Abstract
Background
Transcatheter valve replacement (TAVR) is an important therapeutic intervention for patients with aortic valve stenosis. As TAVR has become available to a broader population, there has been an increase in the number of less common, yet potentially catastrophic, complications. TAVR related infective endocarditis (TAVR-IE) is a rare, but potentially fatal, complication.
Case series
We present here two patients that we encountered for TAVR associated infective endocarditis. Our first patient presented 5 weeks after his TAVR. His initial presentation was consistent with signs of sepsis. The patient then developed Mobitz type I block during hospital course. His TEE was negative for features of infective endocarditis. Due to high suspicion, patient was taken for surgical exploration and was found to have multiple foci of vegetation adhered to the stent frame. Our second patient presented with new onset pulmonary edema, worsening heart failure and systemic inflammatory response. A TEE was done for persistent MSSA bacteremia which showed stable prosthetic valve function with no signs of infective endocarditis. Patient was discharged with a prolonged course of intravenous antibiotics. Patient was re-admitted for worsening sepsis and blood cultures were positive for MSSA. Patient was taken for surgical exploration of his prosthetic aortic valve which showed purulent aortic root abscess.
Conclusion
Through these cases, we aim to raise awareness on TAVR-IE. Due to the atypical clinical presentation, the modified Duke criteria may not be sufficient to diagnose TAVR-IE. Transesophageal echocardiogram in TAVR-IE may be negative or indeterminate. Prosthetic valve shadow may obscure smaller vegetations and/or smaller abscesses. A negative transesophageal echocardiogram should not rule out TAVR-IE and further diagnostic imaging modalities should be considered. PET/CT after administration of 18F-FDG (fluorodeoxyglucose) is a useful diagnostic tool in the diagnosis of infective endocarditis where TEE has been negative or inconclusive. Multi-modal imaging, in addition to the modified Duke criteria, can facilitate early diagnosis and improved mortality outcomes.
Similar content being viewed by others
Introduction
The emergence of transcatheter valve replacement (TAVR) has revolutionized the treatment and care of patients with symptomatic severe aortic stenosis (AS) across the spectrum of risk. With increasing clinical expertise and the advent of a new generation of valves, outcomes have improved significantly and TAVR is now being implemented in a much broader spectrum of patients than ever before.
With TAVR becoming available to a larger population, we also now see a rise in complications that may be less common yet catastrophic. Some of the grave complications of TAVR include paravalvular leak, stroke, vascular injury, heart block, and prosthetic valve endocarditis (PVE). TAVR-IE is a rare, but potentially fatal, complication. One of the challenges in the management of such cases is timely diagnosis. Patients with IE may fail to meet the modified Duke criteria [1,2,3,4]. Transesophageal echocardiogram (TEE), which remains an important diagnostic option for diagnosis in native valve endocarditis, may yield negative or inconclusive results in patients with prosthetic valves. This could be due to the higher density of the prosthetic valve or the metallic frame, which can cause impedance in the ultrasonic waves and acoustic shadowing. As such, a multi-modal imaging approach should be adopted in these patients [5].
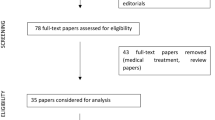
We present two cases of TAVR-IE. These patients had negative TEE for apparent vegetation and failed to meet the modified Duke criteria for IE. Through these case reports and the literature review, we aim to raise the suspicion for TAVR-IE in order to facilitate timely diagnosis and to prevent adverse outcomes.
