Abstract
Background
Little was known about the different predictive power of blood pressure (BP) parameters (SBP, systolic BP; mean arterial pressure, MAP; pulse pressure, PP; and diastolic BP, DBP) and stroke incidence. This study’s aim was to compare power of BP parameters predict stroke events among rural dwelling Chinese individuals with hypertension.
Method
A total of 5097 hypertension patients (56.2% women; mean age, 56.3 ± 11.2 years) were included in the prospective cohort study with a median follow-up of 8.4 years.
Results
Until the end of the last follow-up, there were 501 onset strokes (310 ischemic, 186 hemorrhagic, and 5 unclassified strokes) among the 5097 participants. The results showed that hazard ratio (HR) (95% confidence interval, 95% CI) with an increment of 5 mmHg were 1.095 (1.070–1.121) for PP, 1.173 (1.139–1.208) for MAP, 1.109(1.089–1.130) for SBP, 1.143(1.104–1.185) for DBP. The SBP indicated the largest β coefficient in the Cox proportional hazard model for all stroke except PP or MAP, and the SBP revealed slightly higher value than MAP (βSBP = 0.435, βMAP = 0.430, P = 0.756).
Conclusions
Both PP and MAP were predictive factors for stroke. The MAP showed a stronger ability to predict stroke events than PP, and slightly inferior to SBP for hypertension patients.
Similar content being viewed by others
Background
Stroke is considered to be the second primary cause of death in the world [1], and China has the highest burden of stroke in the glob [2]. In addition, hypertension is considered to be the mainly risk factor of disability-adjusted life-years and deaths [3]. Previous study has indicated that over one-quarter of adult population were hypertension patients in China [4]. For hypertension patients, the incidence of stroke is higher than it in persons with normal BP [5].
Recently, MAP and PP have been used as predictors for stroke events and confirmed in many studies [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21]. MAP is another measure of the overall circulating pressure load and considered to predict adverse cardiovascular outcomes. The value of MAP can be directly determined by cardiac catheterization or estimated by a formula [e.g., diastolic + 1/3 x (systolic-diastolic)]. However, as the age of the patient increases, the discrimination ability of the mean arterial pressure decreases. DBP peaked at the age of 55 and then decreased, while the systolic blood pressure (SBP) continued to grow with age, and higher every 10 years [22]. Thus, based on the individual changes in SBP and DBP with age, actual changes in MAP tend to be low with age. At the same time, there is increasing emphasis on SBP as the effective indicator of cardiovascular disease (CVD) apart from other BP parameters for the middle-aged and elderly person. The correlation between PP and SBP is more closely related to DBP with an increasing age. The PP is regarded as a proper predictor of CVD in the general population. Nevertheless, few researches have been conducted among hypertensive patients, especially in Chinese [6,7,8,9, 23]. It is particularly crucial to discover a strong predictive indicator of stroke in this group, since there were some limitations in previous studies, such as short follow-up time [23], risk factors for stroke adjusted inadequately, or lack of comparisons of HR values among the four BP parameters (PP, DBP, MAP, and SBP) [6,7,8,9,10].
The goal of our study was to explored the relationship between infrequent BP parameters (PP and MAP) and stroke events [All stroke, ischemic stroke (IS), hemorrhage stroke (HS)] in prospective hypertension cohort and compare the predictive values of four BP parameters for stroke events.
Methods
Study population
The China Medical University Ethics Committee had approved the study plan and received the written informed consent from all patients or their guardians.
Our data comes from a prospective cohort from Fuxin county hypertensive population. The first multistage cluster random sampling design was conducted in 64 rural communities in Fuxin county (including seven cities in five locations: east, west, south, north and central) of Liaoning province, China. Hypertensive patients aged ≥35 years who agreed to take part in the study and signed informed consent forms were included. At the same time, pregnant women, those having malignant tumors, severe hepatic and renal insufficiency, those unwilling to participate in the study were excluded. 6412 hypertensive patients were covered at the start of our study [24, 25]. All the eligible participants were invited to the following visits. And the three follow-up visits as detailed previously [24]. The detailed inclusion process of participants is shown in Fig. 1.
Study outcomes
Our study endpoint was stroke, according to the MONICA criteria to confirmed the events. The event with the major events in the etiology of blood vessels, including local or global brain disease lasting for more than 24 h, and stroke events due to death or surgical duration less than 24 h [25]. The project diagnostic team confirmed the new stroke events during follow-up visits and the final verification approved. Data classification and measurement on stroke as detailed previously [24].
