Abstract
Background
Blood urea nitrogen to albumin ratio (BAR) is increasingly recognized as an early predictor for short-term outcomes in critically ill patients, but the association of BAR with long-term outcomes in critically ill surgical patients remains underexplored.
Methods
We enrolled consecutive patients who were admitted to surgical intensive care units (ICUs) at Taichung Veterans General Hospital between 2015 and 2020, and the dates of death were retrieved from Taiwan’s National Health Insurance Research Database. In addition to Cox regression, we also used propensity score matching to determine the hazard ratios (HRs) and 95% confidence intervals (CIs) for one-year post-hospital mortality of the variables.
Results
A total of 8,073 eligible subjects were included for analyses. We found that age, male gender, high Charlson Comorbidity Index, high Acute Physiology and Chronic Health Evaluation II score, positive microbial culture, and leukocytosis were predictors for mortality, whereas high body mass index, scheduled surgery, and high platelet counts were protective factors against long-term mortality. The high BAR was independently associated with increased post-hospital mortality after adjustment for the aforementioned covariates (adjHR 1.258, 95% CI, 1.127–1.405). Notably, the association tended to be stronger in females and patients with fewer comorbidities and lower disease severity of critical illness. The propensity score matching, dividing subjects by BAR higher or lower than 6, showed a consistent association between week-one BAR and post-hospital mortality (adjHR 1.503, 95% CI 1.247–1.811).
Conclusions
BAR is a newly identified predictor of short-term outcome, and we identified long-term outcome-relevant factors, including BAR, and the identified factors may be useful for risk stratification of long-term outcomes in patients discharged from surgical ICUs.
Similar content being viewed by others
Background
The long-term outcome of critically ill patients is an emerging issue in clinical practice; however, evidence focusing on critically ill surgical patients remains sparse [1,2,3]. Blood urea nitrogen (BUN) is a nitrogenous end-product of protein metabolism, and the elevated level of BUN reflects underlying catabolism in patients with acute illnesses, including acute myocardial infarction, pneumonia, acute pancreatitis, and infection with coronavirus disease 2019 (COVID-19) [4,5,6,7,8]. Albumin plays an essential physiological role, such as maintaining osmotic pressure as well as regulating fluid balance, and a low albumin level is a fundamental biomarker of protein-energy metabolism in critically ill surgical patients [9,10,11]. Increasing evidence shows the BUN to Albumin ratio (BAR) can predict the short-term outcome of critically ill patients [12,13,14]. For example, Dundar et al. found that an elevated BAR was a predictor of in-hospital mortality in older (> 65 years of age) emergency department patients [12]. A study conducted by Ata et al. found that BAR was a better independent predictor of in-hospital mortality than BUN or albumin alone in patients with severe COVID-19 infection [15]. Notably, Zhao D. et al. recently used the Medical Information Mart for Intensive Care III (MIMIC III) database with 1,462 patients who underwent coronary artery bypass grafting (CABG) and found that a high BAR during admission at the intensive care unit (ICU) was associated with long-term mortality [14]. These findings highlight the crucial role of BAR in critically ill surgical patients and indicate the need to clarify the prolonged impact of BAR on post-hospital mortality in critically ill surgical patients. In the present study, we linked data from the critical care database at Taichung Veterans General Hospital (TCVGH) with death registration data from Taiwan’s National Health Insurance Research Database to investigate factors associated with post-hospital long-term mortality and to determine the association between BAR and long-term mortality using both Cox regression and propensity score matching in critically ill surgical patients.
Materials and methods
Ethical approval
The study used de-identified data from the TCVGH critical care database and was approved by the Institutional Review Board of Taichung Veterans General Hospital (TCVGH: SE20249B-1), which waived the requirement for informed consent. The study was conducted in accordance with the Declaration of Helsinki.
