Abstract
Background
To report the role of Polymerase Chain Reaction in confirming the diagnosis of presumed Mycobacterium Tuberculosis (MTB) Intermediate Uveitis.
Method
Retrospective analysis of 22 eyes of 14 cases of presumed tubercular intermediate uveitis wherein intraocular fluid was tested for MTB DNA by Nested & Real-time PCR, based on clinical suspicion of tubercular aetiology. QuantiFERON TB gold test and High-Resolution CT Chest were done. Patients were treated with anti-tubercular therapy with oral steroids & immunomodulators. In the study, eleven were male (79%) and three female (21%). The median age was 34 years. Nested PCR for both IS 6110 & MPB 64 was positive in 64% of the cases, IS 6110 positive in 23% and MPB 64 positive in 15%. Real-time PCR was positive in 48% of the cases. Vision improved in 33% of cases, maintained in 57%, and worsened in 10% of cases.
Conclusion
Presumed Tubercular intermediate uveitis can be confirmed by PCR of intraocular fluids. Anti-tubercular therapy with immunosuppression can improve vision and prevent recurrences in such cases.
Similar content being viewed by others
Background
Tuberculosis is a major health problem in India. It is the second leading cause of death by a single infectious agent worldwide [1]. Ocular TB is a recognized form of extrapulmonary TB associated with significant morbidity [2]. Ocular tuberculosis can manifest as anterior, intermediate, posterior or pan uveitis. It often poses a diagnostic dilemma due to its protean manifestations. If it is not treated adequately, it can lead to permanent loss of vision [1]. In recent years, the use of molecular biologic techniques based on DNA amplification to detect small amounts of genomic sequences from fluids or tissues has allowed us to diagnose or confirm infections that were previously difficult to detect [1]. Polymerase chain reaction (PCR) is one such technique for the evaluation of very small amounts of DNA or RNA by enzymatic amplification of nucleic acid sequences [3, 4]. The first use of PCR in detecting Mycobacterium tuberculosis (MTB) from the eye was reported from aqueous samples of two patients with active retinal vasculitis [3, 5]. Quantitative (qPCR) or real-time PCR is a variant of PCR that allows the quantification of nucleic acid in the sample and facilitates the monitoring of the progress of a PCR reaction in real-time [3, 6]. Although PCR positivity for MTB has been reported before in other tubercular uveitis entities (anterior, posterior) and retinal vasculitis, very few studies have reported PCR positivity for the same in intermediate uveitis [7,8,9,10,11]. We studied intraocular fluid by PCR in intermediate uveitis for mycobacterial tuberculosis DNA by both nested and real-time PCR. The objective of the study is to report the clinical profile, management and visual outcome of 14 cases of intermediate uveitis positive for Mycobacterium tuberculosis DNA by PCR of intraocular fluid (aqueous and vitreous). According to COTS-2 guidelines, either one or both immunologic tests (purified protein derivative PPD, interferon-gamma release assay IGRA) along with high resolution computed tomography (HRCT) of the chest suggestive of healed TB aetiology is required to start anti-tubercular treatment [12].
Methodology
It was a retrospective case series wherein 22 eyes of 14 patients diagnosed with unilateral/bilateral intermediate uveitis with intraocular fluid were positive for Mycobacterium tuberculosis (MTB) DNA by PCR – Nested (both IS 6110 & MPB 64 gene) and/or real-time with minimum 1 year follow up were analysed.