Case 1
A 79-year-old male (Table 1) presented with altered mental status and back pain 5 weeks after undergoing TAVR with a 29 mm Medtronic Corevalve Evolut Pro (Medtronic, Galway, Ireland) via transfemoral approach. He had been seen in the outpatient clinic 3 days earlier and no clinical changes, EKG or transthoracic echocardiogram (TTE) abnormalities were noted at that time. In the emergency department, the patient was found to be tachycardiac with heart rate of 110 bpm, tachypneic with respiratory rate of 32 and hypoxic with SpO2 of 96% on 2 L O2 via nasal cannula. Lab results showed: white blood cell count of 5.5 K/μL with 31% bands, lactic acid of 2.2 mmol/L and a normal comprehensive metabolic panel. Urine analysis was negative for any abnormality. CT brain did not show any acute intracranial abnormality and contrast enhanced CT scan of the abdomen and pelvis was unremarkable for any acute process. He was started empirically on broad spectrum antibiotics with vancomycin 15 mg/kg/day and cefepime 1 g every 6 h. Initial blood cultures showed gram positive cocci. MRI of spine was performed which was negative for infection. On day 2, the patient developed Mobitz type I block, widened QRS, and wide escape beats of varying morphology (Figs. 1, 2).
Blood cultures showed methicillin-sensitive Staphylococcus aureus (MSSA). The patient underwent TEE, which showed thickening in the posterior aspect of the aortic root near the site of the interatrial septum. It also showed increased paravalvular aortic regurgitation when compared to the post-TAVR echocardiogram. However, there was no clear evidence of vegetation.
The initial plan was to perform a tagged white blood scan, however due to unavailability of the scan, the patient’s worsening conditioning, and high suspicion for TAVR associated endocarditis, the patient was taken for surgical exploration (Additional file 1: Video S1, Additional file 2: Video S2, Additional file 3: Video S3).
The explanted valve had multiple foci of vegetation adherent to the stent frame. There was aortic root abscess. The prosthetic valve was replaced with a 27 mm Magna-Ease valve (Edwards Lifesciences Corp. Irvine, CA) (Additional file 4: Video S4) (Fig. 3).
The patient was discharged with antibiotics on day 14 in stable condition. Aspirin and clopidogrel were continued at discharge. Patient showed a well-functioning valve with no clinical symptoms at 6 months follow up (Additional file 8).
Case 2
A 71-year-old male with (Table 1) presented with generalized weakness, altered mental status, abdominal pain, diarrhea and fever 8 weeks after TAVR with a 34 mm Corevalve Evolut Pro. He had been seen in the outpatient clinic 2 weeks earlier. No clinical or echocardiographic changes were noted from a previous post-TAVR echocardiogram. In the emergency department, the patient was found to have a temperature of 37.8 C, heart rate of 111 beats per minute, respiratory rate of 36 breath per minute and saturating 92% on room air with normal blood pressure. Complete blood count showed normal leucocyte count with 21% bandemia and platelet count of 86,000/microliter which was chronic for the patient. His basic metabolic panel results were significant for bicarbonate level of 13.6 mEq/L with a lactic acid level of 6.6 mmol/L. Liver function test and coagulation profile was normal on admission. Initial EKG did not show any new changes from the baseline. Chest X-ray did not show any evidence of acute process. Contrast-enhanced CT scan of the abdomen and pelvis did not show any pathology. Infectious panel was sent for diarrhea which included clostridium difficile, and patient was started empirically on broad spectrum antibiotics with vancomycin 15 mg/kg/day, cefepime 1 g every 6 h and metronidazole 500 mg daily. A TTE was done which showed stable prosthetic valve function with no new regurgitation. The patient continued to remain febrile and tachypneic with altered mental status on broad spectrum antibiotics. Initial blood culture showed gram positive cocci in pairs and clumps in 4/4 bottles. A repeat TEE was done which showed no evidence of valvular vegetation; however, the aortic valve bioprosthesis was suboptimally visualized. A trace degree of aortic insufficiency was noted. Blood cultures resulted in MSSA bacteremia in 4/4 bottles and antibiotics were deescalated to intravenous cefazolin (Additional file 5: Video S5, Additional file 9).
One week after presentation the patient developed polymorphic ventricular tachycardia and fibrillation requiring CPR/defibrillation. He also developed acute interstitial nephritis from cefazolin requiring intermittent hemodialysis and was switched to vancomycin/rifampin. The patient continued to improve hemodynamically and clinically, and given no clear evidence of infective endocarditis he was managed medically. Blood cultures became negative and after 9 days and he was discharged to acute rehab with a wearable cardioverter/defibrillator, and his aspirin and apixaban were continued at discharge.
