Abstract
Background
In the present study, the association of the cardio-metabolic risk factors and the status of single-child family were studied in a national representative sample of Iranian children and adolescents.
Methods
This cross sectional study was conducted as the fifth round of “Childhood and Adolescence Surveillance and PreventIon of Adult Non- communicable disease” surveys. The students’ questionnaire was derived from the World Health Organization-Global School Student Health Survey. Using survey data analysis methods, data from questionnaires’; anthropometric measures and biochemical information analyzed by logistic regression analysis.
Results
Overall, 14,274 students completed the survey (participation rate: 99%); the participation rate for blood sampling from students was 91.5%. Although in univariate logistic regression model, single child students had an increased risk of abdominal obesity [OR: 1.37; 95% CI: 1.19–1.58)], high SBP [OR: 1.58; 95% CI:1.17–2.14)], high BP [OR: 1.21; 95% CI:1.01–1.45)] and generalized obesity [OR: 1.27; 95% CI:1.06–1.52)], in multiple logistic regression model, only association of single child family with abdominal obesity remained statistically significant [OR: 1.28; 95% CI:1.1–1.50)]. Also in multivariate logistic regression model, for each increase of a child in the family the risk of abdominal obesity [OR: 0.95; 95% CI: 0.91–0.97), high SBP [OR: 0.88; 95% CI: 0.81–0.95)] and generalized obesity [OR: 0.95; 95% CI: 0.91–0.99)] decreased significantly.
Conclusion
The findings of this study serve as confirmatory evidence on the association of cardio-metabolic risk factors with single-child family in children and adolescents. The findings of study could be used for better health planning and more complementary research.
Similar content being viewed by others
Background
Over the past decade, the global pattern of diseases has significantly shifted from communicable diseases to the non-communicable diseases (NCDs). This concern mainly rooted in epidemiological transition and rapid changes in lifestyle [1]. Considering the behavioral and biological related risk factors, the backgrounds of childhood NCDs is well documented [2].
More than three-quarters of Cardio Vascular Disease (CVD) deaths occur in low and middle-income countries [3]. Through past three decades, we were witnessing an epidemic of obesity in the world among the children and adolescents [4] has been reported the significant increase in waist circumference (WC), low density lipoprotein (LDL), triglyceride (TG), blood pressure (BP), metabolic syndrome (MetS) and the reduction in high density lipoprotein (HDL) among the adolescents in some countries [5, 6]. In children and teens of developing countries such as Iran and Turkey, it has been shown that the most common factors of MetS are high TG and low HDL [7].
Most of these adverse health outcomes could be prevented by addressing the environmental risk factors such as using tobacco, unhealthy diet and obesity, physical activity, alcohol consumption and harms of using broad population strategies [3].
As another related important point, following the demographic transitions happened in most countries in the world, there has been observed the fertility reduction and changes in family structures [8]. As a result, the numbers of the households have been decreases and the single-child families have been increased [8]. In Iran, such reduction was observed both in urban area and rural areas [9]. The impact of family structure on cardio- metabolic risk factors discussed in many previous attempts. Results of a study showed that, compared to single child, children who are siblings, have more daily physical activity [10, 11]. The association of some of cardio-metabolic risk factors assessed through some scattered studies [12, 13].
Despite the priority of the problem, yet there is an evident gap in the related evidence. Many studies have investigated the association between the cardio- metabolic risk factors and the family structure [14, 15], but due to our knowledge, there is not any research on the association of the cardio- metabolic risk factors and the status of single-child families Therefore, the present study was designed to examine the associations of the single-child family associated with cardio-metabolic risk factors in Iranian children and adolescents.
Methods
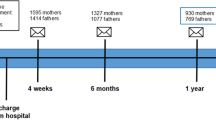
Aim to assess the association between the cardio- metabolic risk factors and the status of single-child family we analyzed the data of comprehensive national survey of CASPIAN-V study was conducted in 2015. Using multistage, stratified cluster sampling method, the study participants selected from, students aged 7–18 years of primary and secondary schools, of urban and rural areas of 30 provinces of Iran. Proportional to size sampling within each province was conducted according to the student’s place of residence (urban or rural) and level of education (primary and secondary) with equal sex ratio. Details on the methodology have been presented before [16], and here we report it in brief.
