Abstract
Background
Decisive information on the parameters involved in cognitive impairment in patients with chronic heart failure is as yet lacking. Our aim was to determine the functional and psychosocial variables related with cognitive impairment using the mini-mental-state examination (MMSE) with age-and education-corrected scores.
Methods
A cohort study of chronic heart failure patients included in an integrated multidisciplinary hospital/primary care program. The MMSE (corrected for age and education in the Spanish population) was administered at enrolment in the program. Analyses were performed in 525 patients. Demographic and clinical variables were collected. Comprehensive assessment included depression (Yesavage), family function (family APGAR), social network (Duke), dependence (Barthel Index), frailty (Barber), and comorbidities. Univariate and multivariate logistic regression were performed to determine the predictors of cognitive impairment.
Results
Cognitive impairment affected 145 patients (27.6 %). Explanatory factors were gender (OR: 2.77 (1.75–4.39) p < 0.001), ischemic etiology (OR: 1.99 (1.25–3.17) p = 0.004), frailty (OR: 1.58 (0.99 to 2.50, p =0.050), albumin > 3.5 (OR: 0.59 (0.35–0.99) p = 0.048), and beta-blocker treatment (OR: 0.36 (0.17 to 0.76, p = 0.007)). No association was found between cognitive impairment and social support or family function.
Conclusion
The observed prevalence of cognitive impairment using MMSE corrected scores was 27.6 %. A global approach in the management of these patients is needed, especially focusing on women and patients with frailty, low albumin levels, and ischemic aetiology heart failure.
Similar content being viewed by others
Background
Cognitive impairment (CI) is particularly common in patients with chronic heart failure (CHF) and has been associated with an increased mortality rate in hospital admissions and worse clinical outcomes [1]. Nevertheless, it is still uncertain when CI should be assessed in common clinical practice, the instruments that should be employed for primary evaluation, and which patients should be included in a more extensive neuropsychological diagnostic battery. Despite interest in the global assessment of CHF there is as yet no decisive information on which factors play a role when deciding whether routine cognition screening in clinical practice would be helpful for an individual patient.
The prevalence of CI depends on the test used and varies widely among studies, ranging from less than 30 % to more than 80 % [2–7]. As cognitive tests are age-and education sensitive [8] the use of a validated screening test in our population would provide valuable information on CI prevalence. The Mini Mental State Examination (MMSE) is a widely used instrument to evaluate cognitive function in CHF patients [9, 10]. It determines global cognitive impairment and is more commonly employed in clinical practice than complex neuropsychological batteries [4, 11].
The present study aims to assess CI prevalence with the MMSE, and identify clinical, psychological, social, family, and frailty-related factors, in a large sample of CHF patients.
Methods
From 2005 to 2010, 805 consecutive patients were enrolled as a cohort of non-institutionalized patients referred to hospital-primary care integrated multidisciplinary nurse led heart failure program [12]. We present here the baseline assessment. Assessment was conducted at the time of patient inclusion in the heart failure program. Once diagnosis was confirmed on an ambulatory basis, the patient was invited to be included in the heart failure registry. Then, clinical and analytical data were collected, and psychosocial evaluations were performed by hospital nurses specifically trained in heart failure. The evaluation was carried out in a single session, with the cognitive test administered first. The study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the local committee of ethics for clinical research and all patients gave written informed consent after recruitment. For inclusion in the study, patients had to be in a stable condition and with a CHF diagnosis of either reduced or preserved ejection fraction, according to the European Society of Cardiology diagnostic criteria [13]. Additionally, inclusion in the study required that patients were able to undergo neuropsychological testing and could communicate adequately in order to follow the tests instructions by themselves. Exclusion criteria for the study were: significant primary valvular disease, hemoglobin levels < 8.5 g/dL, clinical signs of fluid overload, pericardial disease, restrictive cardiomyopathy, hypertrophic cardiomyopathy, active malignancy and chronic liver disease. Patients with serious psychiatric illness, unstable CHF, overt cognitive impairment which impeded psychosocial assessment; and those suffering from extra-cardiac disease with a life expectancy of less than 1 year were also excluded. No experimental intervention was performed.
