Abstract
Background
Transversus abdominis plane (TAP) block has been utilized to alleviate pain following laparoscopic cholecystectomy (LC). However, the optimal timing of administration remains uncertain. This study aimed to compare the efficacy of pre-operative and postoperative TAP blocks as analgesic options after LC.
Methods
A frequentist network meta-analysis of randomized controlled trials (RCTs) was conducted. We systematically searched PubMed (via the National Library of Medicine), EMBASE, Scopus, Cochrane Central Register of Controlled Trials (CENTRAL), and Web of Science up to March 2023. The study included RCTs that enrolled adult patients (≥ 18 years) who underwent LC and received either pre-operative or postoperative TAP blocks. The primary outcome assessed was 24-hour postoperative morphine consumption (mg). Additionally, pain rest scores within 3 hours, 12 hours, and 24 hours, as well as postoperative nausea and vomiting (PONV), were considered as pre-specified secondary outcomes.
Results
A total of 34 trials with 2317 patients were included in the analysis. Postoperative TAP block demonstrated superiority over the pre-operative TAP block in reducing opioid consumption (MD 2.02, 95% CI 0.87 to 3.18, I2 98.6%, p < 0.001). However, with regards to postoperative pain, neither pre-operative nor postoperative TAP blocks exhibited superiority over each other at any of the assessed time points. The postoperative TAP block consistently ranked as the best intervention using SUCRA analysis. Moreover, the postoperative TAP block led to the most significant reduction in PONV.
Conclusions
The findings suggest that the postoperative TAP block may be slightly more effective in reducing 24-hour postoperative opioid consumption and PONV when compared to the pre-operative TAP block.
Trial registration
PROSPERO, CRD42023396880.
Similar content being viewed by others
Introduction
Laparoscopic cholecystectomy (LC) is considered a minimally invasive surgical procedure compared to traditional open cholecystectomy [1, 2]. However, although less severe in LC, procedure-related pain remains a problem that needs to be addressed by clinicians [1, 3]. Pharmacological treatments, such as nonsteroidal anti-inflammatory drugs and opioids, are frequently used in pain management in LC [4, 5]. Also, loco-regional anesthesia techniques, such as port site infiltration and fascial plane blocks, can improve the quality of pain management [3]. The transversus abdominis plane (TAP) block is one of the first fascial plane blocks for pain management after various surgical procedures, including laparoscopic surgeries.
The TAP block aims to provide sensory blockage of the anterior abdominal wall and generally does not affect visceral pain [6, 7]. Numerous studies have been published on the peri-operative analgesic efficacy of TAP block types (because there is more than one approach) in LC [8,9,10]. In many studies on regional anesthesia, the aim was to measure the effectiveness of the blocks. In these studies, measurements are usually set up as parameters such as opioid requirement, pain scores, and healing quality scores at a specific time interval [7]. However, the parameters affecting the results of a study are not limited to block characteristics, such as block type, local anaesthetic volume, and concentration. Comparisons are generally made between the control and experimental groups or between more than one experimental group.
Another critical factor is whether the applied regional anesthesia technique is performed before or after the surgical procedure, i.e., whether it provides pre-emptive/preventive analgesia. The common goal in pre-emptive analgesia applications such as pre-operative TAP block is to reduce the intensity and duration of postoperative pain by preventing central sensitization and reducing peripheral nociceptive input [11]. Based on the data revealing that the application of regional anesthesia to be performed early reduces the immune response to perioperative trauma, debates about whether to apply a pre- or postsurgical block are still ongoing [12, 13].
Therefore, we conducted a meta-analysis of previously published randomised controlled trials to compare the effects of pre-operative and postoperative TAP blocks in LC. Our hypothesis was that a pre-operative TAP block would reduce morphine consumption by providing pre-emptive analgesia and allowing more time for LA to diffuse in the fascial plane.