The diagnosis of intermediate uveitis was made based on the Standardization of Uveitis Nomenclature (SUN) working group international workshop for reporting clinical data, which stated that it is a subset of uveitis where the vitreous is the major site of the inflammation, with or without peripheral vascular sheathing and macular oedema [13]. All patients had a detailed history including systemic illness recorded in the case records. The patients underwent complete ophthalmic examination including best-corrected visual acuity, intraocular pressure by applanation tonometer, slit-lamp biomicroscopy, and posterior segment examination with both slit-lamp biomicroscopy and indirect ophthalmoscopy at baseline and subsequent follow-up visits. Ancillary tests including fundus fluorescein angiography, optical coherence tomography with or without angiography, ultrasound biomicroscopy, etc., were done as and when indicated. Systemic assessment of all patients was done by an in-house internist. All patients underwent laboratory investigations like complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), syphilitic screening by Venereal Disease Research Laboratory (VDRL), and treponema pallidum hemagglutination test, high resolution computed tomography (HRCT) chest, Mantoux test, tuberculosis (TB) interferon-gamma release assay (Quanti-FERON TB gold test) and serum angiotensin-converting enzyme (ACE) level were done. Also, magnetic resonance imaging (MRI) scan of the brain and immune markers consisting of rheumatoid factor (RF), anti-double-stranded deoxyribonucleic acid (anti-dsDNA), antineutrophil cytoplasmic antibodies (ANCA) were done whenever required. After ruling out other causes of intermediate uveitis, the decision to test MTB PCR in ocular fluids was taken if patients show positive results in one of the corroborative investigations suggesting tubercular aetiology which includes positive PPD test, IGRA assay, HRCT chest. PCR was done in the aqueous sample of 7 patients and the vitreous sample of 7 patients. The patients who were tested with vitreous samples had undergone diagnostic as well as therapeutic vitrectomy for non-resolving or recurring inflammation, despite maximal tolerated anti-inflammatory therapy.
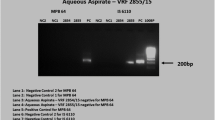
DNA was extracted from the specimens (aqueous aspirate) using a Qiagen DNA extraction kit (Hilden, Germany) following the manufacturer's instructions. The extracted DNA was stored at -20 degrees C till further use. Nested PCR with 2 sets of primers targeting MPB 64 gene and IS6110 region were carried out [14]. Real-time PCR for the detection of the Mycobacterial load was estimated in the DNA extracts of the test sample using a commercial kit—Geno Sen’s® MTb Complex RG quantitative and the assay was performed on Rotor-Gene (Hilden, Germany) real-time PCR equipment based on Taqman principle.
All patients received treatment with oral steroids and four-drug anti-tubercular therapy. Those not responding to corticosteroids immunomodulators were added. The decision regarding treatment regimen in terms of initiation and duration of ATT and the addition of immunomodulatory therapy was taken in consensus with attending physicians in collaboration with respiratory disease physicians.
The primary outcome measure was changed in visual acuity, whether improved or maintained or deteriorated at the 1 year follow up. The secondary outcome measure was the proportion of patients with recurrence of inflammation after 6 months of initiation of treatment. The study was approved by The Institutional Review Board and adhered to the tenets of Helsinki.
Results
The study included fourteen patients, out of which 11 were males and 3 were females; The median age was 34 years (Range: 10-61 years). The disease was bilateral in 8 patients (57%). Defective vision (93%) was the most common presenting complaint, followed by floaters (70%). Twenty-three per cent of patients were previously treated with oral steroids and another 23% with posterior sub tenon steroid injections. The mean best-corrected visual acuity at presentation and at last follow up were 6/24 and 6/18 respectively. The anterior segment was quiet with broad-based posterior synechiae (Fig. 1) in twenty-nine per cent of patients. Vitreous was the most common finding, present in all the eyes and snowballs exudates were present in 33% of the eyes. Fundus examination (pseudocolour fundus picture- Optos 200Tx imaging system, Optos PLC, Dunfermline, Scotland, UK) of both eyes (Fig. 2A and B) of a patient whose aqueous sample was tested positive for PCR MTB showed relatively clear media with snowball vitreous exudates (black arrowheads) and attached retina and the right eye (Fig. 2A) also had peripheral vitreous membranes (blue arrow Fig. 2B). PPD was noted in 46%, positive HRCT in 38% and Quanti-FERON TB gold was positive in 46% of cases. All the three were positive in 1% of the patients. PCR was done in an aqueous sample of 7 patients and a vitreous sample of 7 patients. PCR results are shown in Table 1. Nested PCR for both IS 6110 & MPB 64 was positive in 64% of the cases. IS 6110 positive in 23% and MPB 64 positive in 15%. Real-time PCR was positive in 48% of the cases. Nested and Real-time PCR positivity in the aqueous sample of 7 patients (Fig. 3) and that of a vitreous sample of 7 patients (Fig. 4). All patients were treated with oral steroids with anti-tubercular treatment for 9 months after being evaluated by an attending in-house physician and a pulmonologist with initial 2 months of intensive treatment with all 4 drugs (isoniazid, rifampicin, ethambutol and pyrazinamide) followed by 7 months with 2 drugs (isoniazid and rifampicin). Posterior sub tenon steroid injections were given in 15% of the patients. Immunomodulator therapy was needed in 46% of the patients and the most common drug used was Mycophenolate Mofetil. Ocular complications encountered were epiretinal membranes (29% of eyes), cystoid macular oedema (14%), posterior subcapsular cataract (0.1%), hypotony (0.1%), choroidal neovascular membrane (CNVM) (0.1%). No systemic complications were encountered. Vision improved in 33% of the cases, maintained in 57% and worsened in 10% of cases. Factors associated with poor visual acuity include cystoid macular oedema, epiretinal membrane and cataract. Recurrences were observed in 23% of the eyes 6 months after initiation of treatment.
