Abstract
Background
Atrial fibrillation (AF) may result in procedure cancellations and emergency department (ED) referrals for patients presenting for outpatient GI endoscopic procedures. Such cancellations and referrals delay patient care and can lead to inefficient use of resources.
Methods
All consecutive patients presenting in AF for a colonoscopy or upper endoscopy to the University of Wisconsin Digestive Health Center between October 2013 and September 2014 were defined as the pre-intervention group (Group 1). In 2015, a protocol was initiated for peri-procedural management of patients presenting in AF, new onset or previously known. All consecutive patients after initiation of the protocol from October 2015 to September 2016 were analyzed as the post intervention group (Group 2). Patients with heart failure, hypotension, or chest pain were excluded from the protocol.
Results
One hundred nine and 141 patients were included in Groups 1 and Group 2, respectively. Following protocol initiation, patients were less likely to present to the ED (6.4% Group 1 vs. 1.4% Group 2, RR 0.22, p = 0.04). There was also a trend towards a reduction in procedure cancelations (5.5% Group 1 vs. 1.4% Group 2, RR 0.26, p = 0.08). All attempted procedures were completed and there were no complications in the intervention group.
Conclusions
Implementation of a standardized protocol for management of atrial fibrillation in patients presenting for outpatient gastrointestinal endoscopic procedures resulted in a significant decrease in emergency department visits with an additional trend toward decreased procedural cancellations without an increased risk of complications.
Similar content being viewed by others
Background
Atrial fibrillation (AF) is one of the most common cardiac arrhythmias, impacting approximately 2.7 to 6 million people in the United States (U.S.) and the prevalence is increasing [1]. An estimated 6 billion dollars is spent annually in the U.S. as a result of AF with inpatient admissions and emergency departments (ED) visits, accounting for the bulk of expenses [2, 3]. Several studies have demonstrated that protocol-driven ED management of AF may decrease admissions, length of stay and costs [4,5,6,7,8,9,10]. However, there is a paucity of evidence with respect to the usefulness of AF management protocols in non-acute care or procedural settings. The discovery of AF by non-Cardiology providers may result in unnecessary procedure cancellations and ED referrals. Approaches to safely manage these patients during such procedures may not only improve quality of patient care but also reduce AF related costs.
At our institution, we initiated a protocol to manage patients with AF presenting for outpatient gastrointestinal (GI) endoscopic procedures. The aim of the protocol was to effectively rate control patients peri-procedurally in order to allow for procedure completion. Once the procedure was complete, communication and follow up with the patient’s primary physician was established to avoid ED referrals.
Methods
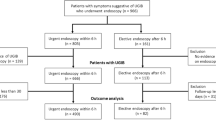
All consecutive outpatients presenting with AF at the time of upper or lower endoscopies at the University of Wisconsin Digestive Health Center were included in the study. Patients presenting between October 2013 and September 2014 were defined as the pre-intervention group. A protocol for peri-procedural management of patients in AF was implemented in August of 2015 (Fig. 1). Patients presenting between October 2015 and September 2016 were defined as the intervention group. Patients with both new onset and known AF were included. Patients were excluded if they exhibited clinical heart failure symptoms, hypotension, or chest pain at the time of index GI procedure. The primary outcome was rate of ED referral or procedural cancellation. Secondary outcome was procedural complications. The follow-up period was 30 days after the scheduled index GI procedure.
All data are reported as mean ± SD for continuous variables and frequencies for categorical data. Continuous variables were compared by unpaired or paired two-tail t-test as appropriate. Categorical variables were compared using χ tests. The Fisher exact test was used to compare proportions. Statistical analyses were performed using R version 3.3.3 (2017-03-06). A p-value of < 0.05 was considered to be significant. In accordance with federal regulations, this project did not constitute research as defined under 45 CFR 46.102(d). Therefore, this project did not require IRB review.
Results
Study population
One-hundred nine patients were included in the pre-intervention group (Group 1) and 141 were included in the intervention group (Group 2). The overall incidence of AF in patients presenting for outpatient endoscopy was approximately 1%. No patients were excluded from the study and 30-day follow-up data was available on all patients. Analysis of baseline demographics did not show any statistically significant differences between the two groups (Table 1).
Patient outcomes
Following protocol implementation, there was a statistically significant reduction in ED referrals for patients presenting with AF at the time of the GI procedure (6.4% Group 1 vs. 1.4% Group 2; p = 0.04). Additionally, there was a trend towards reduced procedural cancellations (5.5% Group 1 vs. 1.4% in Group 2; p = 0.08). There was also a trend towards more frequent administration of AV nodal blocking agents after algorithm implementation (0.9% Group 1 vs. 2.8% Group 2; p = 0.28). There was no significant difference in incidence of new AF between groups (7% in Group 1 vs 11% in Group 2; p = 0.37). Five patients in Group 1 developed complications during the procedure including bradycardia in absence of additional nodal blocking agents (2), bowel perforation (1), g-tube malfunction (1), and hypoglycemia (1). No patients in Group 2 developed complications (Table 2).
