Abstract
Background
The platelet-lymphocyte ratio (PLR), a novel inflammatory marker, is generally associated with increased in-hospital mortality risk. We aimed to investigate the association between PLR and postoperative in-hospital mortality risk in patients with type A acute aortic dissection (AAAD).
Methods
Patients (n = 270) who underwent emergency surgery for AAAD at Xiangya Hospital of Central South University between January 2014 and May 2019 were divided into three PLR-based tertiles. We used multiple regression analyses to evaluate the independent effect of PLR on in-hospital mortality, and smooth curve fitting and a segmented regression model with adjustment of confounding factors to analyze the threshold effect between PLR and in-hospital mortality risk.
Results
The overall postoperative in-hospital mortality was 13.33%. After adjusting for confounders, in-hospital mortality risk in the medium PLR tertile was the lowest (Odds ratio [OR] = 0.20, 95% confidence interval [CI] = 0.06–0.66). We observed a U-shaped relationship between PLR and in-hospital mortality risk after smoothing spline fitting was applied. When PLR < 108, the in-hospital mortality risk increased by 10% per unit decrease in PLR (OR = 0.90, P = 0.001). When the PLR was between 108 and 188, the mortality risk was the lowest (OR = 1.02, P = 0.288). When PLR > 188, the in-hospital mortality risk increased by 6% per unit increase in PLR (OR = 1.06, P = 0.045).
Conclusions
There was a U-shaped relationship between PLR and in-hospital mortality in patients with AAAD, with an optimal PLR range for the lowest in-hospital mortality risk of 108–188. PLR may be a useful preoperative prognostic tool for predicting in-hospital mortality risk in patients with AAAD and can ensure risk stratification and early treatment initiation.
Similar content being viewed by others
Background
Type A acute aortic dissection (AAAD) is characterized by an intimal tear based on medial degeneration, with blood surging into the artery wall to form an intimal flap separating the true and false lumen. It is a lethal cardiovascular emergency with a high incidence and early mortality [1, 2]. Predictive biomarkers for identifying increased mortality risk in AAAD patients are important for both risk stratification and early treatment initiation. Inflammation and hemostasis reportedly play pivotal roles in the initiation and progression of AAAD [3, 4]. Inflammatory cells can infiltrate the aortic wall around the vessel and at the margin of the torn media [4, 5]. Moreover, a variety of inflammatory biomarkers have increasingly attracted attention as prognostic indicators in patients with AAAD [6, 7]. Except for inflammatory cells and cytokines, procalcitonin and prognostic nutritional index have also been reported to be related with mortality in AAAD patients [8, 9]. As mediators of inflammation, activated platelets stimulate pathogenic thrombosis in response to atherosclerotic plaque rupture or erosion [10]. Previously, we reported that a low platelet count was a risk factor for postoperative pneumonia in patients with AAAD [11].
The platelet-lymphocyte ratio (PLR) is an integrated reflection of thrombotic/inflammatory pathways. Initially, it was considered a systemic inflammatory biomarker used in the prognosis of neoplastic diseases; however, it is now considered a prognostic marker in cardiovascular diseases [12]. Studies have shown that a high PLR can be used to predict in-hospital mortality in patients with an ST-elevated myocardial infarction [13], without a reflow postpercutaneous intervention [14], and with an acute exacerbation of chronic obstructive pulmonary disease [15]. Few studies have investigated the association between the PLR and the risk of in-hospital mortality in patients with AAAD. Bedel et al. [16] reported that a high PLR at admission was associated with increased in-hospital mortality in patients with AAAD. However, Yang et al. [17] suggested that a high preoperative PLR in patients with AAAD is correlated with a better prognosis. In addition, a study demonstrated that the PLR could be used for the differential diagnoses of similar diseases, but its usefulness in prognosis assessment should be further investigated [18]. Furthermore, there is no existing evidence of a non-linear relationship between PLR and postoperative in-hospital mortality in patients with AAAD.
Therefore, we aimed to explore the relationship between PLR and postoperative in-hospital mortality in patients with AAAD to improve risk stratification and treatment.
