Abstract
Introduction
Current evidence suggests that high sensitivity cardiac troponin-T (hs-cTnT) values differ based on sex, race, age, and kidney function. However, most studies examining the relationship of hs-cTnT and these individual factors are in healthy participants, leading to difficulty in interpreting hs-cTnT values in the Emergency Department (ED) setting. We seek to examine the relationship between hs-cTnT values and sex, race, age, and kidney function in a contemporary, urban academic setting.
Methods
ED visits from June 2018 through April 2019 with at least 1 hs-cTnT and no diagnosis of acute myocardial infarction (AMI) at an academic medical center in the south side of Chicago were retrospectively analyzed. Median hs-cTnT values were stratified by sex (male or female), race (African American or Caucasian), age, estimated glomerular filtration rate (eGFR), and stage of chronic kidney disease.
Results
9679 encounters, representing 7989 distinct patients, were included for analysis (age 58 ± 18 years, 59% female, 85% black). Males had significantly higher median hs-cTnT values than females (16 [8–34] vs. 9 [6–22] ng/L, p < 0.001), African Americans had a significantly lower median value than Caucasians (10 [6–24] vs. 15 [6–29] ng/L, p < 0.001), and those with atrial fibrillation (27 [16–48] vs. 9 [6–19] ng/L, p < 0.001) and heart failure (28 [14–48] vs. 8 [6–15] ng/L, p < 0.001) had higher median values than those without. Median hs-cTnT values increased significantly with increased age and decreased eGFR. All relationships continued to be significant even after multivariable regression of sex, age, race, eGFR, presence of atrial fibrillation, and presence of heart failure (p < 0.01).
Conclusions
Analysis of hs-cTnT in non-AMI patients during ED encounters showed that males have higher values than females, African Americans have lower values than Caucasians, those with atrial fibrillation and heart failure have higher values than those without, and that older age and lower eGFR were associated with higher median values.
Similar content being viewed by others
Introduction
Since the approval of the high-sensitivity cardiac troponin-T (hs-cTnT) assay by the US Food and Drug Administration in 2017 for clinical care, there has been renewed interest in determining blood concentrations in individuals without acute myocardial infarctions (AMI) [1, 2]. Studies have suggested that hs-cTnT levels vary by sex, race, age, and degree of kidney function [3,4,5,6]. However, many of these studies were conducted in healthy participants without other major comorbidities. As a result, clinicians often have difficulty interpreting hs-cTnT values in the setting of individual patient factors, such as older patients with chronic kidney disease (CKD) [7, 8]. Herein, we describe the ranges of hs-cTnT in Emergency Department (ED) visits across sex, race, age, estimated glomerular filtration rate (eGFR), and presence of heart failure or atrial fibrillation in patients without AMI during usual clinical care.
Materials and methods
Hs-cTnT values from all ED encounters from August 2018 through April 2019 at an academic medical center in the south side of Chicago were retrospectively analyzed. Patients with repeated encounters within 14 days, trauma, cardiac arrest, left ventricular assist devices (LVAD), history of heart transplant, patients without an eGFR value, and patients diagnosed with AMI during the encounter were excluded from analysis (Fig. 1). Sex and race were self-reported at the time of registration. All hs-cTnT tests were performed using the Roche Diagnostics Troponin T Gen 5 assay. Initial verification of the assay was performed on two separate Roche Cobas e602 analyzers. Further information regarding the analytical precision of the assay at various concentrations using three patient pools is provided in Additional file 1: sFigure1. The decision for hs-cTnT testing was based on individual clinician judgement using clinical history, the patient’s past medical history, and other clinical context. For each ED encounter, a single hs-cTnT was calculated as the median of all collected tests for the encounter. Unquantifiable hs-cTnT values were assigned a value of 6 ng/L (the limit of quantification). AMI diagnoses were determined by an associated International Classification of Disease version 10 (ICD-10) diagnosis of acute myocardial infarction (I21–I24) during the encounter. eGFR was calculated using the Modification of Diet in Renal Disease (MDRD) as described elsewhere [9]. End-stage renal disease (ESRD) was defined using ICD-10 codes and current procedural terminology (CPT) codes for dialysis. CKD stages was determined by eGFR cutoffs based on the National Kidney Foundation’s 2002 guidelines on the classification of CKD [10].
