Abstract
Background
We investigated changes of cortical thickness and its association with cognitive performance in patients with high-grade carotid artery stenosis without ischemic brain lesions.
Methods
We studied 25 patients with unilateral carotid artery stenosis ≥50% and 25 age-matched controls. All subjects underwent T1-weighted MRI, and cortical thickness was measured in 33 regions of interest in each hemisphere, as well as in brain regions belonging to the vascular territory of the middle cerebral artery (MCA). General linear mixed models were fitted to the dependent variable cortical thickness. Cognitive assessment comprised the Stroop Test and Trail Making Test B.
Results
In the linear mixed model, presence of carotid stenosis had no effect on cortical thickness. There was a significant interaction of stenosis and region with a trend towards lower cortical thickness in the MCA region on the side of carotid stenosis. Patients with carotid stenosis performed significantly worse on the Stroop test than controls, but there was no correlation with cortical thickness.
Conclusion
In patients with carotid stenosis without ischemic brain lesions, neither a clear pattern of reduced cortical thickness nor an association of cortical thickness with cognitive function was observed. Our data do not support the hypothesized association of cortical thinning and cognitive impairment in carotid stenosis.
Similar content being viewed by others
Background
Carotid stenosis is a known risk factor for stroke [1]. In population based studies, asymptomatic carotid stenosis can be found in up to 5.7%, with higher prevalence in men and with higher age [2, 3]. While carotid stenosis is usually termed “asymptomatic” in the absence of stroke related to the stenosis, there is continuous debate about detrimental effects of carotid stenosis on brain structure and cognition beyond the occurrence of cerebrovascular events.
Non-invasive measurement of cortical thickness by structural MRI has come into focus as a biomarker of brain pathology as it was linked with performance in cognitive tests [4]. It is considered to reflect the structural integrity of cortical gray matter, and can be influenced by age, sex, subcortical lesions, specific training or diseases of the brain [5, 6]. Vascular risk factors were also found to be associated with cortical thinning [7].
Hemodynamic compromise with focal brain lesions, i.e. ischemic stroke, is well known to go together with secondary cortical thinning [8,9,10]. The same was observed for symptomatic hemodynamic impairment, e.g. subclavian steal syndrome [11]. For asymptomatic carotid stenosis, data on cortical thickness is scarce. A pilot study suggested, that altered cerebral perfusion in carotid stenosis is associated with regional cortical thinning [12]. Another study revealed a decrease of cortical thickness specifically in the anterior cerebral artery territory [13]. Several studies report an association of carotid artery stenosis with impaired cognitive performance [14,15,16,17,18,19,20,21,22]. Whether structural brain changes including regional cortical thinning represent a relevant mechanism contributing to cognitive impairment in carotid stenosis remains unclear.
We aimed at evaluating cortical thickness and a hypothesized association of cortical thinning with impaired cognitive function in patients with unilateral carotid stenosis in the absence of focal ischemic brain lesions.
Methods
Patients and controls
Between March 2015 and October 2016, we enrolled 25 patients with findings of unilateral carotid artery stenosis without ischemic brain lesions on MRI, in whom interventional or surgical treatment of carotid stenosis was planned. Patients presented to the outpatient departments or were referred for treatment at the Department of Neurology or at the Department of Vascular Surgery. Decision to perform carotid revascularization was made by interdisciplinary consensus decision as described recently [23]. Inclusion criteria were: unilateral internal carotid artery stenosis of at least 50% assessed by ultrasound following the North American Symptomatic Carotid Endarterectomy Trial (NASCET) [24, 25]; between 60 and 90 years of age; no history of stroke; no ischemic brain lesion on MRI. As a control group, we studied 25 healthy age-matched controls. Inclusion criteria were no history of a TIA or stroke and no neurological or psychiatric disease. Exclusion criteria for both groups were a history of a severe disease, structural brain lesions and inability to undergo MRI. All participants provided written informed consent. The study was approved by the ethics committee of the Hamburg chamber of physicians.
