Abstract
Objective
To explore the relationship between the timing of non-emergency surgery in mild or asymptomatic SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) infected individuals and the quality of postoperative recovery from the time of confirmed infection to the day of surgery.
Methods
We retrospectively reviewed the medical records of 300 cases of mild or asymptomatic SARS-CoV-2 infected patients undergoing elective general anaesthesia surgery at Yijishan Hospital between January 9, 2023, and February 17, 2023. Based on the time from confirmed SARS-CoV-2 infection to the day of surgery, patients were divided into four groups: ≤2 weeks (Group A), 2–4 weeks (Group B), 4–6 weeks (Group C), and 6–8 weeks (Group D). The primary outcome measures included the Quality of Recovery-15 (QoR-15) scale scores at 3 days, 3 months, and 6 months postoperatively. Secondary outcome measures included postoperative mortality, ICU admission, pulmonary complications, postoperative length of hospital stay, extubation time, and time to leave the PACU.
Results
Concerning the primary outcome measures, the QoR-15 scores at 3 days postoperatively in Group A were significantly lower compared to the other three groups (P < 0.05), while there were no statistically significant differences among the other three groups (P > 0.05). The QoR-15 scores at 3 and 6 months postoperatively showed no statistically significant differences among the four groups (P > 0.05). In terms of secondary outcome measures, Group A had a significantly prolonged hospital stay compared to the other three groups (P < 0.05), while other outcome measures showed no statistically significant differences (P > 0.05).
Conclusion
The timing of surgery in mild or asymptomatic SARS-CoV-2 infected patients does not affect long-term recovery quality but does impact short-term recovery quality, especially for elective general anaesthesia surgeries within 2 weeks of confirmed infection. Therefore, it is recommended to wait for a surgical timing of at least greater than 2 weeks to improve short-term recovery quality and enhance patient prognosis.
Similar content being viewed by others
Introduction
Surgery stands as the primary and most efficacious therapeutic intervention for disease management. Perioperative safety is a universally shared concern. Medical teams, particularly anaesthetists, shoulder significant responsibilities in anticipating and mitigating perioperative risks, necessitating proficiency in assessment and management. However, during unforeseen public health emergencies, numerous risk factors necessitate validation through investigative studies to provide evidence for clinical practice.
Since the first confirmed case of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection in 2019, as of December 1, 2022, the global reach of the Corona Virus Disease 2019 (COVID-19) pandemic has impacted over 200 countries and regions, with over 643 million confirmed cases and more than 6.63 million deaths. Individuals infected with SARS-CoV-2 may exhibit short-term and long-term multi-systemic sequelae [1,2,3,4,5], resulting in multi-organ damage and, in severe instances, mortality [6,7,8,9,10,11,12]. In November 2021, the SARS-CoV-2 Omicron variant was identified in South Africa [13], rapidly disseminating, and by December 2022, it emerged as the predominant strain causing infections in Anhui Province, China. Among the numerous variants during the COVID-19 pandemic, Omicron displays the highest mutation count, marked by high transmissibility and lower pathogenicity, leading to significant reductions in hospitalization, severity, and mortality rates [14,15,16]. In response to the evolving situation, China classified SARS-CoV-2 infection as a national category B infectious disease on January 8, 2023. With the easing of stringent epidemic control measures, there has been a notable increase in individuals infected with the Omicron variant awaiting surgery.
SARS-CoV-2 infection significantly heightens perioperative risks for patients. While early expert consensus suggested that most mild or asymptomatic SARS-CoV-2-infected individuals could undergo surgery after 7 weeks of diagnosis (except in cases of clinical urgency and risks surpassing the progression of the disease) [17], the substantial number of patients requiring timely surgery not only imposes a burden on patients during the 7-week waiting period but also significantly increases the healthcare load on society. Furthermore, given the distinctive pathogenic characteristics of Omicron differing markedly from previous strains, investigating the appropriate timing for surgery holds paramount significance.
This study investigates the short-term and long-term postoperative recovery quality of SARS-CoV-2-infected individuals at Yijishan Hospital, Wannan Medical College, considering the widespread transmission of the Omicron variant and post-COVID-19 vaccination. The aim is to examine the impact of different timings for surgery under general anaesthesia on the postoperative recovery quality in SARS-CoV-2-infected individuals.
