Abstract
Background and aims
Liver enzymes, including alanine aminotransferase (ALT) and aspartate aminotransferase (AST), are markers of hepatic dysfunction and fatty liver disease. Although ALT and AST have been suggested as risk factors for cardiovascular disease, their role as predictors of mortality after acute myocardial infarction (AMI) has not been established. The objective of this study was to investigate the predictive value of ALT and AST for mortality in patients with AMI.
Methods
We analyzed records of 712 patients with AMI and no known liver disease treated at the Department of Cardiovascular Center in the First Hospital of Jilin University. The primary outcome was all-cause in-hospital mortality. Relationships between primary outcome and various risk factors, including serum transaminase levels, were assessed using multivariate logistic regression analysis.
Results
Age (P < 0.001), hypertension (P = 0.034), prior myocardial infarction (P < 0.001), AST (P < 0.001), ALT (P < 0.001), creatinine (P = 0.007), blood urea nitrogen (P = 0.006), and troponin I (P < 0.001) differed significantly between ST-segment elevation myocardial infarction (STEMI) and non-STEMI. The following factors were associated with an increased risk of in-hospital all-cause mortality in patients with AMI: ALT ≥ 2ULN (adjusted odds ratio [AOR] 2.240 [95% confidence interval (CI), 1.331–3.771]; P = 0.002); age ≥ 65 year (AOR 4.320 [95% CI 2.687–6.947]; P < 0.001); increased fasting plasma glucose (FPG) (AOR 2.319 [95% CI 1.564–3.438]; P < 0.001); elevated D-dimer (AOR 2.117 [95% CI 1.407–3.184]; P < 0.001); elevated fibrinogen (AOR 1.601 [95% CI 1.077–2.380]; P = 0.20); and reduced estimated glomerular filtration rate (eGFR) (AOR 2.279 [95% CI 1.519–3.419]; P < 0.001).
Conclusions
Our findings demonstrated that elevated ALT was independently associated with increased in-hospital all-cause mortality in patients with AMI. Other risk factors were increased age, FPG, D-dimer, and fibrinogen and decreased eGFR.
Similar content being viewed by others
Introduction
Coronary atherosclerotic disease (CAD) is the main source of cardiovascular disease (CVD), causing more than 7 million deaths worldwide each year. In recent decades, there have been substantial declines in cardiovascular disease mortality across much of Europe [1]. The latest guidelines from the European Heart Association, published in 2019, indicate that CAD is a pathologic process characterized by atherosclerotic plaque accumulation in the epicardial arteries, which is either obstructive or non-obstructive [2]. Acute coronary syndrome (ACS) refers to an acute ischemic syndrome of the heart caused by new thrombosis secondary to rupture or erosion of an unstable coronary artery atherosclerotic plaque. It includes unstable angina and acute myocardial infarction (AMI), either ST-segment elevation myocardial infarction (STEMI) or non-STEMI (NSTEMI).
AMI is associated with high morbidity and mortality. Mortality is influenced by many factors, including advanced age, smoking status, and the presence of hypertension, diabetes mellitus (DM), dyslipidemia, or obesity. Elevated levels of liver transaminases, specifically alanine aminotransferase (ALT) and aspartate aminotransferase (AST), are used as markers of hepatic dysfunction and have attracted attention as emerging risk factors for CVD.
Recent studies have investigated the role of liver transaminases as independent predictors of cardiac-related morbidity and mortality [3, 4]. Several prospective epidemiologic studies have suggested that hepatic dysfunction is common in cardiac disease [5, 6]. When no other causes of liver injury are identified, elevations of liver aminotransferases are associated with an elevated risk of cardiac-related mortality [7]. The goal of this study was to evaluate the association between elevated liver transaminases and in-hospital all-cause mortality in patients with AMI.