MRI protocol and image analysis
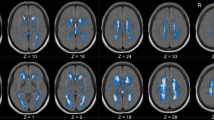
MRI was performed prior to treatment of the stenosis on a 3 T Skyra MRI scanner (Siemens, Erlangen, Germany). For anatomical imaging, a T1-weighted high-resolution three-dimensional magnetization-prepared, rapid acquisition gradient-echo sequence (MPRAGE) was used with the following parameters: TR = 2500 ms, TE = 2.12 ms, FOV = 240 × 192 mm, 256 axial slices, ST = 0.94 mm, IPR = 0.94 × 0.94 mm.
T1-weighted MR-images were preprocessed using the Freesurfer software package 6.0.0 with standard procedures and parameters [26,27,28]. After careful visual inspection of images and skull stripping and registration to MNI space coordinates [29, 30], Freesurfer segments the brain volume into white and grey matter creating white matter-gray matter and pial surface boundary. From these volumes, the cortical thickness is calculated for 35 labelled region of interests (ROIs) on the cortical surface. For our analysis, we excluded the entorhinal ROI resulting from its eccentric position making it prone to artifacts and inaccurate results. Thus, we included 33 ROI in our analysis.
In addition, we defined vascular regions of interest by brain regions in the vascular territory of the middle cerebral artery (MCA) according to previous description of arterial territories [31,32,33]: (MCA region), and all other brain regions (non-MCA region).
Cognitive tests
Cognitive tests were performed on the same day as the MRI examination and comprised the following: Stroop Test and trail making test B (TMT B), being part of the extended Consortium to Establish a Registry for Alzheimer’s disease (CERAD-Plus) test battery. From the results of the TMT B [34], z scores were determined according to evaluation system CERAD-Plus Online (https://www.memoryclinic.ch/de/main-navigation/cerad-plus/), of the Memory Clinic (Universitäre Altersmedizin, Felix Platter-Spital, Basel, memoryclinic@fps-basel.ch) [42]. The CERAD-Plus online analysis program transforms the total raw score into specific values and converts them into z scores that are corrected for age, education and sex, thereby enabling comparison with performance of a standard reference sample. Z scores describe by how many standard deviations the results differ from the reference sample. By subtracting the time to accomplish the Farb-Wort- Test (FWT, corresponding to the Stroop Test) II and III, results were obtained that were modified according to the age of each patient by assessment tables from the Nürnberger Alters-Inventar [35], thereby resulting in C scores. Additionally, the Mini Mental State Examination (MMSE) was performed by all participants and the clock drawing test (CDT) and dementia detection test (DemTect). Higher score in the MMSE and DemTect are reflected by better cognitive function, whereas higher score in the CDT is associated with lower cognitive performance. To compare cognitive tests of patients and controls, Stroop test and TMT results were corrected for age and adjusted to a standard reference sample.
Statistics
All statistical analyses were performed using IBM SPSS Statistics 22. A general linear mixed model (GLMM) was employed to determine significant main effects and interaction effects of independent variables on cortical thickness. The GLMM accounted for random intercepts of patients and hemispheres within patients, considering regions within hemispheres and patients as repeated measures. Non-significant interactions were hierarchically stepwise-backward eliminated from the model until only main effects and significant interactions remained. Two analyses were performed: first, including all 66 ROI, and second, including four vascular regions (ipsilateral and contralateral MCA region and non-MCA region). The following independent variables were included in the model: group (patient or control), hemisphere (left or right), presence of stenosis (yes or no), ROI and age. Group (patient or control) and stenosis (presence of stenosis yes or no) and hemisphere (left or right) were included as interaction terms to be able to identify potential specific regional effects of stenosis on individual hemispheres, thus enabling the separation of possible systematic effects of group from specific effects of unilateral stenosis on cortical thickness.
