Abstract
Background
Acute kidney injury (AKI) is one of the most common postoperative complications in noncardiac surgical patients, has an important impact on prognosis and is difficult to predict. Whether preoperative N-terminal pro-brain natriuretic peptide (NT-proBNP) concentrations and left ventricular ejection fraction (LVEF) levels can predict postoperative AKI in noncardiac surgical patients is unclear.
Methods
We included 3,314 patients who underwent noncardiac surgery and had measurements of preoperative NT-proBNP concentrations and LVEF levels at a tertiary academic hospital in China between 2008 and 2018. Multiple logistic regression analysis was used to construct a postoperative AKI risk prediction model for this cohort. Then, NT-proBNP concentrations and LVEF levels were included in the abovementioned model as independent variables, and the predictive ability of these two models was compared.
Results
Postoperative AKI occurred in 223 (6.72%) patients within 1 week after surgery. Preoperative NT-proBNP concentrations and LVEF levels were independent predictors of AKI after adjustment for clinical variables. The area under the receiver operating characteristic curve (AUROC) of the AKI risk predictive model established with clinical baseline variables was 0.767 (95% CI: 0.732, 0.802). When NT-proBNP concentrations and LVEF levels were added to the base model, the AUROC was 0.811 (95% CI: 0.779, 0.843). The addition of NT-proBNP concentrations and LVEF levels improved reclassification by 22.9% (95% CI 10.5–34.4%) for patients who developed postoperative AKI and by 36.3% (95% CI 29.5–43.9%) for those who did not, resulting in a significant overall improvement in net reclassification (NRI: 0.591, 95% CI 0.437–0.752, P < 0.000). The integral discrimination improvement was 0.100 (95% CI: 0.075, 0.125, P < 0.000).The final postoperative AKI prediction model was constructed, and had a good discriminative ability and fitted to the dataset.
Conclusions
Preoperative NT-proBNP concentrations and LVEF levels were independently associated with the risk of AKI after noncardiac surgery, and they could improve the predictive ability of logistic regression models based on conventional clinical risk factors.
Trial registration
The protocol was preregistered in the Chinese Clinical Trial Registry (ChiCTR1900024056).
Similar content being viewed by others
Background
Acute kidney injury (AKI) is a common complication during the early postoperative period after noncardiac surgery. Some scholars have reported that the prevalence of AKI after thoracic surgery is approximately 12%, while the pooled incidence of AKI after abdominal surgery is 13.4% [1, 2]. Increased postoperative serum creatinine, even in those who did not develop renal disease, was associated with adverse outcomes, including increased morbidity, length of hospitalization, health care costs and short- and long-term mortality [3,4,5,6]. In such settings, the development of risk prediction models for AKI that could be used to risk stratify patients to develop avoidance, preventative or early treatment approaches was listed as a research recommendation in the Kidney Disease: Improving Global Outcomes (KDIGO) clinical practice guidelines for AKI. Currently, a substantial number of risk prediction models have been reported to predict AKI after cardiac surgery, and many of them have been externally validated in more than one independent cohort [7,8,9,10,11,12,13,14,15]. However, the prediction of AKI after major noncardiac surgeries has received much less attention, although the incidence of AKI ranges from 7 to 30% [16]. Only a few prediction models for AKI after noncardiac surgery have been explored in patients who underwent a single type of specialized surgery, which represents only a subset of noncardiac surgeries. Therefore, the value of these models is limited. Moreover, a recent study suggested the predictive ability of NT-proBNP concentrations for AKI in the perioperative period in patients who underwent living donor liver transplantation [17]. Another study found that patients with decreased left ventricular systolic function are at increased risk for postoperative infections and kidney injury, demonstrating a relationship between cardiac dysfunction and noncardiac complications after surgery [18]. Whether NT-proBNP concentrations and LVEF levels could provide additional predictive information beyond conventional AKI risk factors in a broader and heterogeneous group of noncardiac surgical patients is still unknown [19]. Therefore, considering the complex interactions between renal and cardiac dysfunction and that NT-proBNP concentrations and LVEF levels are good markers for assessing haemodynamic stress and cardiac dysfunction, we added preoperative NT-proBNP concentrations and LVEF levels to the preoperative risk prediction model for AKI following noncardiac surgery constructed using by the conventional AKI risk factors and determined whether they could improve the prediction ability.