Methods
Patient selection and study endpoint
In this retrospective cohort study, we identified patients with AAAD who underwent surgery within 48 h of admission to Xiangya Hospital of Central South University between January 2014 and May 2019. Patients with a typical history of chest pain, as well as AAAD-related computed tomography and echocardiography findings, were diagnosed with AAAD. Stanford type A (DeBakey type I and type II) dissection involved the ascending aorta with or without aortic arch. Patients with aches or other related symptoms that occurred within 2 weeks before admission were diagnosed with acute type A dissection [19]. All surgical patients aged ≥ 18 years and diagnosed with AAAD were included. Patients with preoperative severe organ dysfunction or those who died intraoperatively were excluded [20]. Postoperative in-hospital mortality was the primary end point. This study was conducted in accordance with the ethical standards of the Declaration of Helsinki of the World Medical Association and the guidelines for good clinical practice. It was approved by the Medical Ethics Committee of Xiangya Hospital of Central South University (Ethical Number: 2019010038). The requirement for individual consent was waived because of the retrospective nature of the study.
Surgical procedure
During surgery, the patient lay in the supine position and was administered general anesthesia. The point of incision was the middle of the sternum. Cardiopulmonary bypass (CPB) was performed through the right atrial arteries to the right axillary artery by cannulation. Femoral artery cannulation was performed when the dissection involved the right axillary artery, or the pumping pressure was too high. The right axillary artery was used for intubation, and selective anterograde cerebral perfusion was used for cerebral protection. At moderate hypothermia, the circulation was stopped; the ascending aorta was blocked; and cardiac arrest fluid was perfused. When the nasopharyngeal temperature was 25 °C; the three branch vessels of the aortic arch were blocked; the brain was perfused through the right axillary artery; the aortic arch and the ascending aorta were cut longitudinally; the descending aorta was transected; and the frozen elephant trunk stent was implanted into the true lumen of the distal descending aorta and then released; and the ascending aorta was replaced. When the aortic root or valve was also involved, the Bentall procedure, David procedure, or another procedure was performed simultaneously. The stented graft was then anastomosed end-to-end with the 4-branched vessels. On completion of the anastomosis, perfusion in the lower body was resumed through the perfusion limb of the tetrafurcate graft; the CPB flow was gradually returned to 2.0–2.4 L/m2/min; and rewarming was initiated. The branches of the aortic arch were reconstructed during the rewarming phase. Finally, the heartbeat was restored, and the patient’s chest was closed, as performed routinely. Blood pressure during and after operation was measured through the radial and dorsalis pedis arterial line.
Data collection
We collected patients’ demographic, laboratory, and clinical data by reviewing their medical records. Demographic data included age and sex. Laboratory data included lymphocyte, platelet counts, hemoglobin, international normalized ratio, prothrombin time and activated partial thromboplastin time. Clinical information included perioperative data, smoking history, alcohol consumption, hypertension, diabetes mellitus, Marfan syndrome, hemopericardium, coronary artery disease, cerebrovascular disease, chronic renal failure, and the Penn class. Perioperative data included intraoperative CPB time, ventilator use, operative time, surgery type, autologous blood transfusion (≥ 500 mL), and blood product transfusion (platelet, cryoprecipitate, red blood cells [RBCs], and plasma).
PLR was defined as the platelet to lymphocyte ratio; the platelet and lymphocytes counts were obtained from routine blood tests. The patients’ first venous blood samples taken on admission to the hospital were used to run the routine blood investigations. The ethylenediaminetetraacetic-anticoagulated blood samples were run through the Beckman Coulter LH 750 and Sysmex XN-20A1 analyzers (Beckman Coulter Trading (China) Co., Ltd. Shanghai, China).
Statistical analysis
Continuous variables were presented as means ± standard deviations (SD) or medians with quartile (Q) ranges. Categorical variables were presented as frequencies and percentages. Continuous variables were compared using the t-test (for a normal distribution) or Mann–Whitney U test (for a skewed distribution). The χ2 test was used to compare categorical variables. There was no multicollinearity between independent variables.