Methods
Eligibility criteria, literature search, and study selection
This systematic review and meta-analysis followed the steps outlined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [14]. We followed the PRISMA extension statement for reporting systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations [15]. The Cochrane Handbook for Systematic Reviews of Intervention was chosen as the methodological guidance [16]. The protocol was registered prospectively in PROSPERO (CRD42023396880). We defined inclusion criteria using the PICOS acronym items: adult patients (≥ 18 years) who underwent LC (P) who received pre-operative or postoperative ultrasound guided TAP blocks including all approaches reported in the literature for TAP block [17] (I) compared to placebo or no intervention (C). Our primary outcome was 24-hour postoperative morphine consumption (mg). For all papers expressing the cumulative postoperative opioid dose with a drug other than morphine, we converted the amount following the equi-analgesic tables using the GlobalRPh morphine equivalent calculator, considering a 0% cross-tolerance modifier (http://www.globalrph.com/narcotic). Our pre-specified secondary outcomes were pain rest scores within 3 hours and at 12 and 24 hours expressed through the visual analogue scale (VAS) or numerical rating scale (NRS), and postoperative nausea and vomiting (PONV), defined as a self-reported outcome in the first 24 postoperative hours (O) [18]. We decided to include only RCTs (S). Regarding the TAP block timing we defined pre-operative block as a TAP block performed before the surgical incision. All blocks performed after surgical incisions were defined as postoperative blocks. We did not exclude studies based on the type of local anaesthetic and volume injected.
We performed an electronic search of PubMed (via the National Library of Medicine), EMBASE, Scopus, Cochrane Central Register of Controlled Trials (CENTRAL), and Web of Science from database inception to 8 March 2023 using a predefined search strategy (Supplementary Document 1). The research strategy was decided and approved in advance by regional anesthesia experts. Language restrictions were not imposed. In this review, two reviewers (Y.E.K. and M.B.) independently identified and assessed studies to determine if they were eligible, and a third reviewer settled any disagreements that arose (B.D.). Two authors extracted data and evaluated the potential for bias separately (F.G. and A.D.C.).
Data extraction and risk-of-Bias assessment
Data for this systematic review were extracted using an Excel (Microsoft, Redmond, WA, USA) spreadsheet that had been specifically prepared for this purpose. Data regarding the procedure, including the year of publication, the patient’s age, the patient’s American Society of Anaesthesiologists (ASA) physical status score, the type local anaesthetic used, the injection volume, the amount of local anaesthetic used, and the TAP block technique, used was collected. Two researchers used the Risk of Bias (RoB) 2 instrument to assess the reliability of the included RCTs [16]. Randomization, allocation concealment, blinding of outcome assessment, data completeness, and selective outcome reporting were used to assign each study a risk of bias grade of either low, high, or with some concerns. The certainty and quality of the evidence for each outcome was assessed using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology [19]. To check for publication bias, we generated funnel plots, and we intended to conduct additional statistical analysis of funnel plot asymmetry if more than 10 trials were evaluated for each outcome [16]. Evaluations of homogeneity, consistency, and intransitivity are given in the section on statistics that follows.
Statistical analysis
Data meta-analysis was conducted using the R package “netmeta” in R version 4.1 (R Foundation for Statistical Computing, Vienna, Austria). We used the χ2 test and the I2-statistic (classifying I2 values as low (25%), moderate (25–50%), or high (> 50%) to evaluate the degree of heterogeneity within the studies [19]. We used mean differences (MDs) with 95% confidence intervals (CIs) to describe the treatment’s impact on continuous variables. For binary outcomes, we report the effect as an odds ratio (OR) with 95% CI.
We ranked all treatments in terms of their ability to reduce 24-hour morphine consumption, from 0 to 1, using the surface under cumulative ranking (SUCRA) curve [20]. A higher SUCRA (values closer to 1) suggests that a given treatment is more likely to be optimal for the outcome of interest. We were able to rank the treatments by comparing the SUCRA values that were calculated for each. Whenever possible, we used the Hozo method to transform the reported median and interquartile range into an estimated mean and standard deviation (SD) [21]. When different doses of local anaesthetic were used in the same study for the same block, the means and standard deviations were pooled.
Cochrane’s Q test was used to assess the degree of heterogeneity within and between studies. Despite the inconsistency and heterogeneity, a random-effects model was chosen. We inspected funnel plots visually and used the Egger test (p 0.05, indicating possible publication bias) to assess publication bias (Supplementary Document 2). All statistical significance testing was 2-tailed; a p value of < 0.05 was considered statistically significant.
Results
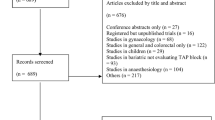
The search results are presented in the PRISMA flow diagram (Fig. 1). Initial screening identified 995 studies. Of these, 82 search results were excluded during the preliminary screening because they were duplicates, and 879 were excluded because they were unrelated to the topic. The full texts were retrieved from the remaining 34 articles, and five more studies were excluded according to our inclusion and exclusion criteria. Five additional studies were identified by screening the references of the included articles. A total of 34 studies were included in the quantitative analysis [11, 22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]. Table 1 summarises the pooled characteristics of the included studies.
