Abstract
Background
The management of leiomyomas, the most common benign mesenchymal tumours, remains highly debated. This case report presents the first laparoscopic enucleation of an extravesical bladder leiomyoma in Indonesia.
Case presentation
A 48-year-old man presented with a lower abdominal mass. An abdominopelvic computed tomography scan showed a solid tumour mass in the right anterolateral wall of the bladder. To excise the mass, it was planned for the patient to undergo laparoscopic enucleation. The mass was removed intact, and a frozen section was taken to determine the malignancy profile. Histopathological examinations, followed by immunohistochemical examinations, confirmed the diagnosis of leiomyoma.
Conclusions
Laparoscopic enucleation is a promising option for managing bladder masses. It is a minimally invasive procedure with optimal results for preserving bladder function. Prior to the surgery, imaging studies and cystoscopy examination are mandatory.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.1 Background
Urinary bladder tumours are almost always carcinomas, with mesenchymal tumours accounting for approximately 1–5% of all bladder tumours. Leiomyomas are the most common benign mesenchymal tumours, accounting for 35% of all mesenchymal tumours and 0.43% of all bladder tumours [1]. Bladder leiomyoma is a rare occurrence typically observed in women aged 40–50. Although the incidence of bladder leiomyomas is comparable between men and women, the prevalence is approximately three times higher in women, with a female-to-male ratio of 2:5 [1, 2]. The underlying pathophysiological mechanisms leading to tumour development remain elusive; however, it is hypothesized that hormonal influences, particularly during the reproductive age, may play a significant role [1,2,3]. Leiomyomas manifest in three distinct locations—intravesical, intramural, and extravesical. Intravesical occurrences constitute the majority, accounting for 63–86% of cases, while extravesical leiomyomas are observed in 11–30%, and intramural leiomyomas are found in 3–7% [1].
The best treatment method for bladder leiomyoma is currently being debated [1,2,3,4]. Abdominal, vaginal, laparoscopic, or transurethral resection, as well as segmental surgical excision or partial cystectomy, are several management options [5, 6]. The tumour's size and anatomical location largely determine the management strategies. Small intravesical leiomyomas can be removed by transurethral resection of the bladder tumour (TURBT); however, bigger intramural or extravesical leiomyomas sometimes require open resection [5]. In this case report, we present the laparoscopic enucleation of an extravesical bladder leiomyoma.
2 Case presentation
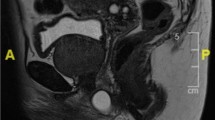
A 48-year-old man presented to our hospital with a lower right infraumbilical mass, accompanied by an absence of urinary symptoms, and significant physical findings. Urinalysis results were within normal limits. The imaging findings from contrast abdominopelvic computed tomography (CT) scans showed the presence of a solid tumour mass with a size of 2.35 × 2 × 2.8 cm in the right anterior superolateral wall of the bladder (Fig. 1). Our protocol entails confirming the location of the bladder tumour, whether it is intravesical or extravesical. If the tumour is intravesical, the preferred management option is transurethral resection of bladder tumour (TURBT), followed by appropriate management based on bladder tissue pathology results. If the tumour is extravesical, the preferred management option is surgery intervention via laparoscopic or open approach utilizing frozen section. As the mass was deemed resectable, we opted for tumour removal with frozen section as it can be managed in more efficiently in one stage. If it is not, biopsy is then performed initially.
The patient granted consent and then underwent laparoscopic enucleation intraperitoneally in the lithotomy position. Before the laparoscopic procedure, a cystoscopy was performed to assess the interior of the bladder, revealing an extravesical mass protruding within the right anterior wall. The lack of polypoid, pedunculated, or well-encapsulated lesions, along with the presence of the tumour surrounded by the bladder wall muscle, indicates that the origin of the tumour is neither intravesical nor intramural. To excise the mass, triangular trocars were inserted, consisting of one supraumbilical 12-mm trocar for the camera port and two 10-mm trocars for the working port. The first trocar is inserted just above the umbilicus and slightly to the left of the midline. The two working port trocars were placed in the lower abdomen, often just above the pubic symphysis and placed laterally on the contralateral lower abdomen. The urachus and peritoneum (Fig. 2A) were identified and dissected towards the bladder, where the mass was located as depicted in the CT scan (Fig. 2B, C). The mass was excised and removed in toto from the bladder. A urethral catheter was passed and eventually removed 7 days later.
A frozen section was performed to determine the malignant profile. We performed the peritonealization procedure laparoscopically (Fig. 2D), the opened peritoneum was sutured, and active bleeding was assessed and found to be absent. No challenges in terms of ergonomics were faced by the operator.