Methods
The clinical data of all patients were obtained from a tertiary hospital in Guangzhou, China. This study complied with the Declaration of Helsinki and was approved by the Ethics Committee of Southern Medical University Nanfang Hospital without the need for informed consent from the participants (NFEC-2019–081). Additionally, as this was a retrospective study, all identifying information of the patients was removed before analysis [19].
Patients
The study was a secondary analysis of a subset of data which have been used in a previous study by our research team [19]. The previous study found that preoperative NT-proBNP concentrations were independently associated with the risk of AKI after noncardiac surgery and could provide predictive information for AKI after noncardiac surgery. The data of all participants were collected retrospectively from the hospital’s perioperative data warehouse, which is a collaborative programme between Shanghai Lejiu Healthcare Technology Co., Ltd and Southern Medical University Nanfang Hospital. The data warehouse contains demographic characteristics, preoperative medical and medication history, laboratory findings and surgical characteristics for all patients undergoing surgery in the Department of Anesthesiology since 2008. We have considered all adult patients who, from February 2008 through May 2018, underwent major or intermediate noncardiac surgical procedures [20] under regional or general anaesthesia at our hospital. Included patients were required to have serum creatinine, NT-proBNP concentrations, and LVEF levels’ measurements within 30 days before surgery and at least one serum creatinine measurement within 7 days of surgery. For patients who have underwent multiple surgeries during a single hospital stay, only the first surgery was considered. The exclusion criteria for this study were as follows: (1) patients who underwent minor surgical procedure as defined by the 2014 ESC/ESA guidelines on non-cardiac surgery: Cardiovascular assessment and management [20]. (2) patients who underwent cardiac, neurological, vascular, urological, ophthalmology, transplant or obstetric procedures; (3) patients with an estimated glomerular filtration rate < 15 ml min-1 1.73 m2; (4) patients with acute kidney injury diagnosed by a clinician before surgery; (5) patients with a history of renal replacement therapy or kidney transplantation [19].
Variables
Baseline factors potentially associated with postoperative AKI were selected based on literature review. We collected the patients’ preoperative demographic characteristics (sex, age, body mass index), preoperative medical and medication histories (hypertension, congestive heart failure, diabetes, coronary heart disease, ascites, stroke or transient ischaemic attack, the use of renin–angiotensin–aldosterone system inhibitors), laboratory findings (the estimated glomerular filtration rate, serum albumin, proteinuria, haemoglobin), surgical characteristics (type and duration of surgery, type of anaesthesia, emergency surgery or not, major or intermediate surgery [20]) and American Society of Anesthesiologists physical status as the baseline information [19]. The preoperative estimated glomerular filtration rate was estimated preoperatively base on the most recent serum creatinine values using a modified Modification of Diet in Renal Disease equation [21].
Preoperative serum NT-proBNP concentrations were measured in the laboratory department of the hospital using a Roche Elecsys NT-proBNP assay (Roche Diagnostics, Shanghai, China). LVEF level was also measured by a Toshiba Apollo 600. The examinations were completed by certified sonographers. If more than 1 echocardiographic measurement existed, the most recent preoperative measurement was used. Measurements of NT-proBNP concentrations and LVEF levels were ordered based on clinical indications or for preoperative cardiac risk assessment. For patients who had multiple measurements of preoperative NT-proBNP concentrations and LVEF levels, the most recent values were used.
AKI was defined by the Kidney Disease: Improving Global Outcomes (KDIGO) criteria (increase in serum creatinine of ≥ 26.5 μmol l−1 within 48 h or ≥ 1.5 times the baseline value within 7 days after surgery) [22].