Subjects enrollment
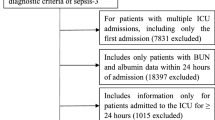
The cohort study was conducted at TCVGH, a tertiary referral hospital with 1,530 beds in central Taiwan. We enrolled consecutive patients who were admitted to three surgical ICUs at TCVGH during 2015–2020. Given that one patient may be admitted to the ICU more than one time, we used data of the first ICU admission for analyses of patients with more than one ICU admission. We retrieved data from the critical care database at TCVGH to obtain information on variables related to critical care, including demographic data, comorbidities using the International Classification of Diseases, both 9th and 10th Revision, Clinical Modification (ICD-9/10-CM) codes, divisions of ICU admission, the Acute Physiology and Chronic Health Evaluation (APACHE) II score, administration of vasopressors, results of microbial culture, mechanical ventilation, and renal replacement therapy.
Primary outcome
The primary outcome of interest of the present study was all-cause mortality after discharge from the surgical ICUs. To ascertain the date-of-death of enrolled subjects, we linked the aforementioned TCVGH critical care database with the death registration data of Taiwan’s National Health Insurance Research Database (NHIRD) [16]. Taiwan’s National Health Insurance (NHI) program is a single-payer, compulsory health insurance system that covers 99.9% of the population, and the information on date-of-death in this study was accurate.
Statistical analyses
Descriptive data were presented as means ± standard deviation or number (percentages). Kaplan-Meier analysis was applied to illustrate the association between BAR and post-hospital mortality. The Cox proportional hazards model was used to determine hazard ratios (HRs) and 95% confidence intervals (CI) of risk factors for mortality after adjustment for age, sex, Charlson Comorbidity Index (CCI), APACHE II, presence of shock, fluid balance, positive microbial culture, anaemia, and potential cofounders, as performed in our previous studies [17,18,19]. Statistical analyses were two-sided, and the level of significance was 0.05. Data analyses were performed using R version 3.6.0.
Propensity score matching
In the present study, we further utilized propensity score matching to mitigate potential selection bias and confounding effects between the two groups [20]. Propensity score matching (1:1) was performed to determine the impact of week-one BAR on one-year post-hospital mortality in critically ill surgical patients. We used the optimal nearest neighbor matching algorithm, and the caliper distance of the standard mean difference was 0.2 [21].
Subgroup analyses
To determine the effect of modification of variables, we further used the Wald test to determine the significance of the modification effect by covariates, including age, sex, body mass index, comorbidities, and severities of critical illness [22].
Results
Demographic and data of the enrolled critically ill surgical patients
In this study, we included 9,148 critically ill patients who were admitted to surgical ICUs at TCVGH between 2015 and 2020. We excluded 1,075 patients who died during hospitalization as the aim of this study was to identify factors associated with long-term, rather than short-term, outcomes. Of the 8,073 enrolled patients, 62.8% of them were male, and the average age was 60.4 ± 15.8 years (Fig. 1; Table 1). The average CCI was 1.6 ± 1.4, and the detailed comorbidities were summarised in the supplemental Table 1. The 30-day, 90-day, and one-year post-hospital mortality rates were 0.78% (63/8,073), 4.1% (329/8,073), and 13.5% (1,092/8,073), respectively. The main divisions of ICU admission were neurosurgery (51.6%), cardiovascular surgery (22.2%), and colorectal surgery/general surgery (10.6%). Among the enrolled subjects, 75.7% (6,111/8,073) of the patients had received the surgery during ICU admission, with 16.1% (1,297/8,073) and 59.6% (4,814/8,073) of the 6,111 patients receiving emergent surgery or scheduled surgery, respectively. Compared with the survivors, patients who died within one year after discharge appeared to have higher disease severities, with a higher APACHE II score (21.7 ± 5.3 vs. 19.8 ± 5.5, p < 0.001), were more likely to have shock (35.3% vs. 27.2%, p < 0.001), receive mechanical ventilation for more than 3 days (46.6% vs. 27.9%, p < 0.001), to undergo renal replacement therapy (6.8% vs. 3.1%, p < 0.001), to have a positive day 1–3 fluid balance (75.4% vs. 62.4%, p < 0.001), and to have a positive microbial culture (49.9% vs. 26.3%, p < 0.001). With regard to laboratory data, the non-survivors tended to have a lower level of hemoglobin (10.5 ± 1.7 vs. 11.5 ± 1.9 g/dL, p < 0.001), lower platelet counts (190.4 ± 94.1 vs. 203.0 ± 83.1 103/µL), and lower serum level of albumin (3.2 ± 0.7 vs. 3.6 ± 0.7 mg/dL, p < 0.001), but had higher levels of BUN (26.2 ± 19.0 vs. 19.4 ± 13.2, p < 0.001) and BAR (8.9 ± 7.4 vs. 5.8 ± 4.8, p < 0.001).
