Abstract
Background
The relationship between neuroticism, depression and cardiovascular disease (CVD) is complex and has so far not been studied in depth. The aim of this study was to determine if neuroticism is an effect-modifier in the association between depression and CVD. Data derived from a longitudinal cohort study on mental health, work and relations among adults (20–64 years), including 10,443 individuals. Depression was assessed using the Major Depression Inventory (MDI) and neuroticism by the Swedish Scale of Personality (SSP). Outcomes of cardiovascular disease were register-based from the National inpatient register.
Results
Both depression (OR 1.9 (95%CI 1.4, 2.5)) and high levels of neuroticism (OR 1.2 (95%CI 1.1–1.3)) were associated with increased risk of CVD. The combined effect of depression and neuroticism on the risk of CVD revealed HRs ranging from 1.0 to 1.9 after adjusting for age and gender, socioeconomic position, prevalent hypertension and diabetes. Almost similar associations were seen after further adjustment for lifestyle factors.
Conclusion
Neuroticism increased the risk of CVD in depressed persons. We found synergistic interaction between neuroticism and depression status in predicting future risk of CVD.
Similar content being viewed by others
Background
Personality traits signify the ability of a person to respond to the environment and this distinguishes one person from another. One of the personality traits; neuroticism is operationally defined by items referring to irritability, anger, sadness, anxiety, worry, hostility, self-consciousness, and vulnerability that have been found to be substantially correlated with one another [1, 2]. Persons with higher levels of neuroticism are often self-critical, sensitive to the criticism of others, and feel personally inadequate [3]. This personality trait appears to be correlated with a wide range of mental and physical health problems [4] including depression [5], stroke and increased coronary heart disease mortality [6, 7]. On the other hand depression increases the risk of cardiovascular diseases, such as heart disease, hypertension and stroke [8,9,10,11,12]. However, it is not yet known if high or low level of neuroticism modifies the relation between depression and CVD. Although in some scales the items that define neuroticism overlaps with symptoms of depression and anxiety which complicates the interpretation of correlations between these disorders [13, 14].
Persons with a high degree of neuroticism more frequently experience higher levels of psychosocial stress which in turn can lead to elevated blood pressure, atherosclerosis, and risky health behaviors such as poor diet, physical inactivity, smoking, sleep disturbances, or lower treatment adherence [15]. Associations with even more serious outcomes have been reported: the British Health and Lifestyle Survey concluded that neuroticism was associated with a higher mortality risk in coronary heart disease but not in stroke [16]. These findings that were later confirmed in a pooled analysis from three cohort studies [6]. In several studies attention has been paid to the association between neuroticism and depression after CVD events. For example, two studies of a post-stroke cohort, have suggested that pre-morbid neuroticism predicts post-stroke depression [17, 18]. However, to our knowledge, only one previous study has addressed the question of whether the effect of neuroticism on future risk of CVD differs in the presence of depression. This study, the Longitudinal Aging Study Amsterdam (LASA), reported that depression is only predictive for future stroke in the absence of high neuroticism [19]. The proposed hypothesis in LASA was that people with lower degree of neuroticism, had more vascular disease leading to incident cardiovascular disease. This implies that people with lower levels of neuroticism might have more atherosclerosis and hence more cardiovascular events. Additionally, the results from the LASA study were limited by the non-participation rate of participants with higher degree of neuroticism at baseline and a relatively low number of incident stroke. In the present study we use data from a longitudinal population-based Swedish cohort where depression has previously been shown to be associated with an increased risk for CVD (OR 1.9 (95%CI 1.4,2.5) [20].
The aim of this study was to investigate the effect of neuroticism on the association between depression and cardiovascular disease. We hypothesize that people with high levels of neuroticism who become depressed have a higher increased risk of CVD than those with low levels of neuroticism.