Materials and methods
Following ethical approval by the Ethics Committee of Yijishan Hospital of Wannan Medical College (Protocol Number: 2023-68) and with waiver of individual written informed consent, we conducted a retrospective cohort study including patients who had elective general anaesthesia surgery at Yijishan Hospital from January 9, 2023, to February 17, 2023. The inclusion criteria were: patients aged 18 to 75 years, with an American Society of Anaesthesiologists (ASA) classification of I to III, who had been confirmed as having a mild or asymptomatic SARS-CoV-2 infection at least 8 weeks prior to surgery. Confirmation of infection was based on the positive detection of viral nucleic acid from nasal or throat swab antigen tests or reverse transcription-polymerase chain reaction (RT-PCR) for the novel coronavirus. Exclusion criteria included: individuals with mental disorders, those with severe dysfunction of the heart, lungs, liver, or kidneys, and individuals with severe hearing or communication impairments.
Data were extracted by reviewing the electronic medical records from the hospital’s information system, which included age, gender, body mass index (BMI), hypertension, diabetes, chest computed tomography (CT) findings with inflammation, ASA classification, grade of surgery, operation time, potential of hydrogen (PH), oxygenation index, intraoperative bleeding, intraoperative fluid replacement, incidence of intraoperative use of vasoactive drugs, intensive care unit (ICU) admission, extubation time, time to leave the post-anaesthesia care unit (PACU), postoperative length of hospital stay (day 0 defined as the day of surgery), postoperative complications, and the QoR-15 scale scores at 3 days, 3 months, and 6 months postoperatively.
Anaesthetic procedure
All patients underwent routine fasting and abstinence from liquids before surgery. Upon admission, all patients received standard anaesthetic management, with routine monitoring of non-invasive blood pressure (BP), heart rate (HR), pulse oxygen saturation (SpO2), temperature (T), and the establishment of upper limb venous access for intravenous infusion of electrolyte solution at 6–8 ml/(kg·h). Anaesthetic induction involved the intravenous administration of midazolam 0.02–0.03 mg/kg, sufentanil 0.3–0.4 µg/kg, etomidate 0.2–0.3 mg/kg, and cisatracurium 0.15–0.2 mg/kg. After meeting intubation criteria, patients received endotracheal intubation or a laryngeal mask, with ventilation set to controlled volume ventilation. Respiratory parameters were adjusted with oxygen flow at 2 L/min, tidal volume (VT) at 6–8 ml/kg, respiratory rate at 12–14 breaths/min, maintaining PETCO2 at 35–45 mmHg, and FiO2 at 100%. Anaesthetic maintenance involved intravenous anaesthesia, with propofol at 4–8 mg/(kg·h), remifentanil at 0.1–0.2 µg/(kg·min), and intermittent injections of cisatracurium at 2–4 mg. Bispectral index (BIS) depth monitoring was maintained between 40 and 60, and arterial blood gas analysis was conducted 15 min after anaesthetic maintenance initiation. Throughout the anaesthetic process, mean arterial pressure (MAP) was maintained within ± 20% of baseline, HR between 60 and 100 beats/min, and body temperature between 36 and 37 °C. After surgery, anaesthetic agents were discontinued, and patients were transferred to the PACU or ICU. Tracheal tubes or laryngeal masks were removed upon meeting extubation criteria, and patients meeting transfer standards were returned to the ward.
Main outcome measures
The primary outcome measures comprised QoR-15 scale scores on postoperative day 3, postoperative month 3, and postoperative month 6. Secondary outcome measures included endotracheal tube removal time, PACU departure time, length of hospital stay (day 0 defined as the day of surgery), ICU admission, postoperative mortality, pulmonary infections, respiratory failure, sepsis, and fatigue incidence.
Statistical methods
Statistical analyses were performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA). Normally distributed continuous data were expressed as mean ± standard deviation, with intergroup comparisons conducted through one-way analysis of variance. Non-normally distributed continuous data were presented as median (25th percentile-75th percentile), and intergroup comparisons were executed using the Kruskal-Wallis test. Adjusted pairwise comparisons for P-values were performed with Bonferroni correction, followed by the Mann-Whitney U test. Count data were reported as frequency/percentage (%), and intergroup comparisons were analysed using the chi-squared test. The significance level was set at α = 0.05, with P < 0.05 indicating statistical significance.
