Abstract
Background
Individuals with established cardiovascular disease (CVD) and risk factors such as age, smoking, hypertension, and diabetes mellitus are at an increased risk of recurrent cardiovascular events and death. The incidence rate of recurrent CVD events varies between countries and populations. The United Arab Emirates (UAE) has one of the highest age-standardized death rates for CVD worldwide. The aim of our study was to estimate the incidence rates and determine the predictors of recurrent CVD events among UAE nationals.
Methods
We investigated an outpatient-based cohort of patients with a history of CVD visiting Tawam Hospital between April 1, 2008 and December 31, 2008. They were followed-up until July 31, 2018. Univariable and multivariable Cox proportional hazards regression models were used to determine the association between major CVD risk factors and the risk of CVD recurrence.
Results
A total of 216 patients (167 males, 49 females) with a history of CVD were included. They were followed for a median (interquartile range) of 8.1 (5.5–9.3) years, with a total of 1184 patient-years of follow-up. The overall incidence rate of recurrent CVD events was 92.1 per 1000 patient-years. The 8-year cumulative incidence was 73.7%. Age, female sex, and diabetes mellitus were significant predictors of recurrent CVD events, where females had a 1.96 times higher risk of recurrent CVD events than males.
Conclusion
Significant predictors of recurrent CVD events are older age, female sex, and diabetes mellitus. The incidence rate of recurrent CVD events was 92.1 per 1000 patient-years. Preventive measures, based on international guidelines for CVD management, may improve CVD morbidity and mortality in the UAE population.
Similar content being viewed by others
Background
Individuals with a history of cardiovascular disease (CVD) are at a much higher risk of recurrent CVD events or death [1]. Nonetheless, the prognosis of CVD has improved due to developments in early revascularization, antithrombotic medications, and other tertiary prevention measures, including the control of major CVD risk factors [2]. The incidence rate of recurrent CVD events varies between countries and populations. The Second Manifestations of ARTerial disease study conducted by the University Medical Centre Utrecht demonstrated a 53% reduction in the crude incidence rate of recurrent CVD events between 1996 and 2014 [3]. Studies from the United States and Western Australia have also documented decreasing trends in incidence and mortality rates [4,5,6]. However, the increasing prevalence of CVD risk factors e.g. obesity and diabetes mellitus [2], and the emergence of novel biochemical risk factors, such as cellular, imaging parameters [7] and C-reactive protein [8] are strong predictors of cardiovascular events, all of which are now challenging these declining trends.
Independent predictors of recurrent CVD events or death include age, smoking, hypertension (HTN), dyslipidemia, diabetes mellitus, chronic kidney disease, and the underutilization of medications recommended by current treatment guidelines [9, 10]. A previous study conducted in the United Arab Emirates (UAE) reported 35% with HTN, 34% having dyslipidemia, 14.4% had a history of coronary artery disease (CAD) and 29.5% with diabetes mellitus also had concomitant macrovascular complications [11]. The UAE has one of the highest age-standardized death rates for CVD, at 204 and 309 per 100,000 [12], when compared to North America, which has a rate of 143 and 204 per 100,000, and Western Europe, which has a rate of 132 and 187 per 100,000 in females and males, respectively [13].
The UAE is experiencing an economic transition since the discovery of oil over 5 decades ago, and as a consequence, there has been a change in lifestyle among UAE populations that has resulted in an increase in CVD risk factors and worsening outcomes. To the best of our knowledge, few studies have investigated the epidemiology of recurrent CVD events in the UAE. Thus, we aimed to assess the incidence rate of recurrent CVD events in males and females and evaluated the influence of major CVD risk factors on the recurrence rate of CVD events among UAE nationals.
Methods
Study setting
This retrospective cohort study was conducted in Tawam Hospital in Al Ain City, which is the fourth largest city in the UAE, with a population of 650,000. Approximately 30% of this population are UAE nationals. Tawam Hospital is one of the largest tertiary care hospitals in Al Ain, providing health care services to UAE nationals and the expatriate community.
