardiac surgery with CPB is still approximately 20–25% [4, 5].
Hypoxemia after CPB may result from primary pulmonary dysfunction, secondary cardiac dysfunction, or both. Hypoxemia is the quantifiable manifestation of pulmonary dysfunction that can be detected easily. The degree of hypoxaemia, which is defined as the ratio of arterial oxygen tension to the inspiratory oxygen fraction (PaO2/FiO2) with different PEEP levels, combined with the clinical insult time, chest imaging, and origin of oedema are the quaternion of acute respiratory distress syndrome (ARDS) [6]. In the definition of paediatric ARDS (PARDS) [7], PaO2/FiO2 ≤ 300 is one of the initial cut-off points of the abnormality in oxygenation. Although there is no consensual definition of hypoxaemia, the European Society of Anaesthesiology (ESA) and the European Society of Intensive Care Medicine (ESICM) [8] have unanimously defined hypoxaemia as a PaO2/FiO2 ≤ 300 mmHg and have recommended the preoperative and periprocedural use of noninvasive respiratory support techniques for these patients.
In studies using adult patients [9, 10] undergoing cardiac surgery, numerous perioperative risk factors for hypoxaemia have been reported. Compared to adults undergoing CPB, paediatric patients with congenital heart disease (CHD) differ greatly in the disease category, basal haemodynamics, postoperative pathophysiology changes, techniques and materials of CPB. Pulmonary complications of CHD occur due to structural compression, which causes paediatric airway malacia or atelectasis of the lung preoperatively, structural trauma to the respiratory system, damage to the alveolar-capillary membrane, and pulmonary oedema contributed by CPB [11]. All of these factors may lead to poorly compliant lungs that can deteriorate and cause hypoxaemia. Therefore, we hypothesized that several factors in paediatric surgery with CPB were involved specially in development of post-cardiopulmonary bypass hypoxaemia in this retrospective study. The aim of this study was to investigate the hypothesis, and to explore the features of the hypoxaemia, pulmonary complications after the surgery.
Methods
Patients
Between January 2015 and March 2016, there were 390 consecutive paediatric patients (≤ 12 years) scheduled for cardiac surgery with congenital heart disease. Based on the electronic medical system, we retrospectively screened the clinical, laboratory, and imageological data. Finally, 318 patients who underwent radical surgery therapy through median sternotomy with CPB were recruited into this study. The exclusion criteria were as follows: (1) surgery without CPB (ligation of patent ductus arteriosus, repair of coarctation of the aorta), (2) palliative surgery (pulmonary artery banding, systemic-to-pulmonary shunting), (3) hypoplastic left heart syndrome (HLHS) and single ventricle, (4) preoperative respiratory dysfunction (supported by mechanical ventilator), (5) residual intracardiac shunting from the right to the left (R to L) diagnosed by transoesophageal ultrasonic examination (TEE) intraoperatively or by echocardiography examination postoperatively, (6) postoperative left heart insufficiency (EF < 50%) as confirmed by echocardiography, and (7) any relevant clinical, laboratory or iconography data missing.
This observational study was approved by the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine (approval No. XHEC-D-2017–006). Data were observed and recorded by health care personnel, including the nurses and medical doctors taking care of the patients. The study protocol was performed in accordance with the relevant guidelines, and informed consent was waived.
Treatment regimen
All intraoperative and postoperative processes followed the routine protocol of our institution. Anaesthesia of all patients was induced by intravenous administration of midazolam, fentanyl, propofol, and rocuronium and maintained using midazolam, fentanyl, propofol, rocuronium, and sevoflurane. Mechanical ventilation was performed by a Grager Primus ventilator (Grager, Lubeck, Germany). The ventilator parameters were oxygen concentration of 40–60% (air-oxygen mixed), volume-controlled ventilation (VCV) mode: tidal volume of 10 ml kg−1 or pressure-controlled ventilation (PCV) mode: pressure limit of 12–15 cmH2O, ventilation frequency of 16–28 to maintain the PETCO2 level at 4.5–5.5 kPa, and I/E ratio of 1/2. In addition to routine monitors, invasive artery pressure monitoring and blood-gas samples were obtained via an arterial line in the radial or femoral artery.