Results
Participants
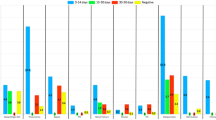
Based on the inclusion and exclusion criteria, a preliminary screening of electronic medical records yielded 313 eligible patients. Further review of anesthesia records and postoperative follow-up revealed that one patient’s surgery was aborted due to an unexpected asthma attack, and that 12 patients had incomplete postoperative follow-up data. Consequently, data from these 13 patients were eliminated, ultimately leaving a total of 300 patients in the study. Then patients’ data have been categorized by the time interval between the diagnosis of initial SARS-CoV-2 infection and the surgery, as depicted in Fig. 1.
Demographic data
There were no statistically significant differences (P > 0.05) among the four groups concerning patients’ age, gender, BMI, hypertension, diabetes, preoperative chest CT, ASA classification, surgical complexity, operative duration, arterial blood PH, oxygenation index, intraoperative bleeding, intraoperative fluid replacement and incidence of intraoperative use of vasoactive drugs. The specifics are delineated in Table 1.
QoR-15 scale scores on postoperative day 3, month 3 and month 6
On postoperative day 3, Group A exhibited consistently lower median QoR-15 scores [124 (110~129)] compared to Group B [128 (119~134)], Group C [131 (122~138)], and Group D [131 (124~138)] (P < 0.05) (Fig. 2a). However, at postoperative months 3 and 6, no statistically significant differences in QoR-15 scores were observed among the four groups (P > 0.05) (Fig. 2b, c).
To identify whether the surgical complexity and the ASA grade have any influence on the QoR-15 scores of postoperative day 3, we stratified comparison. No statistically significant differences (P > 0.05) were noted in the subgroup Grade of surgery 1–2 compared to the subgroup Grade of surgery 3–4, as outlined in Table 2. However, the patients accessed as ASA III have a lower QoR-15 scores in the group A (P = 0.003) and group B (P = 0.007), compared with the ASA I-II group, while there is no significant difference both in the group C and D (P > 0.05), as outlined in Table 3.
Patient outcomes
Hospital Stay, Adverse Postoperative Outcomes, Extubation Time, and PACU Departure Time: In contrast to Group A, patients in Group B, C, and D demonstrated significantly shorter median hospital stays (P < 0.05). No statistically significant differences (P > 0.05) were noted among the four groups concerning Postoperative Mortality, ICU Admission, Pulmonary Infections, Respiratory Failure, Sepsis, Fatigue Incidence, Extubation time, and PACU departure Time, as outlined in Table 4.
Extubation time, PACU departure time and Hospital Stay were presented as median (interquartile ranges: 25th percentile-75th percentile); other continuous variables were represented as the number (percent). P value tested by rank sum test or chi-square test, according to the specific situation. *P < 0.05 compared to Group A.
Discussion
Against the backdrop of widespread COVID-19 vaccination and the emergence of the Omicron variant, our study delved into the correlation between short- and long-term recovery quality and the timing of surgery in patients undergoing general anaesthesia post-SARS-CoV-2 infection. We analysed the data from a six-month follow-up with patients diagnosed with mild or asymptomatic SARS-CoV-2 infection. Notably, the group with an infection duration of less than two weeks displayed diminished QoR-15 scores three days postoperatively and an extended hospital stay. Our findings suggest that scheduling elective general anaesthesia surgery more than two weeks after the diagnosis of mild or asymptomatic SARS-CoV-2 infection may be more favourable for enhancing postoperative recovery quality.