Statistical analysis
Continuous variables are presented as medians and interquartile ranges, and categorical variables are presented as counts and percentages. We compared continuous variables with the Mann–Whitney U test and categorical variables with the χ2 or Fisher exact test. Because the distribution of NT-proBNP concentrations was skewed, it was transformed by taking the natural logarithm (ln) [19]. We performed multivariate logistic regression analysis to construct the AKI prediction model with and without NT-proBNP concentrations and LVEF levels.
We calculated the odds ratio (OR) and 95% confidence interval (CI) of all baseline independent variables in both prediction models to determine the predictive significance of preoperative NT-proBNP concentrations and LVEF levels for postoperative acute kidney injury and to assess whether they are independent risk factors. The discrimination ability of the prediction model when preoperative NT-proBNP concentrations and LVEF levels were included was compared by using DeLong’s method to test the change in the area under the receiver operating characteristic curve (AUROC). To evaluate the impact of preoperative NT-proBNP concentrations and LVEF levels on AKI risk prediction, we determined the continuous net reclassification index (NRI) and the integrated discrimination improvement (IDI) index values [23, 24]. Due to the lack of clearly predefined clinical risk thresholds for postoperative AKI, the categorical NRI was not used. CIs are reported for the AUROC and reclassification indices (continuous NRI, IDI, relative IDI). All baseline variables with NT-proBNP concentrations and LVEF levels were analysed by forward stepwise method for multivariate logistic regression analysis. All significant variables were selected to construct the final model for postoperative AKI prediction. The calibration of the model was tested by the Hosmer and Lemeshow goodness of fit (GOF) test.
Statistical analyses were performed using Rstudio Version 1.1.383, MedCalc Version 19.0.7 and SPSS software Version 22. All statistical tests were 2-tailed.
Results
Characteristics of the study cohort
Among the 3,314 patients enrolled in this study (the patient selection process is shown in Fig. 1), 6.72% (223 of the 3,314 patients) developed AKI within 1 week after surgery. The baseline characteristics of the patients, both overall and stratified by the presence of postoperative AKI, are provided in Table 1. The median age was 67 years (interquartile range 60 to 73 years), and 52.2% of patients in the cohort were male. Patients who developed AKI were older (70 years, interquartile range 63 to 75 years) and more likely to be male (141 males, 63.2%) and more likely to have more baseline comorbidities. Hypertension, diabetes, stroke, coronary heart disease and congestive heart failure were the most common noncardiac comorbidities. In this study, patients who underwent the minor surgeries were excluded. Among the patients included in the study, the proportion of patients with postoperative AKI who underwent major surgery was higher than that of patients without postoperative AKI.
The median overall preoperative NT-proBNP concentration was 76.36 pg ml−1 (interquartile range 39.86 to 178.47 pg ml−1), and the preoperative NT-proBNP concentrations were markedly higher in patients who developed AKI after surgery than among those who did not (median 163.10 versus 72.74 pg ml−1, P < 0.001, Table 1). The median preoperative LVEF level was lower in patients who developed AKI after surgery than among those who did not (median 61.00% versus 66.00%, P < 0.001, Table 1).
Associations between baseline variables and AKI
In the base AKI prediction model containing baseline variables but not NT-proBNP concentrations and LVEF levels, the aORs and 95% CIs of 7 predictors, including sex, ASA physical status, coronary heart disease, congestive heart failure, hypertension, the use of RAAS inhibitors,the duration of surgery, and proteinuria, were greater than 1 (all P values < 0.05). The aOR and 95% CI of thoracic surgery were less than 1, and the P value was < 0.05. When NT-proBNP concentrations and LVEF levels were added to the base model, the aORs and 95% CIs of above-mentioned 7 predictors were still greater than 1, and all P values were < 0.05 (Table 2).