Methods
Study population
A population-based retrospective case–control study was conducted in the First Hospital of Jilin University, Changchun City, Jilin Province. General characteristics and routine laboratory tests of patients diagnosed with AMI were screened to identify patients for inclusion in the study. A total of 712 patients were included in the study (Fig. 1). Baseline demographic data, medical history, laboratory data, and clinical data during hospitalization were retrieved from our departmental heart disease electronic database (Table 1) and all methods were performed in accordance with the relevant guidelines and regulations.
Definitions
The diagnostic criteria for AMI were in accordance with the 2017 guidelines from the European Society of Cardiology (ESC) [8]. Myocardial injury was defined as at least one cardiac troponin value above the 99th percentile upper reference limit. STEMI was defined as persistent chest discomfort or other symptoms suggestive of ischemia and ST-segment elevation in at least two contiguous leads. Ischemic symptoms in the absence of ST-segment elevation at presentation were designated as NSTEMI [8]. Hypoxic liver injury (HLI) was defined as at least one serum transaminase level more than twice the upper limit of normal (ULN). The ULN for ALT was defined as 50 U/L for men and 40 U/L for women, whereas the ULN for AST was defined as 40 U/L for men and 35 U/L for women. The World Health Organization (WHO) defines impaired fasting glucose as a fasting plasma glucose (FPG) value of 6.1 mmol/L or higher, whereas the American Diabetes Association recommends a cutoff value of 5.6 mmol/L [9]. In this study, we used the WHO cutoff value. Estimated glomerular filtration rate (eGFR) was calculated as 175 × plasma creatinine–1.234 × age–0.179 × 0.79 if female [10]. Elevated D-dimer level was defined as a serum concentration ≥ 400 ng/mL and increased fibrinogen was defined as a serum concentration ≥ 3.5 g/L.
Exclusion criteria
Patients with incomplete data were excluded from the study. We also excluded patients with elevated transaminases for various non-AMI reasons, including hepatitis and hepatic cirrhosis, chronic schistosomiasis, hepatobiliary obstructive disease, bone disease, pancreatitis; cardiomyopathy, severe heart failure, severe renal insufficiency, and infectious diseases. It is well known that hyperlipidemia and fatty liver disease are risk factors for CVD. Patients diagnosed with fatty liver disease were not excluded from our study, but we did exclude patients with liver dysfunction attributed to fatty liver disease.
Laboratory data
Peripheral blood samples obtained at the time of admission were tested for the following: complete blood count, creatinine, cardiac troponin I (Tn I), creatine kinase MB (CK-MB), myoglobin, potassium, sodium, brain natriuretic peptide (BNP), prothrombin time (PT), PT activity (PTA), fibrinogen, and D-dimer. Total cholesterol (TC), triglycerides, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), FPG, ALT, AST, alkaline phosphatase (ALP), γ-glutamyl transpeptidase (GGT), cholinesterase, albumin, total bilirubin (T-Bil), and direct bilirubin (D-Bil) were measured after 12 h of fasting following admission. All blood samples obtained at the time of admission were analyzed in the certified laboratory department of First Hospital of Jilin University.
Statistical analysis
All data analysis was performed using SPSS version 22.0, and P < 0.05 indicated statistical significance. Continuous variables were represented by the median (25th and 75th percentiles) or mean ± standard deviation. Categorical data were described by counts and percentages. Continuous variables were compared using two-tailed independent sample t-tests, and categorical variables were compared using the chi-square test. Multivariate logistic regression models were used to identify risk factors for mortality in patients with AMI. These models included adjustments for potential confounding variables, and adjusted odds ratios (AORs) and 95% confidence intervals (CIs) were calculated. The logistic refression models were calibrated by Hosmer–Lemeshow test.