Results of cognitive tests were compared between groups using Student’s t-test or Mann-Whitney-U-test according to the distribution of the numbers. Correlation between test results and cortical thickness was investigated by Spearman correlation. Since this study was exploratory, no correction for multiple testing was performed. An alpha of 0.05 was considered significant.
Results
Mean age of patients and control subjects was 67 (± 9.44) and 64 (± 8.36) years (p = 0.228). Of the 25 patients, 15 had a stenosis of the left carotid artery (cf. demographical table in the online Additional file 1: Table S1). Median degree of stenosis of the patient group was 80% (range 50–95%), all but one patient had stenosis ≥70%.
General linear mixed model
In the GLMM including 66 anatomical ROI, ROI (p < 0.001) and age (p = 0.002) showed a significant effect on cortical thickness, while no significant effect was observed for hemisphere, group, and presence of stenosis (see Table 1). After hierarchical stepwise-backward elimination of non-significant interactions, no significant interaction remained. Estimated mean cortical thickness was numerically lower in the in the hemisphere with upstream carotid stenosis (with stenosis: 2.354; without: 2.363 mm, p = 0.180).
In the second model including MCA and non-MCA regions, region (p < 0.001), hemisphere (p = 0.003), and age (p = 0.009) showed a significant effect on cortical thickness, while stenosis did not (see Table 2). Estimated mean cortical thickness was higher in the MCA region as compared to the non-MCA region (2.344 mm vs. 2.021 mm, p < 0.001). There was a significant interaction between presence of stenosis and region (p = 0.042). Estimated mean cortical thickness in the MCA region in the hemisphere with upstream carotid stenosis was numerically lower than without stenosis (2.332 mm vs. 2.355 mm, p = 0.111).
Cognitive tests
Stroop test C scores and TMT-B z scores were normally distributed for both groups. In the TMT B test, stenosis patients showed a trend towards lower Z-score values compared to controls (− 0.27 vs. 0.32, p = 0.054), indicating a longer time required and thus worse performance in the test. Regarding the Stroop test, patients had significant lower C-values (4.8 vs. 6.2, p = 0.010) indicating worse performance. Patients also achieved significantly worse test results for the CDT (1.52 vs. 1.04, p = 0.005) and DemTect (15.68 vs. 17.40, p = 0.009) (see Table 3). MMSE values were not normally distributed. Thus, a non-parametric test was used for group comparison. There was no significant difference between stenosis patients and controls (28.08 vs. 28.48, p = 0.375).
In patients, no significant correlation between performance in cognitive and cortical thickness across the whole hemisphere, or any of the hemispheres (left or right, stenosis or no-stenosis) was observed (data not shown). In control subjects there also was no significant correlation between cognitive test results and cortical thickness except for a moderate correlation between DemTect result and cortical thickness of the left hemisphere (Spearman’s rank correlation coefficient = 0.403, p = 0.046).
Discussion
In our study of patients with internal carotid artery stenosis without ischemic brain lesions, we did not observe significant alterations of cortical thickness in brain regions ipsilateral to the stenosis. While patients showed worse cognitive test performance than controls, there was no correlation of cognitive function and cortical thickness.
These results are in contrast to a recent study that reported a reduction of cortical thickness in the motor cortex of patients with carotid stenosis ≥80%, while no change of cortical thickness was detected in the visual cortex [12]. In the same patient cohort, a significant difference between cortical thicknesses on the side of stenosis versus non-stenosis side in M1 could be shown for the patients while this was not detectable in healthy controls [36]. A previous study also reported progressive brain atrophy measured by evaluation of brain volume associated with severe carotid stenosis in a longitudinal follow up of 4 years [37].
