Abstract
Background
Primary testicular leiomyosarcoma has a rare occurrence and the diagnosis is uncertain on pre-operative assessment. It is often seen in the background of chronic inflammation, radiotherapy, and the use of high-dose anabolic steroids.
Case presentation
We report a case of a painless testicular lump in a septuagenarian with pre-existing diabetes mellitus and hypertension but without any oncological risk factors. The primary workup did not reveal any elevation of serum tumour markers or any signs of metastatic disease on contrast imaging. The patient underwent a high inguinal orchiectomy due to a suspicion of germ cell tumor, and histopathology and immunohistochemistry confirmed the diagnosis of leiomyosarcoma.
Conclusion
Testicular leiomyosarcoma in the elderly is a rare malignancy and usually occur without any pre-existing risk factors. Early treatment provides long-term curative oncological control.
Similar content being viewed by others
1 Introduction
Testicular neoplasms represent up to 5% of all urological tumours. They are seen in the 2nd–4th decades of life and are predominantly of germinal origin [1]. Although the incidence of germ cell testicular cancer has been increasing over recent years, soft tissue sarcomas are an uncommon diagnostic entity, accounting for approximately 1% of all adult malignancies [2, 3].
Germ cell tumours in the elderly have been reported sporadically with falling incidence with age [4]. Elderly men with testicular lumps are mostly diagnosed with either spermatocytic seminomas, primary testicular lymphoma, or stromal tumours, usually of the Leydig cell type, and rarely metastasis [4]. Sarcomas are infrequently diagnosed, and the diagnosis is entirely based on pathological assessment and immunohistochemistry. Sarcomas are, by definition, indolent in nature and carry a favourable prognosis due to their muted risk of metastasis.
2 Case presentation
A 70-year-old man presented with a painless left testicular swelling for more than 6 months and had indolent progression. The patient was diabetic and hypertensive with a past history of left hydrocele repair. He did not consume alcohol or tobacco and was a non-smoker. There was no history of malignancies in the family or any prior exposure to carcinogenic stimuli. Physical examination revealed a hard, non-tender, enlarged left testicle with the absence of superficial inguinal lymphadenopathy. Serum tumour markers, i.e., Alpha-feto protein (AFP), lactate dehydrogenase (LDH), and b-Human chorionic gonadotropin (b-HCG), were within normal limits. The ultrasound evaluation showed an 8 × 9 cm hypoechoic lesion involving the left testicle with an unremarkable spermatic cord.
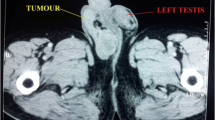
Contrast-enhanced a computed tomography (CECT) scan confirmed a large left testicular mass of 8 × 10 cm without any retroperitoneal or pelvic lymph node enlargement or any evidence of visceral metastasis (Fig. 1). Clinically, it was defined as T1N0M0. The patