Abstract
Background
Controversy persists regarding the superiority of partial nephrectomy (PN) versus radical nephrectomy (RN) in pT2a renal cell carcinoma (RCC) tumors. In this study we aimed to compare survival and clinical outcomes between these two techniques in Iran.
Methods
In this retrospective cohort, 96 patients who underwent either RN or PN for their pT2a RCC tumors were included. Overall survival (OS), cancer specific survival (CSS), recurrence free survival (RFS), major postoperative complications and postoperative renal function were compared, subsequently.
Results
During a mean follow-up time of 57.3 ± 24.0 months, OS, CSS, RFS, postoperative bleeding, postoperative urinary leak, postoperative prolonged wound drainage and length of hospital stay were not statistically different between RN versus PN patients (p = .09, .42, .09, .27, .27, .06 and .78, respectively). Nevertheless, post-operative creatinine was significantly lower in PN patients compared to RN patients (p = .01). Our multivariable cox regression models indicated that higher Fuhrman grade detrimentally affected CSS (p < .01) and increased the risk of recurrence (p = .02). Moreover, prior history of ischemic heart disease (IHD) was a significant determinant of lower OS (p = .03) and RFS (p = .02).
Conclusions
In conclusion, our data suggested that although OS, CSS, RFS and major postoperative complications were similar between PN and RN, PN may offer better postoperative renal function and can be thus regarded as the superior approach in pT2a tumors.
Similar content being viewed by others
1 Background
It has been estimated that more than 400,000 new cases of kidney cancer are diagnosed globally, every year [1]. This high incidence illuminates the significance of choosing the proper surgical technique to lower the mortality and morbidity rate of this cancer. Radical and partial nephrectomy (RN and PN, respectively) are the two feasible surgical approaches for the management of renal tumors [2, 3].
Previous studies have demonstrated that PN is superior to RN in lower stage (T1) renal tumors due to the ability to preserve more nephrons while having similar oncological outcomes [4]. However, the optimal surgical technique in higher stage tumors (T2) still remains controversial. Conventionally, RN was considered the best choice in T2 renal tumors [5]. Nevertheless, recent studies have shown that PN may be a suitable alternative to RN due to better survival and postoperative renal function, despite possibly higher complications [6,7,8]. Moreover, although there are still some concerns about impaired cancer control in PN, it is becoming more popular due to the abovementioned advantages [9].
However, the condition is quite different in under-resourced countries, many of which fail to comply with the developing trend towards wider PN adoption due to limited access to modern technology and difficulties in surgical training, among other factors [10]. To the best of our knowledge, no study has compared oncologic and clinical outcomes between RN and PN in pT2a RCC in developing countries. Therefore, we aimed to investigate this issue in Iran.
2 Methods
2.1 Study population and outcome parameters
In this retrospective cohort study conducted from May 2008 to May 2019, we investigated the health records of all patients who underwent surgical resection of pT2a (7–10 cm) renal tumors at two referral hospitals in Tehran, Iran. The operations were performed by the same surgical team. Only patients with renal cell carcinoma (RCC) diagnosed through clinical and imaging studies, who were candidates for either PN or RN were included. Patients with metastatic tumors in preoperative clinical staging, tumor-induced thrombosis and urothelial carcinoma were excluded. In patients with a prior history of chronic kidney disease (CKD) or those with a single functional kidney or bilateral tumor, PN was the preferred surgical approach. In other cases, the surgical approach was chosen through shared decision-making with the patient, following a comprehensive discussion of the advantages and disadvantages of either of the surgical approaches. The patients were then grouped based on surgical approach (RN or PN). Demographics, preoperative comorbidities, length of hospital stay (LOS), recurrence free time, major postoperative complications, postoperative serum creatinine levels, and survival status were extracted from the patients’ health records. Data regarding the pathologic features of the tumors were obtained from pathologic reports. Since the standard Fuhrman grading is not suitable for chromophobe RCCs, no grade was reported for these tumors and they were all assigned a not applicable (N/A) note throughout our study [11]. The primary outcomes assessed in this study were overall and cancer specific survival rates (OS and CSS, respectively). LOS, RFS, postoperative complications and postoperative renal function were also compared between RN and PN techniques. Additionally, we also assessed the possible effect of demographics, underlying comorbidities and tumor features on OS, CSS and RFS in this study.