An expert team of trained health care professionals involved to processes of data gathering. After identifying eligible students, the mission and purpose of the interview was explained. Following informed consent, through interview with students and their parents, specific questionnaires were completed. These questionnaires were extracted from the World Health Organization-Global School Student Health Survey (WHO-GSHS) [17]. Their validity and reliability of Persian-translated questionnaires were confirmed previously [18]. More than demographic information, many aspects of life skills, health behaviors and history of diseases targeted through these questioners [16].
At the next step, by using calibrated instruments, the physical measurements conducted under the standard protocols [17]. During Anthropometric measurements; weight was measured to the nearest 0.1 kg with wearing a light cloth, and height were measured without shoes to the nearest 0.1 cm. Body mass index (BMI) calculated by dividing weight to height squared (m2). Using a non-elastic tape, WC was measured at a point midway between the lower border of the rib cage and the iliac crest at the end of normal expiration to the nearest 0.1 cm. Hip circumference was measured, to the nearest 0.1 cm, at the widest part of the hip at the level of the greater trochanter [18].
Blood pressure measured in sitting position, on the right arm, using a mercury sphygmomanometer with an appropriate cuff size. It was measured 2 times at 5-min intervals and the average was registered [19]. BMI categories considered based on he WHO growth curves; to define underweight as age and sex-specific BMI < 5th, overweight as sex-specific BMI for age of 85th -95th, and obesity as sex-specific BMI for >95th [20]. Abdominal obesity was defined as waist-to-height ratio (WHtR) equal to or more than 0.5 [21]. High fasting blood sugar (FBG) ≥ 100 mg/dl, high triglyceride (TG) ≥ 100 mg/dl, high total cholesterol (TC): > 200 mg/dL, high LDL ≥ 110 mg/dl and low HDL < 40 mg/dl (except than15–19-year- old boys< 45 mg/dl) were considered as abnormal [22]. Elevated BP was defined as either high systolic or diastolic BP (SBP/ DBP ≥ 90th percentile for age, sex and height). MetS was defined according to ATP-III criteria modified for children and adolescents [22].
Physical activity (PA) assessed through a validated questionnaire, through which the information of past week frequency of leisure time physical activity outside the school was collected. Enough physical activity was considered as at least 30 min duration of exercises per day that led to sweating and large increases in breathing or heart rate [23].
The Screen time (ST) evaluation of the children was assessed through the questionnaire that contains the average number of hours/day spent on watching TV/VCDs, personal computer [24], or electronic games (EG) in time of week days and weekends. The total cumulative spent time categorized into two groups; less than 2 h per day (Low), and 2 h per day or more (High) ( [24]).
Aim to assess the socioeconomic status [25] of students, benefiting from principle component analysis (PCA) method related questions including parental education, parents’ job, possessing private car, school type (public/private), and having personal computer were combined as a unique index values were analyzed as tertiles of low; intermediate and high SES [25].
Underweight, Overweight and obesity in parents were defined according to BMI ≤ 18.5 kg/m2, BMI ≥25 kg/m2 and BMI ≥30 kg/m2, respectively. Abdominal obesity in parents was defined as WC ≥95 cm [26].
Statistical analysis
Using Stata package ver. 11.0 (Stata Statistical Software: Release 11. College Station, TX: Stata Corp LP. Package), all statistical measures were estimated by survey data analysis methods. Results provide as mean and standard deviation (SD) for continuous variables, and number (percentage) for categorical variables.
Comparing the mean differences between quantitative variables assessed by Student t-test and association between qualitative variables evaluated through the Pearson Chi-square test. Logistic regression analysis considered for evaluation of the association between single-child family and cardio- metabolic risk factors in Iranian children and their families.
For each association three models were run; the first one representing the crude association and in second model additionally association was adjusted for age, living area, sex, physical activity and screen time, SES, family history of obesity. The third model additionally adjusted for BMI in all abnormality except weight disorders. Results of logistic regression revealed as odd ratio (OR) and 95% confidence interval (CI).For all measurements p-value of < 0.05 was considered statistically significant.