BP measurement
Standardized measurement of BP values have been detailed in previous articles [24]. We defined hypertension as the take of anti-hypertensive medications in the last 2 weeks or DBP ≥90 mmHg or SBP ≥140 mmHg. Further calculations of BP parameters were included such as: PP = SBP − DBP; MAP = (2 × DBP + SBP)/3.
Other risk factors
Information on other risk factors data (serum glucose, lipids, cholesterol) collection and measurement had been described in previously literature [23, 24, 26]. Professional physicians performed face-to-face interviews with patients to obtain lifestyle factors (smoking, drinking, and BP medication). The smoking and drinking were defined as detailed previously [11, 24]. We defined diabetes as current treatment with oral hypoglycemic agents or insulin or fasting serum glucose levels ≥7.0 mmol/l .
Statistical analysis
The Pearson correlation was applied to assess the correlation coefficient among BP parameters. The Cox proportional hazard model was applied to count the HR value and 95% CI of four BP parameters for the risk of incident stroke. First, four BP parameters in form of continuous variables in the model, and the HRs were calculated with 1 SD mmHg intervals to estimate the relationships among four BP parameters and onset stroke events. The incident stroke was examined to determine the association with four BP values across the age < 60 years and the age of ≥60 years. Multivariable model was adjusted by sex, ethnicity, age, body mass index (BMI), smoking, diabetes mellitus (DM), drinking, heart rate (HR), TC, LDL-C, TG, HDL-C, and anti-hypertensive medications. Principle of comparing the difference in HR values were described in the previous published literature [24]. We used SPSS 22.0 (IBM Inc., Chicago, IL, USA) to conducted data analysis and P < 0.05 was regarded to be significant.
Results
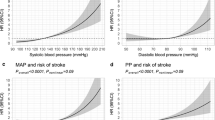
Baseline information in this study were showed in Table 1. Baseline mean (SD) age of women was 56.3 (11.2) years of the 5097 initially no-stroke hypertensive patients. A positive correlation between PP and SBP (r = 0.826; P < 0.001) was found, but PP revealed negative correlations with DBP (r = − 0.158; P < 0.001) and MAP (r = 0.357; P < 0.001) as can be shown in Fig. 2 .
501 onset outcomes occurred until the last follow-up visit(310 IS events, 186 HS events, and 5 unclassified stroke events). The incidence density of all strokes were 1236.30 per 100,000 person-years (95% CI: 1167.81–1304.79), IS was 764.97 (95% CI: 710.97–818.97), and HS was 458.99 (95% CI: 417.10–500.89). HRs (95% CI) of future stroke after multivariate adjustment for each BP parameters increased by 1 SD mmHg were listed in Table 2. All the BP parameters (All stroke, IS, and HS) showed significant association with the risk of stroke incident at 0.001 level.
Table 3 demonstrates the adjusted HRs of BP parameters that had been standardized in the Cox proportional hazard model for stroke according to age categories. The value of HR for PP among hypertensive subjects aged less than 60 revealed slightly lower than that of SBP for all stroke incident [HR (95% CI): 1.635 (1.451–1.842) vs 1.734 (1.562–1.9)] and HS incident [HR (95% CI): 1.788 (1.490–2.145) vs 2.053 (1.757–2.398)]. However, the HR value of PP (1.531, 95% CI: 1.308–1.793, P < 0.001) was the highest among the four BP for IS events. The HR values of PP among hypertensive subjects aged over 60 showed the lowest for all stroke (1.228, 95% CI: 1.86–1.389, P = 0.001), IS (1.244, 95% CI: 1.066–1.451, P = 0.005), and HS (1.200, 95% CI: 0.972–1481, P = 0.090) events.
Table 4 summarizes the results of the predictive power between the four BP parameters for all stroke, IS, and HS. For all stroke, SBP indicated the largest coefficient and PP was lower than SBP, and the difference between SBP and PP were statistically significant (βSBP = 0.435 > βMAP = 0.430 > βPP = 0.351 > βDBP = 0.322). Although the coefficient of MAP was lower than SBP marginally, the difference between MAP and SBP were not statistically significant (P = 0.756). Identical results were observed in the IS and HS events.