CPB was carried out with a Maquel Jostra Cardiopulmonary HL20 (Maquel, Germany). Management of CPB included systemic temperature drift to 33–35 °C, pump flow rates of 150–200 ml kg−1 min−1, mean perfusion pressure between 30 and 60 mmHg, haematocrit between 20 and 30%, a crystal-colloid proportion of the priming solution that was 0.5:1, albumin and plasma priming to maintain the colloid osmotic pressure at 17–19 mmHg, and conventional combined modified ultrafiltration.
Mechanical ventilation was terminated during CPB. Before weaning from CPB and sternal closure, the lungs were re-expanded by the following conventional alveolar recruitment manoeuvre: peak airway pressure of 20–30 cmH2O for three to five consecutive mechanical breaths. Mediastinal drainage connected to continuous negative pressure suction was performed.
The surgical effect and cardiovascular function were routinely evaluated by an iE33 ultrasound device (Philips, Bothell WA, USA) connected to a TEE probe (S7-3t) before weaning from CPB and the transthoracic probe (S5-1) within 24 h postoperatively in the ICU.
The arterial blood-gas analyses were repeated after anaesthetic induction, after weaning from CPB, before transport out of the OR, every 2 h before extubation, and every 4 h after extubation until discharge from the ICU. All patients were routinely examined by thoracic X-ray after admission to the ICU within 8 h after the operation. Thoracic X-ray was repeated, and scanning by computed tomography (CT) was performed whenever necessary.
In the ICU, ventilator setting adjustments were guided by blood-gas analyses and imaging examinations. The timing of extubation and discharge from the ICU was decided according to the haemodynamic, respiratory, and neurological status and other related clinical parameters.
Clinical data collection and examination method
According to the results of adult’s studies [9, 10] and the particularity of paediatric patients with CHD undergoing CPB [11], we hypothesized that several perioperative factors might affect respiratory function after CPB. They were retrospectively collected from the electronic medical record system. These factors included age (months), sex, weight, recent upper respiratory tract infection history (yes/no, Y/N; URI, defined as within seven days preoperatively), history of cardiac operation (Y/N), preoperative intracardiac R-to-L shunt (Y/N), preoperative pulmonary hypertension (Y/N), preoperative left ventricular ejection fraction, Aristotle basic complexity score (ABC) category [12], duration of CPB, duration of aortic cross-clamping, ventilation mode during the operation (PCV/VCV), the total blood products used intraoperatively and postoperatively transfused (including CPB priming), and pleural cavity entry during the operation (Y/N).
The PaO2/FiO2 value by arterial blood-gas analyses at each time point from termination of CPB to discharge from the ICU was used to measure hypoxaemia. The time points were after weaning from CPB and the completion of ultrafiltration, before transport out of the OR, every 2 h before extubation, and every 4 h after extubation in the ICU. The lowest PaO2/FiO2 ≤ 300 was defined as hypoxaemia [8]; 200 < PaO2/FiO2 ≤ 300 was defined as mild hypoxaemia, 100 < PaO2/FiO2 ≤ 200 was defined as moderate hypoxaemia, and PaO2/FiO2 ≤ 100 was defined as severe hypoxaemia [13]. The features of hypoxaemia, including the hypoxaemia degree, hypoxaemia insult time [defined as the earliest time point (hours after the weaning from CPB and completion of ultrafiltration) of hypoxaemia occurrence] and duration of hypoxaemia, were collected. The endpoint of follow-up to hypoxaemia was the discharge time from the ICU. Survival to hypoxaemia referred to the interval from the endpoint of CPB and ultrafiltration to the hypoxaemia insult time or the last follow-up.
Furthermore, the postoperative pulmonary outcomes of all patients were also screened as follows: extubation time (hours after operation), radiographic evidence and pulmonary complications. Pulmonary complications were diagnosed by clinical symptoms and/or radiographic evidence (X-ray or CT) according to the criteria for congenital heart disease: [11, 14] including chylothorax, pleural effusion, pneumonia, pneumothorax, atelectasis, postoperative respiratory insufficiency requiring mechanical ventilatory support > 7 days, postoperative respiratory insufficiency requiring reintubation, and postoperative respiratory failure requiring tracheostomy.