Post-procedure follow-up
All patients with new AF in Group 1 were seen by a provider within 30 days of the procedure vs. 73.3% of patients in Group 2. For those patients who were referred to the ED, 43% in Group 1 were admitted to the hospital versus all patients in Group 2. There was no difference in length of hospital stay between the two groups. There was no difference in the percentage of patients with CHA2DS2VASc ≥ 2 between Group 1 and Group 2 (84.4% vs. 83.7%; p = 0.89). There was no significant difference in anticoagulation rates in patients with a CHA2DS2VASc ≥ 2 between the groups (71.7% Group 1 vs. 76.9% Group 2; p = 0.20). For patients with newly diagnosed AF at the time of their procedure, there was no significant difference in anticoagulation rates in patients with a CHA2DS2VASc ≥ 2 between the two groups 30 days post procedure (66.7% Group 1 vs. 50.0% Group 1; p-0.53 (Table 3)).
Discussion
The present study supports the safety and efficacy of a protocol to manage AF in the outpatient GI endoscopy setting. Not only was there a significant decrease in the number of patients referred to the ED following algorithm implantation, but there was also a trend towards decreased procedural cancellations without an increase in adverse events.
Many patients presenting with asymptomatic or minimally symptomatic AF can be safely managed in the outpatient setting. However, the comfort level may be lower for management of AF by non-cardiology subspecialties and therefore can result in unnecessary referral to the ED or urgent care facilities as well as cancellation of procedures. Armed with a protocol developed in collaboration with cardiovascular specialists, GI providers had increased comfort levels to continue the planned procedures and then arrange for outpatient follow-up for those patients presenting in AF. As shown in the analysis, a sizeable percentage of the AF patients were newly diagnosed at the time of their GI procedure. There has been an increased awareness of the substantial incidence of subclinical AF in older patients through systematic screening efforts [11, 12]. Patients presenting for outpatient GI procedures often have continuous telemetry, pulse oximetry and vitals that lead to the recognition of AF in patients otherwise not undergoing screening and therefore serves as a potential source of newly diagnosed AF. As our study demonstrates, there is a significant number of patients presenting for endoscopies with previously undiagnosed AF. This study provides data to support performing GI endoscopies for patients with newly diagnosed asymptomatic or minimally symptomatic AF. Moreover, patients undergoing outpatient colonoscopies typically present after undergoing a bowel preparation and thus cancellations of these procedures can be burdensome for patients.
Formalized protocols have the ability to standardize care and reduce unnecessary healthcare utilization. In the ED setting, several studies have shown that use of AF management protocols are successful in reducing hospital admissions without increasing adverse events [4, 5, 7, 9, 10, 13]. The present study is the first of its kind to support the report the implementation of an algorithm for management of patients with AF in a setting outside of the ED. The outpatient GI setting was chosen owing to the inherent low procedural risks and short procedural duration. Protocols such as the one used in this study could be applied to other low risk outpatient arenas to improve quality of care for AF patients.
There are several limitations of our study. First, we used a retrospective control group which carries the potential for diagnostic and treatment differences. However, it is unlikely that within the overall time period that management would significantly differ and both the nursing and physician personnel were unchanged during this study period. Second, this is a single center study with a relatively small cohort of patients. Thus, the study may be underpowered to evaluate true differences seen as trends with respect to procedural cancellations and administration of AV nodal blocking agents. Third, concern exists about spontaneous cardioversion to sinus rhythm in individuals with a CHA2DS2VASc ≥ 2 who are not on anticoagulation during a procedure and have newly diagnosed AF. AF guidelines recommend long-term anticoagulation in those patients [2, 6, 14]. While data has shown that bridging anticoagulation in peri-procedural settings is not necessary, there is a lack of data regarding risk of spontaneous cardioversion during endoscopic procedures, and future investigation of this topic may aid further understanding of this risk [15]. Notably, no complications from thromboembolic events were noted during the study period. Lastly, our study did not evaluate the potential cost savings with the associated decreased ED referrals and procedural cancelations.
To assess generalizability, this study would ideally be followed by a multicenter study with a larger cohort of patients. Additionally, changes to the protocol to help facilitate appropriate anticoagulation in patients with newly diagnosed AF could help reduce morbidity and mortality.
