Abstract
Background
This article aimed to study the value of brain natriuretic peptide (BNP) and cardiac troponin I(cTnI) for predicting the prognosis in cancer patients with sepsis.
Methods
A cohort of 233 cancer patients with sepsis admitted to our ICU from January 2017 to October 2020 was included in this retrospective study. The data of BNP and cTnI on the first day (d1) and the third day(d3) after entering ICU, blood lactate (Lac), procalcitonin (PCT), Leucocyte and Sequential Organ failure assessment (SOFA) scores within 24 hr of entering ICU, the incidence of septic shock, acute kidney injury(AKI), acute respiratory failure (ARF) or sepsis-induced myocardial dysfunction(SIMD) in ICU, fluid balance in 24 hr and 72 hr after entering ICU, time of mechanical ventilation(MV), length of stay, emergency surgery were collected. According to 28-day mortality, patients were divided into survival group (190 cases) and death group (43 cases). All the above variables were compared.
Results
BNP was an independent predictor for the mortality in these patients (P < 0.05).While cTnI was not. BNP on d3 in 681.5 pg/ml predicted the mortality with a sensitivity of 91.5 % and a specificity of 88.7 %. All patients were divided into the new two groups following the cutoff value of BNP on d3(681.5pg/ml), and the survival curve showed a significant difference with Kaplan-Meier analysis (P < 0.05). BNP had statistical differences between four groups based on the comorbidities(septic shock, AKI, ARF or SIMD), but cTnI was not.
Conclusions
BNP was a great predictor for the prognosis of cancer patients with sepsis, while cTnI was not.
Similar content being viewed by others
Introduction
Sepsis is “a life-threatening condition that arises when the body’s response to infection injures its own tissues” [1]. Although more progress has been made in the treatment for sepsis, it is still one of the common causes of death in critically ill patients worldwide [2]. Early warning and active intervention for sepsis can significantly reduce mortality and improve prognosis [3]. Poor regulation of normal immune responses caused by sepsis can result in a variety of adverse reactions, including multi-system organ dysfunction in several cases [4]. Sepsis induced myocardial dysfunction(SIMD) is common, with an incidence of about 40 %, which usually indicates a significant poor prognosis in sepsis [2,3,4,5].The application of BNP and cTnI in congestive heart failure and acute coronary syndromes has been extensively recognized and accepted [6, 7]. The two cardiac biomarkers for predicting the prognosis of septic patients have also become a hot spot in domestic and foreign research [7,8,9], but the value of them for predicting the prognosis of sepsis is still controversial.
This retrospective study was designed to clarify the differences of BNP and cTnI for predicting the prognosis of cancer patients with sepsis.
Methods
Participants
The study was carried out in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Peking University Cancer Hospital & Institute. Clinical data on 233 cancer patients with sepsis admitted to ICU from January 2017 to October 2020 who met the inclusion criteria were collected retrospectively(315 were screened, and 82 were excluded according to the exclusion criteria).
Inclusion criteria: Patient data were collected according to the 2016 European definition of sepsis and septic shock [1].Patients with sepsis were treated by active cluster treatment according to the guidelines of Surviving sepsis campaign(SSC) [3].
Exclusion criteria: life expectancy is less than 24 hr, acute coronary syndrome, chronic heart disease (such as severe hypertension, heart valve disease or arrhythmia, etc.), chronic liver and kidney insufficiency, cardiogenic or hemorrhagic shock.
Both clinical and biological data were gathered in the following period after entering ICU.
Clinical data: age, gender, Infection category, comorbidities including septic shock, acute kidney injury(AKI), acute respiratory failure (ARF) and sepsis-induced myocardial dysfunction (SIMD) after entering ICU, time of MV, length of stay in ICU ,24 hr and 72 hr fluid balance in ICU, and emergency surgery conditions.