Results
Demographic and clinical characteristics
Baseline demographic and clinical characteristics of the 714 patients included in the study are shown in Table 1. Of the 474 patients with STEMI, 327 were male, 147 were female, and the median age was 65.0 years. In this group, 270 patients (57.0%) had a smoking history, 133 (28.1%) had a history of drinking alcohol, 247 (52.1%) had hypertension, 135 (28.5%) had DM, 47 (9.9%) had a prior myocardial infarction, and 72 (15.2%) had a prior cerebral infarction. Of the 238 patients with NSTEMI, 153 were male and 85 were female, with a median age of 67.0 years. In this group, 138 patients (58.0%) had a smoking history, 67 (28.2%) had a history of drinking alcohol, 144 (60.5%) had hypertension, 81 (34.0%) had DM, 52 (21.8%) had a previous myocardial infarction, and 27 (11.3%) had a prior cerebral infarction.
Patients with NSTEMI were older and more likely to have DM than those in the STEMI group. AST, ALT, white blood cell count, neutrophil count, Tn I, myoglobin, CK-MB, and in-hospital mortality were also higher in the STEMI group than in the NSTEMI group.
Factors associated with in-hospital mortality in all patients
Multivariate logistic regression analysis was used to identify risk factors for in-hospital mortality in all 712 patients with AMI (Table 2). Age, sex, DM, smoking history, FPG, TC, triglycerides, AST, ALT, GGT, Tn I, D-dimer, fibrinogen, and eGFR were included in the multivariate analysis. Study participants with an ALT ≥ 2 ULN had an AOR of 2.240 (95% CI 1.331–3.771; P = 0.002), when compared with patients with an ALT < 2 ULN. Other factors associated with an increased odds of in-hospital mortality were age ≥ 65 years (AOR 4.320 [95% CI 2.687–6.947]; P < 0.001); FPG (AOR 2.319 [95% CI 1.564–3.438]; P < 0.001); decreased eGFR (AOR 2.279 [95% CI 1.519–3.419]; P < 0.001); elevated fibrinogen (AOR 1.601 [95% CI 1.077–2.380]; P = 0.020); and elevated D-dimer (AOR 2.117 [95% CI 1.407–3.184]; P < 0.001).
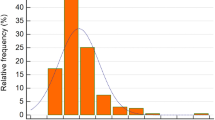
Figures 2, 3 and 4 show the differences in mortality rates according to age, ALT, and eGFR subgroups for the entire study population. These figures clearly illustrate the increase in mortality with increasing age and ALT and decreasing eGFR.
In-hospital mortality rates of patients with acute myocardial infarction categorized by age at presentation. There were 42, 167, 322, 167, and 14 patients in the ≤ 44 year, 45–59 year, 60–74 year, 75–89 year, and ≥ 90 year age groups, respectively. The corresponding mortality rates for each group were 7.1%, 10.8%, 21.1%, 55.1%, and 75.6%
In-hospital mortality rates of patients with acute myocardial infarction categorized by estimated glomerular filtration rate (eGFR) at presentation. There were 11, 25, 88, and 150 patients in the < 15, 15–30, 30–60, and 60–90 mL/min/17.3 m2 eGFR groups, respectively. The corresponding mortality rates for each group were 90.0%, 81.0%, 56.8%, and 32.0%
In-hospital mortality rates of patients with acute myocardial infarction categorized by alanine aminotransferase (ALT) concentration at presentation. There were 212, 70, and 65 patients in the upper limit of normal (ULN)–2 ULN, 2 ULN–3 ULN, and ≥ 3 ULN ALT groups, respectively. The corresponding mortality rates for each group were 17.5%, 24.3%, and 53.8%
Factors associated with in-hospital mortality according to type of myocardial infarction
Multivariate logistic regression analysis was used to identify risk factors for all-cause in-hospital death in 474 patients with STEMI and 238 patients with NSTEMI (Tables 3 and 4). Factors included in the multivariate analysis were the same as those included when analyzing all study participants. Patients with an ALT ≥ 2 ULN had a higher risk of in-hospital mortality in both the STEMI and NSTEMI groups (AOR 1.915 [95% CI 1.028–3.565] and AOR 3.698 [95% CI 1.302–10.500], respectively; P < 0.001 for both). Other factors associated in-hospital mortality in both the STEMI and NSTEMI groups were age ≥ 65 year (AOR 4.668 [95% CI 2.684–8.117] and AOR 2.753 [95% CI 1.053–7.199], respectively); FPG (AOR 2.010 [95% CI 1.236–3.267] and AOR 3.823 [95% CI 1.820–7.808], respectively; P < 0.001 for both); and elevated D-dimer (AOR 1.937 [95% CI 1.175–3.194] and AOR 3.053 [95% CI 1.471–6.334], respectively). Elevated fibrinogen was associated with an increased odds of in-hospital mortality in patients with STEMI (AOR 1.810 [95% CI 1.113–2.944]; P = 0.017), but not in patients with NSTEMI.