The United Arab Emirates University and Tawam Hospital Review Boards (CRD 239/13) granted ethical approval for this study. The Cerner© electronic medical record (EMR) management system was utilized to obtain patient data retrospectively. Patient information was anonymized to protect patients’ identities. Informed consent was waived as identifying data was not collected from the EMR.
Study population
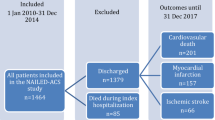
The original study population included all patients who visited the outpatient clinics of Tawam Hospital between April 1, 2008 and December 31, 2008. Patients who were ≥ 18 years old and had an established diagnosis of coronary artery disease (CAD), cerebrovascular disease, or peripheral vascular disease (PVD) were included in this study. Established CAD was defined as a documented history of stable angina, unstable angina, percutaneous coronary intervention (PCI), coronary artery bypass graft surgery, or myocardial infarction (MI). Cerebrovascular disease was defined as a documented diagnosis of transient ischemic attack (TIA) or stroke. PVD was defined as a documented diagnosis of peripheral artery disease. Patients with missing baseline data were excluded. Patients were followed-up from the time of diagnosis until a recurrent CVD event, death, or the end of the study period on July 31, 2018.
Baseline characteristics
Data retrieved from the EMR included sociodemographic parameters such as age; sex; body mass index (BMI); CVD risk factors, included smoking, a history of HTN, systolic blood pressure (SBP), diastolic blood pressure (DBP), history of diabetes mellitus, total cholesterol, and low-density lipoprotein (LDL); and medications, such as the use of anti-hypertensive medications, lipid-lowering medications, and antiplatelet therapy. Smokers were defined as current smokers or having a history of smoking based on the results of a recent local study [14]. BMI was calculated as weight in kilograms divided by the height in meters squared. Commonly accepted BMI ranges are those recommended by the World Health Organization: overweight (BMI 25–29.99 kg/m2), obese class I (BMI 30–34.99 kg/m2), obese class II (BMI 36–40 kg/m2), and obese class III (≥ 41 kg/m2) [15]. Diabetes mellitus was defined as receiving oral hypoglycemic medications or having a diagnosis made by an attending physician. HTN was defined as receiving anti-hypertensive medications or having a SBP ≥140 mmHg or DBP ≥ 90 mmHg, and blood pressure was categorized as follows: normal (SBP < 140 or DBP < 90), grade 1 HTN (SBP 140–159 or DBP 90–99), grade 2 (SBP 160–179 or DBP 100–109), and grade 3 (SBP ≥180 or DBP ≥110) [16]. Based on Adult Treatment Panel III guidelines, a LDL level < 2.6 mmol/L (< 100 mg/dL) was classified as optimal and ≥ 2.6 mmol/L (≥100 mg/dL) as suboptimal, and total cholesterol ≤5.17 mmol/L (≤200 mg/dL) was classified as optimal and > 5.17 mmol/L (> 200 mg/dL) as suboptimal [17].
Recurrent CVD events
The outcome of our study included recurrent CVD events and/or death. Recurrent CVD events included stable angina, unstable angina, PCI, MI, TIA, and cerebral infarction (confirmed by computed tomography scan or magnetic resonance imaging), or ankle-brachial index < 0.9. Vascular death was defined as sudden death or death from a fatal MI or fatal stroke. The data on patients’ comorbidities and CVD events were collected using the histories recorded on the EMR.
The overall incidence rate of recurrent CVD events, the incidence rates in males and females, and the incidence rates according to different age categories were calculated by dividing the number of study participants with recurrent CVD events by the total patient-years of follow-up for the study population and for each subgroup accordingly.
Statistical analysis
The study’s sample size was calculated using a formula for a study designed to estimate incidence in a population [18]. A sample size of 194 was determined based on an anticipated 60% incidence of recurrent CVD events [19] and utilizing 80% power with a 2-sided significance level of 0.05.
