Abstract
Background
A fluid warmer can prevent hypothermia during the perioperative period. This study evaluated the heating capabilities of Hotline and Barkey S-line under different flow rates and initial fluid temperatures, as well as after the extension line installation.
Methods
We measured the temperature of a 0.9% sodium chloride solution at the fluid warmer outlet (TProx) and the extension line end (TDistal) with three different initial fluid temperatures (room, warm, and cold) and two flow rates (250 ml/hr and 100 mL/hr).
Results
At a 250 ml/hr flow rate, the TProx and TDistal values were observed to be higher in Hotline than in S-line when using room-temperature or cold fluid. Administering of the warm fluid at the same flow rate significantly increased the TProx and TDistal values in S-line more than the cold and room-temperature fluids. At flow rates of 100 ml/hr, TDistal values were significantly lower than TProx values in both devices regardless of the initial fluid temperature.
Conclusions
Hotline outperformed S-line for warming fluids at a high flow rate with cold or room-temperature fluids. Administering warm fluid in S-line prevented a decrease in the fluid temperature at a high flow rate. However, at a low flow rate, the fluid temperature significantly decreased in both devices after passing through an extension line.
Similar content being viewed by others
Background
Inadvertent perioperative hypothermia commonly occurs in patients undergoing surgery on account of a cold operating room, anesthetic agents that weaken thermoregulatory control, and administration of un-warmed fluid [1,2,3,4,5,6,7,8]. Even mild hypothermia, defined as a core body temperature ranging from 34 to 36 °C, is associated with complications, such as an increased need for a blood transfusion, increased length of hospitalization, a higher incidence of postoperative myocardial infarction, and the risk of developing a surgical wound infection [7,8,9,10]. Preventing perioperative hypothermia is therefore critical.
It is recommended that physicians assess the risk factors associated with perioperative hypothermia to reduce hypothermia-related complications [3, 11]. After assessing these risk factors, physicians should employ interventions that are appropriately designed for the specific patient population and type of operation [1,2,3, 10]. The use of cold intravenous fluids is one of the most potentially modifiable risk factors [5, 12]. The National Institute for Health and Care Excellence (NICE) published clinical guidelines in 2008 that support the use of intravenous fluid warmers to prevent perioperative hypothermia [13]. Using such a device to warm intravenous fluids before administering it to the patient has been shown to prevent inadvertent hypothermia [4, 5, 12]. However, there are various conditions during fluid administration that must be considered, such as the fluid warmer type, flow rate, fluid temperature, and the IV line length, because the conditions may affect the actual temperature of the administered fluid. Therefore, it is critical to investigate the performance of a fluid warmer in different circumstances.
Numerous commercially available fluid warmers, such as Ranger, ThermoSens, Mega Acer Kit, FT800, and Hotline HL-90, have been investigated under different flow rates and room temperatures [12, 14,15,16]. However, previous studies mainly focused on changing the flow rate [12, 14, 15]. To determine the clinical effectiveness, various clinical factors such as the initial fluid temperature and the use of extension lines should also be considered.
The purpose of this study was to evaluate the fluid heating capabilities of Barkey S-line and Hotline HL-90 according to different flow rates, fluid temperatures, and the presence of an extension line.
Methods
This study was performed in the designated spot next to the nursing station in the post-anesthesia care unit (PACU). The PACU room temperature was maintained at 23 °C, and the humidity level was maintained at approximately 20%. Normal saline fluid (0.9% sodium chloride solution, CJ, Seoul, Republic of Korea) was used for all the experiments in this study. The fluid temperature was measured using a two-channel thermometer (ThermaQ; ThermoWorks, London, UK). For Barkey S-line (Barkey GmbH & Co. KG, Leopoldshöhe, Germany), the operating temperature was maintained at 39.5 °C throughout the experiments. A standard infusion set was inserted in the 1.5-m heating profile of S-line according to the manufacturer instructions. For Hotline HL-90 (Smiths Medical, Minneapolis, MN), the operating temperature was set to 40 °C. The REF L-70 disposable tubing system (length 2.4 m, volume load 20 ml; Level 1 Technologies Inc., MA, USA) was installed according to the manufacturer instructions.