Biological data: lactate, leucocyte and PCT obtained from the blood gas, blood routine and procalcitonin test when patients entered ICU. BNP and cTnI on the first day(d1) and the third day (d3) after entering ICU(The normal value was less than or equal to 100 pg/ml for BNP, less than or equal to 0.05 ng/mL for cTnI).
SOFA scores were recorded to assess the severity of all the patients’s condition within the first 24 hr of admission to the ICU.
Interpretation for some definitions
Sepsis is meant by the loss of control of the body’s inflammatory response to infection leading to life-threatening organ dysfunction. Organ dysfunction is defined as an acute increase in the Sequential Organ Failure Assessment score (SOFA score ≥ 2 points) secondary to infection.
Septic shock is defined as refractory hypotension (patients still need vasopressor drugs to maintain mean arterial pressure ≥ 65mmHg after adequate fluid resuscitation) and blood lactate ≥ 2mmol/l. Patients with sepsis were treated with active cluster treatment according to the sepsis treatment guidelines of Surviving sepsis campaign (SSC) [3].
AKI is meant by any of the following: Increase in serum creatinine(SCr)by 0.3 mg/dL(26.5µmol/L) within 48 h. Increase in SCr to 1.5 times baseline, which is known or presumed to have occurred within the prior 7 days. Urine volume<0.5ml/kg/h for 6 h [10].
ARF is described as acute severe dysfunction of lung ventilation caused by various reasons. Arterial blood oxygen partial pressure (PaO2) is lower than 8 kPa (60mmHg). Or accompanied by carbon dioxide partial pressure (PaCO2) higher than 6.65 kPa (50mmHg).
SIMD is meant by left ventricular ejection fraction (LVEF) less than 50 %. The bedside echocardiogram results were collected within 72 hr of entering ICU [11].
Statistical Analysis
Statistics, Version 26.0 (Armonk, NY: IBM Corp.) was used for statistical analysis. Data were analyzed as the mean ± standard deviation, number(percentage) or median (25th /75th percentile). Unpaired t test and Mann-Whitney U test were used to compare continuous variables and skewed distribution. A χ2 test was used to compare categorical variables. Significantly different variables in univariate analysis were included in COX regression analysis to select the independent risk factors of sepsis. Receiver operating characteristic curve (ROC curve) was used to identify the value of all the independent risk factors for the mortality of cancer patients with sepsis. The patients were divided into the new two groups according to the cut-off value obtained by Youden index in ROC curve, and the difference in survival curve was compared with the Kaplan-Meier method. P < 0.05 was considered statistically significant.
Results
-
1.
According to the 28-day mortality, all cancer patients with sepsis were divided into the survival group and the death group. The baseline data for the two groups were as following (Table 1). The incidence of septic shock, AKI and ARF, the time of MV, 72 hr fluid balance, lactate, BNP and cTnI on d1 and d3, SOFA score in the survival group were significantly different from those in the death group by univariate analysis (P < 0.05).
-
2.
The variables with significant differences in Table 1 were put into the Cox regression analysis. It can be seen that BNP on d3, SOFA score, and 72 hr fluid balance were independent risk factors for mortality of patients (Table 2).
-
3.
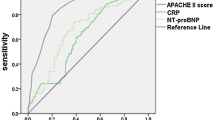
The ROC curve was used to evaluate the predicting ability of the independent risk factors including BNP on d3, SOFA score, and 72 hr fluid balance from Table 2. The area under the ROC curve was 0.91 ± 0.01 (P < 0.01) for BNP on d3, 0.86 ± 0.03(P < 0.01) for SOFA score, 0.84 ± 0.04 (P < 0.01) for 72 hr fluid balance (Fig. 1). BNP on d3 at 681.5 pg/mL predicted mortality with a sensitivity of 91 % and a specificity of 89 %, SOFA score at 7 predicted mortality with a sensitivity of 79 % and a specificity of 81 %, 72 hr fluid balance at 75.9ml/kg predicted mortality with a sensitivity of 81 % and a specificity 77 %. It can be seen that BNP on d3 had the largest area of ROC curve, and it also had the best sensitivity and specificity.