Discussion
One of the most important factors associated with an increased risk of in-hospital mortality in patients with an AMI was an elevated ALT. The liver is a vital organ that is very sensitive to hemodynamic changes because of its complex vascular system and high metabolic activity [11]. Every 10-mm Hg decrease in arterial blood pressure decreases hepatic arterial blood flow by approximately 10% [12]; therefore, abnormal serum transaminases are often observed in patients with AMI. A few recent studies reported that elevated serum transaminases were independently associated with poor clinical outcomes in patients with AMI. The extent of liver injury, in particular in patients with preexisting metabolic syndrome, may have a direct impact on cardiac outcomes [13].
Hypoxic liver injury (HLI) is commonly diagnosed in the emergency room in patients with STEMI (in 22% of patients), and those patients with HLI have higher mortality rate and higher frequency of major adverse cardiovascular events (MACE) after percutaneous coronary intervention [14]. Using multivariable regression analysis, Jantti et al. reported that a > 20% increase in ALT was associated with an increased risk of 90-day mortality independent of other known risk factors [15]. However, the association between liver transaminases and CVD remains a subject of debate. Authors of a narrative review based on prospective data concluded that the available evidence did not support a linear relationship between ALT and CVD events [16]. Differences in the effects of specific aminotransferases have not been clearly elucidated and require further research.
A few potential mechanisms have been proposed to explain the association between elevated ALT levels and increased in-hospital all-cause mortality in patients with AMI. For example, the liver has high metabolic activity and perfusion rates, and acute circulatory changes, such as AMI-related hypotension, will directly influence hepatic blood flow and thereby increase ALT and AST. Liver transaminases may also be elevated because of hepatic congestion from acute right ventricular dysfunction. Current research suggests that venous congestion, reduced capability of hepatocytes to extract oxygen, and reperfusion injury are of particular importance [12]. Although the source of elevated serum transaminases might be ischemic myocardial tissue, increased levels of these enzymes often reflect HLI secondary to both impaired forward perfusion and passive backward congestion, which are prevalent during STEMI [6]. In addition, an analysis of asymptomatic individuals found that increased levels of serum ALT (even high-normal levels) were associated with markers of CVD [17]. It is known that incomplete peripheral lipolysis of very low–density lipoprotein (VLDL) particles over-enriched with triglycerides increases the number of small dense LDL (sdLDL) particles, which carry a disproportionately large amount of LDL-C [17,18,19]. ALT levels are directly related to desmosterol: TC ratio, a marker of cholesterol synthetic activity [20], thereby suggesting that ALT elevations are associated with increased hepatic triglyceride and cholesterol output in VLDL particles and lead to increased production of sdLDL [17].