Clinical variables
At recruitment, peripheral blood samples were taken to measure the usual biological variables needed to perform initial evaluation in heart failure patients. Clinical and demographic information assessed included CHF etiology; New York Heart Association (NYHA) functional class, heart rate, pro-brain natriuretic peptide (Nt proBNP), blood pressure, current medical therapy and the most recent left ventricular ejection fraction (LVEF) evaluation. Recorded comorbidities were current diabetes mellitus, history of stroke or cerebrovascular disease, peripheral arterial disease, chronic kidney disease, anemia, and chronic obstructive pulmonary disease. Once CHF diagnosis had been confirmed on an outpatient basis the patient was invited to be included in the heart failure registry. Clinical and analytical data were then collected, and evaluations were performed by cardiology nurses trained in heart failure management.
Cognitive functions
All the patients who agreed to participate underwent a comprehensive psycho-social assessment. From those invited 122 had an incomplete evaluation and were excluded. The MMSEwas completed at baseline in all the 683 remaining patients, either by a neuropsychologist or a specialized nurse who had received specific training. Of those tested, 158 had not education recorded and were excluded. MMSE [14] Spanish validated version (30 items, cognitive impairment scores ≤ 24) [15]) with scores adjusted by age and education was finally calculated in 525 patients (Fig. 1). The MMSE measures overall cognitive impairment, it includes brief assessments of memory, language, praxis, and orientation and it is regarded as the gold standard in cognitive impairment detection [16]. It has been used in heart failure patients [5], it takes approximately 10 min to administer, and It has been found predictor of hospital readmission [3, 15, 17].
Age and education corrected scores were calculated following Blesa MMSE validation in Spanish population. These corrections add or subtract up to 2 points depending on age bands and education level (Table 1). Other corrections have been proposed but external validity of Blesa correction is particularly appropriate as it was carried out in our area. No experimental intervention was performed.
Psycho-social evaluation
Education was assessed as categorical variable: illiterates, elementary education (4 years of education), high school (up to 9 years), and college (more than 10 years). We recorded marital status, living with a partner, self-administration of medication, and the need for a caregiver.
Dependency was measured by the validated Spanish version of the Barthel test [18] for basic daily activities, in its Spanish validation version; with scores ranging from 0 to 100, those <90indicate dependency. Family function was recorded following The Family APGAR questionnaire in its Spanish form [19], the scale can range from 0 to 10, < 7 represents family dysfunction.
Depression was screened with the short form of the Spanish validated version [20] of the Yesavage Geriatric Depression Scale [21]. Scores > 4 indicate depression.
Social support is positively associated with medication compliance [22–25]. We used The Duke-UNC Functional Social Support Questionnaire [26], an eight-item 3Likert scale in which the higher the average score, the greater the perceived social support. A cut-off of 32 has been proposed in its Spanish version.
Frailty was screened with the self-reported Barber questionnaire [27] in its Spanish validated version [28]. This questionnaire assesses functional status, psychosocial functioning, neurosensory deficits, self-reported health, social support, and previous year hospital admissions. The three major domains in frailty [29]-physical, psychological and social-are represented. It is a 9-item screening tool, easy to understand and self-administer, which identifies individuals who may be at risk of dependency. Any positive item indicates frailty. A cutoff of 2 was applied to increase the positive predictive value of the test since most patients had a recent admission in the previous year.
Statistical methods
Demographic and clinical data were summarized with basic descriptive statistics in the total cohort. For quantitative variables arithmetic mean (± standard deviation) or median (interquartile range) were calculated as appropriate, and P values derived from a two-sample t-test (U-Mann–Whitney tests were used for skewed data). For qualitative variables, percentages within specified groups were calculated and P values were derived using Chi [2] tests. All the tests were two-sided; differences were considered significant at the p < 0.05 level.
The following clinical variables were dichotomized before entering the linear regression model: age over 65/ below 65, higher education meaning more than 10 years versus less than 10 years of formal education, mild NYHA class I, II versus advanced NYHA III, IV, preserved left ventricle ejection fraction vs. impaired, heart rate over 70 versus HR below 70 as heart rate over 70 is a marker of disease severity and mortality predictor [30]. albumin <3,5 yes/no. NtproBNP was dichotomized over the median as multiple factors influence its values beyond the predictive cut off 1000. Logistic regression models (enter) were generated to explore the relationships between dichotomous and clinical variables. Clinical, functional and biochemical values, echocardiography and co-existing diseases were used as explanatory variables. Univariate analysis was composed of the comparison of cognitive impairment/cognitive normal according to MMSE age-education cut-off scores. Differences between the cognitively normal/impaired groups were calculated using logistic regression model one-to one analyses.
