Abstract
Objective
To report acute multifocal retinitis in association with serologically-proven Coxiella (C) Burnetii infection (Q fever) with endocarditis.
Material and methods
A single case report documented with multimodal imaging.
Results
A 67-year-old cattle breeder presented with a 2-week history of persistent fever, headache, and floaters in both eyes. On examination, his best-corrected visual acuity was 20/20, and there was 1+ vitreous cells in both eyes. Bilateral fundus examination showed multiple small superficial white retinal lesions scattered in the posterior pole and midperiphery associated with a few retinal hemorrhages. These retinal lesions did not stain on fluorescein angiography (FA) and showed focal hyperreflectivity and thickening primarily involving the inner retinal layers on optical coherence tomography (OCT). There also was a band-like hyper-reflective area in the middle retina consistent with paramacular acute middle maculopathy. Transthoracic echocardiogram (TTE) showed a mobile echodensity on the anterior aortic leaflet consistent with a diagnosis of endocarditis. Elisa assays performed on paired serum samples collected 2 weeks apart showed increase in antibodies against C burnetii from 60 IU/ml to 255 IU/ml. The patient was treated with doxycycline 100 mg twice a day for 18 months, with subsequent resolution of the endocarditis. Sequential ocular examinations showed gradual resolution of all acute retinal findings without visible scars.
Conclusion
Acute Q fever, caused by C burnetii infection, should be considered in the differential diagnosis of acute multifocal retinitis. A systematic cardiac assessment with echocardiography is essential for early diagnosis of associated endocarditis and for prompt administration of appropriate antibiotic treatment to improve clinical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Q fever is a worldwide distributed zoonosis caused by C burnetii, an obligate gram-negative intracellular organism [1]. It is primarily transmitted to humans through inhalation of aerosols from contaminated soil or animal waste, with cattle, sheep, and goats being the main reservoirs. Incubation period ranges from 2 to 50 days with a median of 18 days [2]. Most patients remain asymptomatic or develop a nonspecific and self-limiting febrile illness, so that Q fever remains frequently undiagnosed. Endocarditis is the most common and most serious manifestation of chronic Q fever, but other severe acute or chronic complications also have been described including pneumonia, hepatitis, osteomyelitis, endovascular infection, and involvement of the central nervous system [3, 4].
Ocular involvement has rarely been described in the course of Q fever including anterior and posterior uveitis, optic neuropathy, exudative retinal detachment, and abducens palsy [5]. We herein describe a patient who developed acute multifocal retinitis (AMR) in association with acute C burnetii infection with endocarditis.
Case report
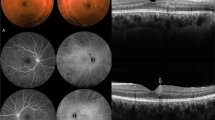
A 67-year-old cattle breeder presented to the emergency department with a 2-week history of persistent fever, headache, and floaters in both eyes. On examination, his best-corrected visual acuity was 20/20 in both eyes. There was no relative afferent pupillary defect, and the ocular motility examination was normal for both eyes. Slit-lamp examination showed a quiet anterior chamber and 1+ vitreous cells bilaterally. Intraocular pressure was 12 mmHg in both eyes. Fundus examination revealed multiple white spots at the level of the inner retina, measuring 200 to 500 microns, scattered in the posterior pole and midperiphery in both eyes. There also were a few retinal hemorrhages, with some them having a white center. A flat, well-circumscribed chorioretinal lesion associating atrophic and hyperpigmented areas was seen along the superotemporal vascular arcade in the left eye (LE) (Fig. 1).
Baseline composite fundus photography shows bilateral small yellow-white retinal lesions in the posterior pole and the periphery (red arrows), with a few retinal hemorrhages, some of which are white-centered (yellow arrow). Note the presence of an old, flat, well-delineated atrophic and pigmented lesion along the superotemporal retinal vascular arcade in the left eye
FA showed a masking effect from retinal hemorrhages, a slight hypofluorescence of retinal infiltrates without late staining, and peripheral retinal vascular leakage.
Swept source-OCT scan (Topcon, DRI triton) through a retinal infiltrate in the LE revealed a focal area of retinal hyperreflective thickening extending from the retinal nerve fiber layer to the outer retinal layers, with sparing of the retinal pigment epithelium and choroid. There also was a band-like hyper-reflective area in the middle retina consistent with paramacular acute middle maculopathy (PAMM) (Fig. 2).