Statistical analysis
All analyses were performed using IBM SPSS Statistics (version 21.0, IBM, Almonk, NK). Continuous variables were screened by the Kolmogorov–Smirnov one-sample test. The results are expressed as the median [interquartile range (IQR)] for nonnormally distributed data and as the mean ± SD for normally distributed data. The frequency variables are expressed as numbers (%). The Mann‒Whitney U test was used for the comparison of continuous variables, while Pearson’s chi-square or Fisher’s exact test was used for univariate analysis. Factors that were significantly different (p < 0.1) in the post-cardiopulmonary bypass hypoxaemia incidence shown by univariate analysis were used for multivariate Cox regression analysis (backwards) [hazard ratio (HR) and 95% confidence interval (CI)] to determine the independent factors associated with post-cardiopulmonary bypass hypoxaemia. Spearman analysis was used for the bivariate correlations. All statistical hypothesis tests were two-sided and performed at the 0.05 significance level. p < 0.05 was considered statistically significant.
Results
Study population
A total of 318 paediatric patients were retrospectively enrolled in this study. Figure 1 shows the flow chart of inclusion and exclusion. The demographic and perioperative data are reported in Table 1.
Risk factors for post-cardiopulmonary bypass hypoxaemia
The overall incidence of post-cardiopulmonary bypass hypoxaemia was 48.4% (154/318). Potential risk factors for post-cardiopulmonary bypass hypoxaemia identified by univariate analysis are shown in Table 2. The difference in hypoxaemia incidence for the factors including age (months), weight, recent URI, pulmonary hypertension, preoperative intracardiac R-to-L shunt, transfusion volume, intraoperative ventilation mode (PCV), and pleural cavity entry were statistically significant (p < 0.1). Next, the abovementioned related univariate factors (except weight, because of the linear interactive effect between weight and month rank in terms of paediatric physical growth) were analysed for multivariate Cox regression statistics. The results are shown in Table 3.
The months (6 < months ≤ 12, 12 < months ≤ 36 and 36 < months compared with 0 ≤ months ≤ 6: HR 0.582, 95% CI 0.388–0.873; HR 0.398, 95% CI 0.251–0.632; HR 0.336, 95% CI 0.197–0.574, respectively; p < 0.01), preoperative intracardiac R-to-L shunting (HR 1.729, 95% CI 1.200–2.493, p = 0.003) and intraoperative pleural cavity entry (HR 1.582, 95% CI 1.128–2.219, p = 0.008) were identified as independent risk factors for the development of post-cardiopulmonary bypass hypoxaemia.
Features of hypoxaemia
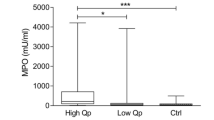
Among all 154 paediatric patients with post-cardiopulmonary bypass hypoxaemia, the hypoxaemia insult time (after CPB) was 0 (0–0) hours. The hypoxaemia duration was 38.0 (2.0–82.5) hours, and the lowest P/F value was 148.7 ± 54.3. There were 28 (18.2%) mild hypoxaemia cases, 93 (60.4%) moderate hypoxaemia cases, and 33 (21.4%) severe hypoxaemia cases. Most hypoxaemia cases (83.8%, 129/154) occurred within 2 h, while 11 (7.1%) cases occurred between 2–6 h, and 14 (9.1%) cases occurred after 6 h. The number and degree of hypoxaemia cases in different periods are shown in Fig. 2.
Postoperative pulmonary outcomes
The extubation times (hours after operation) of hypoxaemia patients and nonhypoxaemia patients were 48.0 (20.5–104.0) and 6 (4.0–16.8), respectively. In hypoxaemia cases, the duration of hypoxaemia (p < 0.001, r = 0.831) and the degree of hypoxaemia (p = 0.001, r = 0.255) were positively correlated with the extubation time. Pulmonary complications postoperatively screened in the population of our study included pneumonia, atelectasis, pleural effusion, pneumothorax, postoperative respiratory insufficiency requiring mechanical ventilatory support > 7 days, and postoperative respiratory insufficiency requiring reintubation. Atelectasis (13.0% vs. 3.0%, p = 0.001), pleural effusion (13.0% vs. 6.1%, p = 0.036) and postoperative respiratory insufficiency requiring mechanical ventilatory support > 7 days (9.7% vs. 0%, p < 0.001) occurred more often in children with hypoxaemia than in those without hypoxaemia (Table 4). Eighty-eight (57.1%) hypoxaemic children had negative radiographic results, and 34 (20.7%) nonhypoxaemic children had positive radiography for pulmonary complications.