Variables that showed statistical significance (p <0.10) in the univariate analysis were included in the multivariable logistic regression (enter method) using MMSE age-and education-corrected scores as the main variable. Three logistic regression models (enter) were completed. Model one included only the clinical factors, model two included psychosocial factors and model three both clinical and psychosocial factors. Results were presented as odds ratios (OR) with 95 % confidence intervals (CI). The Hosmer-Lemeshow chi-square test was used to assess the models’ goodness-of-fit. Various models were developed, including several combinations of adjustment variables. Co-linearity problems were not observed as the change of the standard coefficient errors was not relevant in terms of loss of statistical significance.
All models were carried out in the final patient sample (n = 525). SPSS® version 13.0 (IBM, Armonk, NY, USA) was employed for statistical analyses.
Results
Cognitive impairment and clinical markers
Of the total sample size (n = 525), 145 participants (27.6 %) were affected by CI as determined by MMSE age-and education-corrected scores. There were no differences between participants and non-participants with respect to gender, education level, marital status, CHF etiology, natriuretic peptide levels, ventricular function, cardiovascular risk factors, reactive depression, comorbidity, or need of a caregiver. The former had hypercholesterolemia less frequently (45, 38.5 % vs. 360, 54.1 %, p = 0.001) and were more often included in the advanced NYHA functional class (59, 58.4 % vs. 295, 44.3 % p = 0.005).
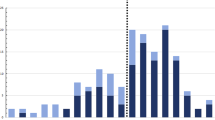
The clinically relevant affected MMSE areas in CHF patients with CI were orientation, attention, recall, language, and copying. The worst scores were found in NHYA advanced stages, and only registration was stable in the functional class (Fig. 2). Markers of disease severity such as higher levels of Nt pro-BNP, heart rate > 70, and advanced NHYA functional class were related to CI (Table 2). Mean albumin levels were lower in patients with CI, with a 3.5 cutoff being the most significant; albumin levels > 3.5 were protective, in contrast, albumin levels < 3.5 were related to CI (Fig. 3). Ischemic and hypertensive patients were more impaired than those with heart failure from other causes. Beta-blocker prescription provided a significant reduction in CI (RR: 0.35 (IC95%, 0.18–0.66)) whilst non-use showed an inverse relationship (RR 1.94 (IC 95 %, 1.37–2.74)). No association was found between CI and other drugs commonly used such as angiotensin-converting-enzyme inhibitor and angiotensin receptor blockers
Cognitive impairment in heart failure patients according to Mini-Mental-State Examination sub-items median scores in initial and advanced NHYA functional class. Statistical significance: (Mann-Whinney U): Orientation: p <0.001, registration: p =0.126, Attention: p =0.004, Recall: p =0.168, Language and copying: p = 0.001. NHYA: New York Heart Association
Parameters associated with overt cognitive impairment defined by age and education corrected MMSE scores in univariate analysis with a P value < .10. n = 525. Risk estimate and confidence limits (CL). Higher education meaning more than 10 years versus less than 10 years of formal education. NYHA: New York Heart Association functional Class. LVEF: left ventricle ejection fraction. DM: diabetes mellitus. CKD: Chronic kidney Disease: eGFR < 60 mL/min/1.73 m2. Anemia defined by hemoglobin < 12. COPD: chronic obstructive pulmonary disease. Nt-proBNP: N-terminal pro Brain Natriuretic Peptide hormone. Albumin levels >3.5. Depressive symptoms: measured by Yesavage scores above 5. Family dysfunction: Family Apgar below 7. Social support meaning lack of social support by DUKE-UNC questionnaire < 32. Frailty when Barber questionnaire above 2. Dependency defined by Barthel test <90
Gender and education
Patients with CHF and CI impairment were older, had less than 9 years of formal education, and were predominantly female. CI was less common in patients with higher education (defined as more than 9 years of formal education) (Table 2). More men had completed higher education than women [153 (47.8 %) vs. 46 (22.4 %) p < 0.001]. CI was more common in women after adjusting by education and NHYA class although the relationship could be moderated by ischemic etiology: CI was more likely in women with ischemic etiology heart failure [OR: 2.303, (95 % IC 1.204–4.405, p < 0.001)].