The histopathological examination obtained from the frozen section (Fig. 3) revealed the mass was composed of syncytial cells that were growing hyperplastically, arranged in rows that partially formed a range structure. The cell nuclei were oval to spindle-shaped, mildly pleomorphic, hyperchromatic, and partially vesicular, with clear daughter nuclei, and mitosis was observed. The stroma had some myxoid hyaline degeneration with dilated blood vessels. No visible necrotic areas were observed in this preparation. The immunohistochemical results (Fig. 4) showed that vimentin and smooth muscle actin (SMA) were positive, desmin was focally positive, S-100 was negative, and Ki-67 was positive in 5–10% of the tumour cells, which supported the diagnosis of leiomyoma of the bladder.
No post-operative complications were observed and were eventually discharged 5 days after the procedure. The patient is scheduled for a 1-year follow-up and is recommended to return if any complications arise.
3 Discussion
Bladder tumours of a benign nature encompass various types, including leiomyomas, fibromyomas, rhabdomyomas, fibromas, osteomas, and myxomas [5]. Among these, leiomyomas are the most frequently occurring benign tumour in the bladder, albeit a rare entity [7]. The exact pathophysiology of these tumours remains unclear, although four theories have been put forth to explain their occurrence. These include hormonal imbalances, dysontogenesis, perivascular inflammation causing metaplastic transformation of the bladder vascular supply, and bladder musculature infection resulting in inflammation and the development of benign tumours [1].
The most common clinical characteristics are urinary voiding symptoms [3]. Patients with bladder leiomyoma are mostly asymptomatic (50–70%), but could be identified with obstructive symptoms (49%), irritative symptoms (38%), and haematuria (11%) [1, 3, 8]. In this patient, such symptoms were absent.
Ultrasound, CT scan, and MRI may help in the diagnosis of bladder leiomyoma. Pelvic ultrasonography can detect a homogeneous mass within the bladder with a hypoechoic or modestly hyperechoic appearance and evaluate its relationship to the uterus and vagina. On CT scan, fibroids, typically observed as soft tissue density lesions with the potential for coarse peripheral or central calcification, can distort the usually smooth uterine contour, while their enhancement pattern remains variable. MRI has the capability to distinguish mesenchymal tumours from the more prevalent transitional cell tumours, including their malignant form, leiomyosarcoma. It offers enhanced details regarding tumour size and localization. When examining composition and its relation to the bladder wall, MRI is the preferred imaging modality. In instances akin to this case, where extravesical growth of bladder cancer, a rare occurrence, eludes detection through cystoscopy, MRI becomes instrumental in identification [2, 9]. Nonetheless, because bladder leiomyoma is made out of bundles of muscle fibres separated by connective tissue, histopathological examinations remain the gold standard for diagnosis, and imaging techniques sometimes cannot rule out malignancy appropriately [5, 6, 10].
The primary treatment for small and easily accessible intravesical-type bladder leiomyomas is transurethral resection of the bladder tumour (TURBT) [1, 3, 11]. But for large tumours, laparoscopic enucleation was preferred. In such circumstances, the procedure is preferred compared to a partial cystectomy as it is less invasive and better at preserving bladder function post-operation [12]. Enucleation or partial cystectomy is typically carried out through a vaginal, abdominal, or laparoscopic method for extravesical and intramural tumours [11]. However, if malignancy cannot be ruled out, Alanya Tosun et al. suggested open surgery to prevent tumour seeding [11]. Hong et al. stated that large extravesical tumour surgery (partial cystectomy or enucleation) can be done with a laparoscopic approach. In their case, laparoscopic enucleation managed to dissect the tumour easily using grasping forceps without electrocoagulation to avert thermal injury to the bladder and without complications upon confirmation with methylene blue into the Foley catheter [6].
Another alternative if frozen section examination is unavailable would be to perform laparoscopic wide excision with a 2-cm margin around the tumour or refer to a facility capable of conducting frozen section examination. In the event of malignancy, management will be tailored to the specific type of tumour obtained based on histopathology results, whether it entails surgery, systemic therapy, or radiotherapy. The management may not be limited to enucleation and observation alone but may necessitate cystectomy with or without adjuvant therapy.
The leiomyoma in our patient was identified as an extravesical mass. Laparoscopic enucleation was chosen as a treatment because it is minimally invasive and has optimal results in preserving bladder function. Fortunately, the bladder and tumour borders are distinct, allowing for complete enucleation. Injury of the ureter and bladder, and severe haemorrhage of the pelvic organs can be seen as complications. Although, considering the reported cases, it is mandatory that the surgeon be able to repair the bladder laparoscopically in terms of minimally invasive technique [6].
When the excision is extensive enough, surgical excision has a very high success rate and should always be considered, because it leaves very low recurrence rates and no symptoms after surgery [1, 7]. Surveillance imaging for 2–3 years after tumour excision may be considered to rule out recurrence. Furthermore, the use of selective progesterone receptor modulators (SPRM) and gonadotropin-releasing hormone (GnRH) agonists has been reported to prevent the growth of uterine leiomyoma. As most bladder leiomyomas occur in females, the same hormone replacement therapy might have potential for preserving the urinary tract [12]. But until now, there are no guidelines available. Although bladder leiomyomas often resemble malignant lesions or radiological findings, their malignant potential is exceedingly low, standing at 0.1%. Hence, in ensuring the best outcome for the patient, extra inpatient days were decided for a more thorough observation. Moreover, there are no reported instances of bladder leiomyomas undergoing malignant transformation, indicating a favourable prognosis [13].