In total, 22 of the included studies compared pre-operative TAP block with a control [22, 23, 25, 27,28,29, 31, 33, 35,36,37,38,39,40,41,42,43, 45, 46, 49, 52, 54], 11 evaluated the effect of postoperative TAP block compared with a control block [24, 26, 30, 32, 34, 44, 47, 48, 50, 51, 53], and only one directly compared pre-operative TAP block with postoperative TAP block [11]. A total of 2317 patients were enrolled in the included trials: 456 patients were randomised to the postoperative TAP block group, 773 to the pre-operative TAP block group, and the remaining to the control group. According to the risk of bias assessment, eight studies had a low risk of bias and three had a high risk. The 23 studies raised some concerns (Fig. 2). The criteria we used to assign the risk of bias judgments can be found in Supplementary Document 3.
Outcomes
Most evidence arises from indirect comparisons, given that only one trial directly compared pre-operative and postoperative TAP blocks. While the cumulative effects of direct and indirect evidence are shown in the following section, the contribution of direct evidence for each comparison is shown in in Supplementary Document 4.
Publication Bias
There was evidence of publication bias only for PONV outcomes (Egger’s test, p = 0.015). All funnel plots are shown in Supplementary Document 2.
Main outcome: postoperative opioid consumption at 24 hours
Postoperative opioid consumption was evaluated in 25 studies. A graphical representation of the network is shown in Fig. 3. Both postoperative and pre-operative TAP blocks resulted in a better reduction in opioid consumption at 24 h than the control (Table 2). However, the postoperative TAP block was superior to the pre-operative TAP block (MD 2.02, 95% CI 0.87. to 3.18, I2 98.6%, p < 0.001) (Table 2). Using the GRADE assessment, we rated the quality of evidence as low, given both the high statistical heterogeneity and the major contribution of indirect evidence to the results.
Postoperative pain
Pain in the first 3 hours was evaluated in 28 studies. Meanwhile, it was reported in 21 and 26 studies at 12 and 24 postoperative hours, respectively. Both techniques were superior to the control in providing better pain control at all times (Table 2). However, neither pre-operative nor postoperative TAP blocks were superior to each other at any of the considered time points (Table 2). A comprehensive summary of the results for this outcome are depicted in Fig.4. The postoperative TAP block was always ranked as the best intervention using SUCRA (Table 3). Using the GRADE assessment, we rated the quality of evidence as low, given both the high statistical heterogeneity and the major contribution of indirect evidence to the results.
PONV
PONV was evaluated in 21 studies. The highest reduction in PONV was obtained with the postoperative TAP block (Table 2). Using the GRADE assessment, we rated the quality of evidence as low, given the major contribution of indirect evidence to the results, moderate statistical heterogeneity (I2 = 37.8%), and possible publication bias.
Discussion
This systematic review and meta-analysis evaluated the analgesic effects of pre-operative and postoperative TAP blocks in patients undergoing LC. Based on 34 randomised controlled trials, we found that postoperative TAP block reduced postoperative 24-hour opioid consumption and PONV compared to pre-operative TAP block. The VAS scores were similar in the two groups.
Pain following laparoscopy has somatic, visceral, and referral components. Somatic pain arises from skin incisions during surgical port insertion, stretching of the abdominal wall due to CO2 insufflation, and surgical stimulation of the parietal peritoneum. It travels across the thoracolumbar spinal nerves (T6-L1), leading to sharp and well-localised pain rather than dull pain. In contrast, tissue traction, compression, or surgical dissection of the abdominal organs causes diffuse and dull visceral pain [1, 55]. This latter noxious impulse is transmitted by autonomic nerves (T5–9, greater splanchnic nerve, celiac ganglion, and vagus) [56, 57]. Furthermore, pneumoperitoneum and gallbladder stimulation may cause diaphragm inflammation, activating the phrenic nerve (C3–5) and causing referred shoulder pain [55]. The most significant component, in this case, is somatic pain [1].