In this study, we found that increased patient age was also significantly associated with mortality, which is consistent with previous reports of higher mortality in elderly patients with AMI [21,22,23]. In the CADILLAC trial, both cardiac and noncardiac causes of death were more frequent in older patients [21]. Myocytes are continuously lost as the heart ages, and senescent cells exhibit increased susceptibility to microvasculature reperfusion injury. D-dimer, one of the degradation products of fibrin, is produced when fibrinolytic enzymes degrade fibrin clots produced by thrombin. Choi et al. reported that in STEMI patients undergoing primary percutaneous coronary intervention, high D-dimer levels on admission were associated with a larger myocardial infarction size [24]. In the current study, higher D-dimer levels were associated with higher all-cause in-hospital mortality in patients with AMI; this finding is consistent with the results reported by Kikkert et al. [25].
In the current study, another important predictor of early mortality in patients with AMI was reduced eGFR. A previous study reported that among patients with AMI, any degree of preexisting renal impairment should be considered a potent, independent, and easily identifiable risk factor for cardiovascular complications, with each 10-unit reduction in eGFR being associated with a 10% increased risk for death and nonfatal cardiovascular outcomes [26]. In general, patients with chronic kidney disease have more cardiovascular risk factors and a higher incidence of MACE with AMI and acute kidney injury (AKI) was revealed to be an independent long-term prognostic indicator in patients with STEMI [27]. Even small, subclinical elevations of serum creatinine that do not fulfil the consensus criteria for acute kidney injury have been independently associated with a twofold increased risk of adverse in-hospital outcomes after AMI [28]. Our findings suggested that serum eGFR was an independent predictor of in-hospital all-cause mortality after AMI, with mortality increasing as eGFR decreased. Various factors associated with impaired renal function, such as insulin resistance, oxidative stress, inflammation, endothelial dysfunction, vascular calcifications, and hypercoagulability, may contribute to adverse outcomes in patients with ACS [29].
The 2019 ESC guidelines regarding diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the European Association for the Study of Diabetes concluded that patients with DM and established CVD have very high cardiovascular risk [30]. Our findings that elevated FPG, but not DM, was associated with mortality suggest that glycemic control is the critical determinant of the risk of death. Previous studies have shown that severe hyperglycemia on admission was associated with increased in-hospital mortality in AMI patients with or without DM [31, 32]. Hyperglycemia can induce abnormalities in endothelial and vascular smooth muscle cell function, as well as a propensity to thrombosis, thereby contributing to atherosclerosis and its complications [33], as well as hypercoagulability and impaired fibrinolysis [34].
This study had several limitations. As a retrospective study, it relied on the accuracy of data in the medical records. It was also based on data from a single center, whose population consisted primarily of a single ethnic group of individuals located in Northeast China. Because of the climate, diet, and other factors, the incidence of cardiovascular disease in this region is significantly higher than in other regions, and the data may not reflect a general population of patients with AMI. Furthermore, although we excluded patients diagnosed with and treated for various liver diseases (including hepatobiliary malignancies, liver fibrosis and cirrhosis, and viral hepatitis) based on medical records, some factors potentially affecting transaminase levels, such as undiagnosed liver disease or medications affecting liver function, may have remained undetected and therefore not been considered when excluding patients.
Conclusions
This retrospective study focused on non-invasive markers of in-hospital death from any cause after AMI. Increased risk of in-hospital all-cause mortality was significantly associated with increased levels of ALT, older age, FPG, D-dimer, and fibrinogen and decreased eGFR. Our results therefore suggest that elevation of the serum transaminase ALT, which likely reflects HLI, may be a useful marker of increased risk of early mortality in patients with AMI.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on request.