Co-morbidities
We observed a relationship between CI and mean glomerular flow. CI was also more frequent in patients with chronic kidney disease, diabetes, and peripheral vascular disease. Cerebrovascular disease almost reached significance (Table 2) and was included in the final model. Anemia was more common in the CI group but not significant (p = 0 .078). Pulmonary obstructive disease was not related with CI in our sample.
Psychosocial factors
Cognitively impaired patients were more likely in need of a caregiver, and not able to administer treatment by themselves. Decreased CI was related to greater patient autonomy for the management of treatment (Table 3).
Depressive symptoms were more frequent in cognitively impaired patients, almost reaching significance (p = 0.064). Lack of social support measured by Duke’s questionnaire was minimal in our sample and non-significant. Less than 15 % of the patients lived in a dysfunctional family, and this factor was un-related to CI.
Multivariate analyses
Adjusting for the significant factors identified in the unvaried analyses, we performed three different multivariate binary logistic regression models to evaluate (i) clinical factors, (ii) functional ones, and (iii) both. Age-and education-corrected MMSE scores were employed as the main variable in all 525 patients (Table 4). In a clinical model (model 1), patients with overt CI were significantly more likely to be women, and have ischemic etiology and low albumin levels. They were less probably receiving beta-blocker treatment. Dependency and frailty presented a significant association with CI in the functional model (model 2). The presumed association between CI and self-reported frailty almost reached statistical significance after clinical variables were included (p = 0.050) (model 3). Gender and ischemic etiology prevailed in the explanatory model when all variables were added. In addition, albumin levels > 3.5 and beta-blocker treatment emerged as potentially protective CI factors.
Discussion
Cognitive impairment
In this single center study we have found that cognitive impairment determined by age-and education-corrected MMSE scores affected 145 of 525 patients (27.6 %), which is consistent with other studies that used this test in patients with heart failure [31]. Nevertheless, other screening methods employed in this type of patients have obtained different figures, as CI prevalence varies according to the test used. Lately, MOCA has emerged as a possible screening tool although it does not take into account the potential false positives that can provide prevalence figures up to 80 % [1]. In a comparative study of the MOCA and MMSE in a small sample of patients, Athilingam et al. (Heart & Lung 2011) found no relationship between clinical parameters of cardiac function and the high rate of CI detected by the MOCA (54 %).
Howkins et al [4] compared the MOCA and MMSE against a neuropsychological battery in 106 patients. They reported adequate sensitivity for both tests (64–70 %) although in terms of specificity, the MMSE was slightly better than the MOCA (70 % vs. 64 %, respectively). This difference in specificity had already been highlighted by Lees et al. [32] in patients with vascular CI.
Both the MOCA and MMSE are clearly influenced by age and education, the former is considered more appropriate in populations with more than 12 years of schooling. The characteristics of the MoCA subtests, which include several complex executive demanding tasks, make it more prone to false positives when it comes to detect cognitive impairment in low educated subjects, making necessary extreme adjustments (up to 4 points in Spanish-speaking individuals; Zhou 2015) [33]. In this regard, we think that MMSE is still useful for its use in low-educated subjects. As a consequence, we employed a validated Spanish MMSE adjusted for age and education which had not only good internal validity but also excellent external validity as it was validated in our area.
Other methods use brief screening tools evaluating only memory, such as the Memory Impairment Screening test (MIS) which in the EFICARE study resulted in 46 % prevalence [34], whilst the MMSE implements more varied subdomains [5–7, 35, 36]. The fact that the prevalence found depends on the test used [5, 37, 38] underlines the importance of using tests validated for the population in focus, with appropriately age-and-education corrected versions. Although there are various tests for mild CI, only MMSE and neuropsychological batteries are recommended for its early detection in Neurology Practice Parameters [39].
The MMSE measures general cognitive functioning, in our study all the sub-items were lower in patients in the advanced functional class, with the exception of registration, which is the ability to acquire the information in the first place, and refers to short-term memory, more influenced by unstable organic conditions [40], and are preserved in many cognitively impaired subjects.
Clinical markers
We observed that in heart failure patients, ischemic aetiology was linked to CI. In a recent study, lower recall scores in cognitive tests, and cerebral grey matter loss in magnetic resonance images, were reported in patients with ischemic heart disease compared to non-ischemic ones [41]. Mild cerebral ischemia/hypoxia resulting from chronic heart failure could augment the ischemic effect and cause synaptic dysfunction, as recently reported [42]. Hypoperfusion could be an explanation although further research is needed to confirm this possibility.