Worse performance of patients with carotid artery stenosis in cognitive tests in our study is in line with previous reports. Patients with either symptomatic or asymptomatic carotid stenosis showed worse results in cognitive tests than controls [19,20,21,22, 38], and lower MMSE scores were observed in patients with carotid stenosis ≥75% [14]. Findings from previous studies also support an association of grey matter volume and cognitive function independent from carotid stenosis. Smaller cortical gray matter volume was correlated with cognitive impairment, including among others tests for attention, memory and language and tests for executive performance [4, 39]. It was also hypothesized, that the association of brain volume and cognitive function might be mediated by cerebrovascular pathology including white matter lesions and brain infarcts30. We did not observe any meaningful correlation of cortical thickness with cognitive tests, although healthy controls achieved better results in the cognitive tests than stenosis patients. Other factors influencing cognitive function beyond cortical thickness may play a role leading to worse performance in patients, such as co-morbidities or vascular risk factors (cf., demographical data, Additional file 1: Table S1).
While cortical thickness provides important information on structural integrity of the brain, further techniques may be helpful to take into account other aspects of structural brain organization. In line with this, a study using diffusion tensor imaging observed reduced fractional anisotropy as a marker of white organization and diminished cognitive test results in patients with carotid stenosis [40]. The analysis of more complex parameters of brain structure including structural network organization may yield further insights into less pronounced structural sequelae of unilateral carotid stenosis and its interaction with cognitive function.
In our study, cortical thickness was associated with age, brain region, and hemisphere, which are well-described factors determining cortical thickness [5, 41]. We interpret the lack of obvious changes of cortical thickness in patents with carotid stenosis as an indicator of the robustness of the brain to chronic alterations of cerebral perfusion in the absence of ischemic brain lesions. Both, the network of collateral arteries and the mechanisms of neurovascular coupling may help render rain perfusion resilient and sufficient for maintaining the functional and structural metabolism within a wide range of changes to the cerebral blood flow. Only when focusing the analysis of cortical thickness changes in brain regions supplied by the middle cerebral artery, we observed an interaction of presence of stenosis and brain region, with slightly decreased cortical thickness in the MCA territory of brain hemispheres with upstream carotid stenosis. This interaction might indicate a small effect of unilateral carotid stenosis on cortical thickness beyond the effects age, brain region, and hemisphere. Our sample, however, may have been too small, to detect this small effect in the statistical model applied.
Conclusion
To summarize, in patients with carotid stenosis without ischemic brain lesions we observed neither significantly reduced cortical thickness nor an association of cortical thickness with cognitive function, although patients performed worse than healthy controls in cognitive tests. These data do not support the hypothesized association of cortical thinning and cognitive impairment in carotid stenosis. In contrast, our results demonstrate the robustness of brain structure to chronic changes of cerebral perfusion in the absence of focal stroke lesions. Future studies should take into account a wider range of clinical and imaging parameters when studying the effects of alterations of cerebral perfusion on brain structure and cognitive function.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CDT:
-
Clock drawing test
- CERAD:
-
Consortium to establish a registry for Alzheimer’s disease
- CI:
-
Confidence interval
- DemTect:
-
Dementia detection test
- FOV:
-
Field of view
- FWT:
-
Farb-Wort-test
- GLMM:
-
General linear mixed model
- IPR:
-
In-plane resolution
- MCA:
-
Middle cerebral artery
- MMSE:
-
Mini mental state examination
- MPRAGE:
-
Magnetization-prepared rapid acquisition gradient-echo
- n/a:
-
Not applicable
- NASCET:
-
North American symptomatic carotid Endarterectomy trial
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- ST:
-
Slice thickness
- TE:
-
Echo time
- TMT:
-
Trail making test
- TR:
-
Repetition time
References
Flaherty ML, Kissela B, Khoury JC, Alwell K, Moomaw CJ, Woo D, et al. Carotid artery stenosis as a cause of stroke. Neuroepidemiology. 2013;40(1):36–41.
