Abstract
Background
Enteroccocus spp. are human opportunistic pathogens causing a variety of serious and life-threating infections in humans, including urinary tract infection, endocarditis, skin infection and bacteraemia. Farm animals and direct contact with them are important sources of Enterococcus faecalis (EFA) and Enterococcus faecium (EFM) infections among farmers, veterinarians and individuals working in breeding farms and abattoirs. The spread of antibiotic-resistant strains is one of the most serious public health concerns, as clinicians will be left without therapeutic options for the management of enterococcal infections. The aim of the study was to evaluate the occurrence and antimicrobial susceptibility of EFA and EFM strains isolated from a pig farm environment and to determine the biofilm formation ability of identified Enterococcus spp. strains.
Results
A total numer of 160 enterococcal isolates were obtained from 475 samples collected in total (33.7%). Among them, 110 of genetically different strains were identified and classified into EFA (82; 74.5%) and EFM (28; 25.5%). Genetic similarity analysis revealed the presence of 7 and 1 clusters among the EFA and EFM strains, respectively. The highest percentage of EFA strains (16; 19.5%) was resistant to high concentrations of gentamicin. Among the EFM strains, the most frequent strains were resistant to ampicillin and high concentrations of gentamicin (5 each; 17.9%). Six (7.3%) EFA and 4 (14.3%) EFM strains showed vancomycin resistance (VRE - Vancomycin-Resistant Enterococcus). Linezolid resistance was found in 2 strains of each species. The multiplex PCR analysis was performed to identify the vancomycin resistant enterococci. vanB, vanA and vanD genotypes were detected in 4, 1 and 1 EFA strains, respectively. Four EFA VRE-strains in total, 2 with the vanA and 2 with the vanB genotypes, were identified. The biofilm analysis revealed that all vancomycin-resistant E. faecalis and E. faecium strains demonstrated a higher biofilm-forming capacity, as compared to the susceptible strains. The lowest cell count (5.31 log CFU / cm2) was reisolated from the biofilm produced by the vancomycin-sensitive strain EFM 2. The highest level of re-isolated cells was observed for VRE EFA 25 and VRE EFM 7 strains, for which the number was 7 log CFU / cm2 and 6.75 log CFU / cm2, respectively.
Conclusions
The irrational use of antibiotics in agriculture and veterinary practice is considered to be one of the key reasons for the rapid spread of antibiotic resistance among microorganisms. Owing to the fact that piggery environment can be a reservoir of antimicrobial resistance and transmission route of antimicrobial resistance genes from commensal zoonotic bacteria to clinical strains, it is of a great importance to public health to monitor trends in this biological phenomenon.
Similar content being viewed by others
Introduction
Enterococcus spp. is a genus of Gram-positive, non-sporulating cocci, commonly found in natural environments (i.e. soil, water, plants), food products and in the digestive tract of humans and farmed animals [1,2,3]. Despite the fact that species comprising the gut microbiome are generally considered commensals, with an average number of 103 to 107 CFU in 1 g of faeces, some Enterococcus spp. are defined as potentially opportunistic pathogens causing life-threatening infections, which mainly affect hospitalized patients [4]. Transmission of enterococci to humans may also involve direct contact with animals and working in their environment. Therefore, individuals such as farmers, veterinarians and employees of breeding farms and slaughterhouses may be at higher risk of Enterococcus spp. infection and colonization. The species E. faecalis and E. faecium, most frequently isolated from humans, can cause urinary tract infections, skin infections (including burn and operative wounds) and infective endocarditis. These strains may be also responsible for sepsis and inflammation, e.g. in the cerebrospinal fluid [1, 5, 6]. In pigs, enterococci can cause serious infections, including sepsis preceded by high fever, rash and muscle flaccidity [6, 9]. In addition to E. faecium and E. faecalis, other species have been isolated from farm animals, including E. hirae, E. durans, E. cecorum, E. casseliflavus, E. gallinarum and E. avium, [2, 3, 6,7,8].
The presence of enterococci in the pig farm milieu has been repeatedly confirmed by isolating them from animal skin surface, faeces, feed and bedding as well as from various equipment for livestock handling [8, 10, 11]. These bacteria were also present in dust samples collected from the air in breeding pig facilities [12].
The risks associated with the presence of enterococci in the milieu of animal husbandry and livestock farming are not limited solely to their pathogenic potential. In comparison to other microorganisms of intestinal origin, enterococci demonstrate a relatively high resistance and adaptability to chemical and environmental stressors. As a consequence, they can adapt and survive under harsh conditions [2, 4, 13]. Enhanced resilience and survival in hostile environments is also attributed to their ability to form biofilms. This results in a reduced disinfection efficiency of surfaces colonized by the bacteria and consequently increased risk of potential infections [4, 14]. Nonetheless, expanding antibiotic resistance of enterococci is nowadays the greatest threat to human health worldwide.
Irrational use (overuse or misuse) of antibiotics in clinical medicine is the major factor contributing to the emergence of antibiotic-resistant bacterial strains in the environment. The routine application of antibiotics for growth promotion and bacterial infection prevention or control in livestock farming has also a great impact on this microbiological phenomenon. Administration of antibiotics in drinking water or feed for farm animals, despite the legitimacy of their use, results in the tissue-fluid penetration of these substances and consequently the deposition of their residues in meat and other raw materials of animal origin [11, 14,15,16]. Notably, there is evidence for a positive correlation between antibiotic administration and the occurence of antibiotic-resistant Entreococcus spp. strains [17].
Enterococcus spp. exhibit a high-level resistance to some classes of antibiotics, e.g. cephalosporins, and low susceptibility to penicillin. A low intrinsic sensitivity to penicillins is attributed particularly to E. faecium [16, 18, 19]. The rapid development of resistance mechanisms by enterococci is a result of a high mutation rate and a specific location of genes in mobile genetic elements (MGE) which are responsible for intracellular and intercellular DNA mobility [15, 16]. These features led to a gradual reduction in the sensitivity of these bacteria to other classes of antibiotics (β-lactams, aminoglycosides, tetracyclines, quinolones, macrolides, streptogramins and chloramphenicol) and the emergence of multi-drug resistant (MDR) strains. In response to the decreasing effectiveness of antibiotics used in established therapies, a natural and rational trend has emerged to test other antibiotics [3, 6, 16]. Satisfactory results in the treatment of infections caused by enterococci have been obtained for glycopeptides, in particular vancomycin. Unfortunately, starting from the 1980s, an increasing number of clinical enterococci strains with resistance to this antibiotic were reported. Currently, vancomycin-resistant enterococci (VRE) are considered to be one of the most important health-care associated (HA) multidrug-resistant pathogens. The rate of their occurrence in European countries and the United States shows an upward trend [5, 20]. Among the nine phenotypes of vancomycin-resistant enterococci strains (VanA, VanB, VanC, VanD, VanE, VanG, VanL, VanM, VanN), the VanA phenotype is dominant in most European countries and the United States [19]. The vanA gene cluster is often found in plasmids, which increases the risk of acquiring resistance to vancomycin and facilitates the dissemination of this trait among strains inhabiting a given environment [21].