Swept source OCT scan of the LE passing through a retinal infiltrate shows hyperreflective preretinal vitreous dots and a focal area of thickened, hyperreflective inner retina with infiltration extending from the nerve fiber layer to the outer retinal layers, with the ellipsoid zone, retinal pigment epithelium, and choroid clearly delineated and spared (red arrow). Note the presence of a band-like hyperreflective area in the middle retina suggestive of PAMM (yellow arrow)
Cardiac examination showed a diastolic decrescendo murmur. TTE showed a mobile echodensity on the anterior aortic leaflet measuring 20 x 14 mm consistent with a diagnosis of endocarditis (Fig. 3).
Repeated blood cultures were negative. A lumbar puncture was performed revealing an aseptic meningitis with increased lymphocyte and protein levels. Laboratory testing was negative for bartonellosis, rickettsial infection, syphilis, and tuberculosis.
The diagnosis of acute Q fever was made on the basis of SERION enzyme-linked immunosorbent assay (ELISA) results with positive C burnetii phase II IgM and increase in IgG titers from 60 IU/ml to 255 IU/ml on paired serum samples collected 2 weeks apart. The patient was treated with doxycycline 100 mg twice a day for 18 months.
Six weeks after initial presentation, the patient reported the disappearance of floaters. Fundus examination showed a complete resolution of retinal hemorrhages and multifocal retinal lesions, with no residual chorioretinal scars (Fig. 4). Swept source-OCT scan showed the disappearance of the band-like hyper-reflective area in the middle retina corresponding to PAMM and a focal area of inner retinal thinning corresponding to a resolved retinal infiltrate (Fig. 5). Sequential TTE over a two-month follow-up period showed gradual regression of the endocardial vegetation.
Discussion
Our report is the first to describe the association of AMR with a serologically proven systemic C burnetii infection. AMR, previously termed acute multifocal inner retinitis, has been considered to be often idiopathic, but several infectious etiologies have been recognized including cat scratch disease, rickettsial infection, and syphilis [6,7,8,9]. Recent data from Tunisia show rickettsial disease, including rickettsia conorii and rickettsia typhi, to be the most common cause of AMR [10]. In the present case, serological testing showed negative results for rickettsial infection and also for cat scratch disease and syphilis. The presence of an associated blood-culture negative endocarditis in a patient with a history of animal contact raised our suspicion of Q fever. The diagnosis was confirmed by the detection of high titers of anti- C burnetii antibodies and the patient accordingly was treated with oral doxycycline. Indirect immunofluorescent assays (IFA) is considered the gold standard for the diagnosis of Q fever ; alternatively, ELISA may be done [11].
The ocular disease pattern of our patient conformed to most of the previously reported features of AMR, especially with regard to the systemic febrile illness, minimal vision impairment, characteristic multiple inner retinitis spots associated with mild vitritis, and benign and self-limiting clinical course.
Endocarditis has been considered as an almost exclusive complication of chronic Q fever. Our findings, consistent with previous recent data, show that acute endocarditis, readily detectable with TTE, can affect a sizable subset of patients with acute Q fever [12,13,14]. Therefore, early diagnosis of Q fever and associated endocardial involvement is of utmost importance for prompt initiation of antibiotic treatment to prevent persistent endocarditis and related morbidity and mortality.
Multifocal superficial retinal infiltrates associated with Q fever may result from intraretinal multiplication of C burnetii, or from immune-mediated response to bacterial antigens caused by the deposition of immune complexes, inflammatory cells, or antibodies through retinal vessels [15, 16]. The vascular tropism of C burnetii also is reflected in our patient in the presence of associated retinal hemorrhages, retinal vascular leakage, and retinal vascular occlusion in the form of PAMM.