At our center, the protocol described by Vigen et al. [7] is used to rule out/in AMI in the ED. Briefly, hs-cTnT is drawn upon arrival in the ED; if the hs-cTnT value is < 6 ng/L and the symptom duration is ≥ 3 h, the patient rules out for AMI. If the initial hs-cTnT value is ≥ 6 and < 52 ng/L, or if the initial hs-cTnT value is < 6 ng/L and the symptom duration is < 3 h, a second hs-cTnT is drawn 1 h later. If this second hs-cTnT value is < 12 ng/L and the change from the initial hs-cTnT to the second hs-cTnT is < 3 ng/L, the patient rules out for AMI. If the second hs-cTnT value is ≥ 12 and < 52 ng/L and the change from the initial hs-cTnT to the second hs-cTnT is ≥ 5 ng/L, the result is considered abnormal and further clinical evaluation for likely AMI is undertaken by a cardiologist. If the second hs-cTnT value is ≥ 12 and < 52 ng/L and the change from the initial hs-cTnT to the second hs-cTnT is < 5 ng/L, or if the second hs-cTnT value is < 12ng/L but the change from the initial hs-cTnT to the second hs-cTnT is ≥ 3 ng/L, a third hs-cTnT is drawn 2 h later (3 h after the initial draw). If the change from the initial hs-cTnT to the third hs-cTnT is < 7 ng/L, the patient rules out for AMI. If the change is ≥ 7 ng/L, the result is considered abnormal and further clinical evaluation for likely AMI is undertaken by a cardiologist. Finally, any hs-cTnT value ≥ 52 ng/L is considered abnormal and further clinical evaluation for likely AMI is undertaken by a cardiologist. The cutoff values for hs-cTnT in this protocol are the same for both male and female patients. For patients considered likely for AMI, the cardiologist then uses a combination of electrocardiographic and laboratory data and findings on history and physical examination to make or exclude the clinical diagnosis of AMI.
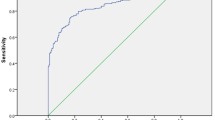
Continuous baseline clinical variables were expressed as means ± standard deviations or medians with interquartile ranges (IQR) if non-normally distributed. Categorical baseline clinical variables were expressed as counts and percentages. Missing data was excluded. Outlier data was removed prior to percentile (%tile) analysis (Table 1). Outliers were considered 1.5 times the IQR. Median hs-cTnT values were compared using Mann-Whitney U test with a two-tailed p-value < 0.05 being statistically significant for all analyses. Each point on the scatter plots represents the median hs-cTnT value of all encounters within the specified x-value. Spearman’s rank correlation coefficients were used to determine the associations between hs-cTnT to age and eGFR. All analyses and visualizations were performed with ‘Tidyverse’, ‘data.table’, and ‘sjPlot’ packages in R 4.0.2 (R Core Team 2020). The University of Chicago Institutional Review Board (IRB) reviewed and approved the study (IRB 17-0324). All methods were carried out in accordance with relevant guidelines and regulations.
Results
11,389 individual ED encounters were collected. 9679 encounters, representing 7989 distinct patients, were included for analysis (Fig. 1). Mean age was 57.8 ± 17.6 years, 59.3% were female, 85.0% were Black (Table 2). The median hs-cTnT across all included encounters was 12.0 [IQR 6.0–29.5] ng/L. 3,061 (31.6%) encounters had median hs-cTnT values at or below the limit of quantification. Males had significantly higher median hs-cTnT values than females (16 [8–34] vs. 9 [6–22] ng/L, p < 0.001, Fig. 2a), African Americans had a significantly lower median value than Caucasians (10 [6–24] vs. 15 [6–29] ng/L, p < 0.001, Fig. 2b), and those with atrial fibrillation (27 [16–48] vs. 9 [6–19] ng/L, p < 0.001) and heart failure (28 [14–48] vs. 8 [6–15] ng/L, p < 0.001) had higher median values than those without (Table 1). All relationships continued to be significant even after multivariable regression of sex, age, race, eGFR, presence of atrial fibrillation, and presence of heart failure (p < 0.01).