-
4.
According to the cut-off value of BNP on d3(681.5 pg/ml), all patients were divided into two groups (BNP on d3 < 681.5pg/ml or BNP on d3 > 681.5pg/ml), Kaplan-Meier analysis performed on the two groups of patients showed a significant difference in the survival curve (P < 0.05) which means that the greater the BNP on d3 above the cut-off value, the higher the 28-day mortality rate of the patients.(Fig. 2).
.
-
5.
There were also significant differences in the comorbidities (septic shock, AKI, ARF, SIMD) after entering ICU occurred in the two groups of patients (BNP on d3 < 681.5pg/ml or BNP on d3 > 681.5pg/ml) (P < 0.05), which indicated that the higher the BNP of the patients, the more likely to merge with shock, AKI, ARF or SIMD. (Table 3)
-
6.
Differences of BNP and cTnI were compared among the four groups according to the comorbidities (septic shock, AKI, ARF, SIMD). It can be seen that the level of BNP increased significantly (P < 0.05) while cTnI was not in patients with comorbidities (Tables 4, 5, 6 and 7).
-
7.
The correlation between BNP on d3 and 72 hr fluid balance was compared. Both of them had a positive correlation (P < 0.05), but the correlation was extremely weak (r = 0.286) (Fig. 3).
.
Discussion
BNP is a definitive marker in patients with congestive heart failure. BNP is released into the blood when the ventricular wall tension increased[12]. The main mechanism of SIMD is that the heart’s variable myocardial contractility would increase the tension of the ventricular wall and cause ventricular dilatation, which leads to a significant increase in the secretion of BNP[13]. Patients with septic shock often have acute renal injury in the initial stage, and the metabolism of BNP produced in plasma is slowed down[14]. These two factors are the main reason why causing the increase of BNP in patients with sepsis. The main finding of this study was to understand that BNP is an independent risk factor for the prognosis of cancer patients with sepsis, especially the BNP on d3 after entering the ICU at 681.5pg/ml had high diagnostic power and great sensitivity and specificity for the mortality of these patients. The higher the BNP level larger than 681.5pg/ml, the higher the 28-day mortality rate, and the greater the possibility of the comorbidities (septic shock, AKI, ARF, SIMD) occurred. This result is consistent with some domestic and foreign studies [15, 16].
Differences of BNP and cTnI were compared among the four groups according to the comorbidities (septic shock, AKI, ARF, SIMD). It can be seen that the level of BNP increased significantly (P < 0.05) while cTnI was not in patients with comorbidities.
cTnI is the most sensitive and specific marker of myocardial injury. Cardiac hypoperfusion and the application of a large number of vasoactive drugs in patients with sepsis both may cause myocardial injury[17]. The degree of elevated cTnI was significantly related to the severity and mortality of patients with sepsis[18]. However, Some studies also had shown that cTnI has no obvious relationship with mortality of septic patients [19, 20]. This study found that cTnI was significantly different between the survival group and the death group (P < 0.05), but cTnI was not an independent risk factor predicting the mortality in patients with sepsis.
126 underwent random bedside echocardiography (the remaining were not available) among the 233 patients with sepsis in this study. A total of 42 cases developed SIMD, with an incidence rate of 33.3 % (30.6 % in the survival group and 40.9 % in the death group). There was no significant differences in the incidence of SIMD between the two groups (P = 0.26). And also there was no significant difference between the non-SIMD and SIMD groups for cTnI on d1 and d3. This conclusion was consistent with the results of RøSjø who found that the increase of cTnI in patients with sepsis only reflected the damage state of myocardial cells and cannot increase the mortality of sepsis or accurately predict the risk of SIMD [21]. Combining the above multiple studies, It can be observed that the value of cTnI for the prognosis of patients with sepsis is still controversial [17].