In rehab, the patient developed persistent fever and patient was re-admitted for developing sepsis. Blood cultures were again positive for MSSA. At this time, a decision was made for explantation of the prosthetic aortic valve based on clinical suspicion of endocarditis.
The explanted valve showed purulent root abscess. A 25 mm Intuity valve (Edwards Lifesciences Corp. Irvine, CA, USA) with Cardiocel pericardial patch (LeMaitre Vascular, Inc., Burlington MA, USA) was placed between the non-coronary cusp and right coronary cusp (Figs. 4, 5).
The patient developed hemodynamic instability and bedside emergent extracorporeal membrane oxygenation (ECMO) was deployed. He developed gastrointestinal ischemia, renal failure and acute blood loss while on ECMO. Due to his poor prognosis, the patient's family requested comfort care.
Discussion
With technological advances, newer generation valves, and increasingly favorable outcomes, TAVR is an indispensable procedure in interventional cardiology. With advancing use, we also see a broader spectrum of complications that may not be adequately diagnosed with strict criteria. Both of our patients failed to meet modified Duke’s criteria for IE which delayed diagnosis as well as inadvertently required unnecessary investigations. Through this literature review, we aim to increase the knowledge regarding TAVR-IE to prevent catastrophic complications.
Incidence
TAVR has become well established as the procedure of choice across all surgical risk patients. With the increasing number of procedures being performed, secondary complications have become an emerging cause of morbidity and mortality. TAVR-IE remains a rare complication.
The incidence of TAVR-IE ranges from 0.1 to 4.4% [1, 6, 7]. The Placement of Aortic Transcatheter Valves (PARTNER II) trial estimates the incidence of infective endocarditis after TAVR at 1.44% [8] but the literature shows the incidence to be up to 4.4% [7], with no difference between TAVR and surgical aortic valve replacement (SAVR).
TAVR-IE can be categorized as early (< 2 months), intermediate (2 months to 1 year), or late (> 1 year) based on the time of diagnosis post implantation. The incidence rates are reported to be 18% for early, 62% for intermediate, and 20% for late TAVR-IE [9, 10]. The risk of endocarditis was greatest in the first year after TAVR [9]. Our patients both presented less than 90 days after TAVR.
Risk factors
Multiple risk factors have been associated with increased risk of TAVR-IE. The risk factors can be grouped as modifiable and non-modifiable. Non modifiable risk factors include young age [2, 3, 5] and male sex [3, 7, 11, 12].
Modifiable factors include chronic kidney disease, higher BMI [13] and diabetes mellitus [3, 6, 7]. Liver cirrhosis, pulmonary disease, peripheral artery disease and chronic dialysis have also been identified as independent risk factors for TAVR-IE [13]. Our review of 16 case reports (Additional file 6: Table S1, Additional file 7) found that that 10 out of the 16 patients described in the reports were male. Major comorbidities reported in these cases include diabetes mellitus, chronic kidney disease and chronic obstructive pulmonary disease. Society of Thoracic Surgeons Predicted Risk of Mortality (PROM) scores of 8 or higher are associated with a higher risk of infective endocarditis in TAVR patients [13].
Nosocomial infections have also been identified as risk factors in TAVR patients as they can act as source of seeding [14]. We noted 4 patients in the literature in whom nosocomial infection could have been a potential cause for TAVR-IE; one patient had undergone a dental procedure, the second had a history of total parenteral nutrition, the third had undergone surgery—a high anterior resection, and the fourth had a history of repeated hospital admissions.
Mangner et al. and Reguiro et al., in their studies determined that moderate or severe para-aortic regurgitations were a significant risk factor for PVE [3, 6]. Mangner also stated that valve-in-valve or more than one prosthetic valve carried a higher risk for IE post TAVR.
The literature does not show any differences in the occurrence of TAVR-IE between procedures performed in the operating room versus those done in a catheterization lab [15]. According to Amat-Santos et al., orotracheal intubation increased the risk of TAVR-IE. They also showed that the self-expandable CoreValve (Medtronic Inc., MN, USA) seemed to illustrate a higher risk when compared to balloon expanded valve [2]. In our review of the case reports (Additional file 6: Table S1, Additional file 7), TAVR-IE was associated with three CoreValves, 5 balloon expandable valves, 3 bioprosthetic valves, and 1 other valve. Valve type was not reported in 3 cases.
