Abstract
Background
Esketamine is increasingly used in clinical anesthesia. The effect of esketamine on the blood flow velocity of the middle cerebral artery has a clinical guiding effect. To investigate the effect of esketamine combined with propofol-induced general anesthesia for endotracheal intubation on the blood flow velocity of middle cerebral artery and hemodynamics during the induction period.
Methods
The randomized clinical trial included 80 patients aged 20-65 years who would undergo non-intracranial elective surgery under general anesthesia in our hospital from May 2022 to May 2023. The participants were divided into two groups based on anesthesia drugs: sufentanil 0.5μg/kg (group C) or 1.5mg/kg esketamine (group E). The primary outcome was variation value in average cerebral blood velocity. The secondary outcomes included cerebral blood flow velocities (CBFV), blood pressure (BP) and heart rate (HR) at four different time points: before induction of general anesthesia (T0), 1 min after the induction drug injected (T1), before endotracheal intubation (T2), and 1min after endotracheal intubation (T3). The occurrence of hypotension, hypertension, tearing and choking during induction was also documented.
Results
The variation of average CBFV from time T0 to T2(ΔVm1) and the variation from time T3 to T0 (ΔVm2) were not obviously different. The median consumption of intraoperative sufentanil in group C was obviously lower than that in group E. At T1, the mean HR of group E was significantly higher than that of group C. At T2 and T3, the BP and HR of group E were obviously higher than that of group C. At T2, the CBFV in the group E were obviously higher than those in the group C. The incidence of hypotension was significantly reduced in the group E compared with the group C. There were no differences in the other outcomes.
Conclusions
The induction of esketamine combined with propofol does not increase the blood flow velocity of middle cerebral artery. Esketamine is advantageous in maintaining hemodynamic stability during induction. Furthermore, the administration of esketamine did not result in an increased incidence of adverse effects.
Trial Registration
15/06/2023 clinicaltrials.gov ChiCTR2300072518 https://www.chictr.org.cn/bin/project/edit?pid=176675.
Similar content being viewed by others
Introduction
Ketamine is an intravenous anesthetic agent that exhibits favorable sedative and analgesic properties, which has a stimulating effect on the sympathetic nerves and circulation, and ketamine is the only drug in intravenous anesthesia that can stimulate brain function. Ketamine could stimulate the sympathetic nerves, so that it causes smooth muscle relaxation and bronchiectasis. It improves lung compliance and reduces airway resistance when given intravenously. However, it may also increase bronchial secretions, which has no positive effect on asthma [1]. Ketamine has been previously reported to increase intracranial pressure (ICP), and its clinical use was limited by the end of the 20th century due to its psychiatric adverse effects [2]. Although ketamine can affect cerebral hemodynamics through direct drug effects [3], many studies have shown that ketamine use does not cause increased ICP in patients with acute brain injury, and even if a few transient increases in ICP occur, there is no evidence of harmful consequences [4]. The neurotoxicity and psychoneurological adverse effects caused by ketamine are dose- and time-dependent [5]. Ketamine combined with propofol anesthesia has been shown in studies to not result in an increase of middle cerebral artery flow velocity and there are no neurologic complications associated with the use of ketamine plus propofol anesthesia in mechanically ventilated patients [6]. At the same time, studies suggest that subanesthetic doses of ketamine may have neuroprotective effects [7, 8].
Esketamine (also known as dextroketamine) is the dextro optical isomer of ketamine. Compared to traditional racemic ketamine, its potency is higher and it has a stronger sedative and analgesic effect with fewer adverse reactions. Studies have shown that dextroketamine alone increases cerebral blood flow velocity and volume [9]. Therefore, further clinical trials are necessary to determine the effect of combining esketamine with propofol on cerebral blood flow velocity. This study aimed to investigate the effect of esketamine combined with propofol on the blood flow velocity and hemodynamics of the middle cerebral artery in patients undergoing non-neurosurgical craniotomy,and the feasibility of esketamine as an analgesic for inducing general anesthesia for endotracheal intubation, providing more evidence for the use of esketamine in neurosurgical craniotomy.