Patients older than or equal to 65 years had significantly higher median troponin values (20 [11–34] ng/L) compared with those between 50 and 64 years (10 [6–19] ng/L, p < 0.001) and patients less than 50 years (6 [6–7] ng/L, p < 0.001). Median hs-cTnT were at the level of detection until age 40 at which point a direct linear relationship existed between age and median troponin value (Fig. 2c, r = 0.48 [95% CI 0.47–0.50], p < 0.001). This relationship remained even during sub-group analysis of encounters where eGFR was ≥ 90 mL/min/1.73 m2 (r = 0.50 [95% CI 0.47–0.53], p < 0.001, Fig. 2).
The median hs-cTnT value of patients without CKD was 6 [6–9] ng/L which was significantly lower when compared to stage 2 CKD (10 [6–17] ng/L), stage 3 CKD (22 [13–35] ng/L), stage 4 CKD (44 [28–70] ng/L), stage 5 CKD (66 [43–110] ng/L), and in patients with ESRD (96 [62–152] ng/L). An inverse exponential relationship existed between eGFR and median hs-cTnT (Fig. 2d, r = − 0.61 [95% CI − 0.62 to -0.60], p < 0.001).
hs-cTnT values at the 25th, 50th, 75th, and 99th percentiles for age, sex, race, and CKD subgroups are presented in Tables 1 and 3.
Discussion
ED encounters from a large, tertiary, academic medical center showed that hs-cTnT values differed considerably by sex, race, age, CKD stage, and presence of atrial fibrillation and heart failure in patients without AMI. Our results from routine clinical care of non-AMI patients support data from healthy participants indicating that males have higher hs-cTnT values than females [2, 4, 5]. Our results indicate that these relationships exist across race and eGFR strata. Of note, the manufacturer-recommended 99th percentiles are 19 ng/L for a US population, 14ng/L for US females, and 22 ng/L for US males. There are no manufacturer recommendations for 99th percentiles by race, age, or CKD stage.
It has also been shown in healthy cohorts that older individuals have higher troponin values than younger individuals [5]. It appears from Fig. 2c that this relationship exists from age 45–85. Age and median hs-cTnT does not appear to have a relationship at the extremes of age (Fig. 2c). While eGFR is also related to age, when controlling for eGFR by analyzing only those without CKD, a similar relationship between age and median hs-cTnT was observed. The pathophysiology behind this phenomenon is unclear but it is likely a combination of both physiology and pathology, such as higher rates of co-morbidities [4].
The relationship between race and hs-cTnT is even less clear in the literature. Data from healthy participants have shown multiple different relationships with some studies suggesting no difference or lower hs-cTnT levels in African Americans compared with Caucasians whereas others have seen increased levels of hs-cTnT in African Americans [2, 5]. A sub-study of the Dallas Heart Study (DHS), a multiethnic, population cohort of residents in Dallas County, showed that black women had higher hs-cTnT levels but after adjustment this relationship disappeared [11]. Our results from an unprecedented percentage of African Americans (85%) show that hs-cTnT levels are lower in African American patients than Caucasian patients. The literature is sparse as to the biologic mechanism by which race would play a role in hs-cTnT concentrations. Interestingly, whites in our study had higher rates of atrial fibrillation and coronary artery disease but lower rates of diabetes, hypertension, and kidney disease (Additional file 1: sTable 2). It is possible that there is no true physiologic reason for these differences and rather a confounder remains unaccounted. However, we believe the racial differences remain an important finding particularly given the disparities in AMI diagnosis between races and should be further studied.
Previous studies have shown that hs-cTnT is inversely related to eGFR [12]. While the exact pathophysiology is unknown, it is thought to be a combination of kidney disease-related subclinical cardiac damage with a minor contribution of impaired renal clearance of cTnT fragments by the kidney membrane [13]. There is still unclear guidance on how to interpret hs-cTnT values in the setting of kidney disease. Our results from a large number of hs-cTnT values in patients without AMI during routine clinical care indicate an inversely exponential relationship between eGFR and median hs-cTnT. When broken down by stage of CKD, it appears that the median hs-cTnT of the CKD stage group doubles until CKD5 and ESRD where a 50% increase is observed for each progressive CKD stage (Table 1).