Methods
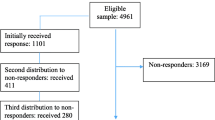
The data originates from the PART study (acronym in Swedish for: Psykisk hälsa, Arbete och RelaTioner, In English: Physical Health, Work and Relations), a longitudinal study of mental health, work and relations among adults residing in Stockholm County, Sweden [21]. The study included three data collections, wave 1 (W1) in 1998–2000, wave 2 (W2) in 2001–2003 and wave 3 (W3) in 2010. In the present study we used data from W1 and W2. Data from W3 was not used as it was collected after 10 years of initial exposure (depression) and self-reported CVD outcomes were reported only for 50.5% (n = 5228) of the participants. In each wave participants responded to a postal questionnaire including questions on risk and protective factors for mental health as well as psychiatric rating scales. In the case of missing answers in the questionnaires, the persons were contacted by telephone. In the present study, all participants from W1 were followed up between 2001 to 2014 for occurrence of cardiovascular diseases through register data from the National Patient Register (NPR) during 2008–2011 [22]. The Ethical Review Board at Karolinska Institutet, Stockholm, approved the study (2010/1185–31/596:260, 01–218, 04–528/3 and 09–880) and written informed consent was obtained from all participants.
The PART study intended to include 19,744 randomly selected Swedish citizens of which 19,457 could be reached, and 10,443 individuals responded to the questionnaire at W1 (participation rate 53%). Non-response analyses have been executed using available administrative registers, and participation was associated with female gender, higher age, higher income and education, being born in the Nordic countries and having no previous psychiatric diagnosis in inpatient registers [23]. In the following two waves the participation rates were 83% (n = 8622) and 61% (n = 5228). Attrition in W2 was associated with similar factors as in W1 [24].
Depression
Depression was evaluated using the Major Depression Inventory (MDI) based on responses given in W1 or W2. For those who were depressed in both waves, the highest score was used to assess level of severity. Severity of depression was based on the MDI score and categorized as follows: not depressed (MDI score < 20), mild depression [20,21,22,23,24], moderate [25,26,27,28,29] and severe depression (MDI >30) [25]. The Cronbach’s alpha coefficient for internal consistency for MDI in W1 was 0.91 and in W2 was 0.90. The MDI has shown high validity in both clinical and non-clinical samples, including the PART study [26,27,28] and can be used to make diagnoses according to DSM-IV.
Neuroticism
The Swedish Universities’ Scales of Personality (SSP) was used for assessment of the personality trait neuroticism (see Appendix for detailed information) [29] and has previously been widely used specially in Swedish patient populations for assessment of personality [30, 31]. The SSP consists of 91 items grouped into 13 different scales. Each scale has seven items and each item is presented as a statement with a four-point response format, ranging from 1 to 4, 1 point for “disagree” and so on to 4 points for “agree”. Scale scores were calculated by summing up the scores from individual items and then dividing by the number of input items. T-scores were then computed from normative standard scores. T-scores are standardized scores on each dimension for each type and a score of 50 represents the mean [29]. The reported Cronbach’s alpha coefficient for internal consistency of SSP ranges from 0.59 to 0.84, and the mean inter-item correlations (MIIC) ranges from 0.17 to 0.43. Previous analyses on the data showed that the scale inter correlation matrix produced a three-factor solution using Principal axis factoring; factor 1 reflecting neuroticism; factor 2 aggressiveness; and factor 3 extraversion. Neuroticism was assessed using three scales from the SSP [29]: somatic trait anxiety, stress susceptibility and embitterment. No imputation was done since no partially missing data was available for the three subscales, i.e. somatic trait anxiety, stress susceptibility and for embitterment. Scores for neuroticism was divided into tertiles at 33.3 and 66.6; lowest tertile 1 ≤ 33.4, middle tertile between 33.5 to 66.6 and highest tertile >66.6. Lowest and middle tertiles were then merged to form the lower level neuroticism and highest tertile as high-level neuroticism. This categorization was used since we were more interested in those who scored higher on the neurotic personality scale. Low-level neuroticism was used as reference group in the analysis.