Association between week-one BUN/Albumin ratio and post-hospital one-year mortality
We used the Kaplan-Meier plot and BAR 6.0, the integral level of the median of BAR among enrolled subjects, as the cut-point value to illustrate that a high BAR was associated with increased post-hospital mortality (Fig. 2). The multivariable Cox proportional hazards model was constructed to identify factors associated with one-year post-hospital mortality in critically ill surgical patients. We found that older age (adjHR 1.253, 95% CI 1.104–1.422), male gender (adjHR 1.379, 95% CI 1.210–1.572), high CCI (adjHR 2.200, 95% CI 1.929–2.508), increased APACHE II score (adjHR 1.016, 95% CI 1.004–1.029), positive microbial culture (adjHR 1.577, 95% CI 1.359–1.829), and leukocytosis (adjHR 1.024, 95% CI 1.010–1.037) were predictors for mortality, whereas high BMI (adjHR 0.919, 95% CI 0.905–0.933), scheduled surgery (adjHR 0.858, 95% CI 0.757–0.973), and high platelet counts (adjHR 0.831, 95% CI 0.798–0.867) were protective factors against long-term mortality. Notably, the high BAR was independently correlated with increased post-hospital mortality after adjustment for the aforementioned covariates (adjHR 1.258, 95% CI, 1.127–1.405) (Table 2). We further assessed the variables with a potential to modify the association between BAR and long-term mortality and found that the correlation tended to be stronger in females and patients with fewer comorbidities and lower disease severity. The association was higher in patients with CCI < 2, APACHE II < 25, no need for hemodialysis, negative microbial culture, level of hemoglobin higher than 10 g/dL, and serum level of creatinine less than 1.5 mg/dL (Table 3). Taken together, we found that high BAR was independently correlated with post-hospital mortality in critically ill surgical patients and the correlation was stronger in patients with fewer comorbidities and low severity of critical illness.
Propensity-matched approach to verify the association between week-one BAR and one-year post-hospital mortality in critically ill surgical patients
In addition to the Cox regression model, we further used the propensity score-based approach to verify the aforementioned association between week-one BAR and one-year mortality in critically ill surgical patients. To be consistent with the Kaplan-Meier plot (Fig. 2), we also divided the enrolled subjects by BAR 6.0 and then used 1:1 propensity score matching for the following analyses (Supplemental Fig. 1 for the flow diagram of propensity score matching). Supplemental Table 1 summarizes the characteristics of the selected subjects whose BAR values were higher and lower than 6.0 (Supplemental Table 2 for characteristis between the patients in the primary cohort and propensity score-matched cohort). The quality of matching was high as the standardized difference of covariates was lower than 0.15 (Supplemental Fig. 2 for the standardised mean difference in primary and propensity score-matched populations). We found a consistent association between week-one BAR and post-hospital mortality in both the primary cohort and PSM cohort, with an adjHR in the PSM of 1.503 (95% CI 1.247–1.811) (Table 4).
Discussion
In this study, we investigated the association between early BAR and long-term post-hospital outcome in critically ill surgical patients. We found that high week-one BAR correlated with post-hospital mortality in critically ill surgical patients, and the association tended to be stronger in females and patients with fewer comorbidities and lower disease severity of critical illness. In addition to the aforementioned Cox regression model, we also used a propensity score-matched approach to demonstrate a consistent association between week-one BAR and post-hospital mortality in critically ill surgical patients. These data highlight the previously underexplored long-term outcome-relevant factors that may be used for risk stratification of long-term outcomes in patients discharged from surgical ICUs.
Long-term outcomes are increasingly recognized as an essential issue in critical care medicine, but it is somewhat difficult to delineate the impact of management in critical illness on short-term and long-term outcomes [1]. The majority of studies that explored early determinants of long-term outcomes used long-term survival as the independent variable; however, long-term survival without the exclusion of hospital mortality might mainly reflect the severity of critical illness rather than the prolonged impact of critical illness [23]. Moreover, most studies exploring long-term outcomes were conducted in medical/mixed ICUs, whereas studies focusing on critically ill surgical patients are sparse [2]. In the present study, we excluded those who died during admission, and the findings support the prognostic role of week-one BAR among patients discharged from surgical ICUs.