Discussion
The present study provided an in-depth analysis of associations between blood pressure parameters and stroke among rural Chinese persons with hypertension. The results indicated that all the BP parameters were associated with the outcomes, significantly. The study results revealed that SBP was a more effective predictor of the outcomes than DBP and PP excluding MAP.
The increase of PP enhances arteries to bear more stress, which leads to the increase of elastic component fatigue and fracture rate and weaken the lining of blood vessels. Current studies have shown that PP’s ability to predict adverse cardiovascular events were controversial [7, 8, 11,12,13,14,15,16,17,18,19,20,21]. Framingham Heart Study had indicated that PP was still a predictor for stroke incident after adjusted by SBP and DBP, even though its predictive ability was inferior to SBP and DBP. Another study had showed that PP was a powerful predictor of stroke incident when DBP and MAP were adjusted, but not when SBP was adjusted [13]. The present study (based on hypertensive patients) showed that the four BP parameters were independent risk factors for stroke after adjusting some acknowledged influential factors of stroke. However, when SBP and DBP were incorporated into the original regulatory factors, the effect of MAP and PP disappeared. The present results doesn’t agree with previous study that PP was an independent risk predictor of stroke in the general population [8].
To eliminate the impact of multiple collinearities among the four BP parameters, the four BP parameters were incorporated into the model to calculate the corresponding coefficient difference. For stroke and its two subtypes (IS and HS), SBP obtained the highest HRs value, which was followed by MAP while the HRs value of PP was lower than the above two and higher than DBP. The comparison results of stroke prediction capacity showed that the prediction ability of SBP was significantly higher than that of DBP and PP, and no significant differences were observed with MAP. The above results suggested that MAP was a sensitive indicator of onset stroke events in hypertensive patients.
It has been observed that BP (DBP and SBP) increasing in a parallel manner until age ≤ 60, as age over 60 years, SBP continues to rise, but DBP begins to decrease as a result of reducing revers capacity of aorta with advancing age [22, 27]. Therefore, PP may be regarded as a powerful indicators of BP for the elderly [8]. The Framingham heart study indicated that the risk of CHD increased by 23% when PP increasing in every 10 mmHg [13]. This association between CHD risk and PP was observed in patients over 50 years old, especially those over 60 years old [14]. Therefore, the age stratification analysis was carried out in our study with the cut-off value of 60 years old (Table 3). The current study result could not verify that PP was more applicable to the elderly population for stroke incident, however, the outcome revealed a high predictive power for the relatively low age group in hypertensive patients.
The main adverse manifestations of stroke are IS and HS, and their incidence increasing with age [28]. As people’s life expectancy increases, the burden of stroke on people and society worldwide will become heavier. 75% of stroke patients were measured to had a high BP at the time of admission [29]. Hypertension-related stroke is a pervasive, on the other hand its preventable public health related problem. Hypertension has been shown to be the most common and the most influential risk factor for IS and HS, and the incidence of IS and HS could be significantly reduced by effective hypertensive therapy [30, 31]. It is particularly crucial to control BP and to use sensitive BP parameters. Both PP and MAP were calculated from the main components of BP (SBP and DBP). PP mainly reflects two aspects of ventricular ejection volume and wave reflection [13, 32]. In addition to reflecting ventricular ejection and peripheral vascular resistance, MAP was considered as the main determinant of cerebral blood flow [13, 32], which was critical for brain tissue damage [33]. This may be the reason that MAP could predict stroke better than PP and this finding corporate the previous result [34].
Limitation
Some critical limitations need to be considered. Firstly, the present cohort study was composed of adults who were completely from rural areas in China, and their diversity may be limited. Secondly, in this study only baseline BP values was used, it should be taken into account that stroke vascular damage is a dynamic and complex process over time. Further study are required to the relationship between dynamic BP parameters levels and stroke and to clarify its pathogenesis.