Discussion
The pathophysiology of postoperative pulmonary dysfunction in CPB surgery is multifactorial and complicated [3], involving the specificity of cardiac surgery, alterations of lung mechanics in CPB, and anomalies in gas exchange. Reduced respiratory function may lead directly to a decreased PaO2/FiO2 ratio,or to pulmonary failure requiring prolonged mechanical ventilatory support and even to ARDS. In studies involving adult patients [10, 15, 16], the incidence of hypoxaemia (PaO2/FiO2 ≤ 200 as the marker) after CPB cardiac surgery has been reported to range from 30.6% to 54.2%. In a recent study [17], the morbidity of PaO2/FiO2 < 300 measured 2 h after CPB cessation was reported to be as high as 39.1%. Herein, we used PaO2/FiO2 ≤ 300 as the marker of hypoxaemia. Our analysis revealed that the overall incidence of post-cardiopulmonary bypass hypoxaemia in paediatric cardiac surgery was 48.4% (154/318).
Several preoperative, intraoperative, and postoperative factors have been identified as significant risk factors for hypoxaemia in adult CPB [9, 10]. In children, the respiratory centre is immature, and the stimuli of the CPB, surgical performance, and anaesthesia procedure decrease pulmonary surfactant. Abnormalities in gas exchange and increased respiratory resistance are common, including the increased alveolar-arterial oxygen partial pressure difference, elevated pulmonary vascular resistance, increased intrapulmonary shunt, and decreased compliance, especially in neonates and younger infants. Stayer et al. [18] reported that age was the only significant factor that affected both dynamic respiratory compliance and total respiratory resistance and was a stronger predictor of these changes in respiratory mechanics. The major cases in our study were infants (45.6%) and children of young age (12 < months ≤ 36: 27.4%). Our univariate analysis revealed that both age (months) and weight were significantly related to post-cardiopulmonary bypass hypoxaemia (p < 0.001). In the results of multivariate analysis, low age (months) was a risk factor for hypoxaemia, which was significantly decreased in older infants and children (6 < months ≤ 12, HR 0.582; 12 < months ≤ 36, HR 0.398; 36 < months, HR 0.336) compared with younger infants (0 ≤ months ≤ 6). Scrupulous perioperative management may be needed for younger children, especially younger infants (0 ≤ months ≤ 6), in order to alleviate deoxygenation.
Preexisting intracardiac R-to-L shunting was related to post-cardiopulmonary bypass hypoxaemia and was a significant predictor identified by univariate (p < 0.001) and multivariate (p < 0.001) analyses. Children with congenital heart disease with intracardiac right-to-left shunts were preoperatively found to have hypoxaemia to varying degrees. Although these children tolerated physiological hypoxaemia, they had numerous pathological changes, such as erythrocytosis, hypervolemia, pulmonary vasodilation, small-pulmonary-vessel and collateral-circulation hyperplasia, and alveolar hyperventilation combined with chronic respiratory alkalosis. Children who had chronic hypoxaemia over a long period had limited cardiac reserve and oxygen evolution capacity. These children might have had a higher blood dilution after CPB than the children who were neither anoxic nor had a right-to-left shunt. In addition, the proinflammatory cytokine interleukin [interleukin 6 (IL-6)] levels after CPB were inversely correlated with PaO2/FiO2 values 24 h postoperatively in infants. IL-6 was higher in the infants with hypoxaemia due to intracardiac right-to-left shunting in contrast to those with intracardiac left-to-right shunts preoperatively, during CPB and after CPB, whereas the natural anti-inflammatory cytokine IL-10 was lower preoperatively and during CPB [19]. Considering the disease categories in our study, there might be intracardiac R-to-L shunting in tetralogy of Fallot, anomalous pulmonary venous drainage, endocardial cushion defects, a double outlet of the right ventricle, pulmonary valve stenosis, Ebstein anomaly and even an atrial or ventricular septal defect with pulmonary vascular resistance close to the systemic vascular resistance. Children who are younger and are in more serious condition with the above diseases need urgent operative correction.