Cardiovascular disease
Cardiovascular disease (CVD) was extracted from hospital discharge diagnoses in the National Patient Register (NPR) during 2001 to 2014 and data was linked to the participants through a unique Personal Identity Number (PIN). A previous validation of the NPR by the National Board of Health and Welfare showed that 85–95% of all diagnoses in the NPR are valid [32, 33]. The diagnosis which were followed were: ischemic/hypertensive heart disease; hypertensive diseases (ICD10 codes: I11–13), ischemic heart diseases (ICD10: I20–25), heart failure (ICD10: I50), other peripheral vascular diseases, embolism and thrombosis (ICD10: I73–74) and stroke (ICD10: I60–67 and I69). Participants reporting a history of ischemic/hypertensive heart disease or stroke at or before baseline n = 267 (2.6%) were excluded from further analysis.
Covariates
Age, gender, socioeconomic position [34], prevalent ischemic heart disease, hypertension, stroke and diabetes were used in the analysis as covariates [35,36,37]. Smoking, hazardous alcohol use, body mass index (BMI) and physical activity were used as mediators since they are traditional risk factors for both depression and CVD [9, 38,39,40,41,42]. Four age categories were used: 30–45; 46–60; 61–70; and >71 years. SEP in W1 was measured using occupational groups defined according to the Nordic Standard Occupational Classification (NSOC) of 1989 [43] and classified into five groups: high/intermediate level salaried employees; assistant non-manual employees; skilled workers; unskilled workers; and self-employed (including farmers). Participants were considered as physically active if they reported exercising habitually at least three times a week. Smoking habits reported in W2 were classified as regular smoker, occasional smoker, previous smoker and never smoker [44] Hazardous alcohol use in W1 and W2 was assessed by the Alcohol Use Disorders Identification Test (AUDIT) [45] and dichotomized following the Swedish cut-off points (≥8 points for men and ≥6 points for women) [46]. If data was available from both W1 and W2, a combined variable was created for both waves indicating presence in both waves or maximum value in either wave for a continuous variable like BMI.
Statistical analyses
Descriptive analyses were performed to report mean and standard deviation (SD) for continuous variables and frequency and percentage for categorical variables. Imputation of missing values for MDI was accomplished by the mean value of the questions in the answered items when there were missing answers for one or two of the ten questions. If answers were missing for three or more questions; 0.2% (n = 23) in W1 and 1.4% (n = 121) in W2, the response was left as missing. The maximum number of missing values for questions were as follows; somatic trait anxiety 0.3% (n = 29), stress susceptibility 0.3% (n = 29) and for embitterment 0.4% (n = 29). As there was no partially missing data on the SSP, no imputation was done for the three subscales i.e. somatic trait anxiety, stress susceptibility and embitterment. Multicollinearity was checked between MDI and SSP and was not significant (Variation Inflation Factor = 1).
Multiplicative and Additive interaction were estimated. Multiplicative interaction was estimated using main effect model with and without multiplicative interaction between depression and neuroticism and p-value was calculated using the Loglikelihood test [47]. Additive interaction was estimated measuring interaction on an additive scale as it is appropriate for assessing the public health importance of interactions [48] and based on dummy variables of depression and levels of neuroticism. Four dummy variables were created; low level neuroticism with no depression (reference), low level neuroticism with depression, high level neuroticism with no depression, and high level neuroticism with depression. Synergy index (S) was calculated to confirm if additive interaction was present. S = 1 means no interaction or exactly additivity; S > 1means positive interaction or more than additivity; S < 1means negative interaction or less than additivity. S can range from 0 to infinity [49]. Logistic regression was used to calculate OR where required.
Cox regression models were constructed to determine hazard ratios with 95% confidence intervals using survival analysis. Participants were followed from January 2001 to December 2014 and endpoints considered were: time of IHD, stroke or death, or end of follow up. Time to event was calculated in years = Time of event (admission date) minus start of follow-up for those who had an event, and end of follow-up minus start of follow-up for those who did not have event. SPSS versions 19.11 and SAS 9.3 were used for the statistical analyses.