Conclusion
Within the limitation of the current study, the following conclusion can be drawn. The SBP was supported as the main indicator of BP parameters in predicting stroke risk in hypertensive patients. Although PP could predict stroke risk in hypertensive patients, its predictive ability was lower than SBP. However, the assessment and management of MAP could be considered in clinical BP control and reducing the risk of stroke.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- CAD:
-
Concluded angina pectoris, myocardial infarction, arrhythmia
- CHD:
-
Coronary heart disease
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- DBP:
-
Diastolic BP
- DM:
-
Diabetes mellitus
- HDL-C:
-
High-density lipoprotein cholesterol
- HR:
-
Hazard ratio
- HS:
-
Hemorrhage stroke
- ICH:
-
Intracerebral hemorrhage stroke
- IS:
-
Ischemic stroke
- LDL-C:
-
Low-density lipoprotein cholesterol
- MAP:
-
Mean arterial pressure
- MONICA:
-
Multinational monitoring of trends and determinants in cardiovascular disease
- PP:
-
Pulse pressure
- SAH:
-
Subarachnoid hemorrhage stroke
- SBP:
-
Systolic BP
- SD:
-
Standard deviations
- TC:
-
Total cholesterol;
- TG:
-
Triglycerides
- TIA:
-
Transient ischemic attacks
References
Top 10 causes of death worldwide. 2018. http://www.who.int/mediacentre/factsheets/fs310/zh/. Accessed 25 Sept 2018.
Wang W, Jiang B, Sun H, et al. Prevalence, incidence, and mortality of stroke in China: results from a Nationwide population-based survey of 480 687 adults. Circulation. 2017;135(8):759–71.
Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990-2010: findings from the global burden of disease study 2010. Lancet. 2013;381(9882):1987–2015.
Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, et al. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. 2018;137(22):2344–56.
Kelly TN, Gu D, Chen J, et al. Hypertension subtype and risk of cardiovascular disease in Chinese adults. Circulation. 2008;118(15):1558–66.
Miura K, Nakagawa H, Ohashi Y, et al. Four blood pressure indexes and the risk of stroke and myocardial infarction in Japanese men and women: a meta-analysis of 16 cohort studies. Circulation. 2009;119(14):1892–8.
Sabayan B, van Vliet P, de Ruijter W, Gussekloo J, de Craen AJ, Westendorp RG. High blood pressure, physical and cognitive function, and risk of stroke in the oldest old: the Leiden 85-plus study. Stroke. 2013;44(1):15–20.
Glasser SP, Halberg DL, Sands CD, Mosher A, Muntner PM, Howard G. Is pulse pressure an independent risk factor for incident stroke, REasons for geographic and racial differences in stroke. Am J Hypertens. 2015;28(8):987–94.
de Simone G, Roman MJ, Alderman MH, Galderisi M, de Divitiis O, Devereux RB. Is high pulse pressure a marker of preclinical cardiovascular disease? Hypertension. 2005;45(4):575–9.
Verdecchia P, Schillaci G, Reboldi G, Franklin SS, Porcellati C. Different prognostic impact of 24-hour mean blood pressure and pulse pressure on stroke and coronary artery disease in essential hypertension. Circulation. 2001;103(21):2579–84.
Li Z, Bai Y, Guo X, Zheng L, Sun Y, Roselle AM. Alcohol consumption and cardiovascular diseases in rural China. Int J Cardiol. 2016;215:257–62.
Pastor-Barriuso R, Banegas JR, Damian J, Appel LJ, Guallar E. Systolic blood pressure, diastolic blood pressure, and pulse pressure: an evaluation of their joint effect on mortality. Ann Intern Med. 2003;139(9):731–9.
Franklin SS, Khan SA, Wong ND, Larson MG, Levy D. Is pulse pressure useful in predicting risk for coronary heart disease? The Framingham heart study. Circulation. 1999;100(4):354–60.
Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103(9):1245–9.
Thomas F, Blacher J, Benetos A, Safar ME, Pannier B. Cardiovascular risk as defined in the 2003 European blood pressure classification: the assessment of an additional predictive value of pulse pressure on mortality. J Hypertens. 2008;26(6):1072–7.
Domanski M, Mitchell G, Pfeffer M, Neaton JD, Norman J, Svendsen K, et al. Pulse pressure and cardiovascular disease-related mortality: follow-up study of the multiple risk factor intervention trial (MRFIT). Jama. 2002;287(20):2677–83.
Franklin SS, Lopez VA, Wong ND, Mitchell GF, Larson MG, Vasan RS, et al. Single versus combined blood pressure components and risk for cardiovascular disease: the Framingham heart study. Circulation. 2009;119(2):243–50.
Lorenzo C, Aung K, Stern MP, Haffner SM. Pulse pressure, prehypertension, and mortality: the San Antonio heart study. Am J Hypertens. 2009;22(11):1219–26.