Median sternotomy and manipulation of the heart and great vessels may result in pleural cavity entry unilaterally or bilaterally. The disappearance of intrathoracic negative pressure may lead to alveolar collapse that radically reduces the aeration area. The fluid and blood filling the pleural cavity compress the pulmonary tissue and induce atelectasis. Although pleural cavity entry is almost always identified by surgeons in the later period of weaning from CPB, therapies including suction of the ruptured cavity, mediastinal drainage, and alveolar recruitment are performed conventionally. Small pneumothorax, atelectasis, or haemothorax may exist until the later postoperative period. Our study showed that intraoperative pleural cavity entry was a significant independent risk factor for hypoxaemia.
Our results showed that hypoxaemia in paediatric cardiac surgery occurred very early [0(0–0) hours] after CPB; in most cases (83.8%), it occurred within 2 h. This phenomenon was similar to that observed in adult patients [17], e.g., PaO2/FiO2 decreased significantly 2 h after CPB. Several factors may have contributed to the timing characteristics, as follows: the atelectasis produced in CPB explained most of the markedly increasing intrapulmonary shunting and hypoxaemia in the early post-CPB period (45 min after separation from CPB) [20]; the extravascular lung water increased by 52% after separation from CPB and decreased to the presurgical values 4 h postoperatively [21]; and the lung and chest wall mechanics were mainly affected from 20–30 min to 4 h after separation from CPB [22].
Hypoxemia is the most easily detected clinical manifestation of postoperative pulmonary dysfunction, as well as the result of pulmonary complications. Studies in adult patients showed that postoperative pulmonary dysfunctions after cardiac surgery included pleural effusion (27–95%), atelectasis (16.6–88%), pneumonia (0.9–4.4%), ARDS (0.5–1.7%), and postoperative hypoxaemia without any clinical symptoms (3–10%) [23]. In paediatric studies, there was a fairly high incidence of pulmonary complications after cardiac surgery, such as nosocomial pneumonia (9.6%-21.5%) [24, 25], chylothorax (3.8%) [26], and diaphragmatic paralysis due to phrenic nerve injury (5.4–17.6%) [27]. Our study explored the relationship between postoperative pulmonary complications and hypoxaemia. Among them, atelectasis, pleural effusion, and postoperative respiratory insufficiency requiring mechanical ventilatory support > 7 days were significantly related to hypoxaemia. More than half of the children with hypoxaemia (57.1%) were not diagnosed with abnormalities based on conventional radiographic evidence (bedside X-ray or CT). Meanwhile, 20.7% of nonhypoxaemic children had positive radiographic findings. In addition, bedside chest X-ray was reported to have a diagnostic accuracy of 47% for pleural effusion, 75% for alveolar consolidation, and 72% for the alveolar–interstitial syndrome, with chest CT being the diagnostic gold standard [28]. Even the ‘golden standard’ CT scanning was used and occasionally repeated as the routine examination, considering the expense and the difficulties in patients with mechanical ventilation.
Our results indicated that the majority of hypoxaemia cases were not positive by conventional radiographic examination; therefore, more effective diagnostic imaging tests for hypoxaemia and more vigorous therapy for improving oxygenation should be considered intraoperatively and in the early postoperative period. One such test is the highly sensitive, specific, and reproducible bedside pulmonary ultrasonogram [28], which can detect the early stage of extravascular water accumulation in the presence of a normal PaO2/FiO2 ratio [29]. Ventilatory support, including the alveolar recruitment manoeuvre, individualized optimal positive end-expiratory pressure (PEEP) as part of a lung-protective strategy, and other “nonconventional” mechanical ventilation [30, 31], may also be promising and reliable for these high-risk children.
The present study has the following limitations: (1) PaO2/FiO2 was used to qualitatively and quantitatively analyse post-cardiopulmonary bypass hypoxaemia. To exclude the interference of intracardiac shunting and abnormal pulmonary blood flow with the P/F value, we only enrolled patients whose anatomical abnormalities could be completely corrected. Thus, this population did not entirely cover children with surgical congenital heart disease. (2) The specific patients in our study had relatively small differences in surgical procedures, CPB techniques, and therapeutic algorithms employed in the ICU. There were not as many perioperative variables included for the risk analyses as in studies using adult patients. (3) This retrospective study was conducted at a single centre. The sample size was determined by the number of potential risk factors and was relatively small, thus limiting the power of the present study.