Results
A description of the study population overall and stratified according to tertiles of neuroticism can be seen in Table 1. The prevalence of depression was 14.4% (n = 1488). Mean t-score for neuroticism was 145 (SD 24.0); somatic trait anxiety 47.9 (SD 9.7), stress susceptibility 51.1 (SD 8.1) and for embitterment 46.5 (SD 9.9) respectively. High level of neuroticism was present in 27.7% (n = 2866) of the participants and of these persons 65.0% (n = 1862) were not depressed and 35.0% (n = 1004) were depressed. During the follow-up period, 5.1% (n = 537) experienced CVD, 3.1% (n = 325) with ischemic/hypertensive heart disease and 2.4% (n = 248) strokes. Depression was associated with an increased risk for CVD (OR 1.9 (95%CI 1.5,2.4) (as published elsewhere) [20]. Having a high level of neuroticism was also associated with an increased risk for CVD; OR 1.2 (95%CI 1.1, 1.3).
The analyses of multiplicative interaction between depression and neuroticism for future risk of CVD, hypertensive/Ischemic heart disease and stroke resulted in p-values for the Log likelihood ratios of 0.4, 0.4 and 0.6 respectively indicating no multiplicative interaction. Additive interaction is demonstrated in Table 2 showing Hazard ratios and Synergy Index (95% CI) between Neuroticism and Depression for CVD, IHD and Stroke. For CVD, those who were depressed, the HR (95%CI) ranged from 1.0 (95%, CI 0.5, 2.0) to 2.0 (95%, CI 1.5, 2.6) for low and high level neuroticism respectively in analyses adjusted for age and gender. The corresponding synergy index is 1.7 (95% CI, 0.4, and 6.3). Similar risk estimates and synergy index for outcome of IHD and Stroke are shown.
Table 3 demonstrates Hazard ratios for CVD, according to depression status and neuroticism after excluding those who had baseline CVD. For CVD, those who were depressed, the HR (95%CI) ranged from 1.0 (95%, CI 0.4, 2.3) to 1.9 (95%, CI 1.3, 2.6) for low and high level neuroticism respectively in analyses adjusted for age and gender, socioeconomic position and history diabetes and hypertension. The association remained after additional adjustment for lifestyle risk factors. Further subgroup analysis for hypertensive/ischemic heart disease and stroke demonstrated similar increased hazard ratios.
Discussion
In this large population-based cohort of 10,341 adults, we found associations between depression and high levels of neuroticism independently for future risk of CVD. These results are in agreement with previous studies [16, 50, 51]. Further, our study found evidence of a synergistic interaction between neuroticism and depression on future risk for CVD. This implies that high level of neuroticism increases the risk of CVD in depressed patients.
Previous studies have concluded that high neuroticism is an important predictor of depression after stroke [17, 52]. Distressed personality is a predictor of adverse cardiac outcomes after acute MI, irrespective of disease severity and the presence of depression but the results have not been consistent [53,54,55]. So far there is only one study, a 9-year follow-up study of 2050 participants, Longitudinal Aging Study Amsterdam (LASA) by Marijnissen et al., which has discussed the effect of neuroticism on the relation between depression and future risk of stroke. The study concluded that older persons with depression and low level of neuroticism had a higher risk of developing stroke, thus indicating a negative interaction between depression and neuroticism in predicting future risk of CVD [19]. In contrast, our study demonstrates that there is an interaction between neuroticism and depression in predicting risk for CVD. The reasons for this could be the relatively reduced power of the former study due to selective dropout of persons with missing neuroticism scores in depressed individuals. Moreover, the cardiovascular outcomes in LASA were based on self-reports, medication or GP based diagnoses. This might have resulted in misclassification bias, as many medications that are used for stroke and myocardial infarctions are also used for hypertension. Thirdly, the number of participants with stroke within subgroups was rather low, especially in the subgroup of non-depressed, non-cardiac patients. Our findings that persons affected by depression who have high levels of neuroticism are at higher risk for CVD, emphasize the need for additional treatment besides antidepressant drugs. In persons scoring higher on neuroticism initial treatment with pharmacotherapy might be necessary since it may target neural systems involved in dysregulated emotion. This could then be followed by cognitive behavioral therapy (CBT) which is a well-documented treatment for both depression and neuroticism [31] and have a protective effect on depression recurrence [56].