Materials and Methods
Study Design and Population
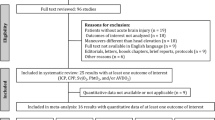
This signal-center, randomized clinical trial was conducted at the First Affiliate Hospital of Chongqing Medical University in Chongqing Province, China, from March 2022 to March 2023. The study protocol was approved by the ethics committees of the Clinical Trial Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (NO.2022-072, 23/03/2022), and registered in the Chinese Clinical Trial Registratiy Center. Written informed consent was obtained from all patients or their families. This report follows the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline for randomized studies. The full trial protocol is available in (Fig. 1).
Study Procedures and Data Collection
Every patient had regular induction of intravenous anesthesia. After admission, open patient's venous access to the upper extremities. After the patient's venous access was opened, the patient's intravenous crystalloid (Ringer’s solution) was routinely given 5ml/kg. At the same time, routinely monitor heart rate (HR), oxygen saturation (SpO2), electrocardiogram (ECG), temperature, and monitor invasive arterial blood pressure by radial artery puncture after Allen test (+). Before induction, there had adequate nitrogen removal and oxygen then patients got slow intravenous injection of anesthetic drugs. The control group (group C) was midazolam 0.04 mg/kg, propofol 1.5 mg/kg, sufentanil 0.4 μg/kg, vicuronium bromide 0.1 mg/kg, the experimental group (group E) was midazolam 0.04 mg/kg, propofol 1.5 mg/kg, esketamine (Jiang Su Hengrui Pharmaceutical Co., Ltd., specification is 2 ml: 50 mg, Approval number: Sinopharm H20193336) 0.5 mg/kg, vecuronium bromide 0.1 mg/kg. Examination was performed using a transcranial color-code doppler (TCCD) machine (GE Venus TM) fitted with 2.0-MHz sector array transducer. The ipsilateral or contralateral middle cerebral artery (MCA) was insonated through the temporal window at a depth of 46–60 mm. Observe and record the changes of middle cerebral artery blood flow velocity (Vp, Vm, Vd), systolic blood pressure (SBP), average blood pressure (ABP), diastolic blood pressure (DBP) and heart rate (HR) before induction of general anesthesia (T0), 1 min after the induction drug injected (T1), before endotracheal intubation (T2), and 1min after endotracheal intubation (T3), and the incidence of adverse reactions of hypotension, hypertension, tearing and choking during the induction period. After the patient's muscles relax, the BIS index reached 40-60, the senior anesthesiologists used a visual laryngoscope (Glide Scope Ranger) to perform intubation. If BIS rises by more than 60 and mean arterial blood pressure and heart rate rise by more than 10% during intubation, sedation is performed with propofol 0.5 to 1.0 mg/kg. If systolic blood pressure is reduced by more than 20% during induction, 50 ug phenylephrine would be used each time. If HR is less than 50 times/min, atropine would be given symptomatically. After endotracheal intubation, mechanical ventilation was performed, tidal volume 6 to 8 ml/kg, respiratory rate 12 to 20 breaths/min control PetCO2 35 to 45 mmHg. Anesthesia maintenance was maintained with propofol 4-10 mg/kg/h, remifentanil 15-30 μg/kg/h, sevoflurane 1%-2% inhalation, maintaining the MAC value of 0.7-1.0, adding vecuronium bromide as needed, and maintaining the BIS value at 40-55. Both groups of patients were given prophylactic antiemetic drug tropisetron 2mg intraoperatively. After the operation, all patients were sent to the PACU, and when the patient's spontaneous breathing is restored and consciousness is clear, the Steward score is greater than 6 points, the tracheal tube is removed, the oral secretion is gently sucked, and the patient is instructed to discharge sputum independently, and assist suction if necessary. Observation for at least half an hour, after the patients' vital signs are stabilized, patients are admitted to back to the ward.
Participants
The CONSORT (https://www.goodreports.org/reporting-checklists/consort/) flowchart is shown in the Fig.1. Select patients aged 20-65 years who will undergo non-intracranial elective surgery under general anesthesia in our hospital from March 2022 to March 2023, and have an American Society of Anesthesiologists (ASA) grade I~III (I for healthy patients, II for patients with mild systemic disease, and III for patients with severe systemic disease), BMI 18-28 kg /m2. The types of surgery include breast and thyroid tumor resection, fracture incision reduction internal fixation and laparoscopic hysterectomy. A total of 102 participants were screened. Exclusion criteria: 1) History of psychiatric disorders and endocrine system diseases; 2) Hypersensitivity to opioids or other anesthetics; 3) History of severe heart and lung diseases; 4) Have a history of drug abuse or alcoholism; 5) `Patients at serious risk of increased blood pressure or intracranial pressure; 6) Poorly controlled or untreated hypertensive patients (arterial hypertension, resting systolic/diastolic blood pressure exceeding 180/100 mmHg); 7) Patients with untreated or undertreated hyperthyroidism; 8) Patients with craniotomy during neurosurgery.