Microbiology
The most common microorganisms known to cause TAVR-IE are gram-positive cocci, which include Staphylococcus aureus, coagulase negative staphylococci, and enterococci [1,2,3, 6, 16,17,18]. Streptococcus has also been reported to be an important cause of TAVR-IE [19].
Other reported causal organisms associated with TAVR related IE include gram negative rods: E. coli [16, 17, 20], acinetobacter [2, 21] pseudomonas aeruginosa [18, 22], serratia [2], and salmonella [21]. Our patients both had MSSA bacteremia.
Our review of case reports shows a variety of pathogens associated with TAVR-IE: Staphylococcus aureus (1 case), Streptococcus (5 cases), Enterococcus (3 cases), and atypical organisms Moraxella (1 case), Corynebacterium (2 cases), and Candida (2 cases). In two cases, no organisms were isolated.
TAVR-IE shows a different pathogen alignment than SAVR. Enterococcus has a higher incidence in TAVR than SAVR [23]. This could be due to the transfemoral approach, as intertriginous regions such as the groin can harbor enterococcus, which grows better in warm, humid conditions.
Clinical features
The most common presenting feature of patients with TAVR-IE is fever, which was seen in both of our patients. Both patients presented with altered mental status, which could be secondary to severe sepsis.
The second most common initial feature seen in patients with TAVR-IE is clinical heart failure, irrespective of previous systolic and diastolic dysfunction [1, 6]. Our first patient did not have a history of diastolic or systolic heart failure. On presentation, he was found to have pulmonary congestion with dyspnea, BNP of 1490, and his ejection fraction was reduced to 50–55% from 60 to 65%. The second patient also showed a newly decreased ejection fraction, in this case, to 40%.
Another possible complication is new conduction defects or arrhythmias. Our first patient developed a new Mobitz type I block with wide QRS, raising concern for aortic root abscess. He further deteriorated, developed Mobitz type II block and required transvenous pacing. The second patient developed episodes of polymorphic ventricular tachycardia and, on day 3, developed ventricular fibrillation requiring CPR and defibrillation. He subsequently developed tachy-brady syndrome, further complicating management.
Clinical presentations may include, but are not limited to, newly developed heart block, arrhythmias, and embolic phenomenon, with stroke as the most common, and signs and symptoms of source infection, if present [24]. Constitutional symptoms may be present in patients with severe sepsis.
Diagnosis
The modified Duke criteria remains the cornerstone of diagnosis of IE. The criteria incorporate clinical findings, echocardiographic evidence and are supported by blood cultures, serological markers and bio-pathological evidence.
As discussed above, patients with TAVR-IE may have atypical symptoms that are not included in the modified Duke criteria. Echocardiographic findings may be negative or inconclusive. TEE in TAVR-IE may be negative or indeterminate. Prosthetic valve shadow may obscure smaller vegetations and smaller abscesses. This is because of the higher density of the prosthetic valve, which impedes the passage of ultrasound waves. The metallic and polymeric components of both mechanical and biologic valves do not transmit ultrasound waves and can lead to sub-optimal imaging due to acoustic shadowing. It may also be difficult to assess the severity and location of paravalvular aortic regurgitation with TAVR-IE because the anatomy and physiology of regurgitant jets differ from those in conventional valves.
Many cases in literature have shown patients who had TAVR-IE but had negative or inconclusive TEE [1,2,3,4]. For both of our patients, infective endocarditis was considered a high probability and TEE was done. TEE for the first patient showed moderately increased aortic regurgitation but no evidence of aortic root abscess or vegetation. The second patient had a well-functioning valve with trace aortic insufficiency and no evidence of vegetation or abscess.
Hence, although considered gold standard of diagnosis in IE related to native valve, TEE may be inconclusive in TAVR-IE and a negative TEE should not be used to rule out IE post TAVR [24, 25].