Results
Overall, 14,274 students and one of their parents completed the survey (participation rate: 99%). From them 14,151 individuals had complete data for analysis in this study (50.7% boys and 71.4% from urban areas); for blood sampling from students, the participation rate was 91.5% (3843 students out of 4200 students selected for blood sampling). The mean (SD) age of participants was 12.3 (3.2) years with no significant difference between girls and boys. Regarding the distribution of sex and resident area, there was no significant difference between two comparing groups. The mean of height of students in single child families significantly was shorter than the other group [(144.07 ± 18.35) vs. (146.75 ± 17.40), p < 0.001] yet the prevalence of abdominal obesity was significantly higher in single child students (26.3% vs. 20.3%, p < 0.001). Given the number of children there was no any detected association between type of families and cardio-metabolic risk factors. Demographic and biochemical characteristics of the participants compared between single/several child families in Table 1. The frequency of MetS components in single child and multiple children families was not statistically different (P-value: 0.16) (Fig. 1).
Comparing the characteristics of the two groups of study, no significant difference was found between age and anthropometric indices of mothers and fathers of single/several child families (Table 2).
Although in univariate logistic regression model (Model I), single child students had an increased risk of abdominal obesity [OR: 1.37; 95% CI: 1.19–1.58)], high SBP [OR: 1.58; 95% CI:1.17–2.14)], high BP [OR: 1.21; 95% CI:1.01–1.45)] and generalized obesity [OR: 1.27; 95% CI:1.06–1.52)], in multiple logistic regression model, only association of single child family with abdominal obesity remained statistically significant [OR: 1.28; 95% CI:1.1–1.50)].
In multivariate logistic regression model, for every increase of a child in the family the risk of abdominal obesity [OR: 0.95; 95% CI: 0.91–0.97), high SBP [OR: 0.88; 95% CI: 0.81–0.95)] and generalized obesity [OR: 0.95; 95% CI: 0.91–0.99)], decreased significantly (Table 3).
Discussion
Based on our knowledge this is the first investigation on the association between the single-child and cardio-metabolic risk factors in national representative data. The results of study have shown that there is a significant statistical association between the single-child family and the obesity among children and adolescents. It is considerable that, there was not significant association between the single-child and other cardio-metabolic risk factors.
There is some evidence on the family structure and its association with the NCDs or their cores pound risk factors. The association of single child dimension of family with increased risk of obesity have been confirmed in previous investigations [27]. In another study, it has been shown that, compared to the single children, the students who have a sister or a brother are less likely to be obese [12]. Another research shown the association between more siblings and less risk for obesity [28].
In the logistic model, there is no significant association between the dimension of family and the risks of high SBP, high DBP, high BP, high TG, low HDL-c, high FBS, MetS, high LDL-c and high TC. When we run the linear model, we investigate the significant association between the numbers of children the decreased risk of high SBP (OR: 0.88, CI: 0.81, 0.95).
Based on the evidence; boys in single-child families, compare with their counterpart in numerous child families; significantly spent more time for watching TV [29] and less time for physical activities. The physical activities shown the inverse association with the levels of LDL and TC [30]. Increasing screen time during a week with, discussed as a predisposing factor of obesity, overweight, diabetes, CVD and MetS [31,32,33].
There is some discussion that shown single children because their sense of loneliness, mostly spend more time for watching TV. This face them with increased risk of cardiometabolic risk factors. Consumption junk food is one of the probable related factors for insulin resistance and high risks of SBP [34]. On the other hand, junk food intake is positively associated with levels of BMI, WC, and TG level [35].
Studies shown that, smaller size families mostly demand for processed outdoors foods. Such nutritional habits could increase the levels of TG and the risk of cardio- metabolic diseases [36]. Some studies also emphasized on the link of fast food consumption with increased levels of serum fat and calorie intake in children obesity [37].
However, we could not found any significant association between single child situation and the majority of metabolic cardiovascular risk factors, but the role of a healthy lifestyle including physical activity and nutrition in cardio- metabolic risk factors emphasized.
One of the strengths of the present study was its national representative large sample of children and adolescents. Considering the nature of study design, the cross-sectional study limit us in causality inference of variables. On the other hand recalling bias should be mentioned as another limitation.
Conclusion
The findings of present study provide the confirmatory evidence on the association of cardio-metabolic risk factors with single-child family in national sample of children and adolescents. As a considerable point the mean of height of students in single child families significantly was shorter than the other group. The findings of study could be used for better health planning and more evidence-based policy making. The achievements also highlighted the path of complementary research.
