Abstract
Background
Metabolic syndrome (MetS) is a prevalent risk factor for coronary artery disease progression. Past studies have shown that MetS and its components tends to increase mortality after coronary artery bypass grafting (CABG), but data on the impact of MetS on postoperative outcome in patients with a left ventricular (LV) ejection fraction (EF) < 50% are still lacking.
Methods
Out of 2300 patients who underwent CABG between 2008 and 2018 in our center, 190 patients were identified as having impaired LV systolic function (EF < 50%). The patients were divided into two groups: those with MetS (n = 87, 45.8%) and those without MetS (n = 103, 54.2%). The influence of MetS on postoperative mortality and major complications was investigated.
Results
Postoperative mortality occurred in 12.6% of patients with MetS and in 3.9% of patients without MetS (p < 0.05). Multivariate analysis showed that patients with MetS had a significantly greater risk of mortality compared with patients without MetS (relative risk 7.23, p < 0.05). After adjustment for other risk factors, the risk of mortality was increased 6.47-fold [95% confidence interval (CI):1.25–33.6; p < 0.05] in patients with MetS and diabetes and 5.4-fold (95% CI: 1.12–29.7; p < 0.05) in patients with MetS and without diabetes, whereas it was not significantly increased in patients with diabetes and without MetS.
Conclusions
MetS is an important predictor of increased mortality in patients with LVEF<50% who undergo CABG. The components of MetS have synergistic effect in postoperative mortality. Multifactorial intervention in MetS is required to improve surgical efficacy in these patients.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) and obesity are increasingly prevalent in the population undergoing coronary artery bypass grafting (CABG), and these conditions are major factors in the development of metabolic syndrome (MetS) [1,2,3,4]. MetS is a clustering of risk factors, including obesity (especially visceral adiposity), diabetes or impaired glucose regulation, lipid disorders and increased blood pressure, that leads to a dramatic increase in the risk of cardiovascular disease (CVD) [5, 6]. CVD is the leading cause of death among the population with these risk factors [7]. Several studies have reported poor prognosis after myocardial infarction (MI) that might be triggered by the unfavorable effects of MetS on left ventricular (LV) function [8,9,10]. MetS may lead to greater infarct size, resulting in LV dysfunction [11]. Past clinical studies have demonstrated that MetS and its components are independent risk factor for operative morbidity and mortality after CABG surgery [6, 7, 12,13,14]. However, the prevalence of MetS among patients with LV ejection fractions (EF) < 50% who undergo CABG and the impact of MetS on postoperative clinical outcomes are still unknown. The aim of this retrospective study was to confirm the effects of MetS on patients with impaired LV systolic function after CABG surgery.
Materials and methods
Study population
Subjects were selected from a total of 2300 patients who underwent CABG at our institution between January 1, 2008, and May 31, 2018. Echocardiographic results were obtained within 2 weeks prior to surgery in all patients. Among these patients, we identified 200 patients who had an LVEF of 50% or less in preoperative echocardiographic evaluations. In all, 10 patients were excluded from the study because of missing data in our database. Of the included patients, 87 (45.8%) met the criteria for MetS and were referred to as the MetS group, and 103 patients (54.2%) who did not were referred to as the non-MetS group. This study was approved by our institutional Ethics Committee, which waived the requirement for informed patient consent because of the retrospective nature of the study.
Surgical technique
During the study period, a team of 9 surgeons performed the CABG procedures. The surgeons adopted different surgical strategies for CABG (off-pump vs. on-pump). On-pump CABG was preferred in patients with unstable hemodynamics or complicating valvular disease or other cardiac malformations. Median sternotomy was performed in all cases. The internal mammary artery (IMA) and/or saphenous vein were harvested using standard techniques.
For off-pump CABG, 3 traction sutures were placed in the posterior pericardium for retraction. Regional myocardial immobilization was achieved with a suction stabilizer (Guidant Axius Coronary Shunt, Guidant, CA, USA) during distal anastomosis, and intracoronary shunts (Chase Medical, Richardson, TX, USA) of appropriate sizes were used to maintain flow to the distal myocardium during the anastomosis. A nontraumatic small bulldog clamp was then applied to the target vessel proximal to the anastomotic site to achieve hemostasis after arteriotomy. For on-pump CABG, all procedures were performed through a standard cardiopulmonary bypass. When patients were cooled to 30 °C (moderate hypothermia), the ascending aorta was cross-clamped, and myocardial preservation was achieved with anterograde tepid blood cardioplegia. All anastomosis were constructed with a continuous-suture technique with 7–0 or 8–0 monofilament sutures.