This study also found that the SOFA score and 72 hr fluid balance were independent risk factors for mortality in these patients. SOFA score is a reliable indicator to assess the severity of critical ill patients[22, 23]. Its predictive value for the mortality of patients with sepsis has been confirmed by a large number of studies and would not be discussed further here[24, 25]. 72 hr fluid balance was also one of the independent risk factors[26]. The area under the ROC curve was 0.84 ± 0.04 (P < 0.01) for 72 hr fluid balance. 72 hr fluid balance at 75.9ml/kg predicted mortality with a sensitivity of 81 % and a specificity 77 %. It can be seen that 72 hr fluid balance has good predictive value for the mortality of cancer patients with sepsis. In the early treatment of sepsis, in order to optimize organ perfusion, fluid shock therapy should be performed in time. But the continuous positive fluid balance in patients with sepsis in the following periods may indicate a poor prognosis. The European SOAP study in 2006 showed that the cumulative fluid balance within 72 hr is the strongest predictor of mortality of sepsis patients in the ICU, which means that fluid balance is the only changeable risk factor identified in their study [27]. Boyd reported a retrospective study of VASST, which also confirmed the relationship between the cumulative fluid balance after 4 days and the mortality of patients with sepsis [28].
The correlation analysis between BNP on d3 and 72 hr fluid balance showed that the two were positively correlated (P<0.05), but the correlation was extremely weak (r = 0.286). BNP didn’t seem to be a reliable marker of fluid status in septic patients. Similar studies had also shown that BNP was not closely associated with fluid volume and fluid responsiveness in patients with sepsis[29, 30].
Limitations
This study referred to the latest definition of sepsis. Enrollment and grouping of sepsis patients had new standards, and the conclusions were different from previous studies. Dynamic observation data of BNP, cTnI and fluid balance increased the accuracy of the results. This study still had certain limitations. First, the enrolled patients had a short hospital stay in ICU, so most of the BNP and cTnI data were within 3 days of entering ICU. The dynamic observation data were relatively limited, which may influence the judgment of the results to a certain extent. Secondly, not all the patients had undergone bedside echocardiography, so the sample size was reduced. Because of the limited technology of bedside echocardiography, patients diagnosed with SIMD were actually based on left ventricular systolic dysfunction, which would lose some patients with left ventricular diastolic dysfunction or right heart dysfunction. The incidence of SIMD may be smaller. The difference of BNP and cTnI with SIMD, and mortality between SIMD and non-SIMD groups may be biased ultimately. In future, more sample size and more cardiac ultrasound parameters should be added. Prospective studies would be conducted to improve the rigor of the research.
Conclusions
For cancer patients with sepsis, early warning and effective intervention to reduce mortality are still the difficulties in ICU. BNP is a great predictor for evaluating the prognosis of cancer patients with sepsis. While cTnI is still controversial. Early judgment on the prognosis of patients with sepsis still needs to look for more biomarkers to enhance their effectiveness.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICU:
-
Intensive care unit
- BNP:
-
Brain natriuretic peptide
- cTnI:
-
Cardiac troponin I
- d1:
-
The first day
- d3:
-
The third day
- Lac:
-
Lactate
- PCT:
-
Procalcitonin
- SOFA:
-
Sequential Organ failure assessment
- AKI:
-
Acute kidney injury
- ARF:
-
Acute respiratory failure
- SIMD:
-
Sepsis-induced myocardial dysfunction
- MV:
-
Mechanical ventilation
- 72hr:
-
72 hour
- 24hr:
-
24 hour
- SSC:
-
Surviving sepsis campaign
- SCr:
-
Serum creatinine
- PaO2:
-
Arterial blood oxygen partial pressure
- PaCO2:
-
Carbon dioxide partial pressure
- LVEF:
-
Left ventricular ejection fraction
- ROC:
-
Receiver operating characteristic
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche J-D, Coopersmith CM: The third international consensus definitions for sepsis and septic shock (Sepsis-3). Jama 2016, 315(8):801–810.