New diagnostic modalities
Multiple diagnostic modalities have been enumerated by the European Society of Cardiology for diagnosis of IE in prosthetic valves [5]. These include multi-slice CT, contrast enhanced multi-slice CT and 18F-FDG PET/CT (PET/CT after administration of fluorodeoxyglucose). This is emerging as a useful diagnostic tool in the diagnosis of infective endocarditis when TEE is negative or inconclusive [4, 26].
18F-FDG PET/CT is a relatively safe and non-invasive procedure with no absolute contraindications. It is safe to use in patients with renal failure, contrast allergy, and in patients with implantable cardiac devices. 18F-FDG is taken up in tissues with infection and inflammation and hence can focally tag infectious processes in the cardiac tissues. It can also show the extent of valve infection as well as extra-cardiac manifestations of IE.
18F-FDG PET/CT has shown higher efficacy than TEE in diagnosing prosthetic valve endocarditis [27, 28]. One meta-analysis showed a sensitivity of 80.5% when using 18F-FDG PET/CT in patients with prosthetic valve IE [29]. Another study showed that when analyzed specifically for IE in prosthetic valve, 18F-FDG PET/CT had 85% sensitivity [30]. A recent meta-analysis by Wang et al. [31] showed a pooled sensitivity of 0.86 (0.81–0.89, 60.0%) when the 18F-FDG PET/CT was analyzed for the sub-group of prosthetic valve endocarditis. Saby et al. showed that abnormal uptake of 18F-FDG in addition to the modified Duke criteria showed an increase in sensitivity of diagnosing prosthetic valve IE to up to 97% [32]. These studies indicate the usefulness of the PET/CT scan in patients with prosthetic valve endocarditis. The sensitivity of testing in patient’s irrespective of meeting modified Duke’s criteria is considerably high and can prevent catastrophic complications due to delay in diagnosis. Per European Society of Cardiology guidelines [5], 18F-FDG PET/CT should be considered in all patients with suspected PVE who have an inconclusive or negative TEE. However, this is currently limited to patients who received the prosthesis at least 3 months prior. This is a limitation as TAVR-IE usually presents early as discussed above.
Management and outcome
The mortality rate associated with TAVR-IE has been reported to be as high as 46% [24]. Complications include aortic root dissection, paravalvular and aortic root abscesses, intra/paravalvular regurgitation, stroke, and high rates of heart failure. A study showed a higher incidence of aortic root destruction when the time between symptom development and diagnosis was more than 14 days [33].
Patients presenting with TAVR-IE should be managed with a multi-disciplinary team including cardiology, cardiothoracic surgery, infectious disease and internal medicine. Timely diagnosis and early initiation of antibiotics, with possible surgery, may prevent catastrophic and fatal outcomes [2, 24]. While surgery with valve explantation is the definitive treatment of TAVR-IE [11, 13], many patients who have undergone TAVR have high surgical risk to begin with, and the risk further increases with IE. Hemodynamic instability may further preclude any surgical intervention and hence many patients are initially managed conservatively with a prolonged course of intravenous antibiotics. Broad spectrum antibiotics are recommended empirically as patients may not have typical microorganisms as the causative factor.
Conclusion
Through our case reports, we aim to raise awareness regarding the atypical symptoms that patients may present. A patient with previous TAVR may present with symptoms that do not meet the modified Duke’s criteria for diagnosis of infective endocarditis. The symptoms of fever, new heart failure, conduction defects, new arrhythmias and/or bacteremia with atypical organism, should raise high concern for IE. A negative TEE may result in delayed diagnosis and management. The addition of multi-modal imaging as an alternate to echocardiogram in the modified Duke’s criteria can help in early diagnosis. Per the ESC 2015 guidelines, 18F-FDG PET/CT is recommended as an alternate major criterion to TEE. However, this is limited to patients who had a prosthesis implanted at least 3 months prior and hence does not apply to a significant sub-set of the patients with TAVR-IE. Recent literature does show increased sensitivity of 18F-FDG PET/CT in all prosthetic valve endocarditis patients and should be considered in all patients who fail to meet modified Duke’s criteria.