Baseline variables were compared between males and females using independent-samples t-test for continuous variables and Fisher’s exact test (2-tailed) for categorical variables. Continuous variables are presented as means [±standard deviation (SD)], while categorical variables are presented as proportions. The patient-years at risk for recurrent CVD events were calculated for each subject from the baseline visit until the occurrence of a recurrent CVD event, death, or the last outpatient clinic visit, whichever occurred first. Univariable and multivariable Cox proportional hazards regression models evaluated the risk factors for recurrent CVD events. The independent predictors included in the multivariable analysis were age (continuous), sex, smoking history, blood pressure (systolic and diastolic), anti-platelet medication, diabetes mellitus, LDL (continuous), and BMI (continuous). Proportional hazards assumption was assessed by log-log plots, while multi-collinearity was evaluated by examining the tolerance value. The results are expressed as hazard ratios and 95% confidence intervals (CIs). A p-value < 0.05 (2-sided) was considered statistically significant for all tests. All statistical analyses were performed using IBM SPSS software, version 25 (IBM Corporation, Armonk, NY, USA).
Results
A total of 216 patients (167 males, 49 females) with a history of CVD at baseline were included in our study. They were followed-up for a median (interquartile range) of 8.1 (5.5–9.3) years, with a total of 1184 patient-years of follow-up. Mean age was 65.7 (SD: 11.2, range: 28–96) years. At baseline, CAD, cerebrovascular disease, and PVD were diagnosed in 69, 38, and 6.5% of the patients, respectively. Over the 8-year follow-up period, at least 51% of patients (79 males, 30 females) had experienced a recurrent CVD event, with 9 (4.2%), 66 (30.6%), and 26 (12.0%) patients having developed PVD, CAD, and cerebrovascular disease, respectively.
The overall incidence rate of recurrent CVD events was 92.1 per 1000 patient-years of follow-up (95% CI: 76.0–110.6). Assuming a constant incidence rate over time, the 8-year cumulative incidence of recurrent CVD events was 73.7%. The annual CVD mortality rate over the study period was 18.5 per 1000 individuals (95% CI: 13.4–25.2) per year. The incidence rates of recurrent CVD events among females and males were 119.8 (95% CI: 82.3–168.9) and 84.6 (95% CI: 67.4–104.9) per 1000 patient-years of follow-up, respectively. The incidence rates for different age categories were as follows: 51.1, 35.5, 68.4, 70.8, and 115.2 for patients aged ≤34, 35–44, 45–54, 55–64, and ≥ 65 years per 1000 years of follow-up, respectively.
Table 1 shows the sociodemographic and risk factor characteristics of our study population. At baseline, 3.7% of patients aged 35–44 years had CVD, and this was even higher, at 7.4%, in patients aged 45–54 years. A sizeable portion of the population were smokers (27%) despite having a history of CVD. Furthermore, 94.9% of our patients were hypertensive, and about 43% of them had elevated BP values with 31.5, 8.3, and 3.2% of patients diagnosed with HTN grade 1, 2, and 3, respectively. Of the 85% on statins, at least half of our patients had elevated LDL levels. An extremely high percentage of patients with diabetes mellitus (62.5%) was noted in our cohort. Furthermore, two-thirds of the study population was either overweight (38.4%) or obese (27.3%). Notably, the prevalence of obesity among female patients with CVD was 41%.
Table 2 shows the univariable and multivariable analyses determining the association between different major CVD risk factors and the risk of recurrent CVD events. The proportional hazards assumption was not significant, and the tolerance ranged from 0.58–0.97, which indicated an absence of multicollinearity. Older age, female sex, and diabetes mellitus were significant predictors of recurrent CVD events or death in the multivariable model, and females had a 1.96 times higher risk for recurrent CVD events than males. Sex and diabetes mellitus, although not significant in the univariable analysis, became significant in the multivariable analysis. We, therefore, tested for an interaction effect in the multivariable model. However, no significant interaction between sex and diabetes mellitus was observed (p = 0.547).
A multivariable survival curve comparing the incidence of CVD events in males and females is shown in Fig. 1. We found that for every 1-year increase in age, patients had a 4% higher probability of developing a recurrent CVD event. Furthermore, a history of diabetes mellitus and prior CVD doubled the risk of recurrent CVD events.
Adjusted for age (continuous), sex (dichotomous), smoking (dichotomous), SBP, DBP, anti-platelet medication, diabetes mellitus (dichotomous), LDL cholesterol (continuous), and BMI (continuous).