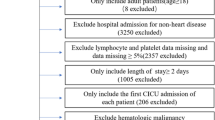
Based on the PLR, the patients were divided into three tertiles: lowest (T1: PLR < 112.73, n = 90), medium (T2: 112.73 ≤ PLR < 179, n = 90), and highest (T3: PLR ≥ 179, n = 90). The baseline characteristics of the three groups were compared (Table 1). A univariate analysis was used to evaluate the associations between the variables and postoperative in-hospital mortality (Fig. 1). We evaluated the independent effect of PLR on postoperative in-hospital mortality in patients with AAAD using four multiple logistic regression models. No variables were adjusted in Model I, while age and sex were adjusted in Model II. In Model III, we adjusted for age, sex, and variables with P-values less than 0.10 (Table 1, Fig. 1). These variables included cerebrovascular disease; chronic renal failure; transfusion of autologous blood (≥ 500 mL), cryoprecipitates, RBCs, plasma, and platelets; surgery type; Marfan syndrome; and operative time. In Model IV, we adjusted for age, sex, and covariances. The covariance adjustment was performed when the variables added to this Model changed the matched odds ratio (OR) by at least 10% [21]. These covariances included alcohol consumption; diabetes mellitus; cerebrovascular disease; chronic renal failure; transfusion of autologous blood (≥ 500 mL), cryoprecipitates, RBCs, plasma, and platelets; and operative time. Smooth curve fitting was performed to determine the linear relationship between PLR and risk of postoperative in-hospital mortality in patients with AAAD. Furthermore, a segmented regression model and the logarithmic likelihood ratio test (LRT) was used to analyze the threshold effect between the PLR and postoperative in-hospital mortality in patients with AAAD.
All statistical analyses were performed with R (http://www.R-project.org, The R Foundation) and EmpowerStats software (http://www.empowerstats.com, X&Y Solutions, Inc, Boston, MA, USA). A two-tailed P value < 0.05 was considered significant.
Results
Patient characteristics
A total of 280 patients were eligible for this study. After excluding one patient with severe preoperative multiple organ failure (0.37%) and nine patients with intraoperative mortality (3.33%), the remaining 270 patients were enrolled in the study; 70.0% (189/270) were men; and 13.33% (36/270) experienced postoperative in-hospital mortality.
The baseline characteristics are shown in Table 1. There were significant differences in postoperative in-hospital mortality among the tertiles (P = 0.002). Intertertile comparisons showed that postoperative in-hospital mortality was the highest, intermediate, and lowest in the T1 (21, 23.33%), T3 (9, 10.00%), and T2 (6, 6.67%) groups, respectively. The number of patients who received platelet transfusion was higher in the T1 and T2 groups (therapeutic dose > 1, P = 0.003) than in the T3 group. There were no significant differences in the other variables between the groups.
Variables related to postoperative in-hospital mortality
The results of the univariate analysis are shown in Fig. 1. PLR and PLR tertiles were negatively associated with the risk of in-hospital mortality (P = 0.03). Moreover, chronic renal failure (OR = 3.53, P = 0.049); cerebrovascular disease (OR = 7.83, P < 0.001); and the transfusion of cryoprecipitates (OR = 2.5, P = 0.01), RBCs (OR = 10.15, P < 0.001), and plasma (OR = 6.47, P < 0.001) were positively associated with the risk of postoperative in-hospital mortality.
Association of the PLR with postoperative in-hospital mortality
When PLR was used as a continuous variable, it was negatively correlate with postoperative in-hospital mortality in the four models (OR: 0.99, 95% confidence interval [CI]: 0.99–1). When the PLR was used as a tertile categorical variable, the risk of postoperative in-hospital mortality in the T2 group was the lowest in Model I (OR: 0.30, 95% CI: 0.12–0.75), compared to those in the T1 and T3 groups. Similar results were observed in Models II (OR: 0.31, 95% CI: 0.12–0.78), III (OR: 0.17, 95% CI: 0.05–0.58), and IV (OR: 0.2, 95% CI: 0.06–0.66). For the sensitivity analysis, PLR was considered as three equal categorical variables and a continuous variable separately, and the trend of the relationship between PLR and postoperative in-hospital mortality was consistent (P < 0.05) (Table 2).