The spread of VRE and MDR strains in the animal production environment may be due to the contact with animals carrying the bacteria and consumption or handling of contaminated food. However, transmission of antibiotic resistance from animals to humans poses a major global threat of growing concern about human and environment health. The process of horizontal transfer of drug resistance genes between bacteria can take place in any environment, including the gut of the host, and may involve both susceptible commensal enterococcal strains and pathogens such as Listeria spp. and Staphylococcus aureus [2, 15, 22].
Given the increase in the number of nosocomial infections caused by antibiotic-resistant enterococcal strains and the resulting serious health consequences, monitoring of their occurrence and antimicrobial resistance in the animal production environment is fully justified and essential to prevent the development of resistance. The aim of this study was to (a) assess the prevalence of E. faecalis and E. faecium in the environment of an industrial pig farm, (b) determine their drug susceptibility profiles, (c) to detect vancomycin resistant strains by phenotypic and genotypic methods and (d) the assessement of biofilom formation on stainless steel coupons using quantitative method.
Results
From 475 samples collected, 121 (25.5%) were E. faecalis-positive and 39 (8.2%) were E. faecium-positive (Table 1). The greatest number of isolates, both E. faecalis (34; 28.1%) and E. faecium (11; 28.2%), were obtained from the weaned pigs sector. Irrespective of the sampling place, the highest number of positive samples was found in animal faeces (Table 1).
Analysis of genetic similarity
Based on the analysis of genetic similarity, 82 and 28 genetically different strains of E. faecalis and E. faecium, respectively, were identified in the analyzed material (Figs. 1 and 2). Some isolates were genetically identical. For E. faecalis and E. faecium, 19 and 7 strains, respectively, were represented by more than one isolate (Figs. 1 and 2). All genetically identical isolates belonging to a given strain were obtained from samples taken from the same production sector. For the cut-off at a level of 80%, 1 cluster (C4 EFA) containing 7 strains, 1 cluster (C5 EFA) containing 5 strains, 1 cluster (C1 EFM) containing 4 strains, 1 cluster (C2 EFA) containing 3 strains and 4 clusters (C1 EFA, C3 EFA, C6 EFA, C7 EFA) containing 2 strains were found (Table 2).
Analysis of antibiotic resistance
The results from the analysis of the resistance of the isolated strains to antibiotics are presented in Fig. 3. In the studied population, all strains of both E. faecalis and E. faecium showed sensitivity to tigecycline. The highest percentage of E. faecalis strains (19.5%) was resistant to gentamicin (HLGR phenotype), which was a statistically significant difference as compared to other phenotypes, followed by strains resistant to streptomycin (9.8%) and imipenem (8.5%). Moreover, among strains sensitive to imipenem and ampicillin, 4.9% and 3.7% of isolates, respectively, were categorised as “susceptible, increased exposure” (formerly “intermediate”) to these antibiotics. In turn, E. faecium strains showed the highest resistance to gentamicin (HLGR phenotype, 17.9%), ampicillin (17.9%) and vancomycin (14.3%). The observed differences were statistically significant when compared to other drugs tested. Similar to E. faecalis, some E. faecium strains were categorised as “susceptible, increased exposure” to ampicillin and imipenem (7.1% each). High level of resistance to streptomycin (HLSR phenotype) was present in 9.8% and 10.7% of E. faecalis and E. faecium strains, respectively. In addition, 6.1% of E. faecalis strains and 14.3% of E. faecium strains showed vancomycin resistance. The number of teicoplanin insensitive strains was lower than VREs and was 2.4% and 7.1%, respectively. Moreover, we found 2 strains of each species resistant to linezolid. The differences in the frequency of resistance to linezolid, ampicillin, fluoroquinolones, glycopeptides and kanamycin between the EFM and EFA strains were statistically significant.
Proportion of antibiotic resistance-susceptibility profiles of E. faecium and E. faecalis strains isolated in the study (KMN—kanamycin, NFE—nitrofurantoin, QDF—quinupristin-dalfopristin, TGC—tigecycline, LIN—linezolid, VAN—vancomycin, TEC—teicoplanin, ST—streptomycin, GN—gentamycin, NXN—norfloxacin, LVX—levofoxacin, CIP—ciprofloxacin, IMP—imipenem, AMP—ampicillin), a,b,c,…—values marked with different letters differ statistically significant
For all strains found to be vancomycin and teicoplanin resistant (according to determined MIC values), the presence of the van gene was confirmed by the multiplexPCR method. The vanB gene was detected in one E. faecalis strain which showed the sensitivity to vancomycin (MIC = 2 mg/L). The screening analysis for vancomycin resistance genes revealed that the vanB genotype was dominant in the E. faecalis population, occurring in 4 strains (4.9%). Moreover, one EFA strain (1.2%) showing both the vanA and vanD genotypes was isolated. In the case of E. faecium, two strains (7.1% each) demonstarted the vanA and vanB genotypes. In total, 26 drug susceptibility profiles were distinguished, of which 18 were found in E. faecalis and 11 in E. faecium (Table 3). The profile A, characterized by sensitivity to all tested antibiotics and chemotherapeutic agents, was dominant in both E. faecalis (67.1%) and E. faecium (53.6%) strains. Multidrug-sensitive strains and strains resistant to one of the tested antibiotics were the most prevalent in the E. faecalis isolates (17.1% of the population). As the number of drugs to which E. faecalis strains are insensitive increased, the percentage of these strains decreased. One strain of E. faecalis assigned with the ZY profile, showed resistance to the highest number (n = 7) of antibiotics. The analysis of E. faecium drug susceptibility profiles revelaed that 21.4% of strains were resistant to one antibiotic, 3.6% to two, and 7.1% of isolated strains each showed the resistance to three, four or five antibiotics. In the studied population, four (4.9%) E. faecalis and four (14.3%) E. faecium strains were identified as multidrug-resistant (MDR).
Assessment of biofilm formation
The biofilm analysis revealed that all vancomycin-resistant E. faecalis and E. faecium strains demonstrated a higher biofilm-forming capacity, as compared to the susceptible strains. The lowest cell count of 5.31 log CFU / cm2 was reisolated from the biofilm produced by the vancomycin-sensitive strain EFM 2, however it was not statistically different from other susceptible strains of this species. The VRE strain EFA 25 was characterized by the highest capacity for biofilm formation (cell count exceeding 7 log CFU / cm2). Its biofilm-forming potential was statistically different from 5 to 6 vancomycin-sensitive E. faecalis strains tested. Among the E. faecium strains, the vancomycin-resistant strain EFM 7 showed the highest biofilm formation which was significantly different from all vancomycin-sensitive EFM strains (Fig. 4).