Discussion
To the best of our knowledge, this is the first study to examine the incidence rates and explore the risk factors for recurrent CVD events among UAE nationals. The overall incidence rate of recurrent CVD events in this study (92.1 per 1000 patient-years) appears to be one of the highest reported rates in literature [19,20,21,22] and in the Middle Eastern region [23]. Older age, female sex and diabetes mellitus were found to be significant risk predictors of recurrent CVD events or death. One of the intriguing findings in our study was the significantly higher risk of recurrent CVD events among females than among males. In addition, about 43% of the patients had poorly controlled blood pressures with 31.5, 8.3, and 3.2% of patients diagnosed with HTN grade 1, 2, and 3, respectively, and despite the majority of patients on prescribed statins, only half had optimal LDL levels.
In this study, recurrent CVD increased exponentially with advancing age, which was supported by the findings of previous studies [5, 21, 23, 24]. For every 1-year increase in age, we found a 4% higher probability for recurrent CVD events in the UAE population, whereas the probability was 2% lower in a neighboring country [23]. Moreover, similar to the findings of Giorda et al., we found that diabetes mellitus was a significant independent risk factor for recurrent CVD events [24]. This study found that 62.5% of patients had concurrent diabetes mellitus and CVD, which was almost double (29.5%) of that found in a study that was conducted in the same city as ours [11]. After adjusting for all risk factors, the probability of CVD recurrence in patients with diabetes mellitus was 2 times higher than that in patients without diabetes mellitus. These findings were similar to those of other studies [20, 25].
While the results of sex-based studies showed that females have more favorable results than males [26,27,28], other studies [29, 30] concurred with the results obtained in this study, showing that females had a 1.96 times higher risk of recurrent CVD events than their male counterparts, and thus, were more likely to have a worse CVD risk-factor profile [29, 30]. Many factors, such as an increased prevalence in HTN, diabetes, and obesity, may contribute to the poor CVD risk profiles of women [30]. Additionally, smoking, coupled with an increased consumption, had a greater negative effect in women than in men. Research on current smokers showed hazard ratios of 3.46 (95% CI: 3.02–3.98) in women compared to 2.23 (95% CI: 2.03–2.44) in men [30].
Based on the existing literature [31,32,33,34], we expected a positive association between the major modifiable risk factors (smoking, HTN, and suboptimal LDL levels) and cardiovascular outcomes. However, in our study the associations between smoking, HTN, elevated levels of LDL with recurrent CVD events were not significant. Evidence suggests that anti-hypertensive treatments [31] and lipid-lowering medications are commonly underutilized in patients at high-risk of recurrent CVD events [31,32,33,34,35,36]. Whether this is due to poor adherence to treatment or inadequate treatment regimens remains unclear and should be further investigated.
Strengths
Our study is the first to report the incidence rates and risk factors associated with recurrent CVD events in the UAE population. The extended duration of the follow-up period, assessing recurrent CVD events and mortality, has enriched the epidemiological data for this region.
Limitations
This study has some limitations. This is a retrospective study, which made researchers rely on the accurate capturing of clinical data by physicians on the EMRs. The relatively small sample size and the geographical distribution limits the generalizability of our results to other cohorts. Further studies should be performed using other population groups. Sociodemographic parameters such as education and occupation would have benefitted the analysis, but these were not available for inclusion. Moreover, prediction models to evaluate the effect of other medical comorbidities such as heart failure, atrial fibrillation, and chronic kidney disease which may have influenced CVD outcomes and prognosis, were not included in the analysis. Thus, future studies should include these parameters.
Conclusions
Our study found high incidence rates of recurrent CVD events among patients with a history of CVD attending the outpatient clinics in a tertiary hospital in Al Ain. Furthermore, older age, female sex, and diabetes mellitus were strong independent predictors of recurrent CVD events. Although local screening programs are designed towards early diagnosis and the provision of disease management interventions [37], more needs to be done to improve primary and tertiary preventative measures in order to improve CVD morbidity and mortality among UAE nationals.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic blood pressure
- HTN:
-
Hypertension
- LDL-C:
-
Low-density lipoprotein-cholesterol
- MI:
-
Myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- PVD:
-
Peripheral vascular disease
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- TIA:
-
Transient ischemic attack
- UAE:
-
United Arab Emirates
References
Lin FJ, Tseng WK, Yin WH, Yeh H-I, Chen J-W, Wu C-C. Residual risk factors to predict major adverse cardiovascular events in atherosclerotic cardiovascular disease patients with and without diabetes mellitus. Sci Rep. 2017;7:9179.