The evidence for the underlying mechanism between neuroticism and depression leading to CVD has been highlighted in a few studies. Studies report that people scoring high on neuroticism and having depression might have less vascular risk factors (hypertension, diabetes mellitus, hypercholesterolemia, smoking, obesity and low physical activity) for stroke, while those scoring low on neuroticism might have more vascular risk factors as a potential explanation for the increased risk of future stroke [57, 58]. In contrast we suggest, based on the results from this study, that since both depression and neuroticism are independent risk factors for CVD, the vascular risk factors linked to these risk factors are shared and hence leads to increased CVD. These vascular risk factors include hypertension, diabetes, smoking and socioeconomic status [9, 59]. Heart rate variability is another biomarker for neuroticism, which partly accounts for its phenotypic association with CVD, and depression. It is associated with neuroticism, depression and CVD; however the path between heart rate variability and depression is not causal [60].
The strengths of this study are the longitudinal design, the use of a population-based sample and the validated instruments for assessing depression and neuroticism. We also excluded participants with CVD at baseline to prevent misclassification of outcome. Our study also has some limitations that have to be acknowledged. The low response rates in W1 (53%) and slightly low baseline prevalence of depression is a limitation [23]. Since persons severely affected by depression most likely were non responders and this might have underestimated the results. Those who had received in-patient psychiatric care were less likely to participate, which potentially limits the generalizability. However, the non-participation analysis revealed that the odds ratios for associations between depression and gender, income, country of origin and education were similar among participants and non-participants [23, 24]. There might have been some change in the degree of neuroticism over a 10-year follow-up and this might have resulted in slight changes in the risk estimates. As the follow-up period started from 2001, some participants might not have had sufficient latent time for the outcome to occur. We were not able to show multiplicative interaction in this study, however we showed additive interaction which has more public health significance and It has been argued that the assessment of interaction on the additive scale is more indicative of the underlying causal mechanism [48]. Although this study was able to adjust for common mediators and confounders, it did not offer the possibility to adjust for dyslipidemia, blood glucose, type and use of antidepressants and treatment compliance due to lack of data.
Conclusion
Higher levels of neuroticism increased the risk of CVD in depressed persons. We found a synergistic interaction between neuroticism and depression in predicting future risk of CVD. Further research is required to test early therapeutic interventions for concomitant neuroticism and depression and its effect on CVD.
Abbreviations
- CVD:
-
Cardiovascular diseases
- HTN:
-
Hypertension
- IHD:
-
Ischemic heart diseases
- MDI:
-
Major depression inventory
- SSP:
-
Swedish scale of personality
References
Costa PT, McCrae RR. The revised neo personality inventory (neo-pi-r). The SAGE handbook of personality theory and assessment. London: Sage Publications; 2008;2:179–98.
Matthews G, Deary IJ, Whiteman MC. Personality traits. Edinburgh: Cambridge University Press; 2003.
Watson D, Clark LA, Harkness AR. Structures of personality and their relevance to psychopathology. J Abnorm Psychol. 1994;103(1):18–31.
Malouff JM, Thorsteinsson EB, Schutte NS. The five-factor model of personality and smoking: a meta-analysis. J Drug Educ. 2006;36(1):47–58.
Steunenberg B, Beekman AT, Deeg DJ, Kerkhof AJ. Personality and the onset of depression in late life. J Affect Disord 2006;92(2–3):243–51.
Jokela M, Pulkki-Raback L, Elovainio M, Kivimaki M. Personality traits as risk factors for stroke and coronary heart disease mortality: pooled analysis of three cohort studies. J Behav Med. 2014;37(5):881–9.