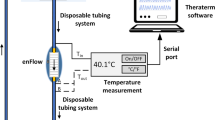
We evaluated the efficacy of the two fluid warmers under several conditions. Three different conditions were set for the initial fluid temperature: room temperature (22–23 °C), cold (9–10 °C), and warm (46–47 °C). The normal saline solutions were respectively maintained for 12 h in the operating room, in a refrigerator, and in a heating cabinet for each of the three different conditions. Two distinct flow rates were tested in this study: 100 ml/hr and 250 ml/hr. The roller clamp was fully open, and the flow rate was adjusted using a micro-flow regulator (I.V. Flow Control Line, Insung Medical Co., Seoul, Republic of Korea) attached to the infusion set at a flow rate of 100 or 250 ml/hr. The regulator tolerance ranged from − 10–20% according to the manufacturer instructions. The height of the infusion bag was the same in all experiments (1.8 m). One unit of a non-insulated extension set (DEHP-free Extension Plus, SBD Medical, Republic of Korea), which was 90 cm in length, was connected to the fluid warmer outlet. The fluid temperature was measured at two points, first at the fluid warmer outlet (TProx) and then at the end of the non-insulated extension line (TDistal). After starting each trial, the temperatures at the two positions (TProx and TDistal) were recorded every minute until the end of the trial (Fig. 1).
The figure shows an overview of the experimental setup. 0.9% NaCl solution is warmed as it travels down the fluid warmer. After fluid exits the warmer, it goes further down through the non-insulated extension line. The temperatures at the outlet of the warmer (TProx) and the outlet of the extension line (TDistal) were measured using thermometers. a and b in the left and right show the setups for Hotline and S-line, respectively
TProx and TDistal were carefully evaluated for the presence of a plateau in each trial. The plateau in each trial was defined as the time point at which the measured temperatures were the most stable without a noted fluctuation for 3 min. In each trial, only the TProx and TDistal values from the middle time point of the plateau were used for the subsequent statistical analysis. Five trials were performed for an individual experimental condition to obtain five data points for TProx and TDistal, respectively.
Statistical analysis was performed using SPSS v.20.0 for Windows (IBM SPSS, Inc., Armonk, NY) and R software version 3.4.4 (R Foundation for Statistical Computing, Austria). A data chart was produced using Microsoft Excel 2007. All fluid temperatures were reported as a median (interquartile [IQR] range). The Wilcoxon signed-rank test was used to test for a statistical difference between TProx and TDistal values. The Hodges–Lehmann estimator was utilized to create the 95% confidence interval for the median difference between TProx and TDistal. The Mann–Whitney U test was employed to compare TProx or TDistal values under different flow rates using the same fluid warmer or between Hotline and S-line at the same flow rate. The bootstrap method was applied to form the 95% confidence interval for the analyses performed using the Mann–Whitney U test. Statistical significance was defined as a p-value < 0.05.
Results
Room‐temperature fluid
The room-temperature fluid was maintained at 21–23 °C. TProx was higher in Hotline (38.7 [38.7–38.8]°C) than in S-line (28.2 [27.6–28.4]°C) based on the median difference of 10.5 °C (95% CI 9.6–12.3) at the flow rate of 250 ml/hr. At the flow rate of 100 ml/hr, the TProx value was higher in Hotline (40.3 [40.1–40.4]°C) than S-line (38.7 [38.6–38.7]°C) according to the median difference of 1.6 °C (95% CI 1.4–2.1. TDistal measured higher in Hotline (37.6 [37.6–37.9]°C) than in S-line (27.8 [27.0-27.9]°C) based on the median difference of 9.8 °C (95% CI 7.6–11.5) at the flow rate of 250 ml/hr. However, the TDistal values were not significantly different between Hotline (25.6 [25.3–26.0]°C) and S-line (23.4 [23.4–23.5]°C) at 100 ml/hr (Fig. 2).
The figure illustrates the measured fluid temperatures using boxplots and line graphs. The red line and blue line connect the data from Hotline and S-line respectively. Boxes indicate the interquartile range, the bold horizontal lines in the box are the median values, and the whiskers are the range. Outliers are displayed as dots. a room-temperature fluid at 250 ml/hr, b cold fluid at 250 ml/hr, c warm fluid at 250 ml/hr, d room-temperature fluid at 100 ml/hr, e cold fluid at 100 ml/hr, f warm fluid at 100 ml/hr
TProx in Hotline was slightly higher at 100 ml/hr than at 250 ml/hr based on the median difference of 1.6 °C (95% CI 1.3–1.9). However, TProx in S-line was much higher at 100 ml/hr than at 250 ml/hr based on the median difference of 10.5 °C (95% CI 9.6–12.3).