Randomization
Eligible participants were randomized to either esketamine or normal sufentanil (control group) using a 1:1 ratio by an online central randomization system. The randomization sequence was based on computer-generated random numbers. Patient clinical management and data collection were sequentially numbered and disclosed by health care practitioners who were not directly involved. Each code was assigned by a random number to one of the two groups: the control group or the esketamine group.
Observation indicators
The main outcome is the variation value in average middle cerebral arterial blood flow velocity after general anesthesia induction. Define the variation of average CBFV from time T0 to T2 as ΔVm1, and define the variation of average CBFV from time T3 to T0 as ΔVm2.
The secondary outcomes include the variation value in average middle cerebral arterial blood flow velocity after endotracheal intubation and the value of Vp, Vm, Vd, SBP, ABP, DBP and HR before induction of general anesthesia (T0), 1 min after the induction drug injected (T1), before endotracheal intubation (T2), and 1min after endotracheal intubation (T3), and the incidence of adverse reactions of hypotension, hypertension, tearing and choking during the induction period.
Sample size calculation
According to the previous pre-experiment, the collected data conformed to the normal distribution, and it was concluded that the change of middle cerebral artery blood flow velocity (ΔVm1 =T0-T2) in the control group was 19.66±14.83 cm/s, and the experimental group was 10.83±5.99 cm/s, using G-power software, when the power was 0.90 and the significance level was 0.05, the required sample size was calculated as 34 per group. After considering potential exclusions, we opted to include 45 patients in each group. In this study, a total of 90 patients were included, and the random number table method was used to divide into 2 groups according to the order of surgery, with 45 cases in each group. A total of 40 patients were finally collected per group.
Statistical analysis
SPSS 26.0 software was used for statistical analysis, measurement data were analyzed and explored, the Shapiro-Wilke test examined the variables, the mean ± standard deviation for those that conformed to the normal distribution was carried out, and the median was carried out if it did not conform to the normal distribution. Independent sample t-test was used for data that conformed to the normal distribution, and independent sample Mann-Whitney U test was used for data that did not conform to normal distribution. Count data are reported as numbers (%), and the χ2 test is used for comparison. P<0.05 is statistically significant.
Results
Baseline Characteristics and Perioperative Data
A total of 102 elective surgery patients were eligibility assessed (Fig. 1), 13 patients were excluded according to exclusion criteria, a total of 89 patients were randomly divided into two groups, 4 patients in the experimental group and 4 patients in the control group did not collect data in time during the induction period, 1 patient in the experimental group lost data during the follow-up process, and finally a total of 80 patients were randomly divided into two groups, the control group (n=40; median [IQR] age 48 [39-56] years) and the experimental group (n=40; median [IQR] age 45 [ 31-53] years) (Table 1). There were no significant differences in gender, age, weight, BMI, and duration of surgery between the two groups. The median consumption of sufentanil in the group E was obviously lower than that in the group C (45[39-50] vs25 [20-34]μg; P<0.001) (Table 1).
Primary Outcome
There was no significant difference in ΔVm1 (13.29[8.49-18.55]cm/s vs 11.90[8.41-16.92] cm/s; P=0.290) and ΔVm2 (0.20±10.45 cm/s vs -2.61±9.16 cm/s; P=0.206) between two groups (Figs. 2 and 3)
Secondary Outcomes
There were no significant differences in SBP, ABP, DBP and HR at the time of T0 between the two groups. Additionally there were no significant differences in SBP, ABP and DBP between the two groups at the time of T1. At the time of T1, the mean HR (SD) in group E was significantly higher than that in group C (74.43±9.66 times/min vs 83.45±11.00 times/min; P<0.001). At the time of T2 and T3,the SBP (98[84-114]mmHg vs 115[101-131]mmHg; P<0.001), ABP (71.59±13.70mmHg vs85.15±14.03mmHg; P<0.001),DBP (58.20±11.17mmHg vs 69.18±12.01mmHg; P<0.001) and HR ( 67[62-79]times/min vs 84[75-89]times/min; P<0.001) in group E were obviously higher than that in group C (Table 2). At the times of T0, T1, T3, there were no significant difference in cerebral blood flow velocity (Vp, Vm, Vd). At the time of T2, the Vp (50.67[42.21-61.26]cm/s vs 59.26[51.30-66.00]cm/s; P =0.016), Vm (32.10[27.46-37.86]cm/s vs 38.37 [33.93-44.27] cm/s; P=0.001), Vd (21.16[18.79-27.23] cm/s vs 28.41[22.92-32.78]cm/s;P<0.001) in group E were obviously higher than that in group C (Table 3).