Associations between NT-proBNP concentrations, LVEF levels and AKI
When patient demographics, medical history, laboratory findings, surgical characteristics, NT-proBNP concentrations and LVEF levels were included in the logistic model, we found that preoperative NT-proBNP concentrations and LVEF levels were significantly and independently associated with AKI risk. The aOR and 95% CI of preoperative NT-proBNP concentrations were greater than 1 (adjusted OR: 1.269, 95% CI 1.001–1.463, P = 0.001, Table 2). The aOR and 95% CI of LVEF levels were less than 1 (adjusted OR: 0.911, 95% CI 0.895–0.928, P < 0.001, Table 2).
Additive value of NT-proBNP concentrations and LVEF levels in risk prediction
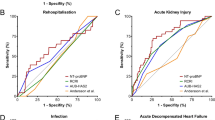
The AUROC of the postoperative AKI prediction models with (0.811, 95% CI 0.779–0.843, Table 3) and without preoperative NT-proBNP concentrations and LVEF levels (0.767, 95% CI 0.732–0.802, Table 3) showed statistical significance (P < 0.001). The addition of NT-proBNP concentrations and LVEF levels to the base model also improved reclassification by 22.9% (95% CI 10.5–34.4%) for patients who developed postoperative AKI and by 36.3% (95% CI 29.5–43.9%) for those who did not, resulting in a significant overall improvement in net reclassification (NRI 0.591 95% CI 0.437, 0.752, P < 0.001). The absolute IDI was 0.100 (95% CI: 0.075, 0.125, P < 0.000).
The final model for the prediction of acute kidney injury after noncardiac surgery
All baseline variables with NT-proBNP concentrations and LVEF levels were analysed by forward stepwise method for multivariate logistic regression analysis. All significant variables were selected for the final model (Table 4), including sex, ASA physical status, coronary heart disease, congestive heart failure, hypertension, the use of RAAS inhibitors,the duration of surgery, proteinuria, NT-proBNP concentrations and LVEF levels. The final postoperative AKI prediction model had a good discriminative ability with AUROC = 0.800 ( 95% CI 0.766–0.833, Fig. 2), and fitted to the dataset by GOF (χ2 = 12.042, P = 0.15).
Discussion
NT-proBNP concentrations and LVEF levels are important predictive markers of adverse cardiovascular events after noncardiac surgery [18, 25,26,27,28]. Guidelines on perioperative cardiac risk assessment recommend measuring NT-proBNP concentrations and LVEF levels in at-risk patients before noncardiac surgery. NT-proBNP concentrations and LVEF levels are increasingly readily available to anaesthesiologists and surgeons before surgery, especially in patients with more cardiovascular comorbidities. However, there are more current studies on the associations between NT-proBNP concentrations and LVEF levels and AKI after cardiac surgery than before noncardiac surgery. Only a few reports have indicated that postoperative AKI is associated with BNP concentrations or LVEF levels in a single type of noncardiac surgery [17, 18, 29]. Our study shows that in a heterogeneous group of patients undergoing mixed types of noncardiac surgery, preoperative NT-proBNP concentrations and LVEF levels are independently associated with postoperative AKI. This result is also consistent with previous reports that NT-proBNP concentration and LVEF level were associated with the risk of AKI in certain settings [18, 19, 30,31,32,33,34,35].
For the convenience of discussion, the postoperative AKI prediction models with and without preoperative NT-proBNP concentrations and LVEF levels are defined as the compound model and the base model, respectively. As shown by the statistically significant improvements in the C statistics (AUC), continuous NRI and IDI, we found that adding preoperative NT-proBNP concentrations and LVEF levels to the base model improved AKI risk prediction in our study cohort. In the two preoperative risk prediction models constructed in this study, the C statistics were both > 0.75, which indicated good prediction abilities, and the C statistic of the compound model was significantly higher than that of the base model (P < 0.05). In the previous risk prediction model of AKI after noncardiac surgery established by Kheterpal et al. [36] and Bell et al. [3], the C statistics ranged from 0.70 to 0.85. In our study, the C statistic was also within this range, indicating that the predictive ability is comparable to that of the previously studied models.