Discussion
Due to the common occurrence of enterococci in the digestive tract of humans and pig, their presence in the pigm farm environment is a naturally occuring phenomenon [23, 24]. Undoubtedly, of particular clinical relevance are two rogue enterococcai species, E. faecalis and E. faecium. They are commonly isolated from animals, e.g. their fecal specimens and meat as well as from materials and surfaces in animal farms and surrounding environment, means of animal transport, and animal farmworkers [8, 25, 26]. The results of most studies demonstrate that E. faecalis is the dominant species in the pig breeding environment. According to Gião et al. [27], of the 249 Enterococcus spp. strains isolated from pigs, E. faecalis and E. faecium accounted for 42.9% and 23.4%, respectively. Tan et al. [14] observed a higher difference in the occurence between E. faecalis (73.0%) and E. faecium (14.5%) in the material collected from animals, workers and the production environment of seven swine farms in Malaysia. In our study, the occurence frequency of the E. faecalis and E. faecium was 25.5% and 8.2%, respectively. Contrary results have been reported by de Jong et al. [2018] who isolated a higher number of E. faecium strains (328 of the 1146 samples taken from the pig gastrointestinal tract; 28.6%) than E. faecium strains (176; 28.6%). The observed differences may depend on many factors, including specific nutritional and hygienic practices implemented in animal farms, climatic conditions, number and source of samples, study area and sampling design. In our study, a much greater number of EFA/EFM-positive samples were fecal specimens, when compared to the study material taken from the production environment. Tan et al. [14] isolated both strains from pig feaces, but identified E. faecalis only from samples taken from the pig farm environment. According to studies by Staley et al. [28] E. faecalis is more abundant in the intestines of pigs than in faeces, in contrast to E. faecium. This was confirmed by Zhao et al. [26] who reported that E. faecium isolates accounted for almost 95% of all enterococci found in pig manure. To date, there is not enough research on the diversity of Enterococcus spp. strains from pig farms in Poland. Skowron et al. [6] showed that among 195 isolates isolated from pig farms, the largest number belonged to the species E. hirae (68%). The other species contributions were: E. faecalis—21%, E. durans—8% and E. faecium—3%. In this study, authors identified 60 genetically distinct strains [6].
The antibiotic resistance of enterococci seems to be a much more serious problem than the very fact of confirming their presence in the environment of farm animals. The global scale of this natural phenomenon is evidenced by the fact that antibiotic-resistant strains have been frequently isolated even from wild animals, theoretically not exposed to contact with chemotherapeutic agents [29, 30]. In the case of antibiotic-resistant zoonotic strains of enterococci, which are opportunistic human pathogens, there is a high risk that they may act as reservoirs of antibiotic resistance encoding genes that could be transmitted to other pathogenic bacteria, including clinically important pathogens [8, 31].
The spectrum of antibiotic resistance of enterococci isolated from the animal breeding environment depends on many factors, including the breeding system, the source of isolates or the specificity of the species and strain [32, 33]. According to the study of Kristich et al. [18], the occurrence of ampicillin resistance is less common in E. faecalis than in E. faecium. In turn, studies by Aasmäe et al. [34] showed, that the frequency of antibiotic resistant enterococci, including MDR, was higher among isolates obtained from pigs than cattle. Among the E. faecalis strains isolated in our study, the highest percentage showed resistance to high-level gentamicin (19.5%). This gentamicin resistance was found only in 17.9% of the E. faecium strains. Lee et al. [35] observed resistance to high-level gentamicin in all strains of E. faecium and E. faecalis derived from finisher pigs. On the contrary, Tan et al. [14] reported that E. faecalis strains (68.0%) were more resistant to high-level gentamicin (120 µg), as compared to E. faecium (39.0%). In other studies in Poland evaluating the resistance of Enterococcus spp. from meat pork, no strains resistant to gentamicin were found [36]. The emergence of high-level gentamicin-resistance (HLGR) in enterococci, first confirmed in E. faecalis and then in E. faecium, was one of the reasons for the increase in nosocomial infections observed since the 1980s worldwide. Importantly, the HLGR strains have become responsible for a significant proportion of enterococcal bacteremia [37, 38]. The possibility of transferring the HLRG gene from food-derived E. faecalis strains to strains colonizing the human gastrointestinal tract was confirmed by Sparo et al. [38].
The occurrence of E. faecalis and E. faecium strains of the HLSR phenotype among isolated streptomycin-resistant enterococci was similar and amounted to 9.8% and 10.7%, respectively. In the studies of Aasmäe et al. [34], the resistance to streptomycin was found in approximately one-third of porcine enterococci. Jahan et al. [39] showed that streptomycin resistance genes (aadA) can be transferred from meat-derived E. faecium to clinical E. faecalis strains by integron-mediated horizontal gene transfer. Conjugal transfer of HLRS genes (aadE) between porcine E. faecalis strains was observed by Chotinantakul et al. [40].
From the epidemiological point of view, vancomycin-resistant strains (VRE) constitute the most serious problem related to antibiotic resistance of enterococci [41, 42]. In 2017, vancomycin-resistant enterococci were responsible for approx. 55,000 hospitalizations in the USA, among which over 5,000 cases resulted in death [43, 44]. It has been proven that vancomycin resistance is confirmed less frequently in E. faecalis strains than in E. faecium isolates [18, 26, 43]. The results of our study are consistent with these observations, where we isolated 6.1% of E. faecalis and 14.3% E. faecium vancomycin-resistant strains that showed resistance to vancomycin. As reported Lee et al. [35] studying enterococci from finisher pigs, none of the 17 E. faecalis strains and only one of the 85 E. faecium strains was resistant to this antibiotic. In turn, in the studies reported by Badul et al. [8] and Tan et al. [14], all enterococcal isolates derived from pigs, farm workers as well as different sectors of animal and meat production (animal husbandry, distribution, transport) were vancomycin-resistant.
Regulation and expression of the vancomycin resistance mechanism is related to the presence of specific determinants in the genetic material of enterococci, called van operons. Clinically significant isolates are most frequently characterized by the vanA and vanB genotypes. Recently, despite the persistently higher frequency of vanA-positive strains, an increase in the number of vanB-positive VRE isolates has been observed [45, 46]. In our study, the genotypic analysis releaved that some E. faecalis strains were found to be positive for vanA (1; 1.2%), vanB (4; 4.9%) and vanD (1; 1.2%). For 4 E. faecium strains, the presence of the vanA (2; 7.1%) and vanB (2; 7.1%) genotypes was confirmed. In the studies by Ramos et al. [47], vanA-positive strains of E. feacium were detected in 18 of the 71 porcine faecal samples (25%), while vanC gene was detected in 7 samples (9.9%). The results of the work by Kotzamanidis et al. [48] revealed that 85% of the vancomycin-resistant E. faecium isolates from pig feaces were vanA-positive. Tan at al. [14] detected vanB and vanC genes in four enterococcal strains, however the phenotypic testing by disc diffusion method did not confirm their vancomycin resistance. Of a great importance is the fact that in clinical practice vanA resistance is induced in the presence of both vancomycin and another glycopeptide antibiotic, teicoplanin. As a consequence, vanA-positive strains do not show sensitivity to these both antibiotics, while vanB-positive strains are sensitive to teicoplanin [46, 49]. Also in the work of Ramos et al. [47], all vanA-positive E. faecium strains showed resistance to teicoplanin. In our study, E. faecalis and E. faecium strains insensitive to teicoplanin accounted for 2.4% and 7.1%, respectively. The results presented by Tan et al. [14] showed the presence of this trait in 2% of the strains of each species. Studies performed in animal farms in South Africa [8] and Australia [35] demonstrated that all E. faecalis and E. faecium strains isolated from pigs as well as from breeding and meat processing environment were sensitive to teicoplanin.
Resistance to vancomycin, which has undoubtedly contributed to the epidemiological importance of enterococci, is not the only problem raising serious public health concerns. The rapid spread of enterococcal multi-drug resistance forces clinicians to modify the previously established treatment regimens. This phenomenon is found not only in clinical isolates, but also in environmental isolates, including those associated with farm animals. It is believed that one of the reasons for the identification of MDR in enterococci may be an inadequate or irrational therapeutic regimens employed in commercial animal husbandry and breeding [33, 50]. In our study, we distinguished 26 drug susceptibility profiles. The profile A, characterized by sensitivity to all antibiotics and chemotherapeutic agents, was dominant in both E. faecalis (67.1%) and E. faecium (53.6%) strains, whereas four strains of each species (4.9% and 14.3%, respectively) were multi-drug resistant to 4 or more therapeutics. Gião et al. [27] showed that 27.4% of E. faecalis and 4.2% of E. faecium isolates from farm animals showed multi-drug resistance to 3 or more antibiotics. However, the results of other studies often report a higher prevalence of MDR strains among enterococci associated with the pig breeding environment. For instance, among all MDR enterococci (resistance to at least three different classes of antibiotics) isolated by Badul et al. [8], multi-drug resistant E. faecalis and E. faecium accounted for 79.3% (176/222 isolates) and 5.9% (13/222 isolates), respectively. An extremely high, as much as 98%, frequency of occurrence of enterococcal strains insensitive to at least four classes of antibiotics was reported by Tan et al. [14]. The same frequency of multi-drug-resistant enterococcal strains was demonstrated in studies by Lee et al. [35]. More than 94% of E. faecium strains were resistant to 3 or more antibiotics, 45.2% of strains showed the resistance to 4 classes of antibiotics, whereas MDR profiles were detected in 76.5% of E. faecalis strains. Also in Poland MDR was observed in the 84.6% and 42.5% strains E. faecium and E. faecalis isolated from pigs, respectively [51]. According to Różańska et al. [36], 56.8% of E. faecalis isolates derived from pork meat in Poland were resistant to 3 or more antimicrobials.
In addition, challenges resulting from antibiotic resistance of enterococci may be related to their ability to produce biofilm. The reduced possibility of penetration of antibiotics through the biofilm matrix contributes to the increase in tolerance to antibiotics. Moreover, compared to the planktonic form, biofilm creates more favorable conditions for the horizontal transfer of drug resistance genes [52]. In the studies by Tan et al. [14], biofilm was produced by 62% of enterococcal strains from pigs and humans. Our present study also showed that E. faecalis strains exhibit a higher biofilm formation potential than E. faecium. Our findings are in accordance with the results obtained by Chotinantakul et al. [40], who reported that at each of the tested temperatures (4 °C, 25 °C, 37 °C), E. faecalis produced significantly more biofilm than E. faecium. In our study, vancomycin-resistant EFA and EFM strains were characterized by higher potential for biofilm formation compared to non-resistant strains, while Ramadhan and Hegedus [53] did not observe statistically significant differences in biofilm formation beetwen these two strains as well as between vancomycin-resistant and vancomycin-sensitive isolates.
Conclusions
The irrational use of antibiotics in agriculture and veterinary practice is considered to be one of the key reasons for the rapid spread of antibiotic resistance among microorganisms. The results presented in this work confirm the presence of antibiotic-resistant E. faecalis and E. faecium strains in pig faeces and various production sectors of the pigsty. Among the isolated Enterococcus strains, both vancomycin-resistant and multi-drug resistant strains have been detected. We also found that vancomycin-resistant strains were characterized by a high ability to create biofilms, which facilitates their survival in conditions of increased environmental stress. Owing to the fact that livestock and animal husbandry environment can be a reservoir of antimicrobial resistance and transmission route of antimicrobial resistance genes from commensal zoonotic bacteria to clinical strains, it is of a great importance to public health to monitor trends in this biological phenomenon.
Materials and methods
Sample size and sampling procedure
The samples for the study were collected in April 2016 in a piggery in the Kuyavian-Pomeranian Voivodeship. The herd was kept in separate group pens. Each technological group was located in a separate building, and production was carried out in a closed system. The sows were placed in individual pens 7 days before farrowing. The average cast comprised of 567 sows and gilts, 2303 piglets, 1719 weaners and porkers, and 15 boars. The material consisted of samples in the form of swabs from troughs, feeding passages and corridors, manure channels, and faeces samples collected from various production sectors of the pigsty: the suckling pigs sector, weaned pigs sector, piglets and porkers sectors, and mating area. Additionally, samples were taken from the loading ramp and platform. In total, 475 samples were collected from the animal husbandry environment in the form of swabs (n = 350) and weights of faeces (n = 125). The swabs were collected using a sterile gauze (5 cm × 5 cm) held by tweezers. In order to standardize the sampling procedure, sterile cardboard templates with an area of 10 × 10 cm were used. Swabs from the troughs, feeding passages, coorridors and manure channels were collected from 5 separate places along the axis of the buildings, and swabs from the pens were collected from the center and each corner. Only pens with healthy animals were included in the study. Faecal samples (10 g) were collected from fresh fecal material.
Isolation of Enterococcus spp. strains
In the first stage of the laboratory tests, the samples were pre-diluted. 10 g of faeces or swab fragments were placed in 25 mL Ringer’s solution (potassium chloride: 0.30 g/L, calcium chloride dihydrate: 0.33 g/L, sodium chloride: 8.60 g/L) and shaken for 30 min. Then 10 mL of the resulting suspension was transferred to 90 mL of azide dextrose broth (Merck). The inoculated media were incubated at 37 °C for 48 h. After that, the inoculum was streaked on kanamycin esculin azide agar (Merck) and incubated at the same conditions. Enterococci grew in the form of tiny gray colonies surrounded by an olive-black agar zone. Single colonies from the resulting cultures were plated on Standard I Nutrient Agar (Merck) and incubated at 37 °C for 24 h. The resulting bacterial colonies were then suspended in nutrient broth (Merck) supplemented with 15% glycerol (Avantor) and stored at -80 °C until use.
Identification of Enterococcus species
For species identification, the frozen strains were plated on nutrient agar (Merck) and incubated for 48 h at 37 °C. After that, the strains were plated again onto nutrient agar (Merck) and incubated under the same conditions. DNA was isolated from the grown colonies by a spin column method using the Genomic Mini AX Bacteria Spin Kit (A&A Biotechnology), according to the manufacturer’s instructions. The isolated DNA served as template in the PCR reaction performed with the use of primers specific to 16 S rRNA gene (for identification of the genus Enterococcus spp.) and primers specific to sodA gene encoding superoxide dismutase (for strain classification). The following reference strains were used in the study: Enterococus faecium PCM 1859 and Enterococcus faecalis PCM 2673. The PCR reaction was performed according to the procedure described previously [54] (Table 4).
The composition of the reaction MasterMix was as follows: 1×DreamTaq polymerase buffer, 16 µM of each primer, dNTPs mix (0.2 mM each), 3.5 U of DreamTaq polymerase, 3.0 mM MgCl2 (all reagents were purchased from Fermentas). Next, 3.0 µL of the isolated DNA were added. The total volume of the reaction mixture was 25 µL. The amplification conditions were as follows: initial denaturation step at 95 °C for 4 min, followed by 30 cycles of denaturation at 95 °C for 30 s, annealing at 55 °C for 60 s and elongation at 72 °C for 60 s. The final extension step was performed at 72 °C for 7 min.
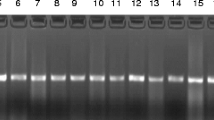
Electrophoretic separation of the PCR products (7 µL) was performed in a 2% agarose gel in 1×TBE buffer (EURx). In order to visualize the DNA fragments, a non-specific DNA intercalating dye SimpleSafe (EURx) was used. In order to assess the size of the PCR products, the GeneRuler 100 bp DNA Ladder (ThermoScientific) with a range of 100 to 1000 bp was used as a DNA molecular weight marker. The DNA electrophoresis was carried out at 20 V for 10 min, and then at 85 V for 110 min. The gel were visualized and documented using a UV transilluminator (BioRad).
Analysis of genetic similarity
In order to determine the degree of genetic similarity of the tested Enterococcus strains, the Random Amplified Polymorphic DNA (RAPD) method was employed with the use of a nine deoxyribonucleotide primer of the following sequence: 5’-ACGCGCCCT-3’ [55]. The composition of the reaction MasterMix was as follows: 1×DreamTaq polymerase buffer containing 1.5 mM MgCl2, 5 µM primer, dNTPs mix (0.2 mM each), 2.5 U of DreamTaq polymerase (all reagents were purchased from Fermentas). 22 µL of MasterMix per sample was pipetted into sterile 200 µL PCR tube strips, followed by addition of 3.0 µL of the isolated DNA. The total volume of the reaction mixture was 25 µL. The amplification conditions were as follows: 4 cycles of denaturation at 94 °C for 45 s, annealing at 30 °C for 120 s and elongation at 72 °C for 60 s, followed by 26 cycles of denaturation at 94 °C for 5 s, annealing at 36 °C for 30 s and elongation at 72 °C for 30 s. The final extension step was performed at 72 °C for 10 min.
Electrophoretic separation of the PCR products (8 µL) was performed in a 1.5% agarose gel in 1×TBE buffer (EURx). The GeneRuler 100 bp DNA Ladder (ThermoScientific) with a range of 100 to 1000 bp was used as DNA molecular weight marker. DNA electrophoresis was carried out at 20 V for 10 min, and then at 85 V for 90 min. DNA visualization and gel documentation were carried out as described above.
Data matrices were prepared for individual isolates in order to document the location of the RAPD reaction products. Then, the degree of genetic relationship between isolates of a given species was determined. For this purpose, phylogenetic trees were plotted in the STATISTICA 11 PL (StatSoft) program, using the UPGMA clustering method and Dice’s similarity coefficient as a distance unit.
Analysis of antibiotic resistance
The antibiotic susceptibility of the identified Enterococcus spp. strains was determined using the disc diffusion method. Following the microbial culture for 24 h at 37 °C, isolate suspensions were prepared in 0.9% saline, with the standard density of 0.5 McFarland, and subsequently spread on Mueller-Hinton agar (MHA, bioMérieux). Antimicrobial discs were applied and pressed firmy onto the agar surface with sterile forceps. The sensitivity to the following antibiotics was assessed: ampicillin (2 µg), imipenem (10 µg), ciprofloxacin (5 µg), levofloxacin (5 µg), norfloxacin (10 µg), teicoplanin (30 µg), vancomycin (5 µg), and quinupristin-dalfopristin (15 µg) for E. faecium; and tigecycline (15 µg), linezolid (10 µg), and nitrofurantoin (100 µg) for E. faecalis. Additionally, in order to detect HLGR (high-level gentamicin-resistant) and HLSR (high-level streptomycin-resistance) phenotypes, discs with gentamicin (30 µg) and streptomycin (300 µg) were applied. The dishes were incubated at 35 °C for 20 h. The results were interpreted in accordance with the EUCAST v. 7.0 recommendations [56].
In addition, minimal inhibitory concentrations (MICs) have been determined for vancomycin, teicoplanin, gentamicin, streptomycin and kanamycin. The MIC determination was carried out for the tested Enterococcus spp. strains using the agar microdilution method in a 96-well titration plate format, according to the CLSI (Clinical and Laboratory Standards Institute) recommendations. Strains were incubated in MHA at 37˚C for 24 h, then cultured in Tryptic Soy Broth (TSB, BioRad) under the same conditions. Then the bacteria were centrifuged at 4000 rpm for 15 min, the supernatant was removed by decantation, and the cell pellet was suspended in 4 mL of MHB at a 0.5 McFarland density. Inoculum suspensions were further diluted 1:100 in Mueller-Hinton broth before inoculation and 100 µl of the suspension were placed on the plate in triplicate. A two-fold serial dilution of tested antibiotics ranging from 0.25 to 2048 µg/mL was prepared in 100 µL of sterile MHB medium. The titration plates were placed in a humidity chamber and incubated at 37˚C for 24 h. Aftewards, suspension turbidity was measured according to the EUCAST guidelines [56]. Enterococcus faecalis ATCC 29,212 was used for quality-control purposes. The obtained results were used to determine the phenotypes of glycopeptide resistance, HLGR, HLSR and kanamycin resistance. Determination of the Van phenotype for Enterococcus spp. strains is based on the determination of the MIC values for vancomycin and teicoplanin. The literature specifies the concentration ranges of both antibiotics within which the established MIC values must fall. On this basis, the Van phenotype is assigned. In turn, determining the genotype consists of detecting the appropriate van gene [20]. The results were interpreted on the basis of the EUCAST recommendations [56] and literature [20] summarized in Table 5.
Detection of glycopeptide resistance genotypes
In order to determine the glycopeptide resistance genotypes in the tested Enterococcus spp. strains, the multiplex PCR reaction was performed with the use of isolated DNA (previously described in the section about identification of Enterococcus species). Details of primers used in the analysis are listed in Table 6.
The reference strains of E. faecium ATCC 700,221 (vanA) and E. faecalis ATCC 51,299 (vanB) were used in the study. Due to the lack of access to reference strains of other VRE genotypes, the control strains were selected based on the phenotype. The composition of PCR reaction mixture and amplification conditions were established according to the work by Depardieu et al. [58]. The composition of the reaction MasterMix was as follows: 1×DreamTaq polymerase buffer, 0.5 µM of each primer, dNTPs mix (0.2 mM each), 2.0 U of DreamTaq polymerase, and 3.0 mM MgCl2 (all reagents were purchased from Fermentas ).The 3.0 µL of the isolated DNA were added. The total volume of the reaction mixture was 25 µL. The amplification conditions were as follows: initial denaturation step at 95 °C for 3 min, followed by 30 cycles of denaturation at 94 °C for 60 s, annealing at 54 °C for 60 s and elongation at 72 °C for 60 s. The final extension step was performer at 72 °C for 7 min. Electrophoretic separation of the PCR products was performed as described above (see Identification of Enterococcus species).
Assessment of biofilm formation on a stainless-steel surface
The assesment of biofilm formation was performed in accordance with previous studies [59]. Sterile steel coupons (1 cm × 2 cm), three replications for each strain, were placed into tubes containing 3 mL of bacterial suspension in BHI (Merck) with standard density of 0.5 McFarland (1.5 × 108/mL) and incubated aerobically at 37 °C for 72 h. Six E. faecalis (EFA 1, 14, 25, 40, 50, 81) vancomycin-resistant strains (VRE), four E. faecium (EFM 7, 15, 22, 27) VRE strains, six vancomycin-susceptible EFA (2, 3, 4, 5, 7, 8) and four EFM (2, 3, 4, 9) strains were used for biofilm formation studies. Strains were randomly selected from each group. The medium was changed every 24 h. At each medium change, the coupons were rinsed with phosphate buffered saline (PBS) (137 mM NaCl, 2.7 mM KCl, 8 mM Na2HPO4, 2 mM KH2PO4) (BTL). After incubation, the samples were rinsed with PBS and placed into a new tube containing 3 mL of PBS. Next, sonication was performed using the Ultrasonic DU-4 sonicator (Nickel-Electro Ltd.) (10 min, 30 kHz, 150 W). After that, serial 10-fold dilutions of the obtained suspension were prepared, plated on the Columbia Agar medium with 5% Sheep Blood (Becton Dickinson) and incubated at 37 °C for 24 h. As positive control, a strong biofilm-forming strain Staphylococcus aureus ATCC 35,556 was used [60, 61]. Stainless steel fragments incubated in the sterile BHI medium only served as negative control. The results were expressed as the log CFU × cm2.
Statistical analysis
The data are expressed as mean ± standard error of mean (SEM) or standard deviation (SD). The results were obtained from at least three technical replicates. To determine the statistical significance, analysis of variance (ANOVA) followed by the Tukey post hoc test for multiple comparisons was performed. Statistical analysis and data visualization were performed with the Statistica 12 PL (StatSoft) software. A p-value < 0.05 was considered statistically significant.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Zou LK, Wang HN, Zeng B, Li JN, Li XT, Zhang AY, Zhou YS, Yang X, Xu CW, Xia Q. Erythromycin resistance and virulence genes in Enterococcus faecalis from swine in China. New Microbiol. 2011;34(1):73–80.
Oguttu JW, Qekwana DN, Odoi A. Prevalence and predictors of antimicrobial resistance among Enterococcus spp. from dogs presented at a Veterinary Teaching Hospital, South Africa. Front Vet Sci. 2021;7:589439. https://doi.org/10.3389/fvets.2020.589439.
Ahmed MO, Baptiste KE, Vancomycin-Resistant Enterococci. A Review of Antimicrobial Resistance Mechanisms and Perspectives of Human and Animal Health. Microbial drug resistance (Larchmont, N.Y.). 2018;24(5):590–606. https://doi.org/10.1089/mdr.2017.0147
Zaheer R, Cook SR, Barbieri R, Goji N, Cameron A, Petkau A, Ortega Polo R, Tymensen L, Stamm C, Song J, Hannon S, Jones T, Church D, Booker CW, Amoako K, Van Domselaar G, Read RR, McAllister TA. Surveillance of Enterococcus spp. reveals distinct species and antimicrobial resistance diversity across a one-health continuum. Sci Rep. 2020;10:3937. https://doi.org/10.1038/s41598-020-61002-5.
Markwart R, Willrich N, Haller S, et al. The rise in vancomycin-resistant Enterococcus faecium in Germany: data from the german Antimicrobial Resistance Surveillance (ARS). Antimicrob Resist Infect Control. 2019;8:147. https://doi.org/10.1186/s13756-019-0594-3.
Skowron K, Jeleńska A, Paluszak Z, Szala B. Prevalence and distribution of VRE (vancomycin resistant enterococci) and VSE (vancomycin susceptible enterococci) strains in the breeding environment. AAEM. 2016;23(2):231–6. https://doi.org/10.5604/12321966.1203882.
de Jong A, Simjee S, Rose M, Moyaert H, El Garch F, Youala M, EASSA Study Group (). Antimicrobial resistance monitoring in commensal enterococci from healthy cattle, pigs and chickens across Europe during 2004-14 (EASSA Study). J Antimicrob Chemother. 2019;l74(4):921–30. https://doi.org/10.1093/jac/dky537.
Badul Abia ALK, Amoako DG, Perrett K, Bester LA, Essack SY. From the farms to the dining table: the distribution and molecular characteristics of antibiotic-resistant Enterococcus spp. in intensive pig farming in South Africa. Microorganisms. 2021;9(5):882. https://doi.org/10.3390/microorganisms9050882.
Lu HZ, Weng XH, Li H, Yin YK, Pang MY, Tang YW. Enterococcus faecium-related outbreak with molecular evidence of transmission from pigs to humans. J Clin Microbiol. 2002;40(3):913–7. https://doi.org/10.1128/JCM.40.3.913-917.2002.
Novais C, Freitas AR, Silveira E, Antunes P, Silva R, Coque TM, Peixe L. Spread of multidrug-resistant Enterococcus to animals and humans: an underestimated role for the pig farm environment. J Antimicrob Chemother. 2013;68(12):2746–54. https://doi.org/10.1093/jac/dkt289.
Beshiru A, Igbinosa IH, Omeje FI, Ogofure AG, Eyong MM, Igbinosa EO. Multi-antibiotic resistant and putative virulence gene signatures in Enterococcus species isolated from pig farms environment. Microb Pathog. 2017;104:90–6. https://doi.org/10.1016/j.micpath.2017.01.020.
Braga TM, Pomba C, Lopes MF. High-level vancomycin resistant Enterococcus faecium related to humans and pigs found in dust from pig breeding facilities. Vet Microbiol. 2013;161(3–4):344–9. https://doi.org/10.1016/j.vetmic.2012.07.034.
Zarzecka U, Zadernowska A, Chajęcka-Wierzchowska W. Effects of osmotic and high pressure stress on expression of virulence factors among Enterococcus spp. isolated from food of animal origin. Food Microbiol. 2022;102:103900. doi: https://doi.org/10.1016/j.fm.2021.103900
Tan SC, Chong CW, Teh CSJ, Ooi PT, Thong KL. Occurrence of virulent multidrug- resistant Enterococcus faecalis and Enterococcus faecium in the pigs, farmers and farm environments in Malaysia. PeerJ. 2018;6:e5353. https://doi.org/10.7717/peerj.5353.
Miller WR, Munita JM, Arias CA. Mechanisms of antibiotic resistance in enterococci. Expert Rev Anti Infect Ther. 2014;12(10):1221–36. https://doi.org/10.1586/14787210.2014.956092.
Talaga-Ćwiertnia K, Bulanda M. Lekooporność rodzaju Enterococcus - aktualny problem wśród ludzi i zwierząt. Article in polish. Post Mikrobiol. 2018;57(3):244–50.
Pissetti C, Kich JD, Allen HK, Navarrete C, de Freitas Costa E, Morés N, Cardoso M. Antimicrobial resistance in commensal Escherichia coli and Enterococcus spp. isolated from pigs subjected to different antimicrobial administration protocols. Res Vet Sci. 2021;137:174–85. https://doi.org/10.1016/j.rvsc.2021.05.001.
Kristich CJ, Rice LB, Arias CA. Enterococcal infection—treatment and antibiotic resistance. In: Gilmore MS, editor. Et. al., Enterococci: from commensals to leading causes of drug resistant infection. Massachusetts Eye and Ear Infirmary; 2014.
Rogoz W, Sypniewski D, Bednarek I. Analysis of selected genetic traits, phenotypes, and epidemiological threat of Enterococcus bacteria resistant to vancomycin.Adv Microbiol. 201958(1):35–48. doi: https://doi.org/10.21307/PM-2019.58.1.035
Szczypta A, Talaga K, Bulanda M. Vancomycin-resistant enterococci as etiologic agents in healthcare-associated infections—pathogenicity and control methods.Hygeia Public Health2016;51(2):134–140
Arredondo-Alonso S, Top J, Corander J, et al. Mode and dynamics of vanA-type vancomycin resistance dissemination in dutch hospitals. Genome Med. 2021;13:9. https://doi.org/10.1186/s13073-020-00825-3.
Hammerum AM. Enterococci of animal origin and their significance for public health. Clin Microbiol Infect: the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2012;18(7):619–625. https://doi.org/10.1111/j.1469-0691.2012.03829.x
Kern M, Aschenbach JR, Tedin K, et al. Characterization of inflammasome components in Pig Intestine and analysis of the influence of probiotic Enterococcus faecium during an Escherichia coli challenge. Immunol Invest. 2017;46(7):742–57.
Cattoir V. The multifaceted lifestyle of enterococci: genetic diversity, ecology and risks for public health. Curr Opin Microbiol. 2022;65:73–80. https://doi.org/10.1016/j.mib.2021.10.013.
Dubin K, Pamer EG. Enterococci and their interactions with the intestinal microbiome. Microbiol Spectr. 2004;5(6). https://doi.org/10.1128/microbiolspec.BAD-0014-2016.
Zhao J, Liu R, Sun Y, Yang X, Yao J. Tracing enterococci persistence along a pork production chain from feed to food in China. Anim Nutr. 2022;9:223–32. https://doi.org/10.1016/j.aninu.2022.01.005.
Gião J, Leão C, Albuquerque T, Clemente L, Amaro A. Antimicrobial susceptibility of Enterococcus isolates from cattle and pigs in portugal: linezolid resistance genes optra and poxta. Antibiotics. 2022;11:615. https://doi.org/10.3390/antibiotics11050615.
Staley C, Dunny GM, Sadowsky MJ. Environmental and animal-associated enterococci. Adv Appl Microbiol. 2014;87:147–86. https://doi.org/10.1016/B978-0-12-800261-2.00004-9.
Oliveira de Araujo G, Huff R, Favarini MO, Mann MB, Peters FB, Frazzon J, Guedes Frazzon AP. Multidrug resistance in Enterococci isolated from wild Pampas Foxes (Lycalopex gymnocercus) and Geoffroy’s cats (Leopardus geoffroyi) in the brazilian pampa biome. Front Vet Sci. 2020;7:606377. https://doi.org/10.3389/fvets.2020.606377.
Nowakiewicz A, Zięba P, Gnat S, Trościańczyk A, Osińska M, Łagowski D, Kosior-Korzecka U, Puzio I. A significant number of multi-drug resistant Enterococcus faecalis in wildlife animals; long-term consequences and new or known reservoirs of resistance? Sci. Total Environ. 2020;705:135830. https://doi.org/10.1016/j.scitotenv.2019.135830.
de Jong A, Simjee S, Garch FE, Moyaert H, Rose M, Youala M, Dry M, EASSA Study Group. (2018). Antimicrobial susceptibility of enterococci recovered from healthy cattle, pigs and chickens in nine EU countries (EASSA Study) to critically important antibiotics. Vet. Microbiol. 2018;216, 168–175. https://doi.org/10.1016/j.vetmic.2018.02.010
van Hoorebeke S, van Immerseel F, Berge AC, Persoons D, Schulz J, Hartung J, Harisberger M, Regula G, Barco L, Ricci A, de Vylder J, Ducatelle R, Haesebrouck F, Dewulf J. Antimicrobial resistance of Escherichia coli and Enterococcus faecalis in housed laying-hen flocks in Europe. Epidemiol Infect. 2011;139(10):1610–20. https://doi.org/10.1017/S0950268810002700.
Liu M, Kemper N, Volkmann N, Schulz J. Resistance of Enterococcus spp. in dust from farm animal houses: a retrospective study. Front Microbiol. 2018;9:3074. https://doi.org/10.3389/fmicb.2018.03074.
Aasmäe B, Häkkinen L, Kaart T, Kalmus P. Antimicrobial resistance of Escherichia coli and Enterococcus spp. Acta Vet Scand. 2019;61(1):5. https://doi.org/10.1186/s13028-019-0441-9. isolated from Estonian cattle and swine from 2010 to 2015.
Lee T, Jordan D, Sahibzada S, Abraham R, Pang S, Coombs GW, O’Dea M, Abraham S. Antimicrobial resistance in porcine enterococci in Australia and the ramifications for human health. Appl Environ Microbiol. 2021;87:e03037–20. https://doi.org/10.1128/AEM.03037-20.
Różańska H, Lewtak-Piłat A, Osek J. Antimicrobial resistance of Enterococcus faecalis isolated from meat. Bull Vet Inst Pulawy. 2015;59:229–33. https://doi.org/10.1515/bvip-2015-0034.
Caballero-Granado FJ, Cisneros JM, Luque R, Torres-Tortosa M, Gamboa F, Díez F, Villanueva JL, Pérez-Cano R, Pasquau J, Merino D, Menchero A, Mora D, López-Ruz MA, Vergara A. Comparative study of bacteremias caused by Enterococcus spp. with and without high-level resistance to gentamicin. J Clin Microbiol. 1998;36(2):520–5. https://doi.org/10.1128/JCM.36.2.520-525.1998.
Sparo M, Urbizu L, Solana MV, Pourcel G, Delpech G, Confalonieri A, Ceci M, Sánchez Bruni SF. High-level resistance to gentamicin: genetic transfer between Enterococcus faecalis isolated from food of animal origin and human microbiota. Lett Appl Microbiol. 2012;54(2):119–25. https://doi.org/10.1111/j.1472-765X.2011.03182.x.
Jahan M, Zhanel GG, Sparling R, Holley RA. Horizontal transfer of antibiotic resistance from Enterococcus faecium of fermented meat origin to clinical isolates of E. faecium and Enterococcus faecalis. Int J Food Microbiol. 2015;199:78–85.
Chotinantakul K, Chansiw N, Okada S. Biofilm formation and transfer of a streptomycin resistance gene in enterococci from fermented pork. JGAR. 2020;22:434–40. https://doi.org/10.1016/j.jgar.2020.04.016.
Cassini A, Högberg LD, Plachouras D, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis. 2019;19(1):56–66.
Ayobami O, Willrich N, Reuss A, Eckmanns T, Markwart R. The ongoing challenge of vancomycin-resistant Enterococcus faecium and Enterococcus faecalis in Europe: an epidemiological analysis of bloodstream infections. Emerg Microbes Infect. 2020;9(1):1180–93. https://doi.org/10.1080/22221751.2020.1769500.
Levitus M, Rewane A, Perera TB. Vancomycin-Resistant Enterococci. StatPearls. 2022StatPearls Publishing.
Centers for Disease Control and Prevention. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf
Bender JK, Cattoir V, Hegstad K, Sadowy E, Coque TM, Westh H, Hammerum AM, Schaffer K, Burns K, Murchan S, Novais C, Freitas AR, Peixe L, Del Grosso M, Pantosti A, Werner G. Update on prevalence and mechanisms of resistance to linezolid, tigecycline and daptomycin in enterococci in Europe: towards a common nomenclature. Drug Resist Updates. 2018;40:25–39. https://doi.org/10.1016/j.drup.2018.10.002.
Correa-Martínez CL, Jurke A, Schmitz J, Schaumburg F, Kampmeier S, Mellmann A. Molecular Epidemiology of Vancomycin-Resistant Enterococci Bloodstream Infections in Germany: A Population-Based Prospective Longitudinal Study. Microorganisms 2022;10:130. https://doi.org/10.3390/microorganisms10010130
Ramos S, Igrejas G, Rodrigues J, Capelo-Martinez JL, Poeta P. Genetic characterisation of antibiotic resistance and virulence factors in vanA-containing enterococci from cattle, sheep and pigs subsequent to the discontinuation of the use of avoparcin. Vet J. 2012;193(1):301–3. https://doi.org/10.1016/j.tvjl.2011.12.007.
Kotzamanidis C, Zdragas A, Kourelis A, Moraitou E, Papa A, Yiantzi V, Pantelidou C, Yiangou M. Characterization of vanA-type Enterococcus faecium isolates from urban and hospital wastewater and pigs. J Appl Microbiol. 2009;107(3):997–1005. https://doi.org/10.1111/j.1365-2672.2009.04274.x.
Hughes CS, Longo E, Phillips-Jones MK, Hussain R. Characterisation of the selective binding of antibiotics vancomycin and teicoplanin by the VanS receptor regulating type A vancomycin resistance in the enterococci. Biochim Biophys Acta Gen Subj. 2017;1861(8):1951–9. https://doi.org/10.1016/j.bbagen.2017.05.011.
Seputiene V, Bogdaite A, Ruzauskas M, Suziedeliene E. Antibiotic resistance genes and virulence factors in Enterococcus faecium and Enterococcus faecalis from diseased farm animals: pigs, cattle and poultry. Pol J Vet Sci. 2012;15(3):431–8.
Nowakiewicz A, Ziółkowska G, Trościańczyk A, Zięba P, Gnat S. Determination of antimicrobial resistance of Enterococcus strains isolated from pigs and their genotypic characterization by method of amplification of DNA fragments surrounding rare restriction sites (ADSRRS fingerprinting). J Med Microbiol. 2017;66(2):175–83. https://doi.org/10.1099/jmm.0.000400.
Ch’ng JH, Chong K, Lam LN, Wong JJ, Kline KA. Biofilm-associated infection by enterococci. Nat Rev Microbiol. 2019;17(2):82–94. https://doi.org/10.1038/s41579-018-0107-z.
Ramadhan AA, Hegedus E. Biofilm formation and esp gene carriage in enterococci. J Clin Pathol. 2005;58(7):685–6. https://doi.org/10.1136/jcp.2004.024109.
Jackson CR, Fedorka-Cray PJ, Barrett JB. Use of a Genus- and species-specific multiplex PCR for identification of Enterococci. J Clin Microbiol. 2004;42(8):3558–65.
Hans-Jurg M, Quednau M, Samuelsson A, Isaksson B, Ahrne S, Jonasson J. Division of the genus Enterococcus into species groups using PCR-based molecular typing methods. Microbiol. 1998;144:1171–9.
The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. http://www.eucast.org. Accessed 30 September 2016
Dutka-Malen SS, Evers S, Courvalin P. Detection of glycopeptide resistance genotypes and identification to the species level of clinically relevant enterococci by PCR. J Clin Microbiol. 1995;33:24–7.
Depardieu F, Perichon B, Courvalin P. Detection of the. alphabet and identification of enterococci and staphylococci at the species level by multiplex PCR J Clin Microbiol. 2004;42(12):5857–60.
Skowron K, Wałecka-Zacharska E, Grudlewska K, Gajewski P, Wiktorczyk N, Wietlicka-Piszcz M, Dudek A, Skowron KJ, Gospodarek-Komkowska E. Disinfectant susceptibility of biofilm formed by Listeria monocytogenes under selected environmental conditions. Microorganisms. 2019;7(9):280. https://doi.org/10.3390/microorganisms7090280.
Seidl K, Goerke C, Wolz C, Mack D, Berger-Bächi B, Bischoff M. Staphylococcus aureus CcpA affects biofilm formation. Infect Immun. 2008;76:2044–50. https://doi.org/10.1128/IAI.00035-08.
Neopane P, Nepal HP, Shrestha R, Uehara O, Abiko Y. In vitro biofilm formation by Staphylococcus aureus isolated from wounds of hospital-admitted patients and their association with antimicrobial resistance. Int J Gen Med. 2018;11:25–32. https://doi.org/10.2147/IJGM.S153268.
Acknowledgements
Not applicable.
Funding
This research was financially supported by the Nicolaus Copernicus University with funds from the maintenance of the research potential of the Department of Microbiology PDB WF 536. The article is financed with funding of publication costs under the “Excellence Initiative - Research University” programme in Nicolaus Copernicus University in Toruń.
Author information
Authors and Affiliations
Contributions
KGB and KS designed the study. KGB, NWK and AB collected the data. AB, MWi and MWu analyzed data. KGB, KS, and AB interpreted the results. KGB and JBK primarily wrote the manuscript. KS and ZP provided valuable insight for revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
None of the procedures authors performed involved animals and authors had no direct contact with them. All samples were from the pig farm environment. These were air samples, swabs, litter and faeces samples (taken after defecation). In addition, samples of litter and faeces were collected by pig house employees so as not to stress the animals with the presence of strangers. The oral consent of the pig farm owner was obtained for sampling.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Grudlewska-Buda, K., Skowron, K., Bauza-Kaszewska, J. et al. Assessment of antibiotic resistance and biofilm formation of Enterococcus species isolated from different pig farm environments in Poland. BMC Microbiol 23, 89 (2023). https://doi.org/10.1186/s12866-023-02834-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-023-02834-9