2.2 Data analysis
All data were analyzed using SPSS software, version 23 (IBM Corp., Armonk, NY, USA). Quantitative and qualitative data were reported as mean ± standard deviation or median (interquartile range) and frequency (percentage), respectively. The assumption of normality was checked by Kolmogorov–Smirnov test. For between-group comparisons of quantitative data, independent T-test or Mann–Whitney U test was performed based on the normality of the data. The associations between qualitative variables were assessed by Chi-squared tests. Multivariable binary logistic regressions were used to adjust for the possible confounding variables in binary outcomes. OS, CSS and RFS were evaluated using Kaplan–Meier (Log-rank) and multivariable cox regression analyses. A p-value of < 0.05 was considered statistically significant in all tests.
3 Results
3.1 Patient demographics and characteristics
A total of 96 patients were included in our study. The mean age of the participants was 55.0 ± 13.8 (range: 27–81) years. Of the total participants, 53 (55.2%) individuals were male and 43 (44.8%) were female. Among the patients, 38 (39.6%) underwent RN, while 58 (60.4%) underwent PN. The mean follow up time was 57.3 ± 24.0 months. Table 1 provides a comparison of the demographics and baseline clinical characteristics between the RN and PN patients. As observed in Table 1, patients who underwent RN had significantly larger renal tumor size compared to the PN group (p < 0.01). Pathologic positive lymph node (pLN+) rate was also significantly higher in RN versus PN (42.1% vs. 19.0%, p = 0.01). Nevertheless, after adjusting for tumor size in a multivariable binary logistic regression, surgical approach did not significantly predict pLN+ (odds ratio (OR) [95% confidence interval (CI)] = 2.42 [0.87, 6.74], p = 0.09). No significant difference was observed in any other factor. It is worth noting that none of the patients in our study had rhabdoid or sarcomatoid pathologic subtypes.
3.2 Clinical outcomes
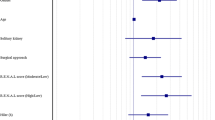
As depicted in Table 2 and Fig. 1, no statistically significant differences were observed in OS, CSS, RFS, postoperative bleeding, postoperative urinary leak, postoperative prolonged wound drainage (duration > 72 h), and LOS between RN and PN (p = 0.09, 0.42, 0.09, 0.27, 0.28, 0.06, 0.78, respectively). However, postoperative fever and surgical site infection (SSI) were significantly higher in the RN group (p < 0.01 and p = 0.03, respectively). Furthermore, post-operative creatinine levels were significantly higher in the RN group compared to the PN group (1.4 ± 0.5 vs. 1.3 ± 0.6 mg/dl, p = 0.01). Notably, a single case of pulmonary embolism was also observed in the RN group. Considering the significant difference in tumor size between RN and PN patients, we further subcategorized the tumors based on 1-cm size stratifications and compared OS, CSS and RFS between these groups. As shown in Table 3, there was not any difference between PN and RN in terms of CSS in different size subcategories. However, in tumors between 7 and 8 cm, PN demonstrated a significantly better OS (89.8% vs. 66.7%, p = 0.02) and a significantly better RFS (89.8% vs. 66.6%, p = 0.02). No significant differences in OS and RFS were observed between RN and PN in other size subcategories.
We also evaluated the potential impact of other variables on OS, CSS and RFS. Our univariable Log-rank analyses (Additional file 1: Table S1) showed that tumor size, Fuhrman grade, personal history of ischemic heart disease (IHD) and CKD significantly affected both OS (p = 0.01, < 0.01, 0.04 and 0.04, respectively) and RFS (p = 0.01, < 0.01, 0.03 and 0.04, respectively). However, after incorporating the significant variables into a multivariable cox regression for OS, tumor size, Fuhrman grade and previous history of CKD lost their significance (p = 0.32, 0.08 and 0.817, respectively) as predictors of OS and only a prior history of IHD remained significant (hazards ratio (HR) [95% CI] = 6.08 [1.09, 33.85], p = 0.03). A multivariable cox analysis for RFS revealed that tumor size and prior history of CKD did not significantly affect the risk of recurrence (p = 0.49 and 0.99, respectively). However, a prior history of IHD (HR [95% CI] = 5.60 [1.13, 33.85], p = 0.04) significantly increased the risk of recurrence. Moreover, the same model indicated that while tumor grade was significant as a whole (p = 0.02), none of its sublevels were individually significant, suggesting only a trend towards a higher risk of recurrence in higher Fuhrman grades. In respect of CSS, Fuhrman grade was the only significant factor (p < 0.01; Additional file 1: Table S1).