Our study has a number of notable strengths. First, we include a large number of patients in the setting of routine clinical care. We believe this is a more clinically relevant population to study as opposed to many other studies which have attempted to characterize troponin values in the setting of healthy cohorts. Second, our study included 85% African Americans. These numbers allow for unprecedented insight into an often under-represented minority in clinical research. Lastly, because of the heterogenous nature of our patient population, we were able to characterize a large range of ages and eGFR including over 600 patients who were on chronic dialysis.
Several limitations should be noted. We recognize exclusion based on ICD codes for AMI is likely incomplete due to mis-classification. In addition, while we excluded patients with AMI, there are patients in our study with conditions that are also known to cause elevations in cardiac troponins (i.e.: pulmonary embolism, myocarditis). As our study described hs-cTnT values in a diverse ED population, it was beneficial to include all conditions except AMI where hs-cTnT change and rate of rise are important diagnostic information. Second, the 99th percentile values in certain sub-groups should be examined with caution as some of the Caucasian groups have low numbers (i.e.: less than 100). Also, the staging of chronic kidney disease based on a single creatinine value taken at the time of acute illness is likely to overestimate the severity of kidney disease. However, data in the context of a single eGFR is more generalizable as clinicians are often required to interpret troponin levels with a single data point.
We chose to use a median value of hs-cTnT across the encounter to give a global representation of hs-cTnT within an encounter. Mean values would be skewed due to the non-normal distribution of hs-cTnT and the maximum values would not be as useful to clinicians in the context of non-AMI patients. While serial testing of hs-cTnT may affect median values, we do not think that this is a major limitation as we excluded patients with AMI and thus most patients would have values that remained stable. It is also worth mentioning that the diagnosis of AMI requires a combination of clinical context and changes in hs-cTnT values over time. Our institution utilizes the rule-out method suggested by Vigen et al. prior to an expert clinician (both a hospital medicine clinician and/or a licensed cardiologist) making the diagnosis of AMI(7). Despite the exclusion of all patients with a diagnosis of AMI from analysis, residual confounders likely remain. Specifically, some patients that were included may have had AMI even though they were not classified as such and some excluded patients did not have AMI. However, our study is focused more on the expected ranges of hs-cTnT values observed in a standard ED population as opposed to making a diagnosis of AMI. It is also worth noting that we excluded outliers in our main analysis as our dataset included extreme values (i.e. > 10,000 ng/L), beyond the measuring limit of our assay. Since it was not possible to determine if these values were due to error, we felt it most appropriate to exclude them. Additionally, hs-cTnT values at the extreme limits are difficult to interpret without clinical context. However, we have also provided data on percentiles without outliers excluded in Additional file 1: sTable 3 and Additional file 1: sTable 4. Finally, it is very important to further stress and acknowledge that myocardial injury is common in hospitalized patients. The population in this study is likely to include substantial numbers of patients with cardiac ischemia in the context of multiple systemic and cardiac conditions other than AMI. This will have implications on the presented results, and consequently the 99th percentile values reported here should not be considered as informative for the clinical diagnosis of AMI in any of the subgroups reported.
Analysis of hs-cTnT in non-AMI patients during routine clinical care at a large, diverse tertiary ED in a contemporary US population showed that males have higher hs-cTnT values than females, African Americans have lower values than Caucasians, older age was associated with higher values, and lower eGFR was associated with higher values. These results suggest that these patient specific factors should be incorporated into the interpretation of hs-cTnT values.
Availability of data and materials
A de-identified dataset generated and used during the current study can be made available from the corresponding author on request and with approval from the IRB at the University of Chicago.
Abbreviations
- hs-cTnT:
-
High-sensitivity cardiac troponin-T
- AMI:
-
Acute myocardial infarctions
- ED:
-
Emergency Department
- eGFR:
-
Estimated glomerular filtration rate
- MDRD:
-
Modification of Diet in Renal Disease
- ESRD:
-
End-stage renal disease
- IQR:
-
Interquartile ranges
- CPT:
-
Current procedural terminology
- CKD:
-
Chronic kidney disease
- LVAD:
-
Left ventricular assist devices
- IRB:
-
Institutional Review Board
References
Reichlin T, Hochholzer W, Bassetti S, Steuer S, Stelzig C, Hartwiger S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med. 2009;361(9):858–67.