Conclusions
Implementation of a novel protocol for AF management during outpatient GI procedures decreased ED referrals with a trend towards decreased procedural cancellations without any direct adverse events. Such protocols provide a practical method for non-cardiac specialists to manage patients with cardiovascular problems and reduce unnecessary healthcare utilization. This is the first study to support use of an algorithm to manage patients with AF in low risk ambulatory procedural settings.
Abbreviations
- AF:
-
Atrial Fibrillation
- CAD:
-
Coronary Artery Disease
- DBP:
-
Diastolic Blood pressure
- ED:
-
Emergency Department
- EF:
-
Ejection Fraction
- GI:
-
Gastrointestinal
- HR:
-
Heart Rate
- HTN:
-
Hypertension
- SBP:
-
Systolic Blood Pressure
- U.S.:
-
United States
References
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146–603.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, et al. 2014 AHA/ACC/HRS guideline for the Management of Patients with Atrial Fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):2071–104.
Kim MH, Johnston SS, Chu B-C, Dalal MR, Schulman KL. Estimation of Total incremental health care costs in patients with atrial fibrillation in the United States. Circ Cardiovasc Qual Outcomes. 2011;4(3):313–20.
Decker WW, Smars PA, Vaidyanathan L, Goyal DG, Boie ET, Stead LG, et al. A prospective, randomized trial of an emergency department observation unit for acute onset atrial fibrillation. Ann Emerg Med. 2008;52(4):322–8.
Domanovits H, Schillinger M, Thoennissen J, Nikfardjam M, Janata K, Brunner M, et al. Termination of recent-onset atrial fibrillation/flutter in the emergency department: a sequential approach with intravenous ibutilide and external electrical cardioversion. Resuscitation. 2000;45(3):181–7.
Hauser TH, Pinto DS, Josephson ME, Zimetbaum P. Safety and feasibility of a clinical pathway for the outpatient initiation of antiarrhythmic medications in patients with atrial fibrillation or atrial flutter. Am J Cardiol. 2003;91(12):1437–41.
Kim MH, Morady F, Conlon B, Kronick S, Lowell M, Bruckman D, et al. A prospective, randomized, controlled trial of an emergency department–based atrial fibrillation treatment strategy with low-molecular-weight heparin. Ann Emerg Med. 2002;40(2):187–92.
Naccarelli GV, Dell’Orfano JT, Wolbrette DL, Patel HM, Luck JC. Cost-effective management of acute atrial fibrillation: role of rate control, spontaneous conversion, medical and direct current cardioversion, transesophageal echocardiography, and antiembolic therapy. Am J Cardiol. 2000;85(10):36–45.
Tran C, Bennell MC, Qiu F, Ko DT, Singh SM, Dorian P, et al. Predictors and clinical outcomes of inpatient versus ambulatory management after an emergency department visit for atrial fibrillation: a population-based study. Am Heart J. 2016;173:161–9.
Zimetbaum P, Reynolds MR, Ho KKL, Gaziano T, McDonald MJ, McClennen S, et al. Impact of a practice guideline for patients with atrial fibrillation on medical resource utilization and costs. Am J Cardiol. 2003;92(6):677–81.
Engdahl J, Andersson L, Mirskaya M, Rosenqvist M. Stepwise screening of atrial fibrillation in a 75-year-old PopulationClinical perspective: implications for stroke prevention. Circulation. 2013;127(8):930–7.
Healey JS, Alings M, Ha A, Leong-Sit P, Birnie DH, de Graaf JJ, et al. Subclinical atrial fibrillation in older patients. Circulation. 2017;136(14):1276–83.
Bellew SD, Bremer ML, Kopecky SL, Lohse CM, Munger TM, Robelia PM, et al. Impact of an emergency department observation unit management algorithm for atrial fibrillation. J Am Heart Assoc. 2016;5(2):e002984.
Macle L, Cairns J, Leblanc K, Tsang T, Skanes A, Cox JL, et al. 2016 focused update of the Canadian cardiovascular society guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2016;32(10):1170–85.
Douketis JD, Spyropoulos AC, Kaatz S, Becker RC, Caprini JA, Dunn AS, et al. Perioperative bridging anticoagulation in patients with atrial fibrillation. N Engl J Med. 2015;373(9):823–33.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
All authors were involved in study design and data acquisition. AC, JL, and MMK analyzed and interpreted patient data. JL, JMW, MEF and MMK were major contributors in drafting the manuscript. All authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and consent was not required as the study was designated QI by the ITB Research determination tool.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Longino, J., Chaddha, A., Kalscheur, M.M. et al. Impact of a novel protocol for atrial fibrillation management in outpatient gastrointestinal endoscopic procedures: a retrospective cohort study. BMC Cardiovasc Disord 18, 179 (2018). https://doi.org/10.1186/s12872-018-0915-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-018-0915-0