Yuan G, Zhou S, Wu W, Zhang Y, Lei J, Huang B. Carotid artery stenting versus carotid Endarterectomy for treatment of asymptomatic Carotid Artery Stenosis. Int Heart J. 2018;59(3):550-8. https://doi.org/10.1536/ihj.17-312. Epub 2018 May 20. J [Internet]. 2018;1–9. Available from: https://www.jstage.jst.go.jp/article/ihj/advpub/0/advpub_17-312/_article%0A. http://www.ncbi.nlm.nih.gov/pubmed/29681577.
Moresoli P, Habib B, Reynier P, Secrest MH, Eisenberg MJ, Filion KB. Carotid stenting versus Endarterectomy for asymptomatic carotid artery stenosis: a systematic review and meta-analysis. Stroke. 2017;48(8):2150–7.
Kim HJ, Ye BS, Yoon CW, Noh Y, Kim GH, Cho H, et al. Cortical thickness and hippocampal shape in pure vascular mild cognitive impairment and dementia of subcortical type. Eur J Neurol. 2014;21(5):744–51.
Lemaitre H, Goldman AL, Sambataro F, Verchinski BA, Meyer-Lindenberg A, Weinberger DR, et al. Normal age-related brain morphometric changes: nonuniformity across cortical thickness, surface area and gray matter volume? Neurobiol Aging. 2012 Mar;33(3):617.e1–9.
Li Q, Pardoe H, Lichter R, Werden E, Raffelt A, Cumming T, et al. Cortical thickness estimation in longitudinal stroke studies: a comparison of 3 measurement methods. NeuroImage Clin. 2015;8:526–35.
Cardenas VA, Reed B, Chao LL, Chui H, Sanossian N, DeCarli CC, et al. Associations among vascular risk factors, carotid atherosclerosis, and cortical volume and thickness in older adults. Stroke. 2012 Nov 1;43(11):2865–70.
Jones PW, Borich MR, Vavsour I, Mackay A, Boyd LA. Cortical thickness and metabolite concentration in chronic stroke and the relationship with motor function. Restor Neurol Neurosci. 2016 Sep 21;34(5):733–46.
Zhang J, Meng L, Qin W, Liu N, Shi FD, Yu C. Structural damage and functional reorganization in Ipsilesional M1 in well-recovered patients with subcortical stroke. Stroke. 2014;45(3):788–93.
Cheng B, Schulz R, Bönstrup M, Hummel FC, Sedlacik J, Fiehler J, et al. Structural plasticity of remote cortical brain regions is determined by connectivity to the primary lesion in subcortical stroke. J Cereb Blood Flow Metab. 2015;35(9):1507–14.
Fierstra J, Poublanc J, Han JS, Silver F, Tymianski M, Crawley AP, et al. Steal physiology is spatially associated with cortical thinning. J Neurol Neurosurg Psychiatry. 2010;81(3):290–3.
Marshall RS, Asllani I, Pavol MA, Cheung Y, Lazar RM. Altered cerebral hemodyamics and cortical thinning in asymptomatic carotid artery stenosis. PLoS One [Internet]. 2017;12(12):e0189727. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29240808.
Avelar WM, D’Abreu A, Coan AC, Lima FO, Guimarães R, Yassuda CL, et al. Asymptomatic carotid stenosis is associated with gray and white matter damage. Int J Stroke. 2015;10(8):1197–203.
Johnston SC, O’Meara ES, Manolio TA, Lefkowitz D, O’Leary DH, Goldstein S, et al. Cognitive impairment and decline are associated with carotid artery disease in patients without clinically evident cerebrovascular disease. Ann Intern Med. 2004;140(4):237–47.
Balucani C, Viticchi G, Falsetti L. Cerebral hemodynamics and cognitive performance in bilateral asymptomatic carotid stenosis; 2012.
Mathiesen EB, Waterloo K, Joakimsen O, Bakke SJ, Jacobsen EA, Bønaa KH. Reduced neuropsychological test performance in asymptomatic carotid stenosis: the Tromsø study. Neurology. 2004 Mar 9;62(5):695–701.