In concurrence with previous research we found other factors directly linked to heart failure, as such as NHYA advanced class, and Nt proBNP [43]. The relationships were not, however, sustained in a multivariate model. LVEF was not related to CI.
Hypoalbuminemia, previously considered a mortality predictor following myocardial infarction [44], has also been reported to be predictive of 1 year mortality among heart failure patients [45]. Classically linked to frailty, in our sample, albumin levels appeared to be related to CI. We found a cutoff of 3.5 meaningful, as levels < 3.5 were more likely associated to CI. This effect persisted after controlling for renal function and was sustained in a regression model.
In our sample, patients under beta blocker treatment showed less CI after adjusting for functional class, and the effect was maintained after adjusting for multiple factors in a regression model. In the 1990s beta-blocker treatment was associated to cognitive impairment [46, 47]. Nevertheless, recent experimental studies have suggested a protective effect [48]. Such an effect was also observed in a retrospective study of hypertensive patients treated with beta blockers [49] versus other drugs.
Gender and education
We observed that CI was more frequent in women, who also were less educated. In the Women’s Health Initiative Study [50], self-reported cardiovascular disease was well documented as a factor that incremented the risk of cognitive decline in postmenopausal women, particularly in those with myocardial infarction and vascular disease (HR 2.10; 95 % CI:1.40–3.15), whereas no association was found with self-reported heart failure. Heart failure of ischemic origin was associated to cognitive impairment in women in our study. Further research in women is needed to explore this relationship.
Co-morbidities
Co-morbidities, including cerebrovascular and peripheral arterial disease [51], must be taken in account in CHF as they have been associated with CI and influence avoidable hospitalization and mortality [52]. A global assessment in CHF patients with co-morbidities illness has been suggested [12]. We found diabetes and peripheral vascular disease to be associated with CI, as previously described [53, 54].
Psychosocial factors
Our study is aimed at both clinical and psychosocial factors and we identified some that require a global evaluation focused on practice. The identified psychosocial factors included increased patient autonomy (dependency level, self-reported frailty, and need of a caregiver) which was associated with less CI. In addition, social support is positively related to medication compliance [22–24]. In our sample, as previously described in Mediterranean countries [55], almost all the patients had a self-perception of having a healthy social network and satisfactory family function.
Depressive symptoms almost reached signification. Depression was associated with poorer performance on multiple cognitive domains in heart failure in a recent study [53].
Functional limitation has emerged as a predictive value in patients with mild CHF. [56] An elevated relationship between frailty and mortality at 12 months follow-up has been found using the Barthel test, the Yesavage depressive symptoms tests and a geriatric exam [56]. We found a link between self-reported frailty and cognitive function. Frailty and heart failure would share a consistent correlation with some inflammatory biomarkers such as interleukin-6 and C-reactive protein [57]. While there is a lack of consensus on the definition of frailty, assessing it could help tailoring treatment in selected patients. Short screening instruments such as Barber tests could be easy to use in clinical practice. We observed that self-reported frailty remained a stable predictor of cognitive impairment in CHF patients after adjusting for clinical variables.
Strengths and limitations
The strengths of this study include the wide sample used, the detailed characterization of the profiled patients, and the multi-dimensional assessment including both clinical and psychosocial factors. Our study has some limitations. Its cross-sectional design implies that conclusions should be confirmed through relevant prospective cohort studies. In addition, from those invited to participate, 122 patients had an incomplete evaluation and were excluded. The excluded participants may well have had worse outcomes or have been more impaired as they were in more advanced functional class, resulting in higher figures in our population than reported. Moreover, education was only recorded in 525 patients in a way that could be later analyzed. The unregistered patients lacking education could be also have been more impaired or have had worse CHF markers. It might not be possible, therefore, to extrapolate our results to patients with other education levels. Furthermore, our sample only included Spanish patients so the results may not be applicable to populations from other regions and ethnic groups.
Conclusions
The observed prevalence of cognitive impairment using MMSE corrected scores was 27.6 %. Screening should focus specially on patients with low albumin levels, frailty, or heart failure of ischemic aetiology, and women in particular. We believe that integrated care improves results in heart failure management and facilitates patient monitoring focused on enhancing quality of life. Almost one in three patients resulted impaired, that justifies the screening in CHF patients as MMSE is a feasible screening instrument, easy to administer on routine settings. Identifying related factors facilitates the selection of patients in which screening would be especially helpful.
Abbreviations
- CHF:
-
Chronic heart failure
- CI:
-
Cognitive impairment
- LVEF:
-
Left ventricular ejection fraction
- MMSE:
-
Mini-mental state examination
- NHYA:
-
New York heart association
- Nt proBNP:
-
pro-brain natriuretic peptide
References
Cameron J, Ski CF, Thompson DR. Cognitive impairment in chronic heart failure and the need for screening. Am J Cardiol. 2011;107:1547–8.
Athilingam P, D’Aoust RF, Miller L, Chen L. Cognitive profile in persons with systolic and diastolic heart failure. Congest Heart Fail. 2013;19:44–50.
Dodson JA, Truong TT, Towle VR, Kerins G, Chaudhry SI. Cognitive impairment in older adults with heart failure: prevalence, documentation, and impact on outcomes. Am J Med. 2013;126:120.
Hawkins MA, Gathright EC, Gunstad J, et al. The MoCA and MMSE as screeners for cognitive impairment in a heart failure population: a study with comprehensive neuropsychological testing. Heart Lung. 2014;43:462–8.
Jurgens CY, Faulkner KM, Lee CS. Phenotypic profiling of cognitive impairment risk among patients with heart failure: a literature review of the usefulness of cardiac-related variables. Eur J Cardiovasc Nurs. 2013;12:109–31.
Triposkiadis FK, Skoularigis J. Prevalence and importance of comorbidities in patients with heart failure. Curr Heart Fail Rep. 2012;9:354–62.
van den Hurk K, Reijmer YD, van den Berg E, et al. Heart failure and cognitive function in the general population: the Hoorn Study. Eur J Heart Fail. 2011;13:1362–9.
Gonzalez Moneo MJ, Escriva FR, Vinyoles BE, Espel MC, Davins MJ, Borrell MM. Estimation of the prevalence of cognitive impairment according to the test used. Aten Primaria. 1997;20:173–9.
Bauer L, Pozehl B, Hertzog M, Johnson J, Zimmerman L, Filipi M. A brief neuropsychological battery for use in the chronic heart failure population. Eur J Cardiovasc Nurs. 2012;11:223–30.
Vogels RL, Oosterman JM, Van HB, et al. Profile of cognitive impairment in chronic heart failure. J Am Geriatr Soc. 2007;55:1764–70.
Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–35.
Comin-Colet J, Verdu-Rotellar JM, Vela E, et al. Efficacy of an integrated hospital-primary care program for heart failure: a population-based analysis of 56,742 patients. Rev Esp Cardiol. 2014;67:283–93.
McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2012;14:803–69.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Blesa R, Pujol M, Aguilar M, et al. Clinical validity of the ‘mini-mental state’ for Spanish speaking communities. Neuropsychologia. 2001;39:1150–7.
Cameron J, Worrall-Carter L, Page K, Stewart S, Ski CF. Screening for mild cognitive impairment in patients with heart failure: Montreal cognitive assessment versus mini mental state exam. Eur J Cardiovasc Nurs. 2013;12:252–60.
National Collaborating Centre for Mental Health (UK). Dementia: a NICE-SCIE Guideline on Supporting People With Dementia and Their Carers in Health and Social Care. Leicester: NICE Guidelines; 2011.
Cabanero-Martinez MJ, Cabrero-Garcia J, Richart-Martinez M, Munoz-Mendoza CL. The Spanish versions of the Barthel index (BI) and the Katz index (KI) of activities of daily living (ADL): a structured review. Arch Gerontol Geriatr. 2009;49:e77–84.
Delgado ALJ. Validez y fiabilidad del cuestionario de función familiar Apgar-familiar. Aten Primaria. 1996;18:289–95.
Ramos Brieva JA, Montejo Iglesias ML, Lafuente LR, Ponce De Leon HC, Moreno SA. Validation of the Geriatric Depression Screening Scale. Actas Luso Esp Neurol Psiquiatr Cienc Afines. 1991;19:174–7.
Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37–49.
Graven LJ, Grant JS. Social support and self-care behaviors in individuals with heart failure: an integrative review. Int J Nurs Stud. 2014;51:320–33.