Adverse reactions
There were no significant abnormalities in the incidence of hypertension, tearing and choking in the two groups. The incidence of hypotension in group E was significantly reduced compared to group C (11 [13.75%] vs 0 [0%]; P<0.001) (Table 4)
Discussion
The main findings of the trial are as follows. Firstly, there was no significant difference on the mean blood flow velocity of middle cerebral artery after administration between the esketamine group and the conventional induction group, and the mean blood flow velocity of the middle cerebral artery in both groups exhibited a reduction prior to endotracheal intubation as compared to pre-induction values, indicating that esketamine combined with propofol induction had no significant advantage over conventional sufentanil combined with propofol induction in maintaining the stability of the average blood flow velocity in the middle cerebral artery. Moreover, the esketamine group did not exhibit an increase in mean blood flow velocity of the middle cerebral artery following endotracheal intubation when compared to the conventional induction group, indicating that esketamine combined with propofol anesthesia did not increase the middle cerebral artery blood flow velocity. Secondly, the results showed that the cerebral blood flow velocity in the esketamine group before endotracheal intubation was significantly higher than that in the control group, while there was no significant difference in ΔVm1, which may be related to the difference in the cerebral blood flow velocity before induction. Although there was no significant difference in cerebral blood flow velocity between the two groups of induction, the study size was small, and the difference in cerebral blood velocity before induction did not necessarily result in a clinically significant difference in cerebral blood velocity between the two groups prior to endotracheal intubation, which deserves further study. Furthermore, the esketamine group had a significant advantage over the conventional induction group in maintaining hemodynamics during the induction process.
General anesthesia is most commonly induced by sedatives, analgesics, and neuromuscular blockers. However, during induction of general anesthesia, the administration of sedatives often causes hypotension, particularly when potent sedatives such as propofol are utilized [10]. Tracheal intubation is an important part of general anesthesia, and opioid-combined propofol is widely used in clinical practice for anesthesia induction to avoid severe stress reactions such as sharp increase in blood pressure and abnormal rapid heart rate [11]. Therefore, the selection of appropriate anesthetic agents to ensure hemodynamic stability during induction is a crucial factor in ensuring surgical safety. At the same time, cerebral blood flow is clearly correlated with peripheral hemodynamics. Cerebral blood flow is related to the cerebral auto-regulation curve, and cerebral blood flow remains relatively stable when the mean arterial pressure is maintained at 50-160mmHg. It was generally believed that hemodynamic stability can maintain relatively stable cerebral blood flow under the automatic regulation mechanism of the brain. Studies have shown that [12] the regulatory mechanisms for maintaining CBF can be broadly divided into brain self-regulation (CA), neurovascular coupling (NVC), and vasomotor responsiveness (VMR). Changes in cerebral blood flow during anesthesia are attributed to the direct vasodilating effect of anesthetics and the partial pressure of carbon dioxide at end-expiration during mechanical ventilation. Cerebral blood flow is pressure passive beyond the autoregulatory range, and there is a risk of ischemic injury to the brain in hypotension, and cerebral edema and disruption of the blood-brain barrier in hypertension [13]. TCCD is considered a valuable tool for investigating cerebral perfusion by measuring the flow velocity of the middle cerebral artery, which plays a crucial role in distributing cerebral blood flow. A significant decrease in middle cerebral artery blood flow can serve as an indicator of overall reduction in cerebral blood flow [14]. Therefore, TCCD was used to monitor the middle cerebral artery blood flow velocity to investigate the effect of esketamine combined with propofol tracheal intubation induction on cerebral blood flow velocity.