Abbreviations
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase;
- AST:
-
Aspartate aminotransferase
- BNP:
-
Brain natriuretic peptide
- BUN:
-
Blood urea nitrogen
- CK-MB:
-
Creatine kinase MB
- CVD:
-
Cardiovascular disease
- D-Bil:
-
Direct bilirubin
- FPG:
-
Fasting plasma glucose
- GGT:
-
γ-Glutamyl transpeptidase
- HDL-C:
-
High-density lipoprotein cholesterol
- INR:
-
International normalized ratio
- LDL-C:
-
Low-density lipoprotein cholesterol
- MI:
-
Myocardial infarction
- NSTEMI:
-
Non–ST-segment elevation myocardial infarction
- PT:
-
Prothrombin time
- PTA:
-
Prothrombin time activity
- RBC:
-
Red blood cell
- STEMI:
-
ST-segment elevation myocardial infarction
- T-Bil:
-
Total bilirubin
- TC:
-
Total cholesterol
- Tn I:
-
Cardiac troponin I
- WBC:
-
White blood cell
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- eGFR:
-
Estimated glomerular filtration rate
- CAD:
-
Coronary atherosclerotic disease
- DM:
-
Diabetes mellitus
- HLI:
-
Hypoxic liver injury
- MACE:
-
Major adverse cardiovascular events
- ESC:
-
European Society of Cardiology
- WHO:
-
World Health Organization
References
Shah R, Wilkins E, Nichols M, et al. Epidemiology report: trends in sex-specific cerebrovascular disease mortality in Europe based on WHO mortality data. Eur Heart J. 2019;40:755–64.
Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–77.
Poelzl G, Ess M, Mussner-Seeber C, et al. Liver dysfunction in chronic heart failure: prevalence, characteristics and prognostic significance. Eur J Clin Investig. 2012;42:153–63.
Allen LA, Felker GM, Pocock S, et al. Liver function abnormalities and outcome in patients with chronic heart failure: data from the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) program. Eur J Heart Fail. 2009;11:170–7.
Fouad YM, Yehia R. Hepato-cardiac disorders. World J Hepatol. 2014;6:41–54.
Alvarez AM, Mukherjee D. Liver abnormalities in cardiac diseases and heart failure. Int J Angiol. 2011;20:135–42.
Yun KE, Shin CY, Yoon YS, et al. Elevated alanine aminotransferase levels predict mortality from cardiovascular disease and diabetes in Koreans. Atherosclerosis. 2009;205:533–7.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77.
American Diabetes A. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S13–28.
Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–44.
Kavoliuniene A, Vaitiekiene A, Cesnaite G. Congestive hepatopathy and hypoxic hepatitis in heart failure: a cardiologist’s point of view. Int J Cardiol. 2013;166:554–8.
Gao M, Cheng Y, Zheng Y, et al. Association of serum transaminases with short- and long-term outcomes in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. BMC Cardiovasc Disor. 2017;17:43.
Baars T, Sowa JP, Neumann U, et al. Liver parameters as part of a non-invasive model for prediction of all-cause mortality after myocardial infarction. Arch Med Sci. 2020;16:71–80.
Moon J, Kang W, Oh PC, et al. Serum transaminase determined in the emergency room predicts outcomes in patients with acute ST-segment elevation myocardial infarction who undergo primary percutaneous coronary intervention. Int J Cardiol. 2014;177:442–7.
Jantti T, Tarvasmaki T, Harjola VP, et al. Frequency and prognostic significance of abnormal liver function tests in patients with cardiogenic shock. Am J Cardiol. 2017;120:1090–7.
Ghouri N, Preiss D, Sattar N. Liver enzymes, nonalcoholic fatty liver disease, and incident cardiovascular disease: a narrative review and clinical perspective of prospective data. Hepatology. 2010;52:1156–61.
Siddiqui MS, Sterling RK, Luketic VA, et al. Association between high-normal levels of alanine aminotransferase and risk factors for atherogenesis. Gastroenterology. 2013;145:1271-9.e1-3.
Packard CJ. Triacylglycerol-rich lipoproteins and the generation of small, dense low-density lipoprotein. Biochem Soc Trans. 2003;31:1066–9.
Tobey TA, Greenfield M, Kraemer F, et al. Relationship between insulin resistance, insulin secretion, very low density lipoprotein kinetics, and plasma triglyceride levels in normotriglyceridemic man. Metabolism. 1981;20:165–71.