Furthermore, TDistal in Hotline was higher at 250 ml/hr than at 100 ml/hr by 12.0 °C (95% CI 9.8–14.2). TDistal in S-line was higher at 250 ml/hr than at 100 ml/hr by 4.4 °C (95% CI 2.6–5.3). The TDistal values were lower at 100 ml/hr than at 250 ml/hr. In addition, TProx was higher than TDistal in both devices regardless of the flow rate. However, the differences were more substantial at 100 ml/hr. At a flow rate of 250 ml/hr, the median differences between TProx and TDistal were 1.1 °C (95% CI 0.9–2.2) in Hotline and 0.4 °C (95% CI 0.3–0.6) in S-line. At 100 ml/hr, the median differences were 14.7 °C (95% CI 14.3–16.7) in Hotline and 15.1 °C (95% CI 13.9–16.0) in S-line.
Cold fluid
The initial temperature of the starting solution was maintained at 9–11 °C in this group. TProx was higher in Hotline (37.2 [36.3–37.4]°C) than in S-line (18.2 [17.6–19.5]°C) by the median difference of 19.0 °C (95% CI 16.7–20.2) at 250 ml/hr. However, the difference between Hotline (40.0 [39.8–40.0]°C) and S-line (38.6 [38.5–38.6]°C) was 1.4 °C (95% CI 0.3–4.3) at 100 ml/hr. TDistal at 250 ml/hr was also higher in Hotline (36.2 [35.6–36.3]°C) than in S-line (19.1 [18.5–20.0]°C) based on the median difference of 17.1 °C (95% CI 15.4–18.2). However, the TDistal values from Hotline (23.5 [23.3–24.1]°C) and S-line (24.5 [24.1–24.7]°C) were not statistically different at 100 ml/hr (Fig. 2).
TProx measured in Hotline was slightly higher at 100 ml/hr than at 250 ml/hr by 2.8 °C (95% CI 1.7–3.8). In S-line, the TProx value was significantly higher at 100 ml/hr than at 250 ml/hr by 20.4 °C (95% CI 17.5–21.4). For TDistal in Hotline, the temperature at 250 ml/hr was higher than at 100 ml/hr, and the median difference was 12.7 °C (95% CI 11.4–13.6). In contrast, TDistal at 100 ml/hr was higher than at 250 ml/hr in S-line, and the median difference was 5.4 °C (95% CI 4.0–6.4). In both devices, the TDistal values at 100 ml/hr were similar to the ambient temperature. The TProx was higher than TDistal in both devices regardless of the flow rate. The only exception was observed in S-line at 250 ml/hr; TProx is 18.2 °C and TDistal is 19.1 °C. The difference between TProx and TDistal was greater at 100 ml/hr than at 250 ml/hr. At 250 ml/hr, the median differences between TProx and TDistal were 0.9 °C (95% CI 0.6–1.2) in Hotline and 0.7 °C (95% CI 0.5–0.9) in S-line. At 100 ml/hr, the median differences were 16.3 °C (95% CI 15.8–16.6) in Hotline and 13.9 °C (95% CI 11.2–14.6) in S-line. At 100 ml/hr, the extension line reversed most of the warming and substantially cooled the fluid as it traveled from TProx to TDistal.
Warm fluid
The initial fluid temperature was maintained at 46–49 °C in the warm temperature group. In this temperature group, the temperature of the initial fluid was higher than the operating temperatures of the fluid warmers themselves. The TProx value at 250 ml/hr in S-line (44.8 [44.7–45.4]°C) was higher than in Hotline (42.1 [42.1–42.1]°C) according to the median difference of 2.7 °C (95% CI 2.4–3.8). At 100 ml/hr, the TProx value was higher in Hotline (40.5 [40.5–40.5]°C) than S-line (37.8 [37.8–37.9]°C) according to the median difference of 2.7 °C (95% CI 1.6–3.7). TDistal in S-line (43.9 [43.5–44.2]°C) at 250 ml/hr was higher than in Hotline (41.2 [41.0-41.2]°C) according to the median difference of 2.7 °C (95% CI 2.2–3.2). At 100 ml/hr, no statistical difference existed between the TDistal values in Hotline (27.6 [27.4–27.9]°C) and S-line (26.6 [26.5–26.8]°C) (Fig. 2).