Prosthetic aortic valve endocarditis carries high mortality and hence clinical suspicion should always supersede set criteria. There is a need for multi-center registries for TAVR-IE to broaden the scope for accurate and efficient diagnosis.
Availability of data and materials
Not applicable.
Abbreviations
- TAVR:
-
Transcatheter aortic valve replacement
- IE:
-
Infective endocarditis
- TAVR-IE:
-
Transcatheter aortic valve replacement associated infective endocarditis
- TEE:
-
Transesophageal echocardiogram
- MSSA:
-
Methicillin sensitive staphylococcus aureus
- PET/CT with 18F-FDG:
-
Positron emission tomography scan/computed tomography scan with administration of 18- fluorodeoxyglucose
- PVE:
-
Prosthetic valve endocarditis
- TTE:
-
Transthoracic echocardiogram
- EKG:
-
Electrocardiogram
- CPR:
-
Cardiopulmonary resuscitation
- ECMO:
-
Extracorporeal membrane oxygenation
- TAVI:
-
Transcatheter aortic valve implantation
- PARTNER II:
-
Placement of aortic transcatheter valves trial
- BMI:
-
Body mass index
- SAVR:
-
Surgical aortic valve replacement
References
Latib A, Naim C, De Bonis M, et al. TAVR-associated prosthetic valve infective endocarditis: results of a large, multicenter registry. J Am Coll Cardiol. 2014;64(20):2176–8. https://doi.org/10.1016/j.jacc.2014.09.021.
Amat-Santos IJ, Messika-Zeitoun D, Eltchaninoff H, et al. Infective endocarditis after transcatheter aortic valve implantation: results from a large multicenter registry [published correction appears in Circulation. 2020 Jun 2;141(22):e879]. Circulation. 2015;131(18):1566–74. https://doi.org/10.1161/CIRCULATIONAHA.114.014089.
Mangner N, Woitek F, Haussig S, et al. Incidence, predictors, and outcome of patients developing infective endocarditis following transfemoral transcatheter aortic valve replacement. J Am Coll Cardiol. 2016;67(24):2907–8. https://doi.org/10.1016/j.jacc.2016.03.588.
Salaun E, Sportouch L, Barral PA, et al. Diagnosis of infective endocarditis after TAVR: value of a multimodality imaging approach. JACC Cardiovasc Imaging. 2018;11(1):143–6. https://doi.org/10.1016/j.jcmg.2017.05.016.
Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075–128. https://doi.org/10.1093/eurheartj/ehv319.
Regueiro A, Linke A, Latib A, et al. Association between transcatheter aortic valve replacement and subsequent infective endocarditis and in-hospital death. JAMA. 2016;316(10):1083–92. https://doi.org/10.1001/jama.2016.12347.
Butt JH, Ihlemann N, De Backer O, et al. Long-term risk of infective endocarditis after transcatheter aortic valve replacement. J Am Coll Cardiol. 2019;73(13):1646–55. https://doi.org/10.1016/j.jacc.2018.12.078.
ClinicalTrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US). 2000 Feb 29 - . Identifier NCT01314313, The PARTNER II Trial: Placement of AoRTic TraNscathetER Valves—PII A (PARTNERII A); https://www.clinicaltrials.gov/ct2/show/results/NCT01314313?view=results. Accessed 14 Mar 2011.
Mylotte D, Andalib A, Thériault-Lauzier P, et al. Transcatheter heart valve failure: a systematic review. Eur Heart J. 2015;36(21):1306–27. https://doi.org/10.1093/eurheartj/ehu388.
López J, Revilla A, Vilacosta I, et al. Definition, clinical profile, microbiological spectrum, and prognostic factors of early-onset prosthetic valve endocarditis. Eur Heart J. 2007;28(6):760–5. https://doi.org/10.1093/eurheartj/ehl486.
Moriyama N, Laakso T, Biancari F, et al. Prosthetic valve endocarditis after transcatheter or surgical aortic valve replacement with a bioprosthesis: results from the FinnValve Registry. EuroIntervention. 2019;15(6):e500–7. https://doi.org/10.4244/EIJ-D-19-00247.