Hagger-Johnson G, Roberts B, Boniface D, Sabia S, Batty GD, Elbaz A, et al. Neuroticism and cardiovascular disease mortality: socioeconomic status modifies the risk in women (UK health and lifestyle Survey). Psychosom Med. 2012;74(6):596–603.
Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. 2006;27(23):2763–74.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
Watkins LL, Koch GG, Sherwood A, Blumenthal JA, Davidson JR, O’Connor C, et al. Association of anxiety and depression with all-cause mortality in individuals with coronary heart disease. J Am Heart Assoc. 2013;2(2):e000068.
Frasure-Smith N, Lesperance F. Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch Gen Psychiatry. 2008;65(1):62–71.
Li CT, Bai YM, Tu PC, Lee YC, Huang YL, Chen TJ, et al. Major depressive disorder and stroke risks: a 9-year follow-up population-based, matched cohort study. Plos One. 2012;7(10):e46818.
Jylha P, Isometsa E. The relationship of neuroticism and extraversion to symptoms of anxiety and depression in the general population. Depress Anxiety. 2006;23(5):281–9.
Bouhuys AL, Flentge F, Oldehinkel AJ, van den Berg MD. Potential psychosocial mechanisms linking depression to immune function in elderly subjects. Psychiatry Res. 2004;127(3):237–45.
Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J Am Coll Cardiol. 2009;53(11):936–46.
Shipley BA, Weiss A, Der G, Taylor MD, Deary IJ. Neuroticism, extraversion, and mortality in the UK health and lifestyle Survey: a 21-year prospective cohort study. Psychosom Med. 2007 Dec;69(9):923–31.
Morris PL, Robinson RG. Personality neuroticism and depression after stroke. Int J Psychiatry Med. 1995;25(1):93–102.
Morris PL, Robinson RG, Raphael B, Samuels J, Molloy P. The relationship between risk factors for affective disorder and poststroke depression in hospitalised stroke patients. Aust N Z J Psychiatry. 1992;26(2):208–17.
Marijnissen RM, Wouts L, Schoevers RA, Bremmer MA, Beekman AT, Comijs HC, et al. Depression in context of low neuroticism is a risk factor for stroke: a 9-year cohort study. Neurology. 2014;83(19):1692–8.
Almas A, Forsell Y, Iqbal R, Janszky I, Moller J. Severity of depression, anxious distress and the risk of cardiovascular disease in a Swedish population-based cohort. Plos One. 2015;10(10):e0140742.
Hällström T, Damström Thakker K., Forsell Y, Lundberg I, Tinghög P. The PART study. A population based study of mental health in the Stockholm County: study design. Phase l (1998–2000); Stockholm: Published by the PART study group; 2003. Contract No.: Document Number|.
Forsberg LRH, Jacobsson A, Nyqvist K, Heurgren M. Kvalitet och innehåll i patientregistret. Utskrivningar från slutenvården 1964–2007 och besök i specialiserad öppenvård (exklusive primärvårdsbesök) 1997–2007. (Quality and content of the Patient Register) (2009–125-15). ed.^eds E, editor.; Stockholm: Socialstyrelsen; 2009.
Lundberg I, Damstrom Thakker K, Hallstrom T, Forsell Y. Determinants of non-participation, and the effects of non-participation on potential cause-effect relationships, in the PART study on mental disorders. Soc Psychiatry Psychiatr Epidemiol. 2005;40(6):475–83.
Bergman P, Ahlberg G, Forsell Y, Lundberg I. Non-participation in the second wave of the PART study on mental disorder and its effects on risk estimates. Int J Soc Psychiatry. 2010;56(2):119–32.
Snaith RP, Harrop FM, Newby DA, Teale C. Grade scores of the Montgomery-Asberg depression and the clinical anxiety scales. Br J Psychiatry. 1986;148:599–601.
Forsell Y. The major depression inventory versus schedules for clinical assessment in neuropsychiatry in a population sample. Soc Psychiatry Psychiatr Epidemiol. 2005;40(3):209–13.