Fitzgerald RL, Hollander JE, Peacock WF, Limkakeng AT, Breitenbeck N, Rivers EJ, et al. The 99th percentile upper reference limit for the 5th generation cardiac troponin T assay in the United States. Int J Clin Chem. 2020;504:172–9.
Freda BJ, Tang WH, Van Lente F, Peacock WF, Francis GS. Cardiac troponins in renal insufficiency: review and clinical implications. J Am Coll Cardiol. 2002;40(12):2065–71.
Gore MO, Seliger SL, Defilippi CR, Nambi V, Christenson RH, Hashim IA, et al. Age- and sex-dependent upper reference limits for the high-sensitivity cardiac troponin T assay. J Am Coll Cardiol. 2014;63(14):1441–8.
Greene DN, Leong TK, Collinson PO, Kamer SM, Huang K, Lorey TS, et al. Age, sex, and racial influences on the Beckman Coulter AccuTnI+3 99th percentile. Clin Chim Acta Int J Clin Chem. 2015;444:149–53.
Olivieri F, Galeazzi R, Giavarina D, Testa R, Abbatecola AM, Ceka A, et al. Aged-related increase of high sensitive Troponin T and its implication in acute myocardial infarction diagnosis of elderly patients. Mech Ageing Dev. 2012;133(5):300–5.
Vigen R, Kutscher P, Fernandez F, Yu A, Bertulfo B, Hashim IA, et al. Evaluation of a novel rule-out myocardial infarction protocol incorporating high-sensitivity troponin T in a US hospital. Circulation. 2018;138(18):2061–3.
Azar RR, Sarkis A, Giannitsis E. A practical approach for the use of high-sensitivity cardiac troponin assays in the evaluation of patients with chest pain. Am J Cardiol. 2021;139:1–7.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–70.
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–47.
Hackler E 3, Lew J, Gore MO, Ayers CR, Atzler D, Khera A, et al. Racial differences in cardiovascular biomarkers in the general population. J Am Heart Assoc. 2019;8(18):e012729.
Guclu T, Bolat S, Senes M, Yucel D. Relationship between high sensitivity troponins and estimated glomerular filtration rate. Clin Biochem. 2016;49(6):467–71.
Diris JH, Hackeng CM, Kooman JP, Pinto YM, Hermens WT, van Dieijen-Visser MP. Impaired renal clearance explains elevated troponin T fragments in hemodialysis patients. Circulation. 2004;109(1):23–5.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
NK and CET conceived the study. CET provided the data. RFMC, SAB, and LH performed the data analyses. SN, TFS, and XMRvW provided technical assistance. NK, CET, SAB, SN, TFS, and XMRvW interpreted the data. NK wrote the manuscript. All authors approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the IRB at the University of Chicago under a general waiver of consent.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: sFigure 1
. Imprecision (% CV) at various levels of hs-cTnT during initial verification. Three patient pools are measured on two Roche Cobas e602 analyzers once per day for 20 days (40 points per pool). 10% CV is estimated at 11 ng/L cTnT. sTable 1. The top 10 reasons for emergency department visits by number of encounters. sTable 2. Baseline demographics by race, aggregated on the patient level. For repeated encounters, only the first patient encounter was used. Categorical variables expressed as count (percent). Normally distributed continuous variables expressed as mean (standard deviation), non-normally distributed continuous variables expressed as mean [inter-quartile range]. sFigure 2. Scatter plot of BMI and high sensitivity cardiac troponin T. Negative weak correlation. sFigure 3. Scatter plot of age with only encounters where eGFR ≥ 90 mL/min/1.73 m2. sTable 3. hs-cTnT values at the 25th, 50th, 75th, and 99th percentiles stratified by sex, race, age group, CKD stage, history of atrial fibrillation, history of heart failure without removing outliers. Results are aggregated at the encounter level. sTable 4. hs-cTnT values at the 25th, 50th, 75th, and 99th percentiles stratified by multiple subgroups without outliers removed. Results are reported aggregated at the encounter level.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kong, N., Chua, R.F.M., Besser, S.A. et al. A retrospective analysis of high sensitivity cardiac troponin-T ranges in non-myocardial infarction emergency department visits. BMC Cardiovasc Disord 21, 283 (2021). https://doi.org/10.1186/s12872-021-02089-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02089-0