Wide-field fundus photo (pseudocolour fundus picture- Optos 200Tx imaging system, Optos PLC, Dunfermline, Scotland, UK) of the right eye (A) and left eye (B) of a patient whose aqueous sample was tested positive for PCR MTB. It showed relatively clear media with snowball vitreous exudates (black arrowheads) and attached retina. The right eye also had peripheral vitreous membranes (blue arrow)
Discussion
Mycobacterium tuberculosis is one of the important infectious agents responsible for intermediate uveitis. It was thought that eye shows hypersensitivity to the non-viable or tubercular bacilli DNA causing such uveitis. For a definite diagnosis of aetiology, isolation of the MTB bacilli from the vitreous sample, aqueous paracentesis or retinal biopsy is required.
Our study provided the clinical spectrum and visual outcome of patients with intermediate uveitis with positive PCR of intraocular fluids for MTB. The Pubmed search did not show any study on Real-Time/nested Quantitative PCR positivity for MTB in intermediate uveitis. PCR has emerged as a powerful tool for rapid detection of the mycobacterial genome, with high specificity and variable sensitivity. The utility of PCR analysis lies in important facts like ocular samples usually are tested negative for the acid-fast bacilli (AFB) with direct smear and culture due to the paucibacillary nature of the disease and the systemic involvement may not be present at the time of ocular disease, causing a delay in diagnosis and management [15].
PCR has a very low false-positive rate on intraocular fluids. External contamination leads to false-positive and polymorphism, specimen degradation, or failure to sample in the acute stages of disease-causing false-negative results [16]. Arora et al. evaluated the role of PCR for the detection of Mycobacterium tuberculosis in aqueous humour samples obtained from eyes with active uveitis and showed that it can be effectively used for the diagnosis of intraocular tuberculosis, which was supported by the review report by Gupta et al [17]. In our study, we performed PCR testing for presumed tubercular intermediate uveitis. As culture is difficult and time-consuming, presently, the use of real-time PCR can be done to establish tubercular aetiology, our study also proved PCR to be an important tool for rapid detection of the mycobacterial genome in suspected tubercular intermediate uveitis cases.
Parchand et al. discussed the clinical profile of intermediate uveitis in the Indian population and concluded that the addition of anti-tuberculosis therapy in cases of intermediate uveitis of presumed tubercular origin can reduce the recurrences [18]. According to them, patients were diagnosed with intermediate uveitis of presumed tubercular aetiology if there was a documented positive tuberculin skin test (10 mm of induration or more) at 48–72 h with evidence of vitritis, snowballs, or snow banking; and all known causes of infectious uveitis except TB and known non-infectious uveitis syndromes were ruled out. Madhavan et al. proved the presence of tuberculosis genome in the vitreous chamber fluid and the epiretinal membrane in Eales disease. They found that 5 out of 14 vitreous (20.8%) fluid samples were positive for the tuberculosis genome. In our study, we found that about 64% of the patients showed positivity for TB genome in nested PCR and 48% of cases showed positivity in real-time PCR in intermediate uveitis. The PCR results showcased circulating antigens of tuberculosis leading to an inflammatory response. In our study, fundus evaluation of patients with positive PCR (AC tap or Vitreous tap) demonstrated features of snowball opacities and vitritis. Our study provides the clinical profile of cases of intermediate uveitis with documented evidence of MTB DNA in ocular fluids. Of note is that 48% of patients in the study had actively multiplying copies of MTB DNA by Real-time PCR. In cases with signs and symptoms of intermediate tubercular uveitis but not fitting into COTS 2 criteria, ocular fluids PCR testing can also be considered as a diagnostic modality for appropriate diagnosis and treatment [19]. Figueira et al. described the role of anti-tuberculosis treatment in inflammatory diseases suggestive of tubercular aetiology [20]. The consensus was that the positively screened patients should be treated for active tuberculosis with 4 drugs (isoniazid, rifampicin, pyrazinamide and ethambutol) for 6–9 months. Patients should be reviewed at end of the initiation phase which is 2 months and the end of treatment, which is 9 months. Sixteen per cent of our patients had recurrences in one year. We considered MPB64 and IS6110 only for the PCR study based on the earlier reports, which suggest MPB64 is 10,000 times more sensitive than IS6110 for the diagnosis of tubercular uveitis [21]. In the Indian population, the lack or presence of relatively few copies of IS6110 has been recorded, which could lead to missing cases of probable intraocular tuberculosis. For the diagnosis of intraocular tuberculosis, the MPB64 gene-based PCR specific for MTB has been carefully studied and found to be more sensitive than the IS6110 PCR.