Hajduk AM, Lemon SC, McManus DD, et al. Cognitive impairment and self-care in heart failure. Clin Epidemiol. 2013;5:407–16.
Maeda U, Shen BJ, Schwarz ER, Farrell KA, Mallon S. Self-efficacy mediates the associations of social support and depression with treatment adherence in heart failure patients. Int J Behav Med. 2013;20:88–96.
McCullough PA, Philbin EF, Spertus JA, Kaatz S, Sandberg KR, Weaver WD. Confirmation of a heart failure epidemic: findings from the Resource Utilization Among Congestive Heart Failure (REACH) study. J Am Coll Cardiol. 2002;39:60–9.
Broadhead WE, Gehlbach SH, De Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26:709–23.
Barber JH, Wallis JB, McKeating E. A postal screening questionnaire in preventive geriatric care. J R Coll Gen Pract. 1980;30:49–51.
Larizgoitia A, Larizgoitia I. Adaptación en nuestro medio de una encuesta para la detección de ancianos con riesgo de dependencia. Rev Gerontol. 1996;6:224–31.
De Vries NM, Staal JB, Van Ravensberg CD, Hobbelen JS, Olde Rikkert MG, Nijhuis-van der Sanden MW. Outcome instruments to measure frailty: a systematic review. Ageing Res Rev. 2011;10:104–14.
Swedberg K, Komajda M, Bohm M, et al. Effects on outcomes of heart rate reduction by ivabradine in patients with congestive heart failure: is there an influence of beta-blocker dose?: findings from the SHIFT (Systolic Heart failure treatment with the I (f) inhibitor ivabradine Trial) study. J Am Coll Cardiol. 2012;59:1938–45.
Graham S, Ye S, Qian M, et al. Cognitive function in ambulatory patients with systolic heart failure: insights from the warfarin versus aspirin in reduced cardiac ejection fraction (WARCEF) trial. PLoS ONE. 2014;9, e113447.
Lees R, Selvarajah J, Fenton C, et al. Test accuracy of cognitive screening tests for diagnosis of dementia and multidomain cognitive impairment in stroke. Stroke. 2014;45:3008–18.
Zhou Y, Ortiz F, Nunez C, et al. Use of the MoCA in Detecting Early Alzheimer’s Disease in a Spanish-Speaking Population with Varied Levels of Education. Dement Geriatr Cogn Dis Extra. 2015;5:85–95.
Hanon O, Vidal JS, De GP, et al. Prevalence of memory disorders in ambulatory patients aged >/=70 years with chronic heart failure (from the EFICARE study). Am J Cardiol. 2014;113:1205–10.
Chaudhry SI, McAvay G, Chen S, et al. Risk factors for hospital admission among older persons with newly diagnosed heart failure: findings from the Cardiovascular Health Study. J Am Coll Cardiol. 2013;61:635–42.
Ganguli M, Fu B, Snitz BE, Hughes TF, Chang CC. Mild cognitive impairment: incidence and vascular risk factors in a population-based cohort. Neurology. 2013;80:2112–20.
Davis KK, Allen JK. Identifying cognitive impairment in heart failure: a review of screening measures. Heart Lung. 2013;42:92–7.
Hajduk AM, Kiefe CI, Person SD, Gore JG, Saczynski JS. Cognitive change in heart failure: a systematic review. Circ Cardiovasc Qual Outcomes. 2013;6:451–60.
Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST. Practice parameter: early detection of dementia: mild cognitive impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:1133–42.
Arslanian-Engoren C, Giordani BJ, Algase D, Schuh A, Lee C, Moser DK. Cognitive dysfunction in older adults hospitalized for acute heart failure. J Card Fail. 2014;20:669–78.
Almeida OP, Garrido GJ, Beer C, Lautenschlager NT, Arnolda L, Flicker L. Cognitive and brain changes associated with ischaemic heart disease and heart failure. Eur Heart J. 2012;33:1769–76.
Hofmeijer J, Mulder AT, Farinha AC, Van Putten MJ, Le FJ. Mild hypoxia affects synaptic connectivity in cultured neuronal networks. Brain Res. 2014;1557:180–9.
Kerola T, Nieminen T, Hartikainen S, Sulkava R, Vuolteenaho O, Kettunen R. B-type natriuretic peptide as a predictor of declining cognitive function and dementia--a cohort study of an elderly general population with a 5-year follow-up. Ann Med. 2010;42:207–15.