Vincent J-L, Marshall JC, Ñamendys-Silva SA, François B, Martin-Loeches I, Lipman J, Reinhart K, Antonelli M, Pickkers P, Njimi H. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–6.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, Kumar A, Sevransky JE, Sprung CL, Nunnally ME. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive care medicine. 2017;43(3):304–77.
Association SoCCMCM. Guidelines for the treatment of severe sepsis/septic shock in China (2014). Chin J Intern Med. 2015;54(6):557–81.
Beesley SJ, Weber G, Sarge T, Nikravan S, Grissom CK, Lanspa MJ, Shahul S, Brown SM. Septic cardiomyopathy. Critical care medicine. 2018;46(4):625–34.
Braunwald E. Biomarkers in heart failure. N Engl J Med. 2008;358(20):2148–59.
Altintas Z, Fakanya WM, Tothill IE. Cardiovascular disease detection using bio-sensing techniques. Talanta. 2014;128:177–86.
Raja DC, Mehrotra S, Agrawal A, Singh A, Sawlani KK. Cardiac biomarkers and myocardial dysfunction in septicemia. J Assoc Phys India. 2017;65:14.
Chen F-c, Xu Y-c, Zhang Z-c. Multi-biomarker strategy for prediction of myocardial dysfunction and mortality in sepsis. J Zhejiang University-SCIENCE B. 2020;21(7):537–48.
Palevsky PM, Liu KD, Brophy PD, Chawla LS, Parikh CR, Thakar CV, Tolwani AJ, Waikar SS, Weisbord SD. KDOQI US Commentary on the 2012 KDIGO Clinical Practice Guideline for Acute Kidney Injury. American Journal of Kidney Diseases the Official Journal of the National Kidney Foundation. 2013;61(5):649–72.
L’Heureux M, Sternberg M, Brath L, Turlington J, Kashiouris MG. Sepsis-induced cardiomyopathy: a comprehensive review. Curr Cardiol Rep. 2020;22(5):1–12.
Egom EE. BNP and heart failure: preclinical and clinical trial data. Journal of Cardiovascular Translational Research. 2015;8(3):149–57.
Kandil E, Burack J, Sawas A, Bibawy H, Schwartzman A, Zenilman ME, Bluth MH. B-type natriuretic peptide: a biomarker for the diagnosis and risk stratification of patients with septic shock. Archives of surgery. 2008;143(3):242–6.
Akgul O, Uyarel H, Pusuroglu H, Isiksacan N, Turen S, Erturk M, Surgit O, Celik O, Oner E, Birant A. High BNP level as risk factor for acute kidney injury and predictor of all-cause mortality in STEMI patients. Herz. 2014;39(4):507–14.
Ueda S, Nishio K, Akai Y, Fukushima H, Ueyama T, Kawai Y, Masui K, Yoshioka A, Okuchi K. Prognostic value of increased plasma levels of brain natriuretic peptide in patients with septic shock. Shock. 2006;26(2):134–9.
Zhao H, An Y, Liu F. Prognostic values of B-type natriuretic peptide in severe sepsis and septic shock. Zhongguo wei zhong bing ji jiu yi xue = Chinese critical care medicine = Zhongguo weizhongbing jijiuyixue. 2009;21(5):293–5.
Kim J-S, Kim M, Kim Y-J, Ryoo SM, Sohn CH, Ahn S, Kim WY. Troponin testing for assessing sepsis-induced myocardial dysfunction in patients with septic shock. Journal of clinical medicine. 2019;8(2):239.
Bessière F, Khenifer S, Dubourg J, Durieu I, Lega J-C. Prognostic value of troponins in sepsis: a meta-analysis. Intensive care medicine. 2013;39(7):1181–9.
Zaky A, Gill E, Paul C, Bendjelid K, Treggiari M. Characteristics of sepsis-induced cardiac dysfunction using speckle-tracking echocardiography: a feasibility study. Anaesthesia intensive care. 2016;44(1):65–76.