After the operation, patients were taken to a dedicated cardiovascular intensive care unit (ICU). They were extubated if they met the following criteria: clear consciousness, hemodynamic stability, recovery of myodynamia and no significant bleeding.
Identification
Patients were considered to have MetS when 3 or more of the following 5 criteria were present, based on a modification of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (NCEP-ATP III): 1) obesity, defined as a body mass index (BMI) > 25 kg/m2 based on the established Chinese criteria for obesity; 2) fasting glycemia ≥6.1 mmol/l or treatment with oral hypoglycemics or insulin; 3) triglycerides ≥1.69 mmol/l; 4) high-density lipoprotein (HDL) cholesterol < 1.04 mmol/l in men and < 1.29 mmol/l in women; and 5) blood pressure > 130/85 mmHg or treatment with antihypertensive medication. The original criterion to classify obesity in the NCEP-ATP III was a waist circumference > 120 cm in men or > 88 cm in women, but this was not measured in this cohort; therefore, we used BMI. Recent studies have shown that most patients identified as having MetS based on BMI would also have been diagnosed as obese according to waist circumference [15, 16].
Perioperative myocardial infarction (MI) was defined as an increase in creatinine kinase-MB (CK-MB) to ≥10 times the upper limit of normal or ≥ 5times the upper limit of normal with new 30-ms Q waves within 24 h of surgery. The criterion for postoperative renal failure was defined as a need for dialysis to treat prolonged oliguria or anuria. The presence of a positive blood culture and signs and symptoms consistent with sepsis was used to define septicemia. Stroke was defined as central neurological deficit persisting for more than 72 h. Atrial fibrillation was defined as the occurrence of any atrial fibrillation during hospitalization. Low cardiac output syndrome (LCOS) was defined as the use of inotropic agents or intra-aortic balloon pump support, or both, to maintain a cardiac index > 2.0 L·min− 1·m2.
Statistical analysis
Continuous variables are described as the means ± standard deviation, and categorical data are expressed as frequencies and percentages. The data were analyzed using a chi-square test or Student’s t test. The association between operative mortality and the different risk factors was examined using logistic regression, and results are expressed as odds ratio (OR) with a 95% confidence interval (CI). Among risk factors, those with a P-value ≤0.05 were selected for the multivariate analyses. The multivariate models were constructed from the Hosmer-Lemeshow approach. A P value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 21.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
The demographic and operative data of the 2 groups are shown in Table 1, and the distribution of the NCEP-ATP III criteria used to define MetS is presented in Table 2. About 49.4% MetS patients do not have DM as part of their MetS criteria. There were no significant differences between the 2 groups for age, gender, various concomitant diseases, severity of coronary artery disease, operative data, echocardiographic findings or the new logistic EuroSCORE II (a measure of the operative risk). However, as expected, the rates of DM, hypertension and obesity were significantly higher in patients with MetS than in those without MetS (P < 0.05 for each comparison). Patients with MetS exhibited significantly higher fasting glycemia, hyperuricemia, and plasma triglyceride levels than those without MetS. Moreover, there was a significant difference in the number of patients with NYHA heart failure class III/IV between the 2 groups. The mean number of anastomoses was 2.50 ± 0.93 in the non-MetS group and 2.75 ± 0.89 in the MetS group (P = 0.059).
Morbidity and mortality
Postoperative morbidity and mortality are presented in Table 3. The overall in-hospital mortality rate was 7.9 (15 of 190 patients). There were statistically significant differences between the 2 groups in the rates of in-hospital mortality, acute renal failure, ventricular fibrillation, septicemia and new intra-aortic balloon pump (IABP) insertion (all p values < 0.05). There was a trend toward higher rates of prolonged ventilation in MetS patients (9.2% vs. 3.9%, p = 0.05), but it did not reach statistical significance.
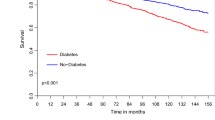
In univariate analysis, MetS was associated with a 3.58-fold increase in the risk of mortality. There was no indication of a cumulative effect in relation to the number of NCEP-ATP III components of MetS (Fig. 1). Among the other risk factors, an age > 70, history of stroke, preoperative renal dysfunction, patients with NYHA class III/IV, urgent or emergent operative status, on-pump bypass surgery and the new logistic EuroSCORE II were significantly associated with higher in-hospital mortality rates (Table 4).