4 Conclusions
In summary, we present a rare case of male asymptomatic bladder leiomyoma. Imaging and histological evaluation are used to make a diagnosis, with open resection indicated upon diagnosis of extravesical leiomyoma. For bigger tumours, laparoscopic enucleation is a promising, supported with the success of this patient’s procedure. However, more extensive research and extended follow-up are required to properly assess these methods.
Availability of data and materials
The data that support the findings of this study are not publicly available due to the containing information that could compromise the privacy of research participants, but are available from the MAM upon reasonable request. All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Abbreviations
- GnRH:
-
Gonadotropin-releasing hormone
- SPRM:
-
Selective progesterone receptor modulators
- TURBT:
-
Transurethral resection of the bladder tumour
References
Khater N, Sakr G (2013) Bladder leiomyoma: presentation, evaluation and treatment. Arab J Urol 11(1):54–61
Erdem H, Yildirim U, Tekin A, Kayikci A, Uzunlar AK, Sahiner C (2012) Leiomyoma of the urinary bladder in asymptomatic women. Urol Ann 4(3):172–174
Ortiz M, Henao DE, Maya WC, Ceballos MM (2013) Leiomyoma of the urinary bladder: a case report. Int Braz J Urol 39:432–434
Kölükçü E, Parlaktaş BS, Deresoy FA, Beyhan M, Özbek LM (2019) Bladder leiomyoma: a case report and brief review of literature. J Surg Med 3(5):411–413
Pramod SV, Safriadi F, Hernowo BS, Dwiyana RF, Ksatriapraja RA (2020) A large bladder leiomyoma. Urol Case Rep 1(32):101211
Hong SY, Lee TS, Kim JH (2009) Laparoscopic enucleation of a bladder leiomyoma. J Minim Invasive Gynecol 16(6):772–774
Singh O, Gupta S, Hastir A (2011) Laparoscopic enucleation of leiomyoma of the urinary bladder: a case report and review of the literature. Urol J 8(2):155–8
Al-Hendy A, Myers ER, Stewart E (2017) Uterine fibroids: burden and unmet medical need. Semin Reprod Med 35(6):473–480. https://doi.org/10.1055/s-0037-1607264
Zachariou A, Filiponi M, Dimitriadis F, Kaltsas A, Sofikitis N (2020) Transurethral resection of a bladder trigone leiomyoma: a rare case report. BMC Urol 20:1–5
AlanyaTosun S, Sozen H, Tefik T, Iyibozkurt A, Salihoglu Y (2021) Giant sized extravesical bladder leiomyoma mimicking uterine cervical leiomyoma: a case report with 8 years’ postoperative follow-up and a review of the literature. J Istanbul Fac Med-Istanbul Tip Fakultesi Dergisi 84(3):448–453
Yoshioka T, Kawakita M, Kameoka H (2019) Cystoscope-assisted laparoscopic enucleation of a large progressive bladder leiomyoma. J Endourol Case Rep 5(3):120–123. https://doi.org/10.1089/cren.2019.0015
McNall S, Park T, Gopal N, Spencer E, Vemulakonda LA, Choudhury M et al (2022) Case series—prioritizing bladder-sparing treatments in patients with urinary tract leiomyoma: a report of three cases and updated literature review. Can Urol Assoc J. 16(11):55. https://doi.org/10.5489/cuaj.7745
Mitchell K, Barnard J, Luchey A (2019) Locally recurrent leiomyoma of the bladder refractory to visually complete transurethral resection: an indication for cystoprostatectomy. Case Rep Urol 25(2019):1086575. https://doi.org/10.1155/2019/1086575
Acknowledgements
Not applicable.
Funding
This case report did not receive any financial support.
Author information
Authors and Affiliations
Contributions
MAM and IAB contribute to the conception or design of the work, the acquisition, analysis, and interpretation of data for the work. IAB, FR, DI, EUI, and RBS draft the work and revise it critically for important intellectual content. IAB and FR approve the final version to be published. MAM and IAB agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by our local committee with number of approval KET-1009/UN2.F1/ETIK/PPM.00.02/2023. The patient has given consent to participate in this research.
Consent for publication
Written informed consent was obtained from the parent/legal guardian of the patient for publication of the details of their medical case and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mahfuz, M.A., Bramono, I.A., Rahman, F. et al. Laparoscopic Enucleation of an Extravesical Bladder Leiomyoma: A Case Report. Afr J Urol 30, 25 (2024). https://doi.org/10.1186/s12301-024-00426-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-024-00426-1