Ketamine is an intravenous anesthetic that exhibits favorable sedative and analgesic properties, while also exerting a stimulatory effect on the sympathetic nervous system and circulation. The primary analgesic effect of ketamine is a noncompetitive antagonist to N-methyl-d-aspartate (NMDA) receptor and μ-opioid receptor [15, 16]. It does not inhibit respiratory or myocardial function or hemodynamics [17], so it is more commonly used for induction of anesthesia in special populations. Unlike the increased CBF observed with ketamine monotherapy or S-ketamine anesthesia [9, 18, 19], recent studies have shown that ketamine does not increase intracranial pressure when combined with common anesthetic drugs [20], while further studies suggest that elevated CBF occurs with ketamine alone is caused by direct vasodilation of medium cerebral vessels rather than through secondary effects due to changes in arterial carbon dioxide and/or mean arterial blood pressure [3, 21].
Esketamine, a racemic isomer of ketamine, exhibits fewer adverse effects and shorter sedation periods compared with racemic ketamine [22], for instance produces less psychiatric adverse reactions [23], while demonstrating approximately twice the efficacy of its counterpart [24]. Therefore, the clinical application of esketamine is gradually increasing, and the impact of this on cerebral blood flow remains unclear and warrants further investigation. In this study, we found that the induction of esketamine combined with propofol anesthesia has no significant advantage in maintaining stable cerebral blood flow velocity and does not increase cerebral blood flow velocity during endotracheal intubation, which may be related to the direct relaxation of cerebral blood vessels by propofol [20, 25]. Numerous studies have shown that propofol reduces cerebral glucose metabolism, cerebral oxygen metabolism, and cerebral blood flow [26, 27]. In this study, the negative impact of propofol on cerebral blood flow velocity outweighed the positive effect of esketamine, possibly due to differences in dosage administration for both drugs. The effect of different doses of esketamine combined with propofol anesthesia induction on cerebral blood flow velocity can be further studied.
The primary mechanism by which esketamine maintains hemodynamic stability is through excitation of the sympathetic nervous system, resulting in increased heart rate, blood pressure, and cardiac output. However, peripheral circulatory resistance remains largely unchanged, effectively preserving hemodynamic stability. The use of esketamine during induction of anesthesia increases the perfusion index and mean arterial pressure after induction [28]. In this study, it was also concluded that esketamine combined with propofol induced general anesthesia for endotracheal intubation could maintain hemodynamic stability, and did not increase the incidence of adverse reactions compared with conventional anesthesia induction. This conclusion is the same as most findings [28, 29].
The study had some limitations. Firstly, the trial was conducted in a single centre and further multicentre studies are needed. Secondly, the sample size of the study was small, and there was a certain difference in the basic value of the randomization group, resulting in the loss of clinical significance of some of the results. In addition, biological samples such as blood were not taken, which may help determine the possible mechanisms behind esketamine. Fourth, the main indicator of the study is only the cerebral blood flow rate, and the effect of esketamine on intracranial pressure, cerebral oxygen metabolism, and cerebral glucose metabolism needs to be further studied. Finally, in terms of the opposite effects of esketamine and propofol on cerebral blood flow, further titrations of the dose of the two need to be explored to find a more appropriate dosage.
Conclusion
This randomized controlled trial showed that esketamine combined with propofol for induction of endotracheal intubation general anesthesia does not have significant advantages in maintaining cerebral blood flow velocity, and does not cause an increase in cerebral blood flow velocity, which can be safely used for endotracheal intubation anesthesia induction and provides more evidence for the further application of esketamine in neurosurgery. Moreover, esketamine does maintain hemodynamic stability during induction. Further studies with larger sample sizes are needed to confirm the effect of eketamine on the rate of blood flow to the brain.