BUN is a low-molecular-weight nitrogen product derived from protein catabolism and excreted by the kidney [24]. Therefore, BUN reflects protein intake, endogenous protein catabolism, fluid balance, hepatic urea synthesis, and fluid/renal status in critically ill patients and have been widely used as a prognostic marker in patients with various surgical diseases [5, 7, 25]. Similarly, albumin also has various biological effects, including maintenance of osmotic pressure, binding and transport of various drugs, and neutralization of free radicals, and hypoalbuminemia has been identified as a poor prognostic factor in critically ill surgical patients [9, 11, 26]. Given that BAR, consisting of elevated BUN with hypoalbuminemia, appeared to be involved in the aforementioned physiological mechanisms, accumulating evidence indicates that high BAR was an independent poor prognostic factor in a variety of diseases, including ischemic stroke, community-acquired pneumonia, gastrointestinal bleeding, and COVID-19 infection [13, 27,28,29].
In the present study, we provide further clinical evidence on the long-term mortality impact of high BAR in the first week in critically ill surgical patients. We postulate that the high BAR may reflect not only organ dysfunction but also ongoing catabolism with impaired protein/albumin synthesis, which is a persistent catabolic state after critical illness [30, 31]. Recent evidence further suggests that hypercatabolism occurs along with persistent inflammation and immunosuppression, giving rise to a syndrome termed PICS (persistent inflammation, immunosuppression and catabolism syndrome). A number of therapeutic approaches, including specific nutritional support, anti-inflammatory agents, anabolic agents, antioxidants, microbiota modulators, and early mobilization, are currently being explored with a view to ameliorating hypercatabolism in critically ill patients [31, 32]. Intriguingly, we not only found that high week-one BAR was correlated with increased post-hospital mortality, but also noted that the aforementioned correlation tends to be stronger among those with relatively fewer comorbidities or low severities of critical illness (Table 3). It is reasonable to suppose that dysregulated protein metabolism and nutritional status would be more likely to be restored within one week in critically ill surgical patients with low disease severity compared with those with high disease severity.
Recently, Zhao D et al. used Medical Information Mart for Intensive Care (MIMIC) III databases to analyze 1,462 patients receiving CABG, and found that BAR higher than 6.45 was associated with increased long-term mortality, which was consistent with our findings [14]. In their study, Zhao D et al. found a higher BAR was an independent risk factor of one-year mortality (HR 3.904; 95% CI 2.559–5.956) [14]. In the present study, we excluded patients who died during admission and focused on the 8,073 patients discharged from surgical ICUs. Furthermore, we found a consistent association between BAR and post-hospital mortality among those receiving cardiovascular surgery, neurosurgery, and abdominal surgery (Table 3). Moreover, we used propensity score matching to further validate the association between BAR and post-hospital mortality in addition to the Cox regression model. Additionally, whereas the MIMIC III (2001–2012) covers a relatively old time span, the dataset used in this study represents the current (2015–2020) management and prognosis of critically ill surgical patients. Both the present study and the study conducted by Zhao D et al. were single-center studies, and therefore, prospective multi-center studies are warranted to confirm our findings.
We used BAR 6.0 as the cut-point value in this study to achieve the balance between patients with high and low BAR. A number of BAR relevant studies have used distinct cut-point values [12,13,14, 28, 33], and we hence tested the consistence of our results using distinct cut-point values of BAR. We found a consistent association between week-one BAR and one-year post-hospital mortality among the enrolled critically ill surgical patients (Supplemental Fig. 3).
There were limitations in this study. First, the study was an observational study, and therefore, it was only possible to observe associations, rather than causal effects of BAR on mortality. Second, multi-center studies are needed to validate our findings, even though the number of subjects in the present study was high. Third, the potential unmeasured confounders in this retrospective study remain a concern despite the application of propensity score matching. Additionally, the potential existence of some unmeasured confounders, such as stroke, coronary arterial disease, or autoimmune disease.