The mechanism by which NT-proBNP concentration and LVEF level predict AKI is currently unclear. An increase in the NT-proBNP concentration and a decrease in the LVEF level may be caused by a patient's increased venous pressure, diastolic filling pressure, and abnormal ventricular systolic function, and the occurrence of these conditions may in turn antagonize the expansion of circulating blood vessels and act on the renin–angiotensin–aldosterone system, which may lead to impaired kidney function. In this study, we constructed the final model, including sex, ASA physical status, coronary heart disease, congestive heart failure, hypertension, the use of RAAS inhibitors,the duration of surgery, proteinuria, NT-proBNP concentrations and LVEF levels. All these factors may result in different pathophysiological characteristics, which can affect the risk and severity of AKI.
Several limitations of this study should be mentioned here. This study was a retrospective cohort study, and it is uncertain whether preoperative intervention for NT-proBNP concentrations and LVEF levels can reduce the risk of postoperative AKI. The lack of data such as fasting blood glucose, glycosylated haemoglobin, intraoperative fluid rehydration and blood loss and intraoperative urine volume may have affected the evaluation of the risk prediction model. In addition, the inclusion criteria of this study stipulated that the patients must have undergone cardiac colour Doppler ultrasound and NT-proBNP measurement before surgery, which limited the number of patients enrolled to a certain extent and reduced the generalizability of the research model. The study cohort was biased towards a population with more cardiovascular comorbidities than the overall noncardiac surgical population, which probably had a higher AKI risk. These untested patients were likely to be younger, have fewer complications and lower preoperative creatinine levels. Therefore, whether the NT-proBNP- and LVEF-based preoperative risk prediction model is applicable to a relatively healthy population needs to be tested in a prospective trial.
Conclusions
In this single-centre retrospective study, we found that preoperative NT-proBNP concentrations and LVEF levels were independently associated with the risk of AKI after noncardiac surgery, and they can improve the predictive ability of logistic regression models based on conventional clinical risk factors. Whether preoperative assessment and intervention based on NT-proBNP concentrations and LVEF levels can reduce the incidence of postoperative AKI requires further prospective studies.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to the protection of the participants' rights to privacy but are available from the corresponding author upon reasonable request.
Abbreviations
- AKI:
-
Acute kidney injury
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- LVEF:
-
Left ventricular ejection fraction
- AUROC:
-
Area under the receiver operating characteristic curve
- KDIGO:
-
Kidney Disease: Improving Global Outcomes
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- GOF:
-
Hosmer and Lemeshow goodness of fitnet
- IDI:
-
Integral discrimination improvement
- NRI:
-
Net reclassification improvement
- SMUNH:
-
Southern Medical University Nanfang Hospital
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- eGFR:
-
Estimated glomerular filtration rate
- IQR:
-
Interquartile range
- RAAS:
-
Renin-angiotensin-aldosterone system
- aOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- AUC:
-
Area under the curve
References
Zarbock A, Koyner JL, Hoste EAJ, Kellum JA. Update on perioperative acute kidney injury. Anesth Analg. 2018;127:1236–45.
O’connor ME, Kirwan CJ, Pearse RM, et al. Incidence and associations of acute kidney injury after major abdominal surgery. Intensive Care Med. 2016;42(4):521–30.
Bell S, Dekker FW, Vadiveloo T, Marwick C, Deshmukh H, Donnan PT, et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery–Development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ. 2015;351:h5639.
O’Connor ME, Hewson RW, Kirwan CJ, Ackland GL, Pearse RM, Prowle JR. Acute kidney injury and mortality 1 year after major non-cardiac surgery. Br J Surg. 2017;104:868–76.
Grams ME, Sang Y, Coresh J, Ballew S, Matsushita K, Molnar MZ, et al. Acute kidney injury after major surgery: a retrospective analysis of veterans health administration data. Am J Kidney Dis. 2016;67:872–80.
Hobson C, Ozrazgat-Baslanti T, Kuxhausen A, Thottakkara P, Efron PA, Moore FA, et al. Cost and mortality associated with postoperative acute kidney injury. Ann Surg. 2015;261:1207–14.