The QoR-15 scale, introduced in 2013 for assessing overall anaesthesia and postoperative recovery quality [18], provides a comprehensive and more efficient evaluation compared to the QoR-40 scale. It is presently endorsed as a standard measurement for clinical trial outcomes [19]. With a total score of 150, higher scores signify superior postoperative recovery quality, and scores of 118 or above are indicative of a good recovery [20]. Our study indicates that the majority of patients, 80% on day 3, and 99% at 3 and 6 months postoperatively, achieved QoR-15 scores of 118 or above, indicating good postoperative recovery quality. However, the group with an infection duration of less than two weeks exhibited significantly lower QoR-15 scores at three days postoperatively, consistent with prior research [21, 22]. This may be attributed to inconsistent waiting times post-SARS-CoV-2 infection and anaesthetic agents known to suppress the body’s immune function, potentially prolonging active viral replication in patients with compromised immunity, thus slowing recovery from SARA-CoV-2 [23]. Research indicates that patients infected with the Omicron variant within eight weeks before surgery experience a shorter postoperative hospital stay and a significantly reduced risk of adverse postoperative outcomes [24,25,26]. This aligns with our findings, where the group with an infection duration of less than two weeks exhibited a significantly longer median hospital stay, aligning with the results of QoR-15 scores three days postoperatively. The consistency between these findings underscores the reliability of study results, emphasizing that undergoing surgery shortly after SARS-CoV-2 infection is not conducive to enhancing recovery quality. SARS-CoV-2 infection may be associated with short-term and long-term multi-system sequelae, including chronic pulmonary dysfunction, cognitive impairment, psychological distress, chronic fatigue, etc. [1,2,3,4,5]. Our study identified one patient in Group A who died due to respiratory failure combined with hepatic and renal failure, one readmitted for sepsis, and four reporting fatigue with slight exertion. In Group B, three patients reported slight fatigue with movement, while in Group C, one patient died due to cancer spread, two reported fatigue with slight exertion. In Group D, two patients reported slight fatigue with movement, consistent with previous reports. However, comparisons among the groups revealed no statistically significant differences. Our study has not observed a significant impact of Omicron variant infection on postoperative survival rates, contrary to previous research indicating an increased risk of postoperative mortality following SARS-CoV-2 infection. Possible reasons include: first, our study focused on patients with mild or asymptomatic infection; second, the low pathogenicity of the Omicron variant itself [27,28,29,30,31]; third, widespread vaccination in China; fourth, previous studies were conducted before the Omicron variant became the dominant strain [32]. Investigating the postoperative short- and long-term sequelae of SARS-CoV-2 infection in Omicron variant-infected individuals with expanded inclusion remains clinically significant. Previous studies primarily explored postoperative mortality and pulmonary complication rates in SARS-CoV-2-infected patients, often conducted before the emergence of the Omicron variant and widespread vaccination, making some findings less applicable to the current scenario. The Omicron variant primarily affects the upper respiratory tract, with most infected individuals exhibiting normal chest CT scans [27,28,29,30,31, 33], resulting in a significant reduction in mortality and pulmonary complications 30 days postoperatively. Therefore, exploring postoperative recovery quality holds greater clinical significance.
We stratified comparison and found that the ASA grade is more sensitive than surgical grade on influencing the quality of recovery. The possible reasons may be as follows: Firstly, the sample size is too small to present significant difference between in the subgroups of surgery grade 1–2 and 3–4 on the QoR-15 scores; Secondly, the surgical grading is based on technical difficulty, complexity and risk of surgery, and a high surgical grade does not mean a high surgical trauma to patients, especially the rapid development of minimally invasive surgery in recent years; Finally, the ASA grading may be more comprehensive, considering not only the surgery grade but also general condition, including the SARS-CoV-2-infected, of the patient observed before anaesthesia. However, we cannot conclude whether the timing of surgery based on the duration of SARS-CoV-2 infection or the grade of surgery has a greater impact on the quality of postoperative recovery in the study. Because, in the precondition with no difference at the proportions of surgery grades between the subgroups, we only explored the influence of the timing of surgery after SARS-CoV-2 infection on the quality of postoperative recovery.
This study has several limitations. Firstly, being a single-center study, the sample size is limited, and the surveyed population is regionally constrained. Larger-scale studies are required for validation. Secondly, some patients with a history of SARS-CoV-2 infection might have been misclassified as never infected. This is particularly plausible for asymptomatic patients who might not have undergone nucleic acid testing and, consequently, were not included in this study. Additionally, our study did not include an uninfected group, lacking a blank control. Lastly, this study is based on the time from SARS-CoV-2 diagnosis to the day of surgery, but delays in diagnosis might have occurred in some patients, potentially underestimating the true interval between infection and surgery.
In summary, this article examines the prognosis of elective general anaesthesia surgery at different timings in patients with mild or asymptomatic SARS-CoV-2 infection. Despite the relatively low pathogenicity of the Omicron variant, immunosuppression is prevalent in surgical patients. The group with an infection duration of fewer than two weeks undergoing non-emergency general anaesthesia surgery showed a decreased short-term postoperative recovery quality, prolonged hospital stay, and increased risk of postoperative complications, without affecting long-term postoperative recovery quality and postoperative mortality. Therefore, we recommend that patients with mild or asymptomatic SARS-CoV-2 infection wait for more than two weeks before undergoing non-emergency general anaesthesia surgery, as it proves to be a more advantageous choice.