In multivariate logistic regression analysis, the presence of MetS was strongly associated with an increased incidence of in-hospital mortality (OR: 5.99, 95% CI: 1.02–35.15, P = 0.047). Ages > 70 were also independent predictors of in-hospital mortality (Table 5). However, DM, hypertension, obesity, and the 5 components of MetS included in the NCEP-ATP III definition did not increase mortality after CABG during hospitalization (all P values < 0.05). In patients without DM, MetS was associated with higher risk of mortality whether DM was part of MetS or not (11.6% vs. 2.4%; p = 0.044), while in diabetes patients MetS was not associated with higher risk (13.6% vs. 10.5%; p = 0.73). Table 6 presents the causes of death. Deaths of cardiac origin accounted for 40% of the deaths. There were no significant differences with respect to the causes of death among patients with or without MetS.
Discussion
MetS increases the risk of developing coronary artery disease (CAD) and is also more prevalent among patients who undergo CABG. MetS has been reported to occur in up to 13% of the general population in China [17]. However, in our study, the prevalence of MetS of 45.8% was consistent with that of previous studies in which MetS and CABG were investigated [5, 12, 18].
Several studies have reported an association between postoperative outcomes and MetS [6, 7, 12, 13, 18]. According to these studies, patients with MetS have increased risks morbidity and mortality after CABG, both overall and from CVD. One of the negative effects of MetS is a change in the structure and function of the left ventricle [19]. As Azevedo et al. found, increased severity of MetS is associated with increasingly compromised structure and function of the heart [20]. Yazicio et al. also reported that more severely impaired LV systolic function after acute MI may contribute to the higher morbidity and mortality observed in patients with MetS [10]. However, whether MetS still has an adverse effect on postoperative prognosis among patients with LV dysfunction who undergo CABG has not been demonstrated. This is the first study to delineate the role of MetS in operative mortality and complications in these patients. In our study, we found that, in line with previous reports, MetS is an important predictor for higher operative morbidity and mortality in CABG patients with impaired LV systolic function.
The components of MetS, such as diabetes, hypertension and obesity, have been reported to be associated with a higher incidence of operative mortality after CABG. When analyzing 41,663 patients with diabetes, Carson JL et al. found increased morbidity and morbidity after CABG in diabetic patients during hospitalization when compared with nondiabetic patients [4]. Despite the lack of convincing evidence in the literature, obesity is often considered to be a significant risk factor for postoperative mortality when selecting candidates for CABG [21,22,23]. Moulton et al. concluded that those with a history of hypertension have an increased frequency of immediate post-operative complications and an increased 2-year mortality after CABG [24]. Aronson S et al. also reported that isolated systolic hypertension is associated with increased perioperative cardiovascular morbidity in coronary artery surgery patients [25]. However, patients with DM, obesity and hypertension did not have increased morbidity and mortality independently in our study. The discordant results may result from disagreement among the criteria adopted or the characteristics of the populations and the methodological strategies used.
We also found the presence of both MetS and DM significantly increased the risk of operative mortality among patients with impaired LV systolic function, whereas patients without MetS were not at higher risk. These results demonstrated that the effect of MetS on operative mortality was not a single effect of DM, but the aggregation of multiple factors, such as hypertension, hyperglycemia, and obesity, which acted as a combined risk factor for operative mortality. The clustering of cardiovascular risk factors in MetS demonstrated that the multiple complex metabolic reactions involved in glycotoxicity, lipotoxicity, altered insulin signaling, increased cytokine activity and interstitial deposition of triacylglycerol may directly or indirectly impact myocardial function, and then reduce survival in MetS patients with LVEF<50%. Moreover, we found that the distributions of the causes of death were similar among patients with or without MetS, and about 40% deaths were of cardiac origin. Regarding postoperative complications, there were differences in the percentages of patients with ventricular fibrillation, septicemia and renal failure after CABG between the two groups.
This study provides further evidence that MetS is a prevalent and important risk factor for operative mortality after CABG in patients with impaired with LV systolic function. Furthermore, the components of MetS have synergistic effect in postoperative mortality among patients with EF<50%. These findings have major clinical implications. For instance, multifactorial intervention in patients with MetS who are referred to CABG is required for improving poor prognosis, including optimal control of lipids, blood pressure, blood glucose and body weight. It should be noted, however, that many patients with MetS are not being treated appropriately [12]. There is a definite need for clinics to focus on developing tools to reduce conditions associated with MetS. These tools include early identification, education, lifestyle modifications, and pharmacological interventions. In addition, the identification of MetS might be helpful for classifying high-risk patients, improving risk stratification for CABG patients and assessing the prognosis of CVD. Further large-scale and long-term studies are needed to determine whether MetS is responsible for the increased mortality after CABG surgery, especially in patients with impaired LV systolic function. Further studies are needed to determine whether perioperative medications might be effective in reducing mortality in MetS patients after CABG surgery. In addition, Further studies are necessary to clarify the mechanisms that the components of MetS work synergistically to increase the risk of operative mortality.