Conclusion
The incidence of post-cardiopulmonary bypass hypoxaemia in paediatric congenital heart disease surgery is considerably high. Younger age, preoperative intracardiac R-to-L shunting, and intraoperative pleural cavity entry were identified as independent risk factors for hypoxaemia. Most hypoxaemia cases were moderate and occurred within 2 h. The postoperative pulmonary complications diagnosed by conventional radiographic evidence did not sensitively or specifically translate to hypoxaemia. Additional manoeuvres to optimize the paediatric patient's oxygenation may be performed perioperatively in high-risk populations to decrease the duration of mechanical ventilation and reduce pulmonary complications, morbidity and hospital costs.
Availability of data and materials
The datasets used and analyzed during the study are available from the corresponding authors on reasonable request.
References
Baer DM, Osborn JJ. The postperfusion pulmonary congestion syndrome. Am J Clin Pathol. 1960;34:442–5.
Shenkman Z, Shir Y, Weiss YG, Bleiberg B, Gross D. The effects of cardiac surgery on early and late pulmonary functions. Acta Anaesthesiol Scand. 1997;41:1193–9.
Badenes R, Lozano A, Belda FJ. Postoperative pulmonary dysfunction and mechanical ventilation in cardiac surgery. Crit Care Res Pract. 2015;2015: 420513.
Apostolakis E, Filos KS, Koletsis E, Dougenis D. Lung dysfunction following cardiopulmonary bypass. J Card Surg. 2010;25:47–55.
Stephens RS, Shah AS, Whitman GJ. Lung injury and acute respiratory distress syndrome after cardiac surgery. Ann Thorac Surg. 2013;95:1122–9.
ARDS Definition Task Force. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA J Am Med Assoc. 2012;307:2526–33.
Khemani RG, Smith LS, Zimmerman JJ, Erickson S. Pediatric acute respiratory distress syndrome: definition, incidence, and epidemiology: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015;16:S23-40.
Leone M, Einav S, Chiumello D, Constantin JM, De Robertis E, Abreu MG, Gregoretti C, Jaber S, Maggiore SM, Pelosi P, Sorbello M, Afshari A. Noninvasive respiratory support in the hypoxaemic peri-operative/periprocedural patient: a joint ESA/ESICM guideline. Eur J Anaesthesiol. 2020;37:265–79.
Weiss YG, Merin G, Koganov E, Ribo A, Oppenheim-Eden A, Medalion B, Peruanski M, Reider E, Bar-Ziv J, Hanson WC, Pizov R. Postcardiopulmonary bypass hypoxemia: a prospective study on incidence, risk factors, and clinical significance. J Cardiothorac Vasc Anesth. 2000;14:506–13.
Ranucci M, Ballotta A, La Rovere MT, Castelvecchio S. Postoperative hypoxia and length of intensive care unit stay after cardiac surgery: the underweight paradox? PLoS ONE. 2014;9:e93992.
Healy F, Hanna BD, Zinman R. Pulmonary complications of congenital heart disease. Paediatr Respir Rev. 2012;13:10–5.
Lacour-Gayet F, Clarke D, Jacobs J, Comas J, Daebritz S, Daenen W, Gaynor W, Hamilton L, Jacobs M, Maruszsewski B, Pozzi M, Spray T, Stellin G, Tchervenkov C, Mavroudis C. The Aristotle score: a complexity-adjusted method to evaluate surgical results. Eur J Cardiothorac Surg. 2004;25:911–24.
Coudroy R, Frat JP, Boissier F, Contou D, Robert R, Thille AW. Early identification of acute respiratory distress syndrome in the absence of positive pressure ventilation: implications for revision of the berlin criteria for acute respiratory distress syndrome. Crit Care Med. 2018;46:540–6.
Jacobs JP. Introduction–databases and the assessment of complications associated with the treatment of patients with congenital cardiac disease. Cardiol Young. 2008;18(Suppl 2):1–37.
Shi S, Gao Y, Wang L, Liu J, Yuan Z, Yu M. Elevated free fatty acid level is a risk factor for early postoperative hypoxemia after on-pump coronary artery bypass grafting: association with endothelial activation. J Cardiothorac Surg. 2015;10:122.
Szeles TF, Yoshinaga EM, Alenca W, Brudniewski M, Ferreira FS, Auler JO, Carmona MJ, Malbouisson LM. Hypoxemia after myocardial revascularization: analysis of risk factors. Rev Bras Anestesiol. 2008;58:124–36.