As a component of multimodal therapy, TAP block guarantees somatic analgesia in the anterolateral abdominal wall by blocking the anterior branches of the thoracolumbar spinal nerves at different levels (T6-L1) [17]. Two meta-analyses compared TAP block to local anaesthetic wound infiltration or the control group, proving superior 24-hour postoperative analgesia [6, 58]. Pre-emptive analgesia blocks the noxious stimuli before they arise. Therefore, it is thought to be more effective than postoperative analgesia in preventing central sensitisation and incisional and inflammatory damage [59]. Therefore, we hypothesised that a pre-operative TAP block would reduce morphine consumption by providing pre-emptive analgesia and allowing more time for LA to diffuse in the fascial plane. Our results contradict these findings. A possible explanation for this discrepancy in the results could be that we included four approaches of TAP blocks, leading to different dermatomal coverages (subcostal, T6–9; lateral, T10–12; posterior, T9–12; and oblique-subcostal approach, T6-L1) [17]. Different dermatomal distributions ‘according to different approach of TAP block such as subcostal, lateral, and posterior’ among the studies may have inadvertently introduced variability in the degree of analgesia provided to the included study participants. This variability in dermatomal coverage could have directly influenced post-operative pain perception and, consequently, morphine consumption.
The optimum timing for performing a TAP block is still debated in the literature. A previous meta-analysis compared the analgesic effects of pre-operative and postoperative TAP blocks on postoperative pain in patients undergoing laparoscopic surgery [60]. The analysis found that pre-operative blocks reduced postoperative pain scores. In contrast, a retrospective study showed that 20 mL of 0.25% plain bupivacaine used for postoperative and pre-operative TAP block had a slightly similar effectiveness in reducing intravenous opioid consumption in the postoperative period. In patients that underwent postoperative TAP block, there was a decreased use of patient controlled analgesia (PCA) but a higher amount of morphine consumption. There was no difference between the groups regarding the duration of PCA or intravenous and oral opioid use [61]. In the same study, Kalu et al. proved better long-term outcomes (opioid prescribed at the discharge and amount of opioid) in the postoperative TAP group.
This network meta-analysis suggests that performing the block in the postoperative period may reduce 24-hour postoperative opioid consumption and PONV and may be slightly superior in terms of postoperative pain scores. Most of the evidence collected in this meta-analysis was indirect. However, a randomised controlled study comparing the timing of the block on postoperative outcomes found that performing a TAP block in the postoperative period significantly decreased postoperative opioid consumption, PONV, and pain scores at rest and during coughing [11]. Multimodal analgesia often relies heavily on opioids, which carry the risk of adverse effects, including nausea, constipation, respiratory depression, and the potential for addiction. In contrast, opioid-sparing analgesia techniques, such as the utilization of TAP blocks, aim to minimize opioid consumption while effectively controlling pain, reducing opioid-related side effects, and expediting postoperative recovery. By reducing opioid usage, patients experience improved pain control, faster return of bowel function, decreased length of hospital stay, and a quicker return to their normal daily activities [8].
Although there is still no agreement to define a clinically significant power of intervention [62], the overall reduction in opioid consumption found in this network meta-analysis was modest (− 2.23 mg), suggesting a small effect. However, considering the concomitant reduction in opioid-related PONV and postoperative pain scores, performing postoperative TAP block may be beneficial. Further studies are needed to confirm our findings, given the relatively low quality of evidence.
In addition, a TAP block requires a high-volume injection in a relatively highly vascularised area. After administration, peak plasma concentrations of ropivacaine and lidocaine were reached at the 30th and 15th minutes, respectively [63, 64]. Considering that the most intense pain occurs in the early postoperative hours, it may be more reasonable to perform a TAP block postoperatively.
Recent clinical findings suggest that the duration of a single shot TAP block can exceed 12 hours, with benefits reported up to 24–48 hours postoperatively for the posterior approach [65]. However, Støving et al. [66] reported in healthy volunteers a high variability effect of the block in terms of cutaneous sensory block area and block duration, which did not exceed 10 hours. In a pharmacokinetic study conducted by Trabelsi et al. [67] the mean elimination half-life of bupivacaine was 8.75 hours after the block. This result suggests a potentially decremental effect over 24 hours related to the metabolism and clearance of the local anaesthetic. The fact that the postoperative TAP block was closer to the assessment of outcomes and the peak of postoperative pain may partially explain its greater effectiveness.
Our meta-analysis is subject to several limitations; thus, caution should be exercised when interpreting our results. Firstly, there was considerable variation in the concentration, dose, and type of local anaesthetic used across the different TAP blocks included in the studies. Secondly, we encompassed all types of TAP blocks, which could introduce heterogeneity and impact the overall findings. Thirdly, the majority of the reported evidence is based on indirect comparisons, as only one study provided a direct comparison. Fourthly, it is important to acknowledge that data pertaining to block performance time and block dermatomal assessment were not available in the included studies. The absence of perioperative data in many of the studies may have influenced the quality of our analysis [68, 69]. Lastly, we observed significant heterogeneity in our analysis, which may affect the reliability and generalizability of the results.