4 Discussion
During the last 2 decades, PN has gained attention as a plausible alternative to RN in T2 tumors, primarily due to reported better OS, CSS, postoperative renal function and lower recurrence rates [6, 7, 12,13,14,15]. Nevertheless, the sophisticated nature of PN in large renal tumors (≥ T2) requires longer operative hours and poses an increased risk of intraoperative blood loss and perioperative complications. These challenges have hindered the consensus on the superiority of PN in T2 tumors [8, 16,17,18].
In this study, our results indicated that OS, CSS, RFS, major postoperative complications and LOS were not significantly different between PN and RN in pT2a RCC tumors. However, postoperative renal function was significantly better in the PN group. Moreover, our data suggested that PN outperformed RN with regards to OS and RFS in tumors at the lower end of the pT2a size spectrum (7–8 cm). These findings were consistent with previous investigations on T2 renal tumors; most of which also reported similar CSS and OS between RN and PN patients while suggesting better renal function with PN [6, 8, 17,18,19,20]. It is noteworthy that earlier studies presented conflicting results and suggested that PN may be associated with poorer survival outcomes [9]. It appears that with the increased adoption of PN for T2 tumors among urologic surgeons over the last decade, their experience has improved, resulting in better outcomes in recent years. This perspective is especially supported by two meta-analyses published within the last 5 years, both emphasizing better survival and postoperative renal function with PN [8, 16]. A notable finding of our study was the significantly higher rate of postoperative fever among RN patients. Previously, a study demonstrated that fever grade is positively correlated with RCC tumor size [21]. Therefore, it can be postulated that the higher incidence of postoperative fever in the RN group was due to their significantly larger tumors. Moreover, the RN group also exhibited a significantly higher rate of SSI; which may have contributed to the increased rate of postoperative fever in this group. The higher incidence of SSI, in the RN group can be attributed to their larger tumor size, a known risk factor for postoperative SSI [22]. Notably, although 3 (5.2%) patients in the PN group experienced postoperative urinary leakage, none in the RN group reported this complication. However, this difference was not statistically significant. Our initial analysis also showed a significantly higher rate of pLN+ in the RN group. However, after accounting for the established confounding effect of tumor size [23], surgical approach lost its significance as a predicator of pLN+.
Our analyses revealed that higher Fuhrman grade was the only predictive factor associated with worse CSS in pT2a tumors. Parallel to these findings, Kopp et al. [17] also demonstrated a significant role for tumor grade in this aspect (p < 0.001). Nevertheless, a contradictory report by de Saint Aubert et al. [24] suggested that Fuhrman grade does not influence CSS (p = 0.10). This inconsistency could be attributed to a smaller sample size and possible selection bias in the latter study. Our multivariable analyses of OS rates also demonstrated that after accounting for possible confounding variables, tumor grade did not have any effect on OS in pT2a patients. These findings were in line with previous studies that have generally denied a meaningful effect of tumor grade on OS [9, 17, 24, 25]. A recently published meta-analysis underpinned this finding by showing that Fuhrman grade does not influence OS [8]. Another notable finding of our study was the possible role of underlying IHD in predicting OS and RFS in pT2a stage. Former studies have conflicting views regarding the impact of underlying comorbidities on OS in RCC, with some suggesting a prominent detrimental impact of comorbidities, while others disagreeing [24, 26]. However, to the best of our knowledge, none of these studies have specifically evaluated the potentially detrimental influence of IHD as an independent prognostic factor for worse OS.