Limitations
This was a retrospective single-center study on ethnic Chinese patients. Its retrospective nature and the small number of patients limit the validity of the clinical outcome. However, the use of specific statistical evaluations enabled relatively precise risk and outcome assessments and comparisons. Although larger samples would be needed to produce more accurate and convincing results, we believe that our study already presents interesting findings related to postoperative outcomes. In addition, because waist circumference data were not available, we selected a BMI > 25 kg/m2 as the cutoff point for obesity based on the results of a previous study on the relationship between BMI, waist circumference, and obesity in a Chinese population. If waist circumstances had been used to define obesity in the detection of MetS, more specific results might have been obtained.
Conclusions
In conclusion, patients with MetS have a higher risk for operative mortality in patients with impaired LV systolic function who undergo CABG. The components of MetS, such as diabetes, hypertension and obesity did not increase operative mortality independently in our study. The effect of MetS on operative mortality was the aggregation of multiple factors, which work synergistically to increase the risk of operative mortality. In addition, the identification of MetS might be helpful for classifying high-risk patients, improving risk stratification for CABG patients with LVEF<50% and assessing the prognosis of CVD.
Abbreviations
- BMI:
-
Body mass index
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CK-MB:
-
Creatinine kinase-MB
- COPD:
-
Chronic obstructive pulmonary disease
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- EF:
-
Ejection fractions
- EuroSCORE:
-
European system for cardiac operatic risk evaluation
- HDL:
-
High-density lipoprotein
- IABP:
-
Intra-aortic balloon pump
- ICU:
-
Intensive care unit
- IMA:
-
Internal mammary artery
- LCOS:
-
Low cardiac output syndrome
- LDL:
-
Low-density lipoprotein
- LV:
-
Left ventricular
- MetS:
-
Metabolic syndrome
- MI:
-
Myocardial infarction
- NCEP-ATP III:
-
National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults
- NYHA:
-
New York Heart Association
- PCI:
-
Percutaneous coronary intervention
- RRs:
-
Relative risks
- SD:
-
Standard deviation
References
Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah A. Effects of obesity and small body size on operative and long-term outcomes of coronary artery bypass surgery: a propensity-matched analysis. Ann Thorac Surg. 2005;79(6):1976–86.
Herlitz J, Malmberg K, Karlson BW, Ryden L, Hjalmarson A. Mortality and morbidity during a five-year follow-up of diabetics with myocardial infarction. Acta Med Scand. 1988;224:31–8.
Wigfield CH, Lindsey JD, Munoz A, Chopra PS, Edwards NM, Love RB. Is extreme obesity a risk factor for cardiac surgery? An analysis of patients with a BMI≥40. Eur J Cardiothorac Surg. 2006;29(4):434–40.
Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schneider SH. Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol. 2002;40:418–23.
Hong S, Youn YN, Yoo KJ. Metabolic syndrome as a risk factor forPostoperative kidney injury after off-pump coronary artery bypass surgery. Circ J. 2010;74:1121–6.
Ardeshiri M, Faritus Z, Ojaghi-Haghighi Z, Bakhshandeh H, Kargar F, Aghili R. Impact of metabolic syndrome on mortality and morbidity after coronary artery bypass grafting surgery. Res Cardiovasc Med. 2014;3(3):e20270.
Ao H, Xu F, Wang X, Tang X, Zheng Z, Hu S. Effects of metabolic syndrome with or without obesity on outcomes after coronary artery bypass graft. A cohort and 5-year study. PLoS One. 2015;10(2):e0117671.
Wong CY, O’Moore-sullivan T, Fang ZY, Haluska B, Leano R, Marwick TH. Myocardial and vascular dysfunction and exercise capacity in the metabolic syndrome. Am J Cardiol. 2005;96(12):1686–91.
Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683–9.
Yazici HU, Poyraz F, Turfan M, Sen N, Tavil Y, Tulmac M, et al. The prevalence of the metabolic syndrome and its impact on the left ventricular systolic function in the patients with non-diabetic first ST elevation myocardial infarction. Eur Rev Med Pharmacol Sci. 2012;16(1):90–5.
Pimenta E, Passarelli O Jr, Borelli F, Sousa MG, Gun C, Amato V, et al. Metabolic syndrome in patients undergoing coronary artery bypass graft: prevalence and a marker of morbidity/mortality during hospitalization and 30 days after hospital discharge. Arq Bras Cardiol. 2007;88(4):413–7.
Echahidi N, Pibarot P, Després JP, Daigle JM, Mohty D, Voisine P, et al. Metabolic syndrome increases operative mortality in patients undergoing coronary artery bypass grafting surgery. J Am Coll Cardiol. 2007;50(9):843–51.
Swart MJ, De Jager WH, Kemp JT, Nel PJ, Van Staden SL, Joubert G. The effect of the metabolic syndrome on the risk and outcome of coronary artery bypass graft surgery. Cardiovasc J Afr. 2012;23(7):400–4.
Ozyazicioglu A, Yalcinkaya S, Vural AH, Yumun G, Bozkurt O. Effects of metabolic syndrome on early mortality and morbidity in coronary artery bypass graft patients. J Int Med Res. 2010;38(1):202–7.
Wong ND, Sciammarella MG, Polk D, Gallagher A, Miranda-Peats L, Whitcomb B, et al. The metabolic syndrome, diabetes and subclinical atherosclerosis assessed by coronary calcium. J Am Coll Cardiol. 2003;41(9):1547–53.
Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med. 2002;162(18):2074–9.
Cheng TO. Metabolic syndrome in China. Circulation. 2004;109(14):e180.
Brackbill ML, Sytsma CS, Sykes K. Perioperative outcomes of coronary artery bypass grafting: effects of metabolic syndrome and patient's sex. Am J Crit Care. 2009;18(5):468–73.
Tadic M, Ivanovic B, Kostic N, Simic D, Matic D, Celic V. Metabolic syndrome and left ventricular function: is the number of criteria actually important? Med Sci Monit. 2012;18(5):CR282–9.
Azevedo A, Bettencourt P, Almeida PB, Santos AC, Abreu-Lima C, Hense HW, et al. Increasing number of components of the metabolic syndrome and cardiac structural and functional abnormalities-cross-sectional study of the general population. BMC Cardiovasc Disord. 2007;7:17.
Birkmeyer NJ, Charlesworth DC, Hernandez F, Leavitt BJ, Marrin CA, Morton JR, et al. Obesity and risk of adverse outcomes associated with coronary artery bypass surgery. Northern New England cardiovascular disease study group. Circulation. 1998;97:1689–94.
Parsonnet V, Dean D. Bernstein AD. A method of uniform stratification of risk for evaluating the results of surgery in acquired adult heart disease. Circulation. 1989;79:3–12.
Kuduvalli M, Grayson AD, Oo AY, Fabri BM, Rashid A. The effect of obesity on mid-term survival following coronary artery bypass surgery. Eur J Cardiothorac Surg. 2003;23(3):368–73.
Herlitz J, Brandrup-Wognsen G, Haglid M, Hartford M, Emanuelsson H, Karlson BW, et al. Mortality and morbidity during a period of 2 years after coronary artery bypass surgery in patients with and without a history of hypertension. J Hypertens. 1996;14(3):309–14.
S A, Boisvert D, Lapp W. Isolated systolic hypertension is associated with adverse outcomes from coronary artery bypass grafting surgery. Anesth Analg. 2002;94(5):1079–84.
Acknowledgements
None.
Funding
None.
Availability of data and materials
The data of this study will not be shared publically because they will be applied for further researches of this series. But authors do agree that the data can be shared individually if requested.
Author information
Authors and Affiliations
Contributions
All authors take responsibility for the integrity of the data, the accuracy of the data analysis and the revise of the manuscript. SC, JL and QL participated in the study design. XW and JL participated in the acquisition of data. SC drafted the manuscript. LC, QL and XW conceived of the study, participated in its design and coordination, revised the paper and obtained funding. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Institutional Ethics Committee of Xiehe Hospital. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, S., Li, J., Li, Q. et al. Metabolic syndrome increases operative mortality in patients with impaired left ventricular systolic function who undergo coronary artery bypass grafting: a retrospective observational study. BMC Cardiovasc Disord 19, 25 (2019). https://doi.org/10.1186/s12872-019-1004-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-1004-8