Azab B, Bibawy J, Harris K, et al. Value of albumin-globulin ratio as a predictor of all-cause mortality after non-ST elevation myocardial infarction. Angiology. 2013;64:137–45.
Uthamalingam S, Kandala J, Daley M, et al. Serum albumin and mortality in acutely decompensated heart failure. Am Heart J. 2010;160:1149–55.
Rogers TK, Bowman CE. Cognitive impairment associated with beta-blockade in the elderly. Postgrad Med J. 1990;66:1050–2.
Solomon S, Hotchkiss E, Saravay SM, Bayer C, Ramsey P, Blum RS. Impairment of memory function by antihypertensive medication. Arch Gen Psychiatry. 1983;40:1109–12.
Kumar A, Dogra S. Neuroprotective effect of carvedilol, an adrenergic antagonist against colchicine induced cognitive impairment and oxidative damage in rat. Pharmacol Biochem Behav. 2009;92:25–31.
Wagner G, Icks A, Abholz HH, Schroder-Bernhardi D, Rathmann W, Kostev K. Antihypertensive treatment and risk of dementia: a retrospective database study. Int J Clin Pharmacol Ther. 2012;50:195–201.
Haring B, Leng X, Robinson J, et al. Cardiovascular disease and cognitive decline in postmenopausal women: results from the Women’s Health Initiative Memory Study. J Am Heart Assoc. 2013;2, e000369.
Zuccala G, Marzetti E, Cesari M, et al. Correlates of cognitive impairment among patients with heart failure: results of a multicenter survey. Am J Med. 2005;118:496–502.
Ottenbacher KJ, Karmarkar A, Graham JE, et al. Thirty-day hospital readmission following discharge from postacute rehabilitation in fee-for-service Medicare patients. JAMA. 2014;311:604–14.
Hawkins MA, Dolansky MA, Schaefer JT, et al. Cognitive Function in Heart Failure Is Associated With Nonsomatic Symptoms of Depression But Not Somatic Symptoms. J Cardiovasc Nurs. 2015;30:E9–E17.
Newman AB, Fitzpatrick AL, Lopez O, et al. Dementia and Alzheimer’s disease incidence in relationship to cardiovascular disease in the Cardiovascular Health Study cohort. J Am Geriatr Soc. 2005;53:1101–7.
Carpenter I, Gambassi G, Topinkova E, et al. Community care in Europe. The Aged in Home Care project (AdHOC). Aging Clin Exp Res. 2004;16:259–69.
Kono Y, Yamada S, Iwatsu K, et al. Predictive value of functional limitation for disease severity in patients with mild chronic heart failure. J Cardiol. 2012;60:411–5.
Afilalo J, Karunananthan S, Eisenberg MJ, Alexander KP, Bergman H. Role of frailty in patients with cardiovascular disease. Am J Cardiol. 2009;103:1616–21.
Acknowledgments
We appreciate the help of the Primary Healthcare Division of Barcelona (Institut Català de la Salut) in the development of the study. We thank to Aida Cuenca Royo and Paula Martinez Bel who collected part of the sample.
Availability of data and materials
The data is available upon request from the authors.
Authors’ contributions
JC, MJG, GS, JV participated in the study conception and design. JC, MJG, JV, GS, CE, SQ, MC, JPC, and JB participated in the analysis and interpretation of data. MJG and JC participated in the drafting of the manuscript. Critically revising the manuscript for important intellectual content and providing final approval for the manuscript to be submitted was a collective task participating JC, MJG, JV, GS, CE, SQ, MC, JPC, and JB. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests in this work.
Consent for publication
Not applicable.
Ethical approval and consent to participate
The study protocol was approved by the local committee of ethics for clinical research (Comité ético de Investigación clínica del Instituto Municipal de Asistencia Sanitaria (CEIC-IMAS-IMIM Hospital del Mar Medical Research Institute N°: 2004/1788/l) and all patients gave written informed consent after recruitment.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
González-Moneo, M.J., Sánchez-Benavides, G., Verdu-Rotellar, J.M. et al. Ischemic aetiology, self-reported frailty, and gender with respect to cognitive impairment in chronic heart failure patients. BMC Cardiovasc Disord 16, 163 (2016). https://doi.org/10.1186/s12872-016-0349-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-016-0349-5