Availability of data and maerials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- CBFV:
-
Cerebral blood flow velocities
- BP:
-
Blood pressure
- HR:
-
Heart rate
- ICP:
-
Intracranial pressure
- SpO2 :
-
Oxygen saturation
- ECG:
-
Electrocardiogram
- MCA:
-
Middle cerebral artery
- Vp :
-
Systolic middle cerebral artery blood flow velocity
- Vm :
-
Average middle cerebral artery blood flow velocity
- Vd :
-
Diastolic middle cerebral artery blood flow velocity
- SBP:
-
Systolic blood pressure
- ABP:
-
Average blood pressure
- DBP:
-
Diastolic blood pressure
- BIS:
-
Bispectral
- MAC:
-
Minimum alveolar concentration
- PACU:
-
Post-anesthesia care unit
- ASA:
-
American society of anesthesiologists
- BMI:
-
Body mass index
- CA:
-
Brain self-regulation
- NVC:
-
Neurovascular coupling
- VMR:
-
Vasomotor responsiveness
- NMDA:
-
N-methyl-d-aspartate
References
La Via L, Sanfilippo F, Cuttone G, Dezio V, Falcone M, Brancati S, Crimi C, Astuto M. Use of ketamine in patients with refractory severe asthma exacerbations: systematic review of prospective studies. Eur J Clin Pharmacol. 2022;78(10):1613–22.
Schatzberg AF. A word to the wise about ketamine. Am J Psychiatry. 2014;171(3):262–4.
Strebel S, Kaufmann M, Schaefer HG. Effects of ketamine on cerebral blood flow velocity in humans. Influence of pretreatment with midazolam or esmolo. Anaesthesia. 1995;50(3):223–8.
Gregers M, Mikkelsen S, Lindvig KP, Brochner AC. Ketamine as an anesthetic for patients with acute brain injury: a systematic review. Neurocrit Care. 2020;33(1):273–82.
Tan Y, Hashimoto K. Risk of psychosis after repeated intermittent administration of (s)-ketamine, but not (r)-ketamine, in mice. J Affect Disord. 2020;269:198–200.
Sakai K, Cho S, Fukusaki M, Shibata O, Sumikawa K. The effects of propofol with and without ketamine on human cerebral blood flow velocity and CO2 response. Anesth Analg. 2000;90(2):377–82.
Lu Y, Ding X, Wu X, Huang S. Ketamine inhibits lps-mediated bv2 microglial inflammation via NMDA receptor blockage. Fundam Clin Pharmacol. 2020;34(2):229–37.
Wang L, Deng B, Yan P, Wu H, Li C, Zhu H, Du J, Hou L. Neuroprotective effect of ketamine against TNF-alpha-induced necroptosis in hippocampal neurons. J Cell Mol Med. 2021;25(7):3449–59.
Langsjo JW, Maksimow A, Salmi E, Kaisti K, Aalto S, Oikonen V, Hinkka S, Aantaa R, Sipila H, Viljanen T, Parkkola R, Scheinin H. S-ketamine anesthesia increases cerebral blood flow in excess of the metabolic needs in humans. Anesthesiology. 2005;103(2):258–68.
Poterman M, Scheeren T, van der Velde MI, Buisman PL, Allaert S, Struys M, Kalmar AF. Prophylactic atropine administration attenuates the negative haemodynamic effects of induction of anaesthesia with propofol and high-dose remifentanil: a randomised controlled trial. Eur J Anaesthesiol. 2017;34(10):695–701.
Sridharan K, Sivaramakrishnan G. Comparison of fentanyl, remifentanil, sufentanil and alfentanil in combination with propofol for general anesthesia: a systematic review and meta-analysis of randomized controlled trials. Curr Clin Pharmacol. 2019;14(2):116–24.
Usui A, Hotta T, Hiroura M, Murase M, Maeda M, Koyama T, Tanaka M, Takeuchi E, Abe T. Cerebral metabolism and function during normothermic retrograde cerebral perfusion. Cardiovasc Surg. 1993;1(2):107–12.
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H. Cerebral autoregulation dynamics in humans. Stroke. 1989;20(1):45–52.
Sorteberg W, Lindegaard KF, Rootwelt K, Dahl A, Russell D, Nyberg-Hansen R, Nornes H. Blood velocity and regional blood flow in defined cerebral artery systems. Acta Neurochir (Wien). 1989;97(1–2):47–52.
Dong TT, Mellin-Olsen J, Gelb AW. Ketamine: a growing global health-care need. Br J Anaesth. 2015;115(4):491–3.
Bonaventura J, Lam S, Carlton M, Boehm MA, Gomez JL, Solis O, Sanchez-Soto M, Morris PJ, Fredriksson I, Thomas CJ, Sibley DR, Shaham Y, Zarate CA Jr, Michaelides M. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;26(11):6704–22.