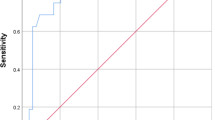
Nonlinear relationship between the PLR and risk of postoperative in-hospital mortality
There was a U-shaped relationship between PLR and postoperative in-hospital mortality risk in patients with AAAD after smoothing spline fitting was applied and covariates were adjusted (Fig. 2). The turning point values of PLR (108, 188) were found using the segmentation regression model (Table 3). When PLR was < 108, the postoperative in-hospital mortality risk increased by 10% per unit decrease in PLR (OR = 0.90, P = 0.001). When PLR was between 108 and 188, the mortality risk was the lowest (OR = 1.02, P = 0.288). When PLR was > 188, the mortality risk increased by 6% per unit increase in PLR (OR = 1.06, P = 0.045). A P value < 0.001 for the LRT illustrated a nonlinear relationship between PLR and postoperative in-hospital mortality risk.
Smoothing spline fitting curve. After adjusting for age; sex; cerebrovascular disease; chronic renal failure; autologous blood (≥ 500 mL), cryoprecipitate, RBCs, plasma, and platelet transfusion; surgery type; Marfan syndrome; and operative time, we observed a U-shaped relationship between PLR and postoperative in-hospital mortality risk in patients with AAAD. Nonlinear plots are displayed with red dotted lines, and the blue dotted lines represent 95% confidence intervals
Discussion
We observed a U-shaped relationship between PLR and postoperative in-hospital mortality in patients with AAAD and found that 108–188 was the range of optimal PLRs associated with the lowest mortality risk. Moreover, PLR was negatively correlated with postoperative in-hospital mortality risk for PLR < 108 and positively correlated for PLR > 188. Du et al. had similar findings in patients with type B AAD [22]. They observed a U-shaped association between PLR at admission and in-hospital death and indicated that patients with a decreased or elevated PLR had significantly increased in-hospital mortality compared to those with an intermediate PLR. Bedel et al. [16] reported a correlation between high PLR (> 195.8) and increased in-hospital mortality in patients with AAAD. However, Yang et al. [17] found that a high preoperative PLR (≥ 150) was associated with a low incidence of postoperative adverse events. Contrastingly, Sbarouni et al. found no association between the PLR and mortality [18]. The optimal PLR range in our study suggested that maintaining the preoperative PLR within this range might effectively reduce the in-hospital mortality risk.
PLR, as an inflammatory biomarker, positively correlated with adverse prognoses in other diseases. In a study of 520 patients who underwent transcatheter aortic valve replacement, a high PLR was associated with an increased occurrence of 30-day adverse outcomes [23]. Similarly, Ye et al. [24] confirmed a positive relationship between PLR and lower extremity peripheral artery disease severity. Turcato et al. [25] reported that PLR was independently associated with 30-day mortality in patients with acute decompensated heart failure.