Mehta RH, Grab JD, O'Brien SM, Bridges CR, Gammie JS, Haan CK, et al. Bedside tool for predicting the risk of postoperative dialysis in patients undergoing cardiac surgery. Circulation. 2006;114:2208–16. quiz.
Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP. A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol. 2005;16:162–8.
Demirjian S, Schold JD, Navia J, Mastracci TM, Paganini EP, Yared JP, et al. Predictive models for acute kidney injury following cardiac surgery. Am J Kidney Dis. 2012;59:382–9.
Wijeysundera DN, Karkouti K, Dupuis JY, Rao V, Chan CT, Granton JT, et al. Derivation and validation of a simplified predictive index for renal replacement therapy after cardiac surgery. JAMA. 2007;297:1801–9.
Jiang W, Teng J, Xu J, Shen B, Wang Y, Fang Y, et al. Dynamic predictive scores for cardiac surgery-associated acute kidney injury. J Am Heart Assoc. 2016;5:e003754.
Birnie K, Verheyden V, Pagano D, Bhabra M, Tilling K, Sterne JA, et al. Predictive models for kidney disease: improving global outcomes (KDIGO) defined acute kidney injury in UK cardiac surgery. Crit Care. 2014;18:606.
Englberger L, Suri RM, Li Z, Dearani JA, Park SJ, Sundt TM 3rd, et al. Validation of clinical scores predicting severe acute kidney injury after cardiac surgery. Am J Kidney Dis. 2010;56:623–31.
Thakar CV, Liangos O, Yared JP, Nelson DA, Hariachar S, Paganini EP. Predicting acute renal failure after cardiac surgery: validation and re-definition of a risk-stratification algorithm. Hemodial Int. 2003;7:143–7.
Candela-Toha A, Elías-Martín E, Abraira V, Tenorio MT, Parise D, De Pablo A, et al. Predicting acute renal failure after cardiac surgery: external validation of two new clinical scores. Clin J Am Soc Nephrol. 2008;3:1260–5.
Wilson T, Quan S, Cheema K, et al. Risk prediction models for acute kidney injury following major noncardiac surgery: systematic review. Nephrol Dial Transplant. 2016;31(2):231–40.
Chae MS, Park H, Choi HJ, Park M, Chung HS, Hong SH, et al. Role of serum levels of intraoperative brain natriuretic peptide for predicting acute kidney injury in living donor liver transplantation. PLoS ONE. 2018;13:e0209164.
Maile MD, Armstrong WF, Jewell ES, Engoren MC. Impact of ejection fraction on infectious, renal, and respiratory morbidity for patients undergoing noncardiac surgery. J Clin Anesth. 2017;36:1–9.
Zhao BC, Zhuang PP, Lei SH, et al. Pre-operative N-terminal pro-B-type natriuretic peptide for prediction of acute kidney injury after noncardiac surgery: a retrospective cohort study. European Journal of Anaesthesiology EJA. 2021;38(6):591–9.
De Herta S, de Robertisb E, Longroisc D, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assessment and management. Eur Heart J. 2014;35:2383–431.
Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–44.
Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, et al. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney international supplements. 2012;2:1–138.
Parikh CR, Thiessen-Philbrook H. Key concepts and limitations of statistical methods for evaluating biomarkers of kidney disease. J Am Soc Nephrol. 2014;25:1621–9.
Pickering JW, Endre ZH. New metrics for assessing diagnostic potential of candidate biomarkers. Clin J Am Soc Nephrol. 2012;7:1355–64.
Karthikeyan G, Moncur RA, Levine O, Heels-Ansdell D, Chan MT, Alonso-Coello P, et al. Is a pre-operative brain natriuretic peptide or N-terminal pro-B-type natriuretic peptide measurement an independent predictor of adverse cardiovascular outcomes within 30 days of noncardiac surgery? A systematic review and meta-analysis of observational studies. J Am Coll Cardiol. 2009;54:1599–606.Wijeysundera DN.