Mendiz OA, Sposato LA, Fabbro N, Lev GA, Calle A, Valdivieso LR, et al. Improvement in executive function after unilateral carotid artery stenting for severe asymptomatic stenosis. J Neurosurg. 2012 Jan;116(1):179–84.
Landgraff NC, Whitney SL, Rubinstein EN, Yonas H. Cognitive and physical performance in patients with asymptomatic carotid artery disease. J Neurol. 2010 Jun 23;257(6):982–91.
Wang T, Xiao F, Wu G, Fang J, Sun Z, Feng H, et al. Impairments in brain perfusion, metabolites, functional connectivity, and cognition in severe asymptomatic carotid stenosis patients: an integrated MRI study. Neural Plast. 2017;2017:1–7.
Norling AM, Marshall RS, Pavol MA, Howard G, Howard V, Liebeskind D, et al. Is Hemispheric Hypoperfusion a Treatable Cause of Cognitive Impairment? Curr Cardiol Rep [Internet]. Current Cardiology Reports; 2019;21(1):4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30661122.
Alhusaini S, Karama S, Nguyen TV, Thiel A, Bernhardt BC, Cox SR, et al. Association between carotid atheroma and cerebral cortex structure at age 73 years. Ann Neurol. 2018;84(4):576–87.
Lal BK, Dux MC, Sikdar S, Goldstein C, Khan AA, Yokemick J, et al. Asymptomatic carotid stenosis is associated with cognitive impairment. J Vasc Surg. 2017;66(4):1083–92.
Rimmele DL, Larena-Avellaneda A, Alegiani AC, Rosenkranz M, Schmidt NO, Regelsberger J, et al. Real-world experience of treatment decision-making in carotid stenosis in a neurovascular board. Neurology. 2017;89(4):399–407.
Cohen S, Tyrrell D, Smith A. Beneficial effect of carotid Endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991 Aug 15;325(7):445–53.
Hathout GM, Fink JR, El-Saden SM, Grant EG. Sonographic NASCET index: a new doppler parameter for assessment of internal carotid artery stenosis. AJNR Am J Neuroradiol. 2005;26(1):68–75.
Fischl B. FreeSurfer. Neuroimage2. 2012;62(2):774–81.
Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage. 1999 Feb;9(2):179–94.
Fischl B, Dale AM. Measuring the thickness of the human cerebral cortex from magnetic resonance images. Proc Natl Acad Sci. 2000;97(20):11050–5.
Wu J, Ngo GH, Greve D, Li J, He T, Fischl B, et al. Accurate nonlinear mapping between MNI volumetric and FreeSurfer surface coordinate systems. Hum Brain Mapp. 2018;(April:1–16.
Fischl B, Sereno MI, Tootell RBH. Dale a M. high-resolution inter-subject averaging and a surface-based coordinate system. Hum Brain Mapp. 1999;8(FEBRUARY 1999):272–84.
Tatu LMD, Moulin TMD, Bogousslavsky JMD, Duvernoy HMD. Arterial territories of the human brain: cerebral hemispheres. Neurology. 1998;50(6):1699–708.
Mutsaerts HJMM, Richard E, Heijtel DFR, Van Osch MJP, Majoie CBLM, Nederveen AJ. Gray matter contamination in arterial spin labeling white matter perfusion measurements in patients with dementia. NeuroImage Clin. 2014;4:139–44.
Cheng B, Golsari A, Fiehler J, Rosenkranz M, Gerloff C, Thomalla G. Dynamics of regional distribution of ischemic lesions in middle cerebral artery trunk occlusion relates to collateral circulation. J Cereb Blood Flow Metab. 2011;31(1):36–40.
Ashendorf L, Jefferson A, Oconnor M, Chaisson C, Green R, Stern R. Trail making test errors in normal aging, mild cognitive impairment, and dementia. Arch Clin Neuropsychol. 2008 Feb 21;23(2):129–37.