Abbreviations
- BMI:
-
Body Mass Index
- BP:
-
blood pressure
- CI:
-
Confidence Interval
- CVD:
-
Cardio Vascular Disease
- DBP:
-
diastolic blood pressure
- EG:
-
Electronic Games
- FBG:
-
fasting blood glucose
- HDL:
-
high density lipoprotein
- LDL:
-
low density lipoprotein
- MetS:
-
metabolic syndrome
- NCDs:
-
Non-Communicable Diseases
- OR:
-
Odd Ratio
- PA:
-
Physical Activity
- PCA:
-
Principle Component Analysis
- SBP:
-
systolic blood pressure
- SD:
-
Standard Deviation
- SES:
-
socioeconomic status
- ST:
-
Screen Time
- TC:
-
total cholesterol
- TFR:
-
Total Fertility Rate
- TG:
-
triglycerides
- WC:
-
Waist Circumference
- WHO-GSHS:
-
World Health Organization-Global School Student Health Survey
- WHtR:
-
Waist-to-Height Ratio
References
Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;15, 380(9859):2095–128.
Kavey R, Allada V, Daniels S, et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association expert panel on population and prevention science; the councils on cardiovascular disease in the young, epidemiology and prevention, nutrition, physical activity and metabolism, high blood pressure research. Cardiovascular nursing, and the kidney in Heart Dis. 2006;114(24):2710–38.
Barbero U, D'Ascenzo F, Nijhoff F, et al. Assessing risk in patients with stable coronary disease: when should we intensify care and follow-up? Results from a meta-analysis of observational studies of the COURAGE and FAME era. Scientifica (Cairo). 2016;2016:3769152.
De Onis M, Blössner M, Borghi E. Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr. 2010;92(5):1257–64.
Okosun IS, Seale JP, Boltri JM, et al. Trends and clustering of cardiometabolic risk factors in American adolescents from 1999 to 2008. J Adolesc Health. 2012;50(2):132–9.
Pérez CM, Ortiz AP, Fuentes-Mattei E, et al. High prevalence of cardiometabolic risk factors in Hispanic adolescents: correlations with adipocytokines and markers of inflammation. J Immigr Minor Health. 2014;16(5):865–73.
Kelishadi R. Childhood overweight, obesity, and the metabolic syndrome in developing countries. Epidemiol Rev. 2007;29(1):62–76.
Goli S, Arokiasamy P. Demographic transition in India: an evolutionary interpretation of population and health trends using ‘change-point analysis’. PLoS One. 2013;8(10):e76404.
Abbasi-Shavazi MJ. Fertility revolution in Iran. Population and For Soc. 2001;373:1–4.
Bagley S, Salmon J, Crawford D. Family structure and children's television viewing and physical activity. Med Sci Sports Exerc. 2006;38(5):910. 8
Davison KK. Activity-related support from parents, peers, and siblings and adolescents’ physical activity: are there gender differences? J Phys Act Health. 2004;1(4):363–76.
Chen AY, Escarce JJ. Family structure and childhood obesity, early childhood longitudinal study—kindergarten cohort. Prev Chronic Dis. 2010;7:3.
Pingali P. Westernization of Asian diets and the transformation of food systems: implications for research and policy. Food Policy. 2007;32(3):281–98.
Kelishadi R, Heshmat R, Shahsanai A, et al. Determinants of tobacco and hookah smoking in a nationally representative sample of Iranian children and adolescents: the Caspian-IV study. Iran Red Crescent Med J. 2016;18(8)
Hajian-Tilaki K, Heidari B. Childhood obesity, overweight, socio-demographic and life style determinants among preschool children in Babol, northern Iran. Iranian J Pub Health. 2013;42:1283–91.
Motlagh ME, Ziaodini H, Qorbani M, et al. Methodology and early findings of the fifth survey of childhood and adolescence surveillance and prevention of adult noncommunicable disease: the Caspian-v study. Int J Prev Med. 2017;8
Kelishadi R, Majdzadeh R, Motlagh M-E, et al. Development and evaluation of a questionnaire for assessment of determinants of weight disorders among children and adolescents: the Caspian-IV study. Int J Prev Med. 2012;3(10):699.
Group WMGRS. WHO child growth standards based on length/height, weight and age, vol. 450. Oslo, Norway: Acta Paediatrica; 1992Supplement 2006. p. 76.
Knowles K, Paiva L, Sanchez S, et al. Waist circumference, body mass index, and other measures of adiposity in predicting cardiovascular disease risk factors among Peruvian adults. Int J Hypertens. 2011;2011
Pediatrics AAo. National High Blood Pressure Education Program Working Group on high blood pressure in children and adolescents. Pediatrics. 2004;114(Supplement 2):iv-iv.