Murata T, Maeda M, Amitani R, Hiromoto A, Shirakawa M, Kambe M, Maruyama Y, Imura H. Postoperative changes in pulmonary function after valve surgery: oxygenation index early after cardiopulmonary is a predictor of postoperative course. J Clin Med. 2021;10:3262.
Stayer SA, Diaz LK, East DL, Gouvion JN, Vencill TL, McKenzie ED, Fraser CD, Andropoulos DB. Changes in respiratory mechanics among infants undergoing heart surgery. Anesth Analg. 2004;98:49–55.
Hövels-Gürich HH, Schumacher K, Vazquez-Jimenez JF, Qing M, Hüffmeier U, Buding B, Messmer BJ, von Bernuth G, Seghaye MC. Cytokine balance in infants undergoing cardiac operation. Ann Thorac Surg. 2002;73:601–8 (discussion 608-609).
Magnusson L, Zemgulis V, Wicky S, Tydén H, Thelin S, Hedenstierna G. Atelectasis is a major cause of hypoxemia and shunt after cardiopulmonary bypass: an experimental study. Anesthesiology. 1997;87:1153–63.
Hachenberg T, Tenling A, Rothen HU, Nyström SO, Tyden H, Hedenstierna G. Thoracic intravascular and extravascular fluid volumes in cardiac surgical patients. Anesthesiology. 1993;79:976–84.
Ranieri VM, Vitale N, Grasso S, Puntillo F, Mascia L, Paparella D, Tunzi P, Giuliani R, de Luca TL, Fiore T. Time-course of impairment of respiratory mechanics after cardiac surgery and cardiopulmonary bypass. Crit Care Med. 1999;27:1454–60.
Wynne R, Botti M. Postoperative pulmonary dysfunction in adults after cardiac surgery with cardiopulmonary bypass: clinical significance and implications for practice. Am J Crit Care. 2004;13:384–93.
Tan L, Sun X, Zhu X, Zhang Z, Li J, Shu Q. Epidemiology of nosocomial pneumonia in infants after cardiac surgery. Chest. 2004;125:410–7.
Fischer JE, Allen P, Fanconi S. Delay of extubation in neonates and children after cardiac surgery: impact of ventilator-associated pneumonia. Intensive Care Med. 2000;26:942–9.
Chan EH, Russell JL, Williams WG, Van Arsdell GS, Coles JG, McCrindle BW. Postoperative chylothorax after cardiothoracic surgery in children. Ann Thorac Surg. 2005;80:1864–70.
Joho-Arreola AL, Bauersfeld U, Stauffer UG, Baenziger O, Bernet V. Incidence and treatment of diaphragmatic paralysis after cardiac surgery in children. Eur J Cardiothorac Surg. 2005;27:53–7.
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100:9–15.
Gargani L, Lionetti V, Di Cristofano C, Bevilacqua G, Recchia FA, Picano E. Early detection of acute lung injury uncoupled to hypoxemia in pigs using ultrasound lung comets. Crit Care Med. 2007;35:2769–74.
Rimensberger PC, Cheifetz IM. Ventilatory support in children with pediatric acute respiratory distress syndrome: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med. 2015;16:S51-60.
Young CC, Harris EM, Vacchiano C, Bodnar S, Bukowy B, Elliott RRD, Migliarese J, Ragains C, Trethewey B, Woodward A, Gama de Abreu M, Girard M, Futier E, Mulier JP, Pelosi P, Sprung J. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth. 2019;123:898–913.
Acknowledgements
Not applicable
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YS designed the study, collected, analyzed and interpreted the data, and drafted the manuscript. XMD conceived and designed the study. YC contributed to the statistical analysis and data collection. LYD and SES conceived and designed the study, reviewed the original data and results, and critically revised the manuscript. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine approved the retrospective protocol of the survey (approval NO. XHEC-D-2017-006). This was an observational study. No intervention was given to any of the patients. The requirement for informed consent was waived by the Ethics Committee of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, Y., Deng, XM., Cai, Y. et al. Post-cardiopulmonary bypass hypoxaemia in paediatric patients undergoing congenital heart disease surgery: risk factors, features, and postoperative pulmonary complications. BMC Cardiovasc Disord 22, 430 (2022). https://doi.org/10.1186/s12872-022-02838-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02838-9