Oswald WD, Fleischmann UM. Das Nürnberger-Alters-Inventar. 4th ed. Göttingen: Hogrefe; 1997.
Asllani I, Slattery P, Fafard A, Pavol M, Lazar RM, Marshall RS. Measurement of cortical thickness asymmetry in carotid occlusive disease. NeuroImage Clin. 2016;12:640–4.
Muller M, Van Der Graaf Y, Algra A, Hendrikse J, Mali WP, Geerlings MI. Carotid atherosclerosis and progression of brain atrophy: the SMART-MR study. Ann Neurol. 2011;70(2):237–44.
Jackson DC, Sandoval-Garcia C, Rocque BG, Wilbrand SM, Mitchell CC, Hermann BP, et al. Cognitive deficits in symptomatic and asymptomatic carotid Endarterectomy surgical candidates. Arch Clin Neuropsychol. 2016;31(1):1–7.
Muller M, Appelman APA, van der Graaf Y, Vincken KL, Mali WPTM, Geerlings MI. Brain atrophy and cognition: interaction with cerebrovascular pathology? Neurobiol Aging. 2011;32(5):885–93.
Cheng H-L, Lin C-J, Soong B-W, Wang P-N, Chang F-C, Wu Y-T, et al. Impairments in cognitive function and brain connectivity in severe asymptomatic carotid stenosis. Stroke. 2012;43(10):2567–73.
Luders E, Narr KL, Thompson PM, Rex DE, Jancke L, Toga AW. Hemispheric asymmetries in cortical thickness. Cereb Cortex. 2006;16(8):1232–8.
CERAD-Plus Online (https://www.memoryclinic.ch/de/main-navigation/cerad-plus/), of the Memory Clinic (Universitäre Altersmedizin, Felix Platter-Spital, Burgfelderstrasse 101, Postfach, 4002 Basel, Tel. +41 61 326 47 60, memoryclinic@fps-basel.ch).
Acknowledgements
Not Applicable.
Authors’contributions
AN1, SK, AN2, JS, CM, FF, MH, BC, JF, HP, AL, CG and GT made a substantial contribution to the concept and design, acquisition of data or analysis and interpretation of data, drafted the article or revised it critically for important intellectual content and approved the final version to be published.
Funding
This work was supported by the DFG, Sonderforschungsbereich (SFB) 936, Project C2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of the Hamburg chamber of physicians (PV4933). Written informed consent was obtained from all patients.
Consent for publication
Not applicable.
Competing interests
Dr. Gerloff reports grants from Deutsche Forschungsgemeinschaft (DFG), SFB 936, Projekt C1, grants from European Union 7th Framework Program, during the conduct of the study; personal fees from AMGEN, personal fees from Bayer Vital, personal fees from Abbott, personal fees from Prediction Biosciences, personal fees from BMS, personal fees from Boehringer Ingelheim, personal fees from Sanofi Aventis, outside the submitted work.
Dr. Larena-Avellaneda reports grants from Förderverein Herzzentrum, from null, outside the submitted work.
Dr. Thomalla reports grants from Deutsche Forschungsgemeinschaft (DFG), SFB 936, Projekt C2, during the conduct of the study; personal fees from Acandis, personal fees from Stryker, personal fees from Bayer, personal fees from Boehringer Ingelheim, personal fees from Daiichi Sankyo, from BristolMyersSquibb, outside the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. Demographic data stratified by group. Table S2. Beta values and 95% confidence interval for each region of interest. (DOCX 17 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nickel, A., Kessner, S., Niebuhr, A. et al. Cortical thickness and cognitive performance in asymptomatic unilateral carotid artery stenosis. BMC Cardiovasc Disord 19, 154 (2019). https://doi.org/10.1186/s12872-019-1127-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-1127-y