In Hotline, the TProx value was higher at 250 ml/hr than at 100 ml/hr, and the median difference was 1.6 °C (95% CI 1.5–1.7). For the TDistal value, the temperature measured at 250 ml/hr was again higher, and the median difference was 13.6 °C (95% CI 13.1–14.9). Similarly, the TProx value in S-line was higher at 250 ml/hr than at 100 ml/hr; the median difference was 7.0 °C (95% CI 5.9–8.1). For the TDistal value, the measurement at 250 ml/hr was higher than at 100 ml/hr based on the median difference of 17.3 °C (95% CI 16.7–18.6). TProx was higher than TDistal at the two flow rates in both Hotline and S-line. A flow rate of 100 ml/hr produced larger differences between TProx and TDistal. At 250 ml/hr, the median differences between TProx and TDistal were 1.0 °C (95% CI 0.9–1.1) in Hotline and 1.2 °C (95% CI 0.8–1.5) in S-line. At 100 ml/hr, the median differences were 12.9 °C (95% CI 12.5–14.2) in Hotline and 11.3 °C (95% CI 11.1–12.1) in S-line. The slower flow rate correlated with a more substantial difference in the median values.
Discussion
This study showed that Hotline was superior to S-line for warming fluids when using room-temperature or cold saline at a high flow rate. However, at a low flow rate, the fluid temperature significantly decreased in both devices after passing through an extension line.
The difference in heating capacity between the two devices was likely due to the differences in their respective heating mechanisms, i.e., a coaxial circulating water bath (Hotline) versus a dry heating profile (S-line). The dry-heating system is expected to incur greater heat losses on account of the exposed portion of the extension line in ambient temperature. Thus, the Hotline coaxial warming system is apparently more effective than S-line in preventing hypothermia during rapid fluid administration. When administrating fluid rapidly, pre-warming fluid appears to be effective in maintaining fluid temperature warm especially in S-line. However, it would be important to check the warming temperature beforehand to avoid getting too hot fluid.
At 100 ml/hr, changing the initial temperature affected the TProx less in both Hotline and S-line. The slow flow rate would have provided sufficient time for both fluid warmers to affect the fluid temperatures. However, Tdistal of the warm fluid seem to be slightly higher than those of the room-temperature or cold fluids at 100 ml/hr in both Hotline and S-line. This suggests that using pre-warmed fluid may have some role in maintaining fluid temperature even at the low flow rate when the extension line is used. Warm fluid could have influenced TDistal through heating up the tube in which the fluid traveled down, however, the exact mechanism behind this finding remains to be further investigated.
There are several studies evaluating the performance of fluid warmers in literature [4, 12, 15, 16]. The previous studies produced detailed analyses on effect of changing one or two variables on the final fluid temperature among different fluid warmers. For example, the studies were descriptive of the effect of changing the flow rate or the initial fluid temperature. The current study has a strength that it analyzed how extension line, flow rate and initial fluid temperature interact to influence the final fluid temperature and presented comprehensive and clinically relevant performance profiles of Hotline and S-line.
It is clinically important to determine whether warmed fluids can be delivered to the patient without heat loss as they pass through a non-insulated extension line. Interestingly, in this study, a statistically significant change in fluid temperature was observed after the extension line in every experimental condition regardless of the fluid warmer type, initial fluid temperature, or flow rate. The change in fluid temperature was more pronounced at the low flow rate than at the high one. The fluid lost a significant amount of heat as it traveled an additional 90 cm at a rate of 100 ml/hr. This finding warrants the utilization of additional measures for hypothermia prevention when using an extension at the low flow rate, especially when administering fluids to patients with a high risk of developing hypothermia such as neonatal and older patients [17]. Furthermore, it is essential to minimize heat loss as the fluid travels down the extension line, which can be achieved by an extension line innovation or by applying supplemental measures against hypothermia.
Several limitations of this study should be noted. In an actual clinical setting, the fluid administration rate, initial fluid temperature, and extension line length may differ from the conditions used in this study. For example, during rapid fluid resuscitation, the infusion rate can be as high as 60 to 80 mL/kg per hour [18]. Also, in this study, the fluid temperature in the warm temperature group was greater than 45 °C, which can be problematic because the proteins in red blood cells can degenerate at a temperature higher than 45 °C [19]. Moreover, precautionary measures should be taken against preparing fluids that are excessively hot for clinical practice. Finally, extension lines longer than 90 cm can be employed in certain clinical scenarios. Longer extension lines could affect the fluid temperature more markedly than the line length employed in this study.