De Geer L, Engvall J, Oscarsson A. Strain echocardiography in septic shock–a comparison with systolic and diastolic function parameters, cardiac biomarkers and outcome. Crit Care. 2015;19(1):122.
Røsjø H, Varpula M, Hagve T-A, Karlsson S, Ruokonen E, Pettilä V, Omland T, Group FS. Circulating high sensitivity troponin T in severe sepsis and septic shock: distribution, associated factors, and relation to outcome. Intensive care medicine. 2011;37(1):77–85.
Safari S, Shojaee M, Rahmati F, Barartloo A, Hahshemi B, Forouzanfar MM, Mohammadi E. Accuracy of SOFA score in prediction of 30-day outcome of critically ill patients. Turkish journal of emergency medicine. 2016;16(4):146–50.
Fuchs PA, Czech IJ, Krzych ŁJ. Mortality Prediction Using SOFA Score in Critically Ill Surgical and Non-Surgical Patients: Which Parameter Is the Most Valuable? Medicina 2020, 56(6):273.
Chae B-R, Kim Y-J, Lee Y-S. Prognostic accuracy of the sequential organ failure assessment (SOFA) and quick SOFA for mortality in cancer patients with sepsis defined by systemic inflammatory response syndrome (SIRS). Support Care Cancer. 2020;28(2):653–9.
Rhee C, Zhang Z, Kadri SS, Murphy DJ, Martin GS, Overton E, Seymour CW, Angus DC, Dantes R, Epstein L. Sepsis surveillance using adult sepsis events simplified eSOFA criteria versus sepsis-3 SOFA criteria. Critical care medicine. 2019;47(3):307.
Acheampong A, Vincent JL. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care. 2015;19(1):1–7.
Vincent J-L, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall J-R, Payen D. Sepsis in European intensive care units: results of the SOAP study. Critical care medicine. 2006;34(2):344–53.
Boyd JH, Forbes J, Nakada T-a, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Critical care medicine. 2011;39(2):259–65.
Zhang Z, Zhang Z, Xue Y, Xu X, Ni H. Prognostic value of B-type natriuretic peptide (BNP) and its potential role in guiding fluid therapy in critically ill septic patients. Scand J Trauma Resusc Emerg Med. 2012;20(1):86.
Takahashi EA, Moran SE, Hayashi MS, Inouye DS, Takanishi DM Jr, Yu M. Brain-type natriuretic peptide and right ventricular end-diastolic volume index measurements are imprecise estimates of circulating blood volume in critically ill subjects. Journal of Trauma Acute Care Surgery. 2013;75(5):813–8.
Acknowledgements
The authors thank Elise for English language revision.
Funding
This work was supported by the Capital Health Research and Development of Special Funds (approval No. :2020-1-1021), Beijing Municipal Administration of Hospital’s Ascent Plan (approval No. : DFL20181104), Beijing Municipal Administration of Hospitals’ Youth Programme(approval No. QML20181104) and B. Braun Anaesthesia Science Research Foundation (BBFD-2015-16). Labor services for the data collation, analysis and post-publication layout fees of the study are provided by the above funds.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: Y Yang, Hz Wang; (II) Administrative support: Jh Leng, Cy Hao; (III) Provision of study materials or patients: Y Yang, Xy Tian; (IV) Collection and assembly of data: Y Yang, Xy Tian; (V)Data analysis and interpretation: Y Yong, Hz Wang; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was in line with the Helsinki Declaration and approved by the Peking University Cancer Hospital Ethics Committee. Written informed consent was obtained from the patients for their anonymized information to be published in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Y., Leng, J., Tian, X. et al. Brain natriuretic peptide and cardiac troponin I for prediction of the prognosis in cancer patients with sepsis. BMC Anesthesiol 21, 159 (2021). https://doi.org/10.1186/s12871-021-01384-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-021-01384-9