The underlying mechanism of the relationship between PLR and mortality in patients with AAAD remains unclear. In our study, a U-shaped relationship existed between PLR and mortality; that is, low PLR (caused by low platelet counts on admission) and high PLR (caused by a low lymphocyte) were related with increased in-hospital mortality risk. Platelets reflected the degree of thrombosis in AAAD, and lower platelet counts suggested platelet dysfunction, which increased the overall bleeding risk of perioperative patients and aggravated ischemia–reperfusion injury [26]. Decreased platelet counts and platelet dysfunction were related to platelet activation [10, 27] and disseminated intravascular coagulation [28]. Activated platelets release inflammatory mediators into the local microenvironment to recruit leukocytes and trigger platelet aggregation [29]. They may deteriorate the state of inflammation and coagulation, aggravate the aortic intimal injury, and increase the incidence of poor outcomes. Furthermore, massive platelet consumption can increase the hazards of dissection rupture and aggravate organ ischemia [10]. Many studies have demonstrated that a low platelet count is associated with increased in-hospital mortality in patients with AAAD [6, 30, 31]. Contrarily, low lymphocyte counts can reflect the severity of inflammation, which is related to poor outcomes in patients with cardiovascular diseases [32]. Physiological stress and overall immune metabolic depression in patients with AAAD can lead to lymphopenia [4, 18], which reduces effectivity against oxidative and inflammatory injury. Taken together, both inflammation and hemostasis play important roles in the pathogenesis and prognosis of AAAD; however, assessment of inflammatory and thrombosis aids in studying the complete thrombo-inflammatory process in AAAD. Based on this mechanism, PLR, as the inflammatory and thrombotic coexistence biomarker, could reflect the degree of thrombosis and inflammation simultaneously and was a stronger predictor of in-hospital mortality than either of those biomarkers alone. Thus, it is reasonable to believe that an elevated or decreased PLR is associated with adverse outcomes in patients with AAAD.
This study had some limitations. First, this was a single-center retrospective study with a small sample size, which may have limited the subgroup analysis and introduced inevitable bias. Furthermore, the lymphocyte cell count was influenced by many factors, including age, gender, race, smoking, pregnancy, infections and so on [33]. However, to control for bias, we adjusted for potential confounding factors during the data analysis; therefore, our results remain credible.
Second, this was a retrospective study and can only show the association between PLR and mortality. Therefore, we will design a prospective, multi-center and large-scale study to verify the U-shaped correlation between PLR and postoperative in-hospital mortality in patients with AAAD. Third, due to the acute onset of AAAD, we could not collect blood samples of patients at the same time of day, this might cause us to ignore the impact of the diurnal or circadian variation of lymphocyte cell count. Fourth, we did not explore the relationship between PLR and the long-term prognosis of patients with AAAD. Currently, these patients have been following up to determine the relationship between PLR and the long-term prognosis.
Conclusions
We found a novel U-shaped relationship between PLR and postoperative in-hospital mortality in patients with AAAD, with the optimal PLR range for the lowest in-hospital mortality being 108–188. Thus, PLR may serve as a preoperative prognostic tool to predict the risk of in-hospital mortality in patients with AAAD, as this could assist in risk stratification and early treatment initiation.
Availability of data and materials
The datasets used and analyzed during the current study available from the corresponding authors on reasonable request.
Abbreviations
- AAAD:
-
Type A acute aortic dissection
- PLR:
-
Platelet–lymphocyte ratio
- CPB:
-
Cardiopulmonary bypass
- RBCs:
-
Red blood cells
- LRT:
-
Likelihood ratio test
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Xia L, Li JH, Zhao K, Wu HY. Incidence and in-hospital mortality of acute aortic dissection in China: analysis of China Health Insurance Research (CHIRA) Data 2011. J Geriatr Cardiol. 2015;12(5):502–6.
Reutersberg B, Salvermoser M, Trenner M, Geisbüsch S, Zimmermann A, Eckstein HH, Kuehnl A. Hospital incidence and in-hospital mortality of surgically and interventionally treated aortic dissections: secondary data analysis of the nationwide German diagnosis-related group statistics from 2006 to 2014. J Am Heart Assoc. 2019;8(8):e11402.
Erdolu B, As AK. C-Reactive protein and neutrophil to lymphocyte ratio values in predicting inhospital death in patients with Stanford type A acute aortic dissection. Heart Surg Forum. 2020;23(4):E488–92.
Wu D, Choi JC, Sameri A, Minard CG, Coselli JS, Shen YH, LeMaire SA. Inflammatory cell infiltrates in acute and chronic thoracic aortic dissection. AORTA. 2013;1(6):259–67.
He R, Guo D, Estrera AL, Safi HJ, Huynh TT, Yin Z, Cao S, Lin J, Kurian T, Buja LM, et al. Characterization of the inflammatory and apoptotic cells in the aortas of patients with ascending thoracic aortic aneurysms and dissections. J Thorac Cardiovasc Surg. 2006;131(3):671–8.