Conclusion
Long-term outcome-associated early predictors are an emerging research priority in critically ill surgical patients, and recent studies have shown that BAR was a predictor of short-term outcome in patients with inflammatory diseases and critical illnesses. In the present study, we linked two databases to investigate the factors associated with one-year post-hospital mortality in critically ill surgical patients. We used both the Cox regression model and propensity score matching approach to identify a consistent association between week-one BAR and one-year post-hospital mortality in critically ill surgical patients. Our findings highlight the crucial role of BAR as a long-term prognostic factor in critically ill surgical patients, and more studies are warranted to elucidate the underlying mechanism.
Data availability
The data underlying this article will be shared upon reasonable request to the corresponding author.
References
Gayat E, Cariou A, Deye N, Vieillard-Baron A, Jaber S, Damoisel C, et al. Determinants of long-term outcome in ICU survivors: results from the FROG-ICU study. Crit Care. 2018;22:8.
Shankar-Hari M, Ambler M, Mahalingasivam V, Jones A, Rowan K, Rubenfeld GD. Evidence for a causal link between sepsis and long-term mortality: a systematic review of epidemiologic studies. Crit Care. 2016;20:101.
Wilcox ME, Ely EW. Challenges in conducting long-term outcomes studies in critical care. Curr Opin Crit Care. 2019;25:473–88.
Zhu Y, Sasmita BR, Hu X, Xue Y, Gan H, Xiang Z, et al. Blood Urea Nitrogen for short-term prognosis in patients with cardiogenic shock complicating Acute myocardial infarction. Int J Clin Pract. 2022;2022:9396088.
Arnan MK, Hsieh TC, Yeboah J, Bertoni AG, Burke GL, Bahrainwala Z, et al. Postoperative blood urea nitrogen is associated with stroke in cardiac surgical patients. Ann Thorac Surg. 2015;99:1314–20.
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82.
Faisst M, Wellner UF, Utzolino S, Hopt UT, Keck T. Elevated blood urea nitrogen is an independent risk factor of prolonged intensive care unit stay due to acute necrotizing pancreatitis. J Crit Care. 2010;25:105–11.
Cheng A, Hu L, Wang Y, Huang L, Zhao L, Zhang C, et al. Diagnostic performance of initial blood urea nitrogen combined with D-dimer levels for predicting in-hospital mortality in COVID-19 patients. Int J Antimicrob Agents. 2020;56:106110.
Nicholson JP, Wolmarans MR, Park GR. The role of albumin in critical illness. Br J Anaesth. 2000;85:599–610.
Dubois MJ, Orellana-Jimenez C, Melot C, De Backer D, Berre J, Leeman M, et al. Albumin administration improves organ function in critically ill hypoalbuminemic patients: a prospective, randomized, controlled, pilot study. Crit Care Med. 2006;34:2536–40.
Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg. 2003;237:319–34.
Dundar ZD, Kucukceran K, Ayranci MK. Blood urea nitrogen to albumin ratio is a predictor of in-hospital mortality in older emergency department patients. Am J Emerg Med. 2021;46:349–54.
Kucukceran K, Ayranci MK, Girisgin AS, Kocak S, Dundar ZD. The role of the BUN/albumin ratio in predicting mortality in COVID-19 patients in the emergency department. Am J Emerg Med. 2021;48:33–7.
Zhao D, Chen S, Liu Y, Xu Z, Shen H, Zhang S, et al. Blood Urea Nitrogen-to-albumin ratio in Predicting Long-Term Mortality in Patients following coronary artery bypass grafting: an analysis of the MIMIC-III database. Front Surg. 2022;9:801708.
Ata F, As AK, Engin M, Kat NK, Ata Y, Turk T. Can blood urea Nitrogen-to-Albumin ratio predict mortality in patients with moderate-to-severe COVID-19 pneumonia hospitalized in the intensive care unit? Rev Assoc Med Bras (1992). 2021;67:1421-6.
Hsing AW, Ioannidis JP. Nationwide Population Science: Lessons from the Taiwan National Health Insurance Research Database. JAMA Intern Med. 2015;175:1527–9.