Eikermann M, Grosse-Sundrup M, Zaremba S, Henry ME, Bittner EA, Hoffmann U, Chamberlin NL. Ketamine activates breathing and abolishes the coupling between loss of consciousness and upper airway dilator muscle dysfunction. Anesthesiology. 2012;116(1):35–46.
Langsjo JW, Kaisti KK, Aalto S, Hinkka S, Aantaa R, Oikonen V, Sipila H, Kurki T, Silvanto M, Scheinin H. Effects of subanesthetic doses of ketamine on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology. 2003;99(3):614–23.
Langsjo JW, Salmi E, Kaisti KK, Aalto S, Hinkka S, Aantaa R, Oikonen V, Viljanen T, Kurki T, Silvanto M, Scheinin H. Effects of subanesthetic ketamine on regional cerebral glucose metabolism in humans. Anesthesiology. 2004;100(5):1065–71.
Schlunzen L, Juul N, Hansen KV, Cold GE. Regional cerebral blood flow and glucose metabolism during propofol anaesthesia in healthy subjects studied with positron emission tomography. Acta Anaesthesiol Scand. 2012;56(2):248–55.
Zeiler FA, Sader N, Gillman LM, Teitelbaum J, West M, Kazina CJ. The cerebrovascular response to ketamine: a systematic review of the animal and human literature. J Neurosurg Anesthesiol. 2016;28(2):123–40.
Marland S, Ellerton J, Andolfatto G, Strapazzon G, Thomassen O, Brandner B, Weatherall A, Paal P. Ketamine: use in anesthesia. Cns Neurosci Ther. 2013;19(6):381–9.
Molero P, Ramos-Quiroga JA, Martin-Santos R, Calvo-Sanchez E, Gutierrez-Rojas L, Meana JJ. Antidepressant efficacy and tolerability of ketamine and esketamine: a critical review. Cns Drugs. 2018;32(5):411–20.
Arendt-Nielsen L, Nielsen J, Petersen-Felix S, Schnider TW, Zbinden AM. Effect of racemic mixture and the (s+)-isomer of ketamine on temporal and spatial summation of pain. Br J Anaesth. 1996;77(5):625–31.
Kaisti KK, Langsjo JW, Aalto S, Oikonen V, Sipila H, Teras M, Hinkka S, Metsahonkala L, Scheinin H. Effects of sevoflurane, propofol, and adjunct nitrous oxide on regional cerebral blood flow, oxygen consumption, and blood volume in humans. Anesthesiology. 2003;99(3):603–13.
Qiu M, Scheinost D, Ramani R, Constable RT. Multi-modal analysis of functional connectivity and cerebral blood flow reveals shared and unique effects of propofol in large-scale brain networks. Neuroimage. 2017;148:130–40.
Laaksonen L, Kallioinen M, Langsjo J, Laitio T, Scheinin A, Scheinin J, Kaisti K, Maksimow A, Kallionpaa RE, Rajala V, Johansson J, Kantonen O, Nyman M, Siren S, Valli K, Revonsuo A, Solin O, Vahlberg T, Alkire M, Scheinin H. Comparative effects of dexmedetomidine, propofol, sevoflurane, and s-ketamine on regional cerebral glucose metabolism in humans: a positron emission tomography study. Br J Anaesth. 2018;121(1):281–90.
Zhou N, Liang X, Gong J, Li H, Liu W, Zhou S, Xiang W, Li Z, Huang Y, Mo X, Li W. S-ketamine used during anesthesia induction increases the perfusion index and mean arterial pressure after induction: a randomized, double-blind, placebo-controlled trial. Eur J Pharm Sci. 2022;179: 106312.
Li J, Wang Z, Wang A, Wang Z. Clinical effects of low-dose esketamine for anaesthesia induction in the elderly: a randomized controlled trial. J Clin Pharm Ther. 2022;47(6):759–66.
Acknowledgements
We thank Xuelian Yang, Lu Zhang, and Shuhan Cheng for their help with their expertise.
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by SY , KH and QL. The first draft of the manuscript was written by SY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of The First Affiliated Hospital of Chongqing Medical University (NO:2020-072, 23/03/2022), written informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yan, S., Li, Q. & He, K. The effect of esketamine combined with propofol-induced general anesthesia on cerebral blood flow velocity: a randomized clinical trial. BMC Anesthesiol 24, 66 (2024). https://doi.org/10.1186/s12871-024-02446-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-024-02446-4