Chen Y, Lin Y, Zhang H, Peng Y, Li S, Huang X. Relationship of platelet counts and inflammatory markers to 30-Day mortality risk in patients with acute type A aortic dissection. Biomed Res Int. 2020;2020:1–7.
Lin Y, Peng Y, Chen Y, Li S, Huang X, Zhang H, Jiang F, Chen Q. Association of lymphocyte to monocyte ratio and risk of in-hospital mortality in patients with acute type A aortic dissection. Biomark Med. 2019;13(15):1263–72.
Keskin HA, Kurtul A, Esenboğa K, Çiçek MC, Katırcıoğlu SF. Prognostic nutritional index predicts in-hospital mortality in patients with acute Stanford type A aortic dissection. Perfusion. 2021;36(7):710–6.
Liu H, Luo Z, Liu L, Yang X, Zhuang Y, Tu G, Ma G, Zhang Y, Zheng J, Zhu D, et al. Inflammatory biomarkers to predict adverse outcomes in postoperative patients with acute type A aortic dissection. Scand Cardiovasc J. 2020;54(1):37–46.
Jennings L. Mechanisms of platelet activation: need for new strategies to protect against platelet-mediated atherothrombosis. Thromb Haemostasis. 2017;102(08):248–57.
Yao R, Liu X, He Y, Mei C, Shen Y, Zhan Q, Huang L, Li B, Li N. Low platelet count is a risk factor of postoperative pneumonia in patients with type A acute aortic dissection. J Thorac Dis. 2020;12(5):2333–42.
Kurtul A, Ornek E. Platelet to lymphocyte ratio in cardiovascular diseases: a systematic review. Angiology. 2019;70(9):802–18.
Temiz A, Gazi E, Gungor O, Barutcu A, Altun B, Bekler A, Binnetoglu E, Sen H, Gunes F, Gazi S. Platelet/lymphocyte ratio and risk of in-hospital mortality in patients with ST-elevated myocardial infarction. Med Sci Monit. 2014;20:660–5.
Yildiz A, Yuksel M, Oylumlu M, Polat N, Akyuz A, Acet H, Aydin M, Ülgen MS. The utility of the platelet–lymphocyte ratio for predicting no reflow in patients with ST-Segment elevation myocardial infarction. Clin Appl Thromb Hemost. 2015;21(3):223–8.
Yao C, Liu X, Tang Z. Prognostic role of neutrophil–lymphocyte ratio and platelet–lymphocyte ratio for hospital mortality in patients with AECOPD. Int J Chron Obstruct Pulmon Dis. 2017;12:2285–90.
Bedel C, Selvi F. Association of platelet to lymphocyte and neutrophil to lymphocyte ratios with In-Hospital mortality in patients with type A acute aortic dissection. Braz J Cardiov Surg. 2019;34(6):694–8.
Yang T, Wang L, Xiao L, Huang F, Chen X. Prognostic value of platelet/lymphocyte ratio in patients with type A acute aortic dissection. Mod Med J. 2018;46(06):656–9.
Sbarouni E, Georgiadou P, Kosmas E, Analitis A, Voudris V. Platelet to lymphocyte ratio in acute aortic dissection. J Clin Lab Anal. 2018;32(7):e22447.
Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(41):2873–926.
Helgason D, Helgadottir S, Ahlsson A, Gunn J, Hjortdal V, Hansson EC, Jeppsson A, Mennander A, Nozohoor S, Zindovic I, et al. Acute kidney injury after acute repair of type A aortic dissection. Ann Thorac Surg. 2021;111(4):1292–8.
Kernan WN, Viscoli CM, Brass LM, Broderick JP, Brott T, Feldmann E, Morgenstern LB, Wilterdink JL, Horwitz RI. Phenylpropanolamine and the risk of hemorrhagic stroke. New Engl J Med. 2000;343(25):1826–32.