Pearse RM, Shulman MA, Abbott TEF, Torres E, Ambosta A, et al. Assessment of functional capacity before major non-cardiac surgery: an international, prospective cohort study. Lancet. 2018;391:2631–40.
Rodseth RN, Biccard BM, Le Manach Y, Sessler DI, Lurati Buse GA, Thabane L, et al. The prognostic value of pre-operative and post-operative B-type natriuretic peptides in patients undergoing noncardiac surgery: B-type natriuretic peptide and N-terminal fragment of pro-B-type natriuretic peptide: a systematic review and individual patient data meta-analysis. J Am Coll Cardiol. 2014;63:170–80.
Cardinale D, Colombo A, Sandri MT, Lamantia G, Colombo N, Civelli M, et al. Increased perioperative N-terminal pro-B-type natriuretic peptide levels predict atrial fibrillation after thoracic surgery for lung cancer. Circulation. 2007;115:1339–44.
Cardinale D, Cosentino N, Moltrasio M, Sandri MT, Petrella F, Colombo A, et al. Acute kidney injury after lung cancer surgery: incidence and clinical relevance, predictors, and role of N-terminal pro B-type natriuretic peptide. Lung Cancer. 2018;123:155–9.
Belley-Côté EP, Parikh CR, Shortt CR, Coca SG, Garg AX, Eikelboom JW, et al. Association of cardiac biomarkers with acute kidney injury after cardiac surgery: a multicenter cohort study. J Thorac Cardiovasc Surg. 2016;152:245–51.e4.
Jarai R, Dangas G, Huber K, Xu K, Brodie BR, Witzenbichler B, et al. B-type natriuretic peptide and risk of contrast-induced acute kidney injury in acute ST-segment-elevation myocardial infarction: a substudy from the HORIZONS-AMI trial. Circ Cardiovasc Interv. 2012;5:813–20.
Haines R, Crichton S, Wilson J, Treacher D, Ostermann M. Cardiac biomarkers are associated with maximum stage of acute kidney injury in critically ill patients: a prospective analysis. Crit Care. 2017;21:88.
Naruse H, Ishii J, Takahashi H, Kitagawa F, Nishimura H, Kawai H, et al. Predicting acute kidney injury using urinary liver-type fatty-acid binding protein and serum N-terminal pro-B-type natriuretic peptide levels in patients treated at medical cardiac intensive care units. Crit Care. 2018;22:197.
Patel UD, Garg AX, Krumholz HM, Shlipak MG, Coca SG, Sint K, et al. Preoperative serum brain natriuretic peptide and risk of acute kidney injury after cardiac surgery. Circulation. 2012;125:1347–55.
Nowak A, Breidthardt T, Dejung S, Christ-Crain M, Bingisser R, Drexler B, et al. Natriuretic peptides for early prediction of acute kidney injury in community-acquired pneumonia. Clin Chim Acta. 2013;419:67–72.
Kheterpal S, Tremper KK, Heung M, Rosenberg AL, Englesbe M, Shanks AM, et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology. 2009;110:505–15.
Acknowledgements
Not applicable.
Funding
This work has not been funded by any entity.
Author information
Authors and Affiliations
Contributions
J.W.: Performed data collection and data analysis, wrote the first draft of the paper, and revised the paper. Y.D.: Performed data collection and data analysis and revised the paper. B.Z., K.L.: Designed the study, analysed the data and revised the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study complied with the Declaration of Helsinki and was approved by the Ethics Committee of Southern Medical University Nanfang Hospital without the need for informed consent from the participants (NFEC-2019–081). As this was a retrospective study, all identifying information of patients was removed before analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, J., Dong, Y., Zhao, B. et al. Preoperative NT-proBNP and LVEF for the prediction of acute kidney injury after noncardiac surgery: a single-centre retrospective study. BMC Anesthesiol 22, 196 (2022). https://doi.org/10.1186/s12871-022-01727-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01727-0