Simonen P, Kotronen A, Hallikainen M, et al. Cholesterol synthesis is increased and absorption decreased in non-alcoholic fatty liver disease independent of obesity. J Hepatol. 2011;54:153–9.
Guagliumi G, Stone GW, Cox DA, et al. Outcome in elderly patients undergoing primary coronary intervention for acute myocardial infarction: results from the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) trial. Circulation. 2004;110:1598–604.
Cinar T, Hayiroglu M, Seker M, et al. The predictive value of age, creatinine, ejection fraction score for in-hospital mortality in patients with cardiogenic shock. Coron Artery Dis. 2019;30:569–74.
Tanik VO, Cinar T, Arugaslan E, et al. The predictive value of PRECISE-DAPT score for in-hospital mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology. 2019;70:440–7.
Choi S, Jang WJ, Song YB, et al. D-dimer levels predict myocardial injury in ST-segment elevation myocardial infarction: a cardiac magnetic resonance imaging study. PLoS ONE. 2016;11:e0160955.
Kikkert WJ, Claessen BE, Stone GW, et al. D-dimer levels predict ischemic and hemorrhagic outcomes after acute myocardial infarction: a HORIZONS-AMI biomarker substudy. J Thromb Thrombolysis. 2014;37:155–64.
Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351:1285–95.
Hayiroglu MI, Bozbeyoglu E, Yildirimturk O, et al. Effect of acute kidney injury on long-term mortality in patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock who underwent primary percutaneous coronary intervention in a high-volume tertiary center. Turk Kardiyol Dern Ars. 2020;48:1–9.
Margolis G, Gal-Oz A, Khoury S, et al. Relation of subclinical serum creatinine elevation to adverse in-hospital outcomes among myocardial infarction patients. Eur Heart J Acute Cardiovasc Care. 2018;7:732–8.
Rozenbaum Z, Benchetrit S, Minha S, et al. The effect of admission renal function on the treatment and outcome of patients with acute coronary syndrome. Cardiorenal Med. 2017;7:169–78.
Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323.
Karetnikova V, Gruzdeva O, Uchasova E, et al. Glucose levels as a prognostic marker in patients with ST-segment elevation myocardial infarction: a case-control study. BMC Endocr Disord. 2016;16:31.
Hayıroglu M, Keskin M, Uzun AO, et al. Predictors of In-hospital mortality in patients with ST-segment elevation myocardial infarction complicated with cardiogenic shock. Heart Lung Circ. 2019;28:237–44.
Liang H, Guo YC, Chen LM, et al. Relationship between fasting glucose levels and in-hospital mortality in Chinese patients with acute myocardial infarction and diabetes mellitus: a retrospective cohort study. BMC Cardiovas Disor. 2016;16:156.
Creager MA, Luscher TF, Cosentino F, et al. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Circulation. 2003;108:1527–32.
Acknowledgements
None.
Funding
This work was supported by the Science and Technology Development Program of Jilin Province under Grant No. 20190103079JH, the Youth Development Foundation of the First Hospital of Jilin University under Grant No. JDYY102019004, the National Natural Science Foundation of China(82071853) and the Youth Development Foundation of the First Hospital of Jilin University under Grant No. JDYY102019005.
Author information
Authors and Affiliations
Contributions
XL and JL made main contribution to design of the study, drafted the manuscript, and performed the statistical analysis and participated. ZZ and MJJ performed data collection and helped to draft the manuscript and make the statistical analysis. HJ and GY participated in the design and coordination of the study and participated in the data collection. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics review board of the First Hospital of Jilin University (No. 2016-263). All patients gave written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Zhao, Z., Jiang, H. et al. Predictive value of elevated alanine aminotransferase for in-hospital mortality in patients with acute myocardial infarction. BMC Cardiovasc Disord 21, 82 (2021). https://doi.org/10.1186/s12872-021-01903-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-01903-z