This case shows that C burnetii infection should be considered in the differential diagnosis of AMR associated with systemic febrile illness. Serological confirmation is required for a definitive diagnosis that could be challenging. A systematic echocardiography is of utmost importance for early detection of disease-related endocarditis and for prompt administration of appropriate antibiotic treatment to improve clinical outcomes.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AMR:
-
Acute Multifocal Retinitis
- C:
-
Coxiella
- FA:
-
Fluorescein Angiography
- LE:
-
Left Eye
- OCT:
-
Optical Coherence Tomography
- PAMM:
-
Paramacular Acute Middle Maculopathy
- TTE:
-
Transthoracic Echocardiogram
References
Angelakis E, Raoult D (2010) Q Fever Vet Microbiol 140:297–309
Todkill D, Fowler T, Hawker JI (2018) Estimating the incubation period of acute Q fever, a systematic review. Epidemiol Infect 146(6):665–672
Derrick EH (1973) “Q” fever, new fever entity: clinical features, diagnosis and laboratory investigation. Med J Aust 2:281–299
Kazar J (2005) Coxiella burnetii infection. Ann N Y Acad Sci 1063:105–114
Million M, Halfon J, Le Lez ML, Drancourt M, Drancourt M, Raoult D (2011) Relapsing uveitis and optic neuritis due to chronic Q fever. Br J Ophthalmol 95(7):1026–7 (1038-9)
Jones MR, Cunningham ET Jr (1997) Bartonella henselae-associated AMR in a patient with acquired immunodeficiency syndrome. Retina. 17(5):457–459
Lukas JR, Egger S, Parschalk B, Stur M (1998) Bilateral small retinal infiltrates during rickettsial infection. Br J Ophthalmol 82:1217–1218
Khairallah M, Ben Yahia S, Toumi A, Jelliti B, Loussaief C, Romdhane FB, Messaoud R, Chakroun M (2009) Ocular manifestations associated with murine typhus. Br J Ophthalmol 93(7):938–942
Cunningham ET Jr, Schatz H, McDonald HR, Johnson RN (1997) Acute multifocal retinitis. Am J Ophthalmol 123(3):347–357
Khochtali S, Gargouri S, Zina I, Ksiaa N, Abroug SZ et al (2018) Acute multifocal retinitis: a retrospective review of 35 cases. J Ophthalmic Inflamm Infect 8 8:18
Slabá K, Skultéty L, Toman R (2005) Efficiency of various serological techniques for diagnosing Coxiella burnetii infection. Acta Virol 49(2):123–127
Million M, Thuny F, Bardin N, Angelakis E, Edouard S, Bessis S et al (2016) Antiphospholipid Antibody Syndrome with Valvular Vegetations in Acute Q Fever. Clin Infect Dis 62:537–544
Bitsori M, Vergadi E, Germanakis I, Raissaki M, Galanakis E (2020) Case Report: Α Case of Endocarditis and Embolic Stroke in a Child, Suggestive of Acute Q Fever Infection. Am J Trop Med Hyg 103(4):1435–1438
Melenotte C, Epelboin L, Million M, Hubert S, Monsec T, Djossou F et al (2019) Acute Q Fever Endocarditis: A Paradigm Shift Following the Systematic Use of Transthoracic Echocardiography During Acute Q Fever. Clin Infect Dis 69(11):1987–1995
Khairallah M, Ladjimi A, Chakroun M, Messaoud R, Yahia SB, Zaouali S, Romdhane FB, Bouzouaia N (2004) Posterior segment manifestations of Rickettsia conorii infection. Ophthalmology. 111(3):529–534
Lumio J, Penttinen K, Pettersson T (1981) Q fever in Finland: clinical, immunological and epidemiological findings. Scand J Infect Dis 13:17–21
Acknowledgements
Ministry of Higher Education and Research of Tunisia
Funding
Authors received no funding
Author information
Authors and Affiliations
Contributions
All authors contributed to the study concept and design, and all authors acquired and interpreted study data. AM, FA, MK, SA, HIHA and ABHK collected data. AM, FA, MK and SM drafted the manuscript. RM and MK provided critical manuscript revisions and supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from our patient.
Consent for publication
Oral and written consent to publication of the case was obtained from the patient. This report does not contain any personal information that could lead to the identification of the patient.
Competing interests
None of the authors has any financial/conflicting interests to disclose
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahmoud, A., Abid, F., Khairallah, M. et al. Acute multifocal retinitis in a patient with Q fever (Coxiella Burnetii infection) with endocarditis. J Ophthal Inflamm Infect 12, 19 (2022). https://doi.org/10.1186/s12348-022-00295-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-022-00295-1