Quiles J, Miralles-Vicedo B. Update: acute coronary syndromes (IX). Secondary prevention strategies for acute coronary syndrome. Rev Esp Cardiol. 2014;67:844–8.
Berkelmans GFN, Graaf Y, Dorresteijn JAN, et al. Decline in risk of recurrent cardiovascular events in the period 1996 to 2014 partly explained by better treatment of risk factors and less subclinical atherosclerosis. Int J Cardiol. 2018;251:96–102.
Ergin A, Muntner P, Sherwin R, He J. Secular trends in cardiovasculardisease mortality, incidence, and case fatality rates in adults in the United States. Am J Med. 2004;117:219–27.
Briffa TG, Hobbs MS, Tonkin A, et al. Population trends of recurrent coronary heart disease event rates remain high. Circ Cardiovasc Qual Outcomes. 2011;4:107–13.
Brown TM, Deng L, Becker DJ, et al. Trends in mortality and recurrent coronary heart disease events after an acute myocardial infarction among Medicare beneficiaries, 2001–2009. Am Heart J. 2015;170:249–55.
Thomas MR, Lip GY. Novel risk markers and risk assessments for cardiovascular disease. Circ Res. 2017;120:133–49.
Barbero U, D'Ascenzo F, Nijhoff F, et al. Assessing risk in patients with stable coronary disease: when should we intensify care and follow-up? Results from a meta-analysis of observational studies of the COURAGE and FAME era. Scientifica. 2016;2016:3769152.
Chen D-Y, Li C-Y, Hsieh M-J, et al. Predictors of subsequent myocardial infarction, stroke, and death in stable post-myocardial infarction patients: A nationwide cohort study. Eur Heart J Acute Cardiovasc Care. 2019;8(7):634–42.
Lu W, Resnick HE, Jablonski KA, et al. Non-HDL cholesterol as a predictor of cardiovascular disease in type 2 diabetes: the strong heart study. Diabetes Care. 2003;26:16–23.
Al-Maskari F, El-Sadig M, Norman JN. The prevalence of macrovascular complications among diabetic patients in Al-Ain District. United Arab Emirates. Cardiovasc Diabetol. 2007;6:24.
Loney T, Aw TC, Handysides DG, et al. An analysis of the health status of the United Arab Emirates: the 'Big 4′ public health issues. Glob Health Action. 2013;6:20100.
Roth GA, Johnson C, Abajobir A, et al. Global, regional and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25.
Al-Houqani M, Leinberger-Jabari A, Al Naeemi A, et al. Patterns of tobacco use in the United Arab Emirates healthy future (UAEHFS) pilot study. PLoS One. 2018;13:e0198119.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation (WHO Technical Report Series 894). Switzerland: World Health Organization, 2000. http://apps.who.int/iris/bitstream/10665/42330/1/WHO_TRS_894.pdf?ua=1&ua=1. Accessed 5 Sept 2019.
Mancia G, Fagard R, Narkiewicz K, et al. ESH/ESC guidelines for the management of arterial hypertension. J Hypertens. 2013;31:1281–357.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Rosner B. Fundamentals of biostatistics. Boston: Cengage Learning, Inc; 2010.
Bansilal S, Castellano JM, Fuster V. Global burden of CVD: focus on secondary prevention of cardiovascular disease. Int J Cardiol. 2015;201:S1–7.
Wattanakit K, Folsom AR, Chambless LE, Nieto FJ. Risk factors for cardiovascular event recurrence in the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2005;149:606–12.
Jernberg T, Hasvold P, Henriksson M, Hjelm H, Thuresson M, Janzon M. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J. 2015;36:1163–70.
Laleman N, Henrard S, van den Akker M, et al. Time trends in statin use and incidence of recurrent cardiovascular events in secondary prevention between 1999 and 2013: a registry-based study. BMC Cardiovasc Disord. 2018;18:209.