Although not statistically significant, our analyses also indicated that RFS was lower in RN versus PN (31.6% vs. 15.5%, p = 0.09) in pT2a patients. Moreover, PN patients had significantly better RFS compared to RN specifically in the lower size range (7–8 cm) within the pT2a spectrum. This topic has been extensively studied in previous investigations, and the cumulative effect has been evaluated in two meta-analyses, both emphasizing on the lower risk of recurrence among PN patients [8, 16]. Our multivariable analysis suggested that higher Fuhrman grade and a prior history of IHD significantly increased the risk of tumor recurrence. While ample evidence exists regarding the role of higher Fuhrman grade in increasing the risk of recurrence in RCC [27,28,29], the possible role of IHD has never been investigated in this context before. Previously, a comprehensive review suggested that underlying cardiac diseases can increase the risk of solid tumor recurrence through the reprogramming of the innate immune system [30]. This may partly explain our finding of a higher recurrence rate in RCC patients with a personal history of IHD. In concordance with previous studies, our data also demonstrated that despite LOS was lower in the RN group in pT2a tumors; this difference was not statistically significant; refuting the inferiority of PN in this aspect [17, 24,25,26].
Our study had some limitations. Firstly, the tumors in the RN group were significantly larger compared to PN group, which we attempted to address by subgrouping tumor sizes into 1cm stratifications. Moreover, the study was conducted in a retrospective manner and some important variables that could affect the choice of surgical approach (e.g., R.E.N.A.L. nephrometry score) or ultimate survival (e.g., lymphovascular invasion, capsular invasion, or tumor necrosis on pathology) were unavoidably omitted due to incomplete medical records. Moreover, although our data suggested superiority for PN in terms of OS and RFS in the lower end of the pT2a size spectrum, multivariable models must have been fitted to make robust conclusions in this regard; which was unattainable due to the relatively small sample size in this size subgroup. Lastly, the retrospective design of our study and the potential defects in our health records may have introduced selection and information bias. However, the proposition of the novel perspective of 1cm size stratifications and comparison of outcomes within these sublevels, the involvement of the same surgical team in all operations, and being among the first studies in this regard from the Middle East and North African region contribute to the significance of our findings.
5 Conclusions
In conclusion, our data suggested that OS, CSS, RFS, major postoperative complications, and LOS were comparable between the two surgical approaches in pT2a patients. However, postoperative renal function was significantly better in the PN group. Based on these findings, PN may be considered as the superior surgical approach for pT2a RCC patients.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CKD:
-
Chronic kidney disease
- CSS:
-
Cancer specific survival
- LOS:
-
Length of hospital stay
- N/A:
-
Not applicable
- OS:
-
Overall survival
- pLN+:
-
Pathologic positive lymph node
- PN:
-
Partial nephrectomy
- RCC:
-
Renal cell carcinoma
- RFS:
-
Recurrence free survival
- RN:
-
Radical nephrectomy
- SSI:
-
Surgical site infection
References
Observatory, G.C. Kidney (2020). https://gco.iarc.fr/today/data/factsheets/cancers/29-Kidney-fact-sheet.pdf. Cited 30 Jan 2023
Wasserman M, Sobel D, Pareek G (2020) Choice of surgical options in kidney cancer and surgical complications. Semin Nephrol 40(1):42–48
Zahir M et al (2023) Current status and future perspectives of Wilms tumor treatment in Iran. Ann Med Surg (Lond) 85(5):1425–1429
Ljungberg B et al (2015) EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 67(5):913–924
McDougal WS et al (2015) Campbell-Walsh urology 11th edition review E-book. Elsevier Health Sciences, Amsterdam
Mühlbauer J et al (2020) Partial nephrectomy preserves renal function without increasing the risk of complications compared with radical nephrectomy for renal cell carcinomas of stages p T2–3a. Int J Urol 27(10):906–913
Rinott Mizrahi G et al (2018) Comparison of partial and radical laparascopic nephrectomy: perioperative and oncologic outcomes for clinical T2 renal cell carcinoma. J Endourol 32(10):950–954