Cuijpers P, van Straten A, Warmerdam L. Problem solving therapies for depression: a meta-analysis. Eur Psychiatry. 2007;22(1):9–15.
Olsen LR, Jensen DV, Noerholm V, Martiny K, Bech P. The internal and external validity of the major depression inventory in measuring severity of depressive states. Psychol Med. 2003;33(2):351–6.
Gustavsson JP, Bergman H, Edman G, Ekselius L, von Knorring L, Linder J. Swedish universities scales of personality (SSP): construction, internal consistency and normative data. Acta Psychiatr Scand. 2000;102(3):217–25.
Fagerberg T, Soderman E, Gustavsson JP, Agartz I, Jonsson EG. Personality traits in established schizophrenia: aspects of usability and differences between patients and controls using the Swedish universities Scales of Personality. Nord J Psychiatry. 2016;22:1–8.
Hedman E, Andersson G, Lindefors N, Gustavsson P, Lekander M, Ruck C, et al. Personality change following internet-based cognitive behavior therapy for severe health anxiety. Plos One. 2014;9(12):e113871.
Nilsson AC, Spetz CL, Carsjo K, Nightingale R, Smedby B. [Reliability of the hospital registry. The diagnostic data are better than their reputation]. Lakartidningen. 1994;91(7):598, 603–605.
Ludvigsson JF, Andersson E, Ekbom A, Feychting M, Kim JL, Reuterwall C, et al. External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450.
Seifert CL, Poppert H, Sander D, Feurer R, Etgen T, Ander KH, et al. Depressive symptoms and the risk of ischemic stroke in the elderly--influence of age and sex. Plos One. 2012;7(11):e50803.
Thurston RC, El Khoudary SR, Derby CA, Barinas-Mitchell E, Lewis TT, McClure CK, et al. Low socioeconomic status over 12 years and subclinical cardiovascular disease: the study of women’s health across the nation. Stroke. 2014;45(4):954–60.
Roest AM, Zuidersma M, de Jonge P. Myocardial infarction and generalised anxiety disorder: 10-year follow-up. Br J Psychiatry. 2012;200(4):324–9.
Eurelings LS, Ligthart SA, van Dalen JW, Moll van Charante EP, van Gool WA, Richard E. Apathy is an independent risk factor for incident cardiovascular disease in the older individual: a population-based cohort study. Int J Geriatr Psychiatry. 2014;29(5):454–63.
Covey LS, Glassman AH, Stetner F. Cigarette smoking and major depression. J Addict Dis. 1998;17(1):35–46.
Prescott E, Hippe M, Schnohr P, Hein HO, Vestbo J. Smoking and risk of myocardial infarction in women and men: longitudinal population study. BMJ. 1998;316(7137):1043–7.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–9.
Strohle A. Physical activity, exercise, depression and anxiety disorders. J Neural Transm. 2009;116(6):777–84.
Cornelius JR, Bukstein O, Salloum I, Clark D. Alcohol and psychiatric comorbidity. Recent Dev Alcohol. 2003;16:361–74.
Statistiska centralbyra°n (1989). Occupations in population and housing census 1985 (FoB 85) according to Nordic standard occupational classification (NYK) and Swedish socio-economic classification (SEI): alphabetical version. Centralbyra°n S. In: SCB, editor. Stockholm: Meddelanden i samordningsfra°gor; 1989.
Hassmiller KM, Warner KE, Mendez D, Levy DT, Romano E. Nondaily smokers: who are they? Am J Public Health. 2003;93(8):1321–7.
Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction. 1993;88(6):791–804.
Kallmen H, Wennberg P, Berman AH, Bergman H. Alcohol habits in Sweden during 1997–2005 measured with the AUDIT. Nord J Psychiatry. 2007;61(6):466–70.
Maity A. A powerful test for comparing multiple regression functions. J Nonparametr Stat. 2012;24(3):563–76.
Rothman KJ, Greenland S, Walker AM. Concepts of interaction. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.]. Am J Epidemiol. 1980;112(4):467–70.