Prendergast BD, Redwood S, Cahill TJ. Infective endocarditis after TAVR. J Am Coll Cardiol. 2020;75(24):3031–2. https://doi.org/10.1016/j.jacc.2020.04.057.
Summers MR, Leon MB, Smith CR, et al. Prosthetic valve endocarditis after TAVR and SAVR: insights from the PARTNER trials. Circulation. 2019;140(24):1984–94. https://doi.org/10.1161/CIRCULATIONAHA.119.041399.
Van Mieghem NM, van der Boon RM, Nuis RJ, et al. Cause of death after transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2014;83(7):E277–82. https://doi.org/10.1002/ccd.24597.
Kuttamperoor F, Yandrapalli S, Siddhamsetti S, Frishman WH, Tang GHL. Infectious endocarditis after transcatheter aortic valve replacement: epidemiology and outcomes. Cardiol Rev. 2019;27(5):236–41. https://doi.org/10.1097/CRD.0000000000000244.
Olsen NT, De Backer O, Thyregod HG, et al. Prosthetic valve endocarditis after transcatheter aortic valve implantation. Circ Cardiovasc Interv. 2015;8(4): e001939. https://doi.org/10.1161/CIRCINTERVENTIONS.114.001939.
Puls M, Eiffert H, Hünlich M, et al. Prosthetic valve endocarditis after transcatheter aortic valve implantation: the incidence in a single-centre cohort and reflections on clinical, echocardiographic and prognostic features. EuroIntervention. 2013;8(12):1407–18. https://doi.org/10.4244/EIJV8I12A214.
Dapás JI, Rivero C, Burgos P, Vila A. Pseudomonas aeruginosa infective endocarditis following transcatheter aortic valve implantation: a note of caution. Open Cardiovasc Med J. 2016;10:28–34. https://doi.org/10.2174/1874192401610010028.
Tinica G, Tarus A, Enache M, et al. Infective endocarditis after TAVI: a meta-analysis and systematic review of epidemiology, risk factors and clinical consequences. Rev Cardiovasc Med. 2020;21(2):263–74. https://doi.org/10.31083/j.rcm.2020.02.68.
Gallouche M, Barone-Rochette G, Pavese P, et al. Incidence and prevention of infective endocarditis and bacteraemia after transcatheter aortic valve implantation in a French university hospital: a retrospective study. J Hosp Infect. 2018;99(1):94–7. https://doi.org/10.1016/j.jhin.2017.11.013.
Martínez-Sellés M, Bouza E, Díez-Villanueva P, et al. Incidence and clinical impact of infective endocarditis after transcatheter aortic valve implantation. EuroIntervention. 2016;11(10):1180–7. https://doi.org/10.4244/EIJY15M02_05.
Scisło P, Grodecki K, Wilimski R, et al. Different types of endocarditis after transcatheter aortic valve implantation. Echocardiography. 2019;36(6):1132–8. https://doi.org/10.1111/echo.14346.
Harding D, Cahill TJ, Redwood SR, Prendergast BD. Infective endocarditis complicating transcatheter aortic valve implantation. Heart. 2020;106(7):493–8. https://doi.org/10.1136/heartjnl-2019-315338.
Amat-Santos IJ, Ribeiro HB, Urena M, et al. Prosthetic valve endocarditis after transcatheter valve replacement: a systematic review. JACC Cardiovasc Interv. 2015;8(2):334–46. https://doi.org/10.1016/j.jcin.2014.09.013.
Bjursten H, Rasmussen M, Nozohoor S, et al. Infective endocarditis after transcatheter aortic valve implantation: a nationwide study. Eur Heart J. 2019;40(39):3263–9. https://doi.org/10.1093/eurheartj/ehz588.
Miranda WR, Connolly HM, Baddour LM, et al. Infective endocarditis following transcatheter aortic valve replacement: diagnostic yield of echocardiography and associated echo-Doppler findings. Int J Cardiol. 2018;271:392–5. https://doi.org/10.1016/j.ijcard.2018.03.124.