Du R, Li D, Yu J, Ma Y, Zhang Q, Zeng Z, Zeng R. Association of platelet to lymphocyte ratio and risk of in-hospital mortality in patients with type B acute aortic dissection. Am J Emerg Med. 2017;35(2):368–70.
Condado JF, Junpaparp P, Binongo JN, Lasanajak Y, Witzke-Sanz CF, Devireddy C, Leshnower B, Mavromatis K, Stewart J, Guyton R, et al. Neutrophil-lymphocyte ratio (NLR) and platelet-lymphocyte ratio (PLR) can risk stratify patients in transcatheter aortic-valve replacement (TAVR). Int J Cardiol. 2016;223:444–9.
Ye M, Qian X, Guo X, Wang H, Ni Q, Zhao Y, Xue G, Deng H, Zhang L. Neutrophil–lymphocyte ratio and platelet–lymphocyte ratio predict severity and prognosis of lower limb arteriosclerosis obliterans. Ann Vasc Surg. 2020;64:221–7.
Turcato G, Sanchis-Gomar F, Cervellin G, Zorzi E, Sivero V, Salvagno GL, Tenci A, Lippi G. Evaluation of neutrophil–lymphocyte and platelet–lymphocyte ratios as predictors of 30-day mortality in patients hospitalized for an episode of acute decompensated heart failure. J Med Biochem. 2019;38(4):452–60.
Tanaka M, Kawahito K, Adachi H, Ino T. Platelet dysfunction in acute type A aortic dissection evaluated by the laser light-scattering method. J Thorac Cardiovasc Surg. 2003;126(3):837–41.
Sbarouni E, Georgiadou P, Analitis A, Voudris V. Significant changes in platelet count, volume and size in acute aortic dissection. Int J Cardiol. 2013;168(4):4349–50.
Liu Y, Han L, Li J, Gong M, Zhang H, Guan X. Consumption coagulopathy in acute aortic dissection: principles of management. J Cardiothorac Surg. 2017;12(1):50.
Liu X, Wang G, Zhang T. The analysis of the levels of plasma inflammation-related cytokines and endotoxins in patients with acute aortic dissection. Clin Hemorheol Micro. 2020;76(1):1–7.
Huang B, Tian L, Fan X, Zhu J, Liang Y, Yang Y. Low admission platelet counts predicts increased risk of in-hospital mortality in patients with type A acute aortic dissection. Int J Cardiol. 2014;172(3):e484–6.
Li S, Lu J, Cheng W, Zhu J, Jin M. Factors associated with low admission platelet count in adults with acute aortic dissection. Ann Thorac Cardiovasc Surg. 2019;25(3):142–8.
Núñez J, Sanchis J, Bodí V, Núñez E, Heatta AM, Miñana G, Merlos P, Rumiz E, Palau P, Sanjuán R, et al. Therapeutic implications of low lymphocyte count in non-ST segment elevation acute coronary syndromes. Eur J Intern Med. 2009;20(8):768–74.
Shete A, Thakar M, Abraham PR, Paranjape R. A review on peripheral blood CD4+ T lymphocyte counts in healthy adult Indians. Indian J Med Res. 2010;132:667–75.
Acknowledgements
We wish to thank Editage (www.editage.cn) for the English language editing.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 81873574). The funding bodies did not have role in the design of the study, data collection and analysis, nor on the interpretation and dissemination of the results.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study concept and design; XF, YZ and DY collected and assembled data; RY and XX operated the software and statistical analysis; WH, LH and YD performed the data analysis and interpretation; XX contributed to writing-original draft; NL obtained the funding. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Xiangya Hospital of Central South University (Ethical Number: 2019010038). The requirement for individual consent was waived because of the retrospective nature of the study, which was approved by the Medical Ethics Committee of Xiangya Hospital of Central South University. We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xie, X., Fu, X., Zhang, Y. et al. U-shaped relationship between platelet–lymphocyte ratio and postoperative in-hospital mortality in patients with type A acute aortic dissection. BMC Cardiovasc Disord 21, 569 (2021). https://doi.org/10.1186/s12872-021-02391-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02391-x