Okada K, Iso H, Cui R, Inoue M, Tsugane S. Pulse pressure is an independent risk factor for stroke among middle-aged Japanese with normal systolic blood pressure: the JPHC study. J Hypertens. 2011;29(2):319–24.
Panagiotakos DB, Kromhout D, Menotti A, Chrysohoou C, Dontas A, Pitsavos C, et al. The relation between pulse pressure and cardiovascular mortality in 12,763 middle-aged men from various parts of the world: a 25-year follow-up of the seven countries study. Arch Intern Med. 2005;165(18):2142–7.
Assmann G, Cullen P, Evers T, Petzinna D, Schulte H. Importance of arterial pulse pressure as a predictor of coronary heart disease risk in PROCAM. Eur Heart J. 2005;26(20):2120–6.
Franklin SS, Gustin W 4th, Wong ND, Larson MG, Weber MA, Kannel WB, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham heart study. Circulation. 1997;96:308–15.
Zheng L, Sun Z, Li J, Zhang R, Zhang X, Liu S, et al. Pulse pressure and mean arterial pressure in relation to ischemic stroke among patients with uncontrolled hypertension in rural areas of China. Stroke. 2008;39(7):1932–7.
Zheng J, Sun Z, Zhang X, Li Z, Guo X, Xie Y, et al. Non-traditional lipid profiles associated with ischemic stroke not hemorrhagic stroke in hypertensive patients: results from an 8.4 years follow-up study. Lipids Health Dis. 2019;18:1–9.
Zhao D, Liu J, Wang W, Zeng Z, Cheng J, Liu J, et al. Epidemiological transition of stroke in China: twenty-one-year observational study from the Sino-MONICA-Beijing project. Stroke. 2008;39(6):1668–74.
Zheng L, Sun Z, Zhang X, Li J, Hu D, Sun Y. The association between glomerular filtration rate and stroke in hypertensive patients in rural areas of China. J Hypertens. 2012;30(5):901–7.
Messerli FH, Sundgaard-Riise K, Ventura HO, Dunn FG, Glade LB, Frohlich ED. Essential hypertension in the elderly: haemodynamics, intravascular volume, plasma renin activity, and circulating catecholamine levels. Lancet. 1983;2(8357):983–6.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
Qureshi AI, Ezzeddine MA, Nasar A, Suri MF, Kirmani JF, Hussein HM, et al. Prevalence of elevated blood pressure in 563,704 adult patients with stroke presenting to the ED in the United States. Am J Emerg Med. 2007;25(1):32–8.
Vaccarino V, Berger AK, Abramson J, Black HR, Setaro JF, Davey JA, et al. Pulse pressure and risk of cardiovascular events in the systolic hypertension in the elderly program. Am J Cardiol. 2001;88(9):980–6.
Staessen JA, Thijs L, O'Brien ET, Bulpitt CJ, de Leeuw PW, Fagard RH, et al. Ambulatory pulse pressure as predictor of outcome in older patients with systolic hypertension. Am J Hypertens. 2002;15:835–43.
Nichols WW, Nicolini FA, Pepine CJ. Determinants of isolated systolic hypertension in the elderly. J Hypertens Suppl. 1992;10(6):S73–7.
Willie CK, Tzeng YC, Fisher JA, Ainslie PN. Integrative regulation of human brain blood flow. J Physiol. 2014;592(5):841–59.
Millar JA, Lever AF, Burke V. Pulse pressure as a risk factor for cardiovascular events in the MRC mild hypertension trial. J Hypertens. 1999;17(8):1065–72.
Acknowledgments
Not applicable.
Funding
This work was supported by the National Nature Science Foundation of China [No. 81773510]; National Key R&D Program of China [Grant #2017YFC1307600]. All the funding bodies had influence on designing research, data collection, data analyzing, and writing the manuscript.
Author information
Authors and Affiliations
Contributions
YS contributed conception and design of the study; JZ, ZS, LZ, XG, GS, and YX organized the database; JZ conducted statistical analysis and wrote the first draft of the manuscript. LZ and ZJ contributed to manuscript revision. All authors have read and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The China Medical University Ethics Committee had approved the study plan and received the written informed consent from all patients or their guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zheng, J., Sun, Z., Guo, X. et al. Blood pressure predictors of stroke in rural Chinese dwellers with hypertension: a large-scale prospective cohort study. BMC Cardiovasc Disord 19, 206 (2019). https://doi.org/10.1186/s12872-019-1186-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-1186-0