Conclusions
This systematic review and meta-analysis demonstrates that both pre-operative and postoperative TAP blocks are effective in reducing postoperative opioid consumption and pain scores. The postoperative TAP block appears to have a slight superiority and effectiveness in reducing 24-hour postoperative opioid consumption and PONV. However, it is essential to note that a high level of heterogeneity in the results may limit the robustness of our findings. Therefore, future studies on this topic will be of paramount importance to further validate and strengthen these results.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- TAP:
-
Transversus Abdominis Plane
- LC:
-
Laparoscopic cholecystectomy
- RCT:
-
Randomized Controlled Trial
- PONV:
-
Postoperative Nausea And Vomiting
- SUCRA:
-
Surface Under The Cumulative Ranking Curve
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PICOS:
-
Population, Intervention, Comparison, Outcomes and Study
- PCA:
-
Patient Controlled Analgesia
References
Bisgaard T, Klarskov B, Rosenberg J, Kehlet H. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. 2001;90(3):261–9.
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Meta-analysis of laparoscopic vs open cholecystectomy in elderly patients. World J Gastroenterol. 2014;20(46):17626–34.
Ramkiran S, Jacob M, Honwad M, Vivekanand D, Krishnakumar M, Patrikar S. Ultrasound-guided combined fascial plane blocks as an intervention for pain management after laparoscopic cholecystectomy: a randomized control study. Anesth Essays Res. 2018;12(1):16–23.
Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg. 2000;87(3):273–84.
Eftekhariyazdi M, Ansari M, Darvishi-Khezri H, Zardosht R. Pharmacological methods of postoperative pain management after laparoscopic cholecystectomy: a review of Meta-analyses. Surg Laparosc Endosc Percutan Tech. 2020;30(6):534–41.
Grape S, Kirkham KR, Akiki L, Albrecht E. Transversus abdominis plane block versus local anesthetic wound infiltration for optimal analgesia after laparoscopic cholecystectomy: a systematic review and meta-analysis with trial sequential analysis. J Clin Anesth. 2021;75:110450.
De Cassai A, Sella N, Geraldini F, Tulgar S, Ahiskalioglu A, Dost B, et al. Single-shot regional anesthesia for laparoscopic cholecystectomies: a systematic review and network meta-analysis. Korean J Anesthesiol. 2023;76(1):34–46.
Alsharari AF, Abuadas FH, Alnassrallah YS, Salihu D. Transversus abdominis plane block as a strategy for effective pain Management in Patients with pain during laparoscopic cholecystectomy: a systematic review. J Clin Med. 2022;11(23):6896.
Wang W, Wang L, Gao Y. A Meta-analysis of randomized controlled trials concerning the efficacy of Transversus abdominis plane block for pain control after laparoscopic cholecystectomy. Front Surg. 2021;8:700318.
Barazanchi AWH, MacFater WS, Rahiri JL, Tutone S, Hill AG, Joshi GP. Evidence-based management of pain after laparoscopic cholecystectomy: a PROSPECT review update. Br J Anaesth. 2018;121(4):787–803.
Rahimzadeh P, Faiz SHR, Latifi-Naibin K, Alimian M. A comparison of effect of preemptive versus postoperative use of ultrasound-guided bilateral transversus abdominis plane (TAP) block on pain relief after laparoscopic cholecystectomy. Sci Rep. 2022;12(1):623.
Bloc S, Perot BP, Gibert H, Law Koune JD, Burg Y, Leclerc D, et al. Efficacy of parasternal block to decrease intraoperative opioid use in coronary artery bypass surgery via sternotomy: a randomized controlled trial. Reg Anesth Pain Med. 2021;46(8):671–8.
Kim SC, Anwar S. Response to 'Efficacy of parasternal block to decrease intraoperative opioid use in coronary artery bypass surgery via sternotomy: a randomized controlled trial' by Bloc et al. Reg Anesth Pain Med. 2022;47:587–8.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Higgins JPTTJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). Cochrane; 2022.
Tsai HC, Yoshida T, Chuang TY, Yang SF, Chang CC, Yao HY, et al. Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:8284363.