Prendergast BD. Diagnostic criteria and problems in infective endocarditis. Heart. 2004;90(6):611–3. https://doi.org/10.1136/hrt.2003.029850.PMID:15145855;PMCID:PMC1768277.
de Camargo RA, Sommer Bitencourt M, Meneghetti JC, et al. The role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in the diagnosis of left-sided endocarditis: native vs prosthetic valves endocarditis. Clin Infect Dis. 2020;70(4):583–94. https://doi.org/10.1093/cid/ciz267.
Mahmood M, Kendi AT, Ajmal S, et al. Meta-analysis of 18F-FDG PET/CT in the diagnosis of infective endocarditis. J Nucl Cardiol. 2019;26(3):922–35. https://doi.org/10.1007/s12350-017-1092-8.
Ricciardi A, Sordillo P, Ceccarelli L, et al. 18-Fluoro-2-deoxyglucose positron emission tomography-computed tomography: an additional tool in the diagnosis of prosthetic valve endocarditis. Int J Infect Dis. 2014;28:219–24. https://doi.org/10.1016/j.ijid.2014.04.028.
Wang TKM, Sánchez-Nadales A, Igbinomwanhia E, Cremer P, Griffin B, Xu B. Diagnosis of infective endocarditis by subtype using 18F-fluorodeoxyglucose positron emission tomography/computed tomography: a contemporary meta-analysis. Circ Cardiovasc Imaging. 2020;13(6): e010600. https://doi.org/10.1161/CIRCIMAGING.120.010600.
Saby L, Laas O, Habib G, et al. Positron emission tomography/computed tomography for diagnosis of prosthetic valve endocarditis: increased valvular 18F-fluorodeoxyglucose uptake as a novel major criterion. J Am Coll Cardiol. 2013;61(23):2374–82. https://doi.org/10.1016/j.jacc.2013.01.092.
Grubitzsch H, Tarar W, Claus B, Gabbieri D, Falk V, Christ T. Risks and challenges of surgery for aortic prosthetic valve endocarditis [published correction appears in Heart Lung Circ. 2020 Jun;29(6):e84]. Heart Lung Circ. 2018;27(3):333–43. https://doi.org/10.1016/j.hlc.2017.05.143.
Acknowledgements
Authors would like to acknowledge Ms. Helen Houpt, Medical Librarian at UPMC Pinnacle for her contributions in preparing this manuscript.
Funding
This manuscript did not receive any funding.
Author information
Authors and Affiliations
Contributions
KL, SA, SM—preparing the manuscript, literature review. HG, ANV—Manuscript review, corrections, literature updates. MM, DL, NJT—surgical input and information. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This manuscript has been approved by the Institutional Review Board of University of Pittsburgh Medical Center, Harrisburg, Pennsylvania.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
There are no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Video S1. There is a TAVR present. There is normal leaflet excursion without obvious vegetations. There is no obvious peri-aortic abscess. There is mild to moderate paravalvular insufficiency present.
Additional file 2: Video S2. There is a TAVR present. There is normal leaflet excursion without obvious vegetations. There is no obvious peri-aortic abscess. There is mild to moderate paravalvular insufficiency present.
Additional file 3: Video S3. There is a TAVR present. There is normal leaflet excursion without obvious vegetations. There is no obvious peri-aortic abscess. There is mild to moderate paravalvular insufficiency present.
Additional file 4: Video S4. Endocarditis seen in the CoreValve struts.
Additional file 5: Video S5. There is a bioprosthetic aortic valve present. Visualization of the bioprosthetic aortic valve was difficult. No vegetations were noted. There is no aortic insufficiency present.
Additional file 7.
TAVR Table references.
Additional file 8.
CARE checklist for Case 1.
Additional file 9.
CARE checklist for Case 2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lnu, K., Ansari, S., Mahto, S. et al. Transcatheter aortic valve replacement associated infective endocarditis case series: broadening the criteria for diagnosis is the need of the hour. BMC Cardiovasc Disord 21, 559 (2021). https://doi.org/10.1186/s12872-021-02364-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02364-0