Choi DH, Hur YI, Kang JH, et al. Usefulness of the waist circumference-to-height ratio in screening for obesity and metabolic syndrome among Korean children and adolescents: Korea National Health and nutrition examination survey, 2010–2014. Nutrients. 2017;10:256.
Zimmet P, Alberti G, Kaufman F, et al. The metabolic syndrome in children and adolescents. Lancet (London, England) 2007;369(9579):2059.
Kelishadi R, Qorbani M, Djalalinia S, et al. Physical inactivity and associated factors in Iranian children and adolescents: the weight disorders survey of the CASPIAN-IV study. J Cardiovasc Thorac Res. 2017;9(1):41.
Salmon J, Campbell KJ, Crawford DA. Television viewing habits associated with obesity risk factors: a survey of Melbourne schoolchildren. Med J Aust. 2006;184(2):64.
Caro DH, Cortés D. Measuring family socioeconomic status: an illustration using data from PIRLS 2006. IERI Monograph Series Issues and Methodologies in Large-Scale Assessments. 2012;5:9–33.
Azizi F, Hadaegh F, Khalili D, et al. Appropriate definition of metabolic syndrome among Iranian adults: report of the Iranian National Committee of obesity. Arch Iran Med. 2010;13:426–8.
Chen AY, Escarce JJ. Family structure and childhood obesity: an analysis through 8th grade. Matern Child Health J. 2014;18(7):1772–7.
Ochiai H, Shirasawa T, Ohtsu T, et al. Number of siblings, birth order, and childhood overweight: a population-based cross-sectional study in Japan. BMC Public Health. 2012;12(1):766.
Salmon J, Timperio A, Telford A, et al. Association of family environment with children's television viewing and with low level of physical activity. Obesity. 2005;13(11):1939–51.
Mora S, Lee I-M, Buring JE, et al. Association of physical activity and body mass index with novel and traditional cardiovascular biomarkers in women. JAMA. 2006;295(12):1412–9.
Morales-Ruán MC, Hernández-Prado B, Gómez-Acosta LM, et al. Obesity, overweight, screen time and physical activity in Mexican adolescents. Salud Publica Mex. 2009;51:S613–S20.
Mark AE, Janssen I. Relationship between screen time and metabolic syndrome in adolescents. J Public Health. 2008;30(2):153–60.
Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Springer. 2012;55(11):2895–905.
Johnson-Down L, Labonte M, Martin I, Tsuji L, et al. Quality of diet is associated with insulin resistance in the Cree (Eeyouch) indigenous population of northern Quebec. Nutr Metab Cardiovasc Dis. 2015;25(1):85–92.
Bogl L, Pietiläinen K, Rissanen A, et al. Association between habitual dietary intake and lipoprotein subclass profile in healthy young adults. Nutr Metab Cardiovasc Dis. 2013;23(11):1071–8.
Ryman T, Boyer B, Hopkins S, et al. Associations between diet and cardiometabolic risk among Yup'ik Alaska native people using food frequency questionnaire dietary patterns. Nutr Metab Cardiovasc Dis. 2015;25(12):1140–5.
Fraser LK, Clarke GP, Cade JE, et al. Fast food and obesity: a spatial analysis in a large United Kingdom population of children aged 13–15. Am J Prev Med. 2012;42(5):e77–85.
Acknowledgments
The authors thank from cooperation of all of participants of the medical sciences universities who have made this experience.
Authors’ contribution
Study concept and design: SD, RH, MQ, MEM, AMG and RK; drafting of the manuscript, and critical revision of the manuscript: SD, MQ, HZ, FR, GSH, FO and RK; Statistical Analysis: TA, MQ, AMG and MT. All of the authors have given final approval of the version to be published.
Availability of data and materials
The dataset of this article is accessible on reasonable request from the corresponding author.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Study protocols and ethical consideration guide were reviewed and approved by the Research and Ethics council of Isfahan University of Medical Sciences approved the study (Project number: 194049). After complete explanation of the study objectives and protocols, written informed consent and verbal consent were obtained from the parents and students, respectively. Participation in the study was voluntarily.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kelishadi, R., Qorbani, M., Rezaei, F. et al. Is single-child family associated with cardio-metabolic risk factors: the CASPIAN-V study. BMC Cardiovasc Disord 18, 109 (2018). https://doi.org/10.1186/s12872-018-0844-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-018-0844-y