Wu CL, Pai KC, Wong LT, Wang MS, Chao WC. Impact of early fluid balance on long-term mortality in critically Ill Surgical Patients: a retrospective cohort study in Central Taiwan. J Clin Med. 2021;10.
Wu YC, Wong LT, Wu CL, Chao WC. The association between culture positivity and long-term mortality in critically ill surgical patients. J Intensive Care. 2021;9:66.
Wu F-H, Wong L-T, Wu C-L, Chao W-C. Week-One Anaemia was Associated with increased one-year mortality in critically Ill Surgical Patients. Int J Clin Pract. 2022;2022:8121611.
ROSENBAUM PR, RUBIN DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Dehejia RH. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 2002;84:151–61.
Laskar MR, King ML. Modified Wald test for regression disturbances. Econ Lett. 1997;56:5–11.
Braber A, van Zanten AR. Unravelling post-ICU mortality: predictors and causes of death. Eur J Anaesthesiol. 2010;27:486–90.
Checchio LM, Como AJ. Electrolytes, BUN, creatinine: who’s at risk? Ann Emerg Med. 1986;15:363–6.
Liu Y, Hu H, Li Z, Han Y, Chen F, Zhang M, et al. Association between pre-operative BUN and post-operative 30-Day mortality in patients undergoing craniotomy for tumors: data from the ACS NSQIP database. Front Neurol. 2022;13:926320.
Lapenna D, Ciofani G, Ucchino S, Pierdomenico SD, Cuccurullo C, Giamberardino MA, et al. Serum albumin and biomolecular oxidative damage of human atherosclerotic plaques. Clin Biochem. 2010;43:1458–60.
Xu WH, Dong C, Rundek T, Elkind MS, Sacco RL. Serum albumin levels are associated with cardioembolic and cryptogenic ischemic strokes: Northern Manhattan Study. Stroke. 2014;45:973–8.
Agarwal M, Joshi M, Gupta M, Bharti N, Chakraborti A, Sonigra M. Role of blood urea nitrogen and serum albumin ratio in predicting severity of community acquired pneumonia (CAP). Monaldi Arch Chest Dis. 2021;92.
Bae SJ, Kim K, Yun SJ, Lee SH. Predictive performance of blood urea nitrogen to serum albumin ratio in elderly patients with gastrointestinal bleeding. Am J Emerg Med. 2021;41:152–7.
Mira JC, Brakenridge SC, Moldawer LL, Moore FA. Persistent inflammation, immunosuppression and catabolism syndrome. Crit Care Clin. 2017;33:245–58.
Voiriot G, Oualha M, Pierre A, Salmon-Gandonniere C, Gaudet A, Jouan Y, et al. Chronic critical illness and post-intensive care syndrome: from pathophysiology to clinical challenges. Ann Intensive Care. 2022;12:58.
Zhang J, Luo W, Miao C, Zhong J. Hypercatabolism and anti-catabolic therapies in the persistent inflammation, immunosuppression, and catabolism syndrome. Front Nutr. 2022;9:941097.
Wang Y, Gao S, Hong L, Hou T, Liu H, Li M, et al. Prognostic impact of blood urea nitrogen to albumin ratio on patients with sepsis: a retrospective cohort study. Sci Rep. 2023;13:10013.
Acknowledgements
We thank Dr. Chieh-Liang Wu and the TCVGH artificial intelligence studio to provide technical help for the TCVGH critical care database.
Funding
This study was supported by Veterans General Hospitals (TCVGH-112G213 and TCVGH-112G211). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Study conception and design: K-NN, T-IC, M-CC, and W-CC. Acquisition of data: L-TW, M-CC, and W-CC. Analysis and interpretation of data: L-TW and W-CC. Drafting of manuscript: K-NN, T-IC, and W-CC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. The study used de-identified data from the TCVGH critical care database and was approved by the Institutional Review Board of Taichung Veterans General Hospital (TCVGH: SE20249B-1), which waived the requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nguyen, K.N., Chuang, TI., Wong, LT. et al. Association between early blood urea nitrogen-to-albumin ratio and one-year post-hospital mortality in critically ill surgical patients: a propensity score-matched study. BMC Anesthesiol 23, 247 (2023). https://doi.org/10.1186/s12871-023-02212-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02212-y