Knol MJ, Vander Weele TJ, Groenwold RH, Klungel OH, Rovers MM, Grobbee DE. Estimating measures of interaction on an additive scale for preventive exposures. Eur J Epidemiol. 2011;26(6):433–8. [Research Support, N.I.H., Extramural].
Van der Kooy K, van Hout H, Marwijk H, Marten H, Stehouwer C, Beekman A. Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007;22(7):613–26.
Mommersteeg PM, Pouwer F. Personality as a risk factor for the metabolic syndrome: a systematic review. J Psychosom Res. 2012;73(5):326–33.
Hwang SI, Choi KI, Park OT, Park SW, Choi ES, Yi SH. Correlations between pre-morbid personality and depression scales in stroke patients. Ann Rehabil Med. 2011;35(3):328–36.
Martens EJ, Mols F, Burg MM, Denollet J. Type D personality predicts clinical events after myocardial infarction, above and beyond disease severity and depression. J Clin Psychiatry. 2010;71(6):778–83.
de Jonge P, Denollet J, van Melle JP, Kuyper A, Honig A, Schene AH, et al. Associations of type-D personality and depression with somatic health in myocardial infarction patients. J Psychosom Res. 2007;63(5):477–82.
Mols F, Martens EJ, Denollet J. Type D personality and depressive symptoms are independent predictors of impaired health status following acute myocardial infarction. Heart. 2010;96(1):30–5.
Vittengl JR, Clark LA, Dunn TW, Jarrett RB. Reducing relapse and recurrence in unipolar depression: a comparative meta-analysis of cognitive-behavioral therapy’s effects. J Consult Clin Psychol. 2007;75(3):475–88.
Marijnissen RM, Bus BA, Schoevers RA, Wouts L, Holewijn S, Franke B, et al. Atherosclerosis decreases the impact of neuroticism in late-life depression: hypothesis of vascular apathy. Am J Geriatr Psychiatry. 2014;22(8):801–10.
Wouts L, Janzing JG, Lampe IK, Franke B, de Vegt F, Tendolkar I, et al. The interaction between cerebrovascular disease and neuroticism in late-life depression: a cross-sectional study. Int J Geriatr Psychiatry. 2011;26(7):702–10.
Aben I, Denollet J, Lousberg R, Verhey F, Wojciechowski F, Honig A. Personality and vulnerability to depression in stroke patients: a 1-year prospective follow-up study. Stroke. 2002;33(10):2391–5.
Cukic I, Bates TC. The association between neuroticism and heart rate variability is not fully explained by cardiovascular disease and depression. Plos One. 2015;10(5):e0125882.
Acknowledgements
Not applicable.
Funding
Funding for the PART was provided by the Swedish Research Council (to YF, the Stockholm County Council), the Karolinska Institutet Faculty Funds (to YF). The PhD student support was provided by Faculty Development Award, Aga Khan University Karachi, Pakistan.
Availability of data and materials
Data are ethically restricted for patient privacy concerns. However, de identified, participant level data can be obtained pending ethical approval. Please send requests for a Minimal dataset to Dr. Yvonne Forsell, yvonne.forsell@aku.edu.
Author information
Authors and Affiliations
Contributions
The study idea and study design was conceived by AA, YF and JM. AA performed the statistical analyses and wrote the first draft. All authors have been involved in interpretation of the results and made important contributions to the drafting of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Authors’ information
The author AA is a PhD student at the Karolinska Institutet, Stockholm, Sweden. She works as an internist with primary affiliation with Aga Khan University, Karachi, Pakistan.
Ethics approval and consent to participate
Ethical Review Board at Karolinska Institutet, Stockholm, approved the study (2010/1185–31/596:260, 01–218, 04–528/3 and 09–880) and written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Almas, A., Moller, J., Iqbal, R. et al. Effect of neuroticism on risk of cardiovascular disease in depressed persons - a Swedish population-based cohort study. BMC Cardiovasc Disord 17, 185 (2017). https://doi.org/10.1186/s12872-017-0604-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-017-0604-4