Postoperative nausea and vomiting. https://www.uptodate.com/contents/postoperative-nausea-and-vomiting. Accessed 20 July 2023.
Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. A GRADE working group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630.
Rücker G, Schwarzer G. Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol. 2015;15(1):58.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13.
Arık E, Akkaya T, Ozciftci S, Alptekin A, Balas Ş. Unilateral transversus abdominis plane block and port-site infiltration : comparison of postoperative analgesic efficacy in laparoscopic cholecystectomy. Anaesthesist. 2020;69(4):270–6.
Dost B, Yalçın Sezen G, İskender A, Özlü O. A comparison of transversus abdominis plane block guided with ultrasonography and local anesthetic infiltration in laparoscopic cholecystectomy operations. Agri. 2018;30(2):51–7.
Bhatia N, Arora S, Jyotsna W, Kaur G. Comparison of posterior and subcostal approaches to ultrasound-guided transverse abdominis plane block for postoperative analgesia in laparoscopic cholecystectomy. J Clin Anesth. 2014;26(4):294–9.
Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012;37(2):188–92.
Suseela I, Anandan K, Aravind A, Kaniyil S. Comparison of ultrasound-guided bilateral subcostal transversus abdominis plane block and port-site infiltration with bupivacaine in laparoscopic cholecystectomy. Indian J Anaesth. 2018;62(7):497–501.
Vrsajkov V, Mančić N, Mihajlović D, Milićević ST, Uvelin A, Vrsajkov JP. O bloqueio do plano transverso abdominal subcostal pode melhorar a analgesia após colecistectomia laparoscópica. Braz J Anesthesiol. 2018;68(2):149–53.
Karl Nicholas SA, Ribeiro JCM, Eapen A, Naik SA. Ultrasound guided oblique subcostal transverse abdominis plane block using local Anaesthetic versus saline for laparoscopic cholecystectomies: a randomised controlled trial. J Clin Diagn Res. 2019;13(1):UC07–10.
Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58(4):362–8.
Dai L, Ling X, Qian Y. Effect of ultrasound-guided Transversus abdominis plane block combined with patient-controlled intravenous analgesia on postoperative analgesia after laparoscopic cholecystectomy: a double-blind, randomized controlled trial. J Gastrointest Surg. 2022;26(12):2542–50.
Al-Refaey K, Usama EM, Al-Hefnawey E. Adding magnesium sulfate to bupivacaine in transversus abdominis plane block for laparoscopic cholecystectomy: a single blinded randomized controlled trial. Saudi J Anaesth. 2016;10(2):187–91.
Lee SY, Ryu CG, Koo YH, Cho H, Jung H, Park YH, et al. The effect of ultrasound-guided transversus abdominis plane block on pulmonary function in patients undergoing laparoscopic cholecystectomy: a prospective randomized study. Surg Endosc. 2022;36(10):7334–42.
Jung J, Jung W, Ko EY, Chung YH, Koo BS, Chung JC, et al. Impact of bilateral subcostal plus lateral Transversus abdominis plane block on quality of recovery after laparoscopic cholecystectomy: a randomized placebo-controlled trial. Anesth Analg. 2021;133(6):1624–32.
Baral B, Poudel PR. Comparison of analgesic efficacy of ultrasound guided subcostal Transversus abdominis plane block with port site infiltration following laparoscopic cholecystectomy. J Nepal Health Res Counc. 2019;16(41):457–61.
Basaran B, Basaran A, Kozanhan B, Kasdogan E, Eryilmaz MA, Ozmen S. Analgesia and respiratory function after laparoscopic cholecystectomy in patients receiving ultrasound-guided bilateral oblique subcostal transversus abdominis plane block: a randomized double-blind study. Med Sci Monit. 2015;21:1304–12.
El-Dawlatly AA, Turkistani A, Kettner SC, Machata AM, Delvi MB, Thallaj A, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth. 2009;102(6):763–7.
Petersen PL, Stjernholm P, Kristiansen VB, Torup H, Hansen EG, Mitchell AU, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg. 2012;115(3):527–33.
Houben AM, Moreau AJ, Detry OM, Kaba A, Joris JL. Bilateral subcostal transversus abdominis plane block does not improve the postoperative analgesia provided by multimodal analgesia after laparoscopic cholecystectomy: a randomised placebo-controlled trial. Eur J Anaesthesiol. 2019;36(10):772–7.