Taravatmanesh S, Khalili D, Khodakarim S, et al. Determining the factors associated with cardiovascular disease recurrence: Tehran lipid and glucose study. J Tehran Heart Cent. 2017;12:107–13.
Giorda CB, Avogaro A, Maggini M, et al. Recurrence of cardiovascular events in patients with type 2 diabetes: epidemiology and risk factors. Diabetes Care. 2008;31:2154–9.
Cubbon RM, Abbas A, Wheatcroft SB, et al. Diabetes mellitus and mortality after acute coronary syndrome as a first or recurrent cardiovascular event. PLoS One. 2008;3:e3483.
Yu HT, Kim KJ, Bang WD, et al. Gender-based differences in the management and prognosis of acute coronary syndrome in Korea. Yonsei Med J. 2011;52:562–8.
Puddu PE, Iannetta L, Schiariti M. Age- and gender-normalized coronary incidence and mortality risks in primary and secondary prevention. Cardiol Res. 2012;3:193–204.
van der Meer MG, Cramer MJ, van der Graaf Y, Doevendans PA, Nathoe HM, (on behalf of the SMART study group). Gender difference in long-term prognosis among patients with cardiovascular disease. Eur J Prev Cardiol. 2012;21:81–9.
Dallongevillle J, De Bacquer D, Heidrich J, et al. Gender differences in the implementation of cardiovascular prevention measures after an acute coronary event. Heart. 2010;96:1744–9.
Millett ERC, Peters SAE, Woodward M. Sex differences in risk factors for myocardial infarction: cohort study of UK Biobank participants. BMJ. 2018;363:k4247.
Abdulla AM, Nagelkerke NJ, Abouchacra S, Pathan JY, Adem A, Obineche EN. Under-treatment and under diagnosis of hypertension: a serious problem in the United Arab Emirates. BMC Cardiovasc Disord. 2006;6:24.
Wakabayashi I. Gender differences in cardiovascular risk factors in patients with coronary artery disease and those with type 2 diabetes. J Thorac Dis. 2017;9:E503–6.
De Smedt D, Annemans L, De Backer G, et al. Cost-effectiveness of optimized adherence to prevention guidelines in European patients with coronary heart disease: results from the EUROASPIRE IV survey. Int J Cardiol. 2018;272:20–5.
Punekar RS, Fox KM, Richhariya A. Burden of first and recurrent cardiovascular events among patients with hyperlipidemia. Clin Cardiol. 2015;38:483–91.
Rockberg J, Jørgensen L, Taylor B, Sobocki P, Johansson G. Risk of mortality and recurrent cardiovascular events in patients with acute coronary syndromes on high intensity statin treatment. Prev Med Rep. 2017;6:203–9.
Murphy A, Palafox B, O'Donnell O, et al. Inequalities in the use of secondary prevention of cardiovascular disease by socioeconomic status: evidence from the PURE observational study. Lancet Glob Health. 2018;6:e292–301.
HAAD. Guidelines for The Provision of Cardiovascular Disease Management Programs. 2017. https://www.haad.ae › ... › Healthcare Professionals › HAAD Guidelines. Accessed 5 Sept 2019.
Acknowledgements
We are indebted to Shehab Majud for his helpful comments on the language in the manuscript.
Funding
This work was supported by the College of Medicine and Health Sciences, United Arab Emirates University (G00002956). The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
The study was conceived by RDG, who also designed the study in collaboration with SAS, DR, and ESS. SAS contributed to the acquisition of the data. SAS conducted all statistical analyses. RDG wrote the first draft of the manuscript, while all authors interpreted the data, and contributed to the writing of the subsequent versions of the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by Tawam Hospital and the United Arab Emirates University research and ethics board (CRD 239/13). The requirement for informed consent was waived because patient records and information were anonymized and de-identified prior to analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Govender, R.D., Al-Shamsi, S., Soteriades, E.S. et al. Incidence and risk factors for recurrent cardiovascular disease in middle-eastern adults: a retrospective study. BMC Cardiovasc Disord 19, 253 (2019). https://doi.org/10.1186/s12872-019-1231-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-1231-z