Data availability
The datasets generated and/or analysed during this study are not publicly available due to institutional policy on data confidentiality but are available from the corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anaesthesiologists
- BIS:
-
Bispectral index
- BMI:
-
Body Mass Index
- BP:
-
Blood Pressure
- CT:
-
Computed Tomography
- COVID-19:
-
Corona Virus Disease 2019
- ECG:
-
Electrocardiogram
- FiO2 :
-
Fraction of Inspiration O2
- HR:
-
Heart Rate
- ICU:
-
Intensive Care Unit
- MAP:
-
Mean Arterial Pressure
- PACU:
-
Post-Anaesthesia Care Unit
- PH:
-
Potential of Hydrogen
- PETCO2 :
-
Peak Expiratory CO2 Pressure
- SpO2:
-
Pulse Oxygen Saturation
- T:
-
Temperature
- SARS-CoV-2:
-
Severe Acute Respiratory Syndrome Coronavirus 2
- VT :
-
Tidal Volume
References
Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study[J]. Lancet, 2021, 397(10270): 220–232.
Zhao Y M, Shang Y M, Song W B, et al. Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery[J]. EClinicalMedicine, 2020, 25: 100463.
Carfì A, Bernabei R, Landi F. Persistent Symptoms in Patients After Acute COVID-19[J]. Jama, 2020, 324(6): 603–605.
Ceban F, Ling S, Lui L M W, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis[J]. Brain Behav Immun, 2022, 101: 93–135.
Mahmoud Z, East L, Gleva M, et al. Cardiovascular symptom phenotypes of post-acute sequelae of SARS-CoV-2[J]. Int J Cardiol, 2022, 366: 35–41.
Han X, Ye Q. Kidney involvement in COVID-19 and its treatments[J]. J Med Virol, 2021, 93(3): 1387–1395.
Tian D, Ye Q. Hepatic complications of COVID-19 and its treatment[J]. J Med Virol, 2020, 92(10): 1818–1824.
Ye Q, Lu D, Shang S, et al. Crosstalk between coronavirus disease 2019 and cardiovascular disease and its treatment[J]. ESC Heart Fail, 2020, 7(6): 3464–3472.
Luo H C, You C Y, Lu S W, et al. Characteristics of coagulation alteration in patients with COVID-19[J]. Ann Hematol, 2021, 100(1): 45–52.
Ye Q, Wang B, Zhang T, et al. The mechanism and treatment of gastrointestinal symptoms in patients with COVID-19[J]. Am J Physiol Gastrointest Liver Physiol, 2020, 319(2): G245-g252.
Gupta A, Madhavan M V, Sehgal K, et al. Extrapulmonary manifestations of COVID-19[J]. Nat Med, 2020, 26(7): 1017–1032.
Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study[J]. Lancet, 2020, 395(10223): 507–513.
Classification of Omicron (B.1.1.529): SARS-CoV-2 Variant of Concern[EB/OL]. [2023-06-01]. https://www.who.int/news/item/26-11-2021-classification-of-omicron-(b.1.1.529)-sars-cov-2-variant-of-concern.
Xu R, Wang W, Zhang W. As the SARS-CoV-2 virus evolves, should Omicron subvariant BA.2 be subjected to quarantine, or should we learn to live with it?[J]. Front Public Health, 2022, 10: 1039123.
Fan Y, Li X, Zhang L, et al. SARS-CoV-2 Omicron variant: recent progress and future perspectives[J]. Signal Transduct Target Ther, 2022, 7(1): 141.
Halfmann P J, Iida S, Iwatsuki-Horimoto K, et al. SARS-CoV-2 Omicron virus causes attenuated disease in mice and hamsters[J]. Nature, 2022, 603(7902): 687–692.
El-Boghdadly K, Cook T M, Goodacre T, et al. SARS-CoV-2 infection, COVID-19 and timing of elective surgery: A multidisciplinary consensus statement on behalf of the Association of Anaesthetists, the Centre for Peri-operative Care, the Federation of Surgical Specialty Associations, the Royal College of Anaesthetists and the Royal College of Surgeons of England[J]. Anaesthesia, 2021, 76(7): 940–946.
Stark P A, Myles P S, Burke J A. Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15[J]. Anaesthesiology, 2013, 118(6): 1332-40.
Kleif J, Waage J, Christensen K B, et al. Systematic review of the QoR-15 score, a patient- reported outcome measure measuring quality of recovery after surgery and anaesthesia[J]. Br J Anaesth, 2018, 120(1): 28–36.