Liang M, Chen Y, Zhu W, Zhou D. Efficacy and safety of different doses of ropivacaine for laparoscopy-assisted infiltration analgesia in patients undergoing laparoscopic cholecystectomy: a prospective randomized control trial. Medicine (Baltimore). 2020;99(46):e22540.
Shin HJ, Oh AY, Baik JS, Kim JH, Han SH, Hwang JW. Ultrasound-guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy: a randomized, controlled, observer-blinded study. Minerva Anestesiol. 2014;80(2):185–93.
Breazu C, Margarit S, Bartos A, Ionescu D. Postoperative analgesia after laparoscopic cholecystectomy - prospective, randomized, double blind, control trial. Chirurgia. 2022;117(5):563–71.
Dilek Andıç K, Nadir AH, Lafci A, Gogus N. Evaluation of the effects of ultrasound-guided Transversus abdominis plane block on perioperative analgesia and patient comfort in patients undergoing laparoscopic cholecystectomy. JARSS. 2021;29(2):112–8.
Chen CK, Tan PC, Phui VE, Teo SC. A comparison of analgesic efficacy between oblique subcostal transversus abdominis plane block and intravenous morphine for laparascopic cholecystectomy. A prospective randomized controlled trial. Korean J Anesthesiol. 2013;64(6):511–6.
Tolchard S, Davies R, Martindale S. Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol. 2012;28(3):339–43.
Breazu CM, Ciobanu L, Hadade A, Bartos A, Mitre C, Mircea PA, et al. The efficacy of oblique subcostal transversus abdominis plane block in laparoscopic cholecystectomy - a prospective, placebo controlled study. Rom J Anaesth Intensive Care. 2016;23(1):12–8.
Huang SH, Lu J, Gan HY, Li Y, Peng YG, Wang SK. Perineural dexamethasone does not enhance the analgesic efficacy of ultrasound-guided subcostal transversus abdominis plane block during laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int. 2016;15(5):540–5.
Saliminia A, Azimaraghi O, Babayipour S, Ardavan K, Movafegh A. Efficacy of transverse abdominis plane block in reduction of postoperation pain in laparoscopic cholecystectomy. Acta Anaesthesiol Taiwanica. 2015;53(4):119–22.
Ali L, Waseem M, Iqbal A. Comparison of analgesic efficacy of transversus abdominis plane block with conventional local anesthetic wound infiltration. Pak Armed Forces Med J. 2018;68(5):1106–10.
Bava EP, Ramachandran R, Rewari V, Chandralekha, Bansal VK, Trikha A. Analgesic efficacy of ultrasound guided transversus abdominis plane block versus local anesthetic infiltration in adult patients undergoing single incision laparoscopic cholecystectomy: a randomized controlled trial. Anesth Essays Res. 2016;10(3):561–7.
Paudel B, Paudel S, Rai P, Dahal S, Pokhrel A. Comparison of ultrasound guided bilateral subcostal Transversus abdominis plane block versus local infiltration of port site with bupivacaine in patients undergoing laparoscopic cholecystectomy under general anesthesia. Birat J Health Sci. 2021;6(3):1642–6.
Emile SH, Elfeki H, Elbahrawy K, Sakr A, Shalaby M. Ultrasound-guided versus laparoscopic-guided subcostal transversus abdominis plane (TAP) block versus no TAP block in laparoscopic cholecystectomy; a randomized double-blind controlled trial. Int J Surg. 2022;101:106639.
Choi YM, Byeon GJ, Park SJ, Ok YM, Shin SW, Yang K. Postoperative analgesic efficacy of single-shot and continuous transversus abdominis plane block after laparoscopic cholecystectomy: a randomized controlled clinical trial. J Clin Anesth. 2017;39:146–51.
Kapil Prajapati KKP, Baghel H, Prakash R. Alok Pratap Singh: ultrasound guided versus peripheral nerve stimulator guided Transversus abdominis plane block for postoperative analgesia in patients undergoing laparoscopic cholecystectomy: a randomised clinical study. J Clin Diagn Res. 2022;16(10):UC13–6.
Ergin A, Aydin MT, Çiyiltepe H, Karip AB, Fersahoğlu MM, Özcabi Y, et al. Effectiveness of local anesthetic application methods in postoperative pain control in laparoscopic cholecystectomies; a randomised controlled trial. Int J Surg. 2021;95:106134.
Richard Drake AWV, Mitchell A, Tibbitts R, Richardson P. Visceral afferent (sensory) innervation and referred pain diagram. In: Gray’s atlas of anatomy, third edition; 2020. p. 204.