Conclusions
In summary, Hotline outperformed S-line for warming fluids at a high flow rate with cold or room-temperature fluids. Administering warm fluid in S-line prevented a decrease in the fluid temperature at a high flow rate. Finally, using an extension line can reduce the final fluid temperature delivered to the patient at a low flow rate in both devices.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TProx :
-
Temperature at the fluid warmer point
- TDistal :
-
Temperature at the extension line point
- PACU:
-
Post-anesthesia care unit
References
Diaz M, Becker DE. Thermoregulation: physiological and clinical considerations during sedation and general anesthesia. Anesth Prog. 2010;57(1):25–32. quiz 33 – 24.
Matika R, Ibrahim M, Patwardhan A. The importance of body temperature: An anesthesiologist’s perspective. Temperature (Austin). 2017;4(1):9–12.
Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008;109(2):318–38.
Tansey EA, Johnson CD. Recent advances in thermoregulation. Adv Physiol Educ. 2015;39(3):139–48.
Wax DB, Tyson W, Smith N. Avoidance of Inadvertent Hypothermia With a Fluid-Warming/Infusion System. J Cardiothorac Vasc Anesth. 2018;32(5):e4–5.
Moola S, Lockwood C. Effectiveness of strategies for the management and/or prevention of hypothermia within the adult perioperative environment. Int J Evid Based Healthc. 2011;9(4):337–45.
Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC Jr. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery. 2014;156(5):1245–52.
Flores-Maldonado A, Medina-Escobedo CE, Rios-Rodriguez HM, Fernandez-Dominguez R. Mild perioperative hypothermia and the risk of wound infection. Arch Med Res. 2001;32(3):227–31.
Mahoney CB, Odom J. Maintaining intraoperative normothermia: a meta-analysis of outcomes with costs. AANA J. 1999;67(2):155–63.
Tsuei BJ, Kearney PA. Hypothermia in the trauma patient. Injury. 2004;35(1):7–15.
Moran DS, Mendal L. Core temperature measurement: methods and current insights. Sports Med. 2002;32(14):879–85.
Zoremba N, Bruells C, Rossaint R, Breuer T. Heating capabilities of small fluid warming systems. BMC Anesthesiol. 2018;18(1):98.
National Institute for Health and Care Excellence. (2008) Hypothermia: prevention and management in adults having surgery. https://www.nice.org.uk/guidance/cg65. Accessed 23 March 2020.
Xu X, Lian C, Liu Y, Ding H, Lu Y, ShangGuan W. Warming efficacy of Ranger and FT2800 fluid warmer under different room temperatures and flow rates. J Clin Monit Comput. 2020;34(5):1105–10.
Thongsukh V, Kositratana C, Jandonpai A. Effect of Fluid Flow Rate on Efficacy of Fluid Warmer: An In Vitro Experimental Study. Anesthesiol Res Pract. 2018;2018:4.
Kim DJ, Kim SH, So KY, An TH. Mega Acer Kit(R) is more effective for warming the intravenous fluid than Ranger and ThermoSens(R) at 440 ml/h of infusion rate: an experimental performance study. Korean J Anesthesiol. 2017;70(4):456–61.
Macario A, Dexter F. What are the most important risk factors for a patient’s developing intraoperative hypothermia? Anesth Analg. 2002;94(1):215–20. table of contents.
Santry HP, Alam HB. Fluid resuscitation: past, present, and the future. Shock. 2010;33(3):229–41.
Gershfeld NL, Murayama M. Thermal instability of red blood cell membrane bilayers: temperature dependence of hemolysis. J Membr Biol. 1988;101(1):67–72.
Acknowledgements
Not applicable.
Funding
Support was provided solely from departmental resources of the Department of Anesthesiology and Pain Medicine, Seoul National University Hospital.
Author information
Authors and Affiliations
Contributions
HK and TKK collected and analyzed the study data. SY and J-TK designed the study and interpreted the study data. HK and TKK were the major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hosu Kim and Tae Kyong Kim contributed equally as the first authors of this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, H., Kim, T.K., Yoo, S. et al. Influence of flow rate, fluid temperature, and extension line on Hotline and S-line heating capability: an in vitro study. BMC Anesthesiol 21, 1 (2021). https://doi.org/10.1186/s12871-020-01225-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-020-01225-1