The study’s major limitations include small sample size, retrospective nature, lack of comparison with other causes of intermediate uveitis with intraocular fluids negative for PCR and relatively short follow up, lack of standardization of PCR, and not using multiplex PCR targeting more than one gene and low sensitivity. Further studies are needed to find out the role of PCR in intermediate uveitis of tubercular origin.
Conclusion
Tuberculosis should be considered an important aetiology of intermediate uveitis in endemic countries like India. Intermediate uveitis of tubercular aetiology can be diagnosed by polymerase Chain Reaction of intraocular fluids. It can also be considered a diagnostic modality in cases with strong clinical suspicion of tubercular origin. Although anti-inflammatory therapy in the form of oral steroids with or without immunosuppression remains the mainstay of treatment of intermediate uveitis, the addition of anti-tubercular therapy to the treatment regime in PCR MTB positive cases can cause resolution of uveitis and reduce the recurrences.
Availability of data and materials
Available with the corresponding author.
Abbreviations
- PCR:
-
Polymerase Chain Reaction
- MTB:
-
Mycobacterium Tuberculosis
- HRCT:
-
High-Resolution Coherence Tomography
- qPCR:
-
Quantitative Polymerase Chain Reaction
- COTS:
-
Collaborative Ocular Tuberculosis Study
- IGRA:
-
Interferon Gamma Release Assay
- SUN:
-
Standardization of Uveitis Nomenclature
- PPD:
-
Purified Protein Derivative
- ATT:
-
Anti Tubercular Treatment
References
Ortega-Larrocea G, Bobadilla-del-Valle M, Ponce-de-León A, Sifuentes-Osornio J (2003) Nested polymerase chain reaction for mycobacterium tuberculosis DNA detection in aqueous and vitreous of patients with uveitis. Arch Med Res 34(2):116–119. https://doi.org/10.1016/s0188-4409(02)00467-8
Shakarchi FI (2015) Ocular tuberculosis: current perspectives. Clin Ophthalmol 9:2223–2227
Sharma P, Bansal R, Gupta V, Gupta A (2010) Diagnosis of tubercular uveitis by quantitative polymerase chain reaction. J Ophthalmic Inflamm Infect 1(1):23–27. https://doi.org/10.1007/s12348-010-0004-8.PMID:21475653;PMCID:PMC3062759
Chi-Chao C, DeFen C, Tuo J (2005) Polymerase chain reaction in the diagnosis of uveitis. Int Ophthalmol Clin 45:41–55. https://doi.org/10.1097/01.iio.0000155936.98330.3d
Kotake S, Kimura K, Yoshikawa K et al (1994) Polymerase chain reaction for detection of Mycobacterium tuberculosis in ocular tuberculosis [letter]. Am J Ophthalmol 117:805–806
Heid CA, Stevens J, Livak KJ, Williams PM (1996) Real-time quantitative PCR. Genome Res 6:986–994. https://doi.org/10.1101/gr.6.10.986
Sagar Sudhakar Bhuibhar & Jyotirmay Biswas (2012) Nested PCR-positive tubercular ampiginous choroiditis: a case report. Ocul Immunol Inflamm 20(4):303–305. https://doi.org/10.3109/09273948.2012.685684
Biswas J, Kazi MS, Agarwal VA, Alam MS, Therese KL (2016) Polymerase chain reaction for Mycobacterium tuberculosis DNA detection from ocular fluids in patients with various types of choroiditis in a referral eye centre in India. Indian J Ophthalmol 64(12):904–907. https://doi.org/10.4103/0301-4738.198857.PMID:28112131;PMCID:PMC5322705
Gupta A, Gupta V, Arora S et al (2001) PCR-positive tubercular retinal vasculitis. Retina 21(5):435–444
Madhavan HN, Therese KL, Gunisha P, Jayanthi U, Biswas J (2000) Polymerase chain reaction for detection of Mycobacterium tuberculosis in the epiretinal membrane in Eales’ disease. Invest Ophthalmol Vis Sci 41(3):822–859
Kharel (Sitaula) R, Janani MK, Madhavan HN, et al. Outcome of polymerase chain reaction (PCR) analysis in 100 suspected cases of infectious uveitis. J Ophthal Inflamm Infect. 2018;8:2. https://doi.org/10.1186/s12348-017-0144-1
Agrawal R, Testi I, Bodaghi B, Barisani-Asenbauer T, McCluskey P, Agarwal A, Kempen JH, Gupta A, Smith JR, de Smet MD, Yuen YS, Mahajan S, Kon OM, Nguyen QD, Pavesio C, Gupta V. Collaborative Ocular Tuberculosis Study Consensus Group. Collaborative Ocular Tuberculosis Study Consensus Guidelines on the Management of Tubercular Uveitis-Report 2: Guidelines for Initiating Antitubercular Therapy in Anterior Uveitis, Intermediate Uveitis, Panuveitis, and Retinal Vasculitis. Ophthalmology. 2021;128(2):277–87. https://doi.org/10.1016/j.ophtha.2020.06.052. Epub 2020 Jun 27.
Wakabayashi T, Morimura Y, Miyamoto Y, Okada AA (2003) Changing patterns of intraocular inflammatory diseases. Ocul Immunol Inflamm 11:277–286
Therese KL, Gayathri R, Dhanurekha L et al (2013) Diagnostic appraisal of simultaneous application of two nested PCRs targeting MPB64 gene and IS6110 region for rapid detection of M. tuberculosis genome in culture-proven clinical specimens. Indian J Med Microbiol 31(4):366–369
Verma A, Biswas J, Lakshmipathy D, Ramasubban G, Therese L (2015) Detection of Mycobacterium tuberculosis with nested polymerase chain reaction analysis in the enucleated eyeball in Eales’ disease. Int Ophthalmol 36:413–7. https://doi.org/10.1007/s10792-015-0144-9
Van Gelder RN (2003) CME review: polymerase chain reaction diagnostics for posterior segment disease. Retina 23(4):445–452
Gupta V, Gupta A, Rao NA (2007) Intraocular tuberculosis—an update. Surv Ophthalmol 52(6):561–587
Parchand S, Tandan M, Gupta V et al (2011) Intermediate uveitis in Indian population. J Ophthal Inflamm Infect 1:65–70. https://doi.org/10.1007/s12348-011-0020-3
Agrawal R, Gunasekeran DV, Grant R et al (2017) Clinical features and outcomes of patients with tubercular uveitis treated with antitubercular therapy in the collaborative ocular tuberculosis study (COTS)–1. JAMA Ophthalmol 135(12):1318–1327. https://doi.org/10.1001/jamaophthalmol.2017.4485
Figueira L, Fonseca S, Ladeira I, Duarte R (2017) Ocular tuberculosis: position paper on diagnosis and treatment management. Rev Port Pneumol 23(1):31–38
Madhavan HN, Therese KL, Gunisha P, Jayanthi U, Biswas J (2000) Polymerase chain reaction for detection of Mycobacterium tuberculosis in the epiretinal membrane in Eales’ disease. Invest Ophthalmol Vis Sci 41(3):822–825 PMID: 10711699
Acknowledgements
Ms Esther Sunita Doss for English editing.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Dr JS: manuscript preparation. Dr AJ: Manuscript preparation. Dr NK: Manuscript preparation. Dr JB: Manuscript preparation and supervision. MKJ: PCR related work with manuscript preparation. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Taken.
Consent for publication
Yes.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sreenivasan, J., Jain, A., Kamalini, P.N. et al. Polymerase chain reaction confirmed mycobacterium tuberculosis intermediate uveitis – analysis of 22 eyes of 14 cases from a tertiary care centre in South India: a retrospective study. J Ophthal Inflamm Infect 12, 23 (2022). https://doi.org/10.1186/s12348-022-00296-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-022-00296-0