Myles P S, Shulman M A, Reilly J, et al. Measurement of quality of recovery after surgery using the 15-item quality of recovery scale: a systematic review and meta-analysis[J]. Br J Anaesth, 2022, 128(6): 1029–1039.
Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study[J]. Lancet, 2020, 396(10243): 27–38.
Outcomes and Their State-level Variation in Patients Undergoing Surgery With Perioperative SARS-CoV-2 Infection in the USA: A Prospective Multicenter Study[J]. Ann Surg, 2022, 275(2): 247–251.
Ackerman R S, Luddy K A, Icard B E, et al. The Effects of Anaesthetics and Perioperative Medications on Immune Function: A Narrative Review[J]. Anaesth Analg, 2021, 133(3): 676–689.
Le S T, Kipnis P, Cohn B, et al. COVID-19 Vaccination and the Timing of Surgery Following COVID-19 Infection[J]. Ann Surg, 2022, 276(5): e265-e272.
Prasad N K, Lake R, Englum B R, et al. COVID-19 Vaccination Associated With Reduced Postoperative SARS-CoV-2 Infection and Morbidity[J]. Ann Surg, 2022, 275(1): 31–36.
Garnier M, Constantin J M, Cinotti R, et al. Association of preoperative COVID-19 and postoperative respiratory morbidity during the Omicron epidemic wave: the DROMIS-22 multicentre prospective observational cohort study[J]. EClinicalMedicine, 2023, 58: 101881.
Menni C, Valdes A M, Polidori L, et al. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study[J]. Lancet, 2022, 399(10335): 1618–1624.
Jassat W, Abdool Karim S S, Mudara C, et al. Clinical severity of COVID-19 in patients admitted to hospital during the omicron wave in South Africa: a retrospective observational study[J]. Lancet Glob Health, 2022, 10(7): e961-e969.
Davies M A, Kassanjee R, Rousseau P, et al. Outcomes of laboratory-confirmed SARS-CoV-2 infection in the Omicron-driven fourth wave compared with previous waves in the Western Cape Province, South Africa[J]. Trop Med Int Health, 2022, 27(6): 564–573.
Ulloa A C, Buchan S A, Daneman N, et al. Estimates of SARS-CoV-2 Omicron Variant Severity in Ontario, Canada[J]. Jama, 2022, 327(13): 1286–1288.
Abdullah F, Myers J, Basu D, et al. Decreased severity of disease during the first global omicron variant covid-19 outbreak in a large hospital in tshwane, south africa[J]. Int J Infect Dis, 2022, 116: 38–42.
Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study[J]. Anaesthesia, 2021, 76(6): 748–758.
Tsakok M T, Watson R A, Saujani S J, et al. Reduction in Chest CT Severity and Improved Hospital Outcomes in SARS-CoV-2 Omicron Compared with Delta Variant Infection[J]. Radiology, 2023, 306(1): 261–269.
Acknowledgements
Not applicable.
Funding
This study was supported by funding from Anhui University Research Project (No. 2023AH040252, 2023AH051745), Natural Science Foundation of Anhui Province (No.2208085MC55), Wannan Medical College Research Fund Project (No. WK2022F03), the Key Project of Anhui Province ’Leading the Charge with Open Competition’, Anhui, China, and Anhui Province Clinical Key Specialty Construction Project.
Author information
Authors and Affiliations
Contributions
Q.B.W., Y.L.W. and Y.F.W. conceptualized and designed the study, data collection, wrote the main manuscript text. H.C. and W.C. carried out the initial analyses, reviewed and revised the manuscript. Y.L.W. and Y.Q.C. coordinated and supervised the data collection, critically reviewed the manuscript, and approved the final manuscript as submitted. All authors reviewed the manuscript and approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol approved by the Ethics Committee of Yijishan Hospital of Wannan Medical College (2023-68). All methods were carried out in accordance with relevant guidelines and regulations. Due to retrospective nature of the study, the informed consent is waived by the Ethics Committee of Yijishan Hospital of Wannan Medical College.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, QB., Wang, YL., Wang, YF. et al. Impact of non-emergency surgical timing on postoperative recovery quality in mild or asymptomatic SARS-CoV-2 infected patients: a grouped cohort study. BMC Anesthesiol 24, 225 (2024). https://doi.org/10.1186/s12871-024-02600-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-024-02600-y