Yi SQ, Ohta T, Tsuchida A, Terayama H, Naito M, Li J, et al. Surgical anatomy of innervation of the gallbladder in humans and Suncus murinus with special reference to morphological understanding of gallstone formation after gastrectomy. World J Gastroenterol. 2007;13(14):2066–71.
Raj P. Celiac plexus/splanchnic nerve blocks. Tech Reg Anesth Pain Manag. 2001;5(3):102–15.
Peng K, Ji F, Liu H, Wu S. Ultrasound-guided Transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: a systematic review and Meta-analysis. Med Princ Pract. 2016;25(3):237–46.
Xuan C, Yan W, Wang D, Li C, Ma H, Mueller A, et al. Efficacy of preemptive analgesia treatments for the management of postoperative pain: a network meta-analysis. Br J Anaesth. 2022;129(6):946–58.
De Oliveira GS Jr, Castro-Alves LJ, Nader A, Kendall MC, McCarthy RJ. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesth Analg. 2014;118(2):454–63.
Kalu R, Boateng P, Carrier L, Garzon J, Tang A, Reickert C, et al. Effect of preoperative versus postoperative use of transversus abdominis plane block with plain 0.25% bupivacaine on postoperative opioid use: a retrospective study. BMC Anesthesiol. 2021;21(1):114.
Muñoz-Leyva F, El-Boghdadly K, Chan V. Is the minimal clinically important difference (MCID) in acute pain a good measure of analgesic efficacy in regional anesthesia? Reg Anesth Pain Med. 2020;45(12):1000–5.
Griffiths JD, Barron FA, Grant S, Bjorksten AR, Hebbard P, Royse CF. Plasma ropivacaine concentrations after ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010;105(6):853–6.
Kato N, Fujiwara Y, Harato M, Kurokawa S, Shibata Y, Harada J, et al. Serum concentration of lidocaine after transversus abdominis plane block. J Anesth. 2009;23(2):298–300.
Abdallah FW, Laffey JG, Halpern SH, Brull R. Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth. 2013;111(5):721–35.
Støving K, Rothe C, Rosenstock CV, Aasvang EK, Lundstrøm LH, Lange KH. Cutaneous sensory block area, muscle-relaxing effect, and block duration of the Transversus abdominis plane block: a randomized, blinded, and placebo-controlled study in healthy volunteers. Reg Anesth Pain Med. 2015;40(4):355–62.
Trabelsi B, Charfi R, Bennasr L, Marzouk SB, Eljebari H, Jebabli N, et al. Pharmacokinetics of bupivacaine after bilateral ultrasound-guided transversus abdominis plane block following cesarean delivery under spinal anesthesia. Int J Obstet Anesth. 2017;32:17–20.
Fusco P, Scimia P, Paladini G, Fiorenzi M, Petrucci E, Pozone T, et al. Transversus abdominis plane block for analgesia after cesarean delivery. A systematic review. Minerva Anestesiol. 2015;81(2):195–204.
Fusco P, Cofini V, Petrucci E, Scimia P, Pozone T, Paladini G, et al. Transversus abdominis plane block in the Management of Acute Postoperative Pain Syndrome after caesarean section: a randomized controlled clinical trial. Pain Physician. 2016;19(8):583–91.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization, B.D., F.G. and A.A.; methodology, A.D.C, C.K. and E.B.; software, F.G., A.D.C.; validation, P.N., S.T. and A.A.; formal analysis, A.D.C., P.N., Y.E.K. and E.B.; investigation, B.D., F.G, M.B., Y.E.K and A.A.; resources,E.B., C.K., P.N.; data curation, B.D. and S.T.; writing—original draft preparation, B.D., A.D.C., E.B., S.T., M.B., Y.E.K.; writing—review and editing, B.D.,F.G., A.D.C., E.B., S.T., and A.A.; project administration, B.D. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary material 1.
Search Strategy.
Additional file 2: Supplementary material 2.
Funnel Plots.
Additional file 3: Supplementary Document 3.
Risk of bias assessment.
Additional file 4: Supp. 4.
Proportion of direct evidence for each comparison.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dost, B., De Cassai, A., Balzani, E. et al. Analgesic benefits of pre-operative versus postoperative transversus abdominis plane block for laparoscopic cholecystectomy: a frequentist network meta-analysis of randomized controlled trials. BMC Anesthesiol 23, 408 (2023). https://doi.org/10.1186/s12871-023-02369-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02369-6