Huang R et al (2021) Partial nephrectomy versus radical nephrectomy for clinical T2 or higher stage renal tumors: a systematic review and meta-analysis. Front Oncol 11:2182
Jeldres C et al (2009) Partial versus radical nephrectomy in patients with adverse clinical or pathologic characteristics. Urology 73(6):1300–1305
Ologunde R et al (2014) Surgical care in low and middle-income countries: burden and barriers. Int J Surg 12(8):858–863
Delahunt B et al (2007) Fuhrman grading is not appropriate for chromophobe renal cell carcinoma. Am J Surg Pathol 31(6):957–960
Tsivian M et al (2017) Laparoscopic partial nephrectomy for tumors 7cm and above. Perioperative outcomes. Int Braz J Urol 43:857–862
Streja E et al (2018) Radical versus partial nephrectomy, chronic kidney disease progression and mortality in US veterans. Nephrol Dial Transplant 33(1):95–101
Huang WC et al (2006) Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol 7(9):735–740
Kim SP, Thompson RH (2013) Kidney function after partial nephrectomy: current thinking. Curr Opin Urol 23(2):105–111
Mir MC et al (2017) Partial nephrectomy versus radical nephrectomy for clinical T1b and T2 renal tumors: a systematic review and meta-analysis of comparative studies. Eur Urol 71(4):606–617
Kopp RP et al (2014) Survival outcomes after radical and partial nephrectomy for clinical T 2 renal tumours categorised by RENAL nephrometry score. BJU Int 114(5):708–718
Breau RH et al (2010) Outcome of stage T2 or greater renal cell cancer treated with partial nephrectomy. J Urol 183(3):903–908
Amparore D et al (2021) Comparison between minimally-invasive partial and radical nephrectomy for the treatment of clinical T2 renal masses: results of a 10-year study in a tertiary care center. Minerva Urol Nephrol 73(4):509–517
Reix B et al (2018) Overall survival and oncological outcomes after partial nephrectomy and radical nephrectomy for cT2a renal tumors: a collaborative international study from the French kidney cancer research network UroCCR. Prog Urol 28(3):146–155
Foggo V, Cavenagh J (2015) Malignant causes of fever of unknown origin. Clin Med (Lond) 15(3):292–294
Sasaki H et al (2018) Risk factors for surgical site infection after soft-tissue sarcoma resection, including the preoperative geriatric nutritional risk index. Nutrients 10(12):1900
Pantuck AJ et al (2003) Renal cell carcinoma with retroperitoneal lymph nodes: role of lymph node dissection. J Urol 169(6):2076–2083
de Saint Aubert N et al (2018) Nephron sparing surgery in tumours greater than 7cm. Prog Urol 28(6):336–343
Margulis V et al (2007) Oncological efficacy and safety of nephron-sparing surgery for selected patients with locally advanced renal cell carcinoma. BJU Int 100(6):1235–1239
Shum CF, Bahler CD, Sundaram CP (2017) Matched comparison between partial nephrectomy and radical nephrectomy for T2 N0 M0 tumors, a study based on the national cancer database. J Endourol 31(8):800–805
Chen SH et al (2021) Tumor volume: a new prognostic factor of oncological outcome of localized clear cell renal cell carcinoma. BMC Cancer 21(1):79
Zhang ZL et al (2011) Stage T1N0M0 renal cell carcinoma: the prognosis in Asian patients. Chin J Cancer 30(11):772–778
Suzuki K et al (2012) Prognostic significance of high nuclear grade in patients with pathologic T1a renal cell carcinoma. Jpn J Clin Oncol 42(9):831–835
Koelwyn GJ et al (2020) Myocardial infarction accelerates breast cancer via innate immune reprogramming. Nat Med 26(9):1452–1458
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Research conceptualization and design: AB, NS. Data acquisition: GN, MP. Data analysis and interpretation: HSO, MZ, NB. Drafting of the manuscript: HSO. Critical revision of the manuscript: MZ, NB. Administrative and technical support: AB, NS, MP. Approval of the final manuscript: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to Helsinki and Istanbul declarations. It has been ethically reviewed and approved by Shahid Beheshti University of Medical Sciences IRB (IR.SBMU.UNRC.REC.1401.028). All patients had given written consent before undergoing operation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Univariable analyses of the possible effect of different variables on OS, CSS and RFS'.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Basiri, A., Salehi Omran, H., Zahir, M. et al. Partial versus radical nephrectomy in pT2a renal cell carcinoma tumors: which is the superior surgical approach?. Afr J Urol 29, 43 (2023). https://doi.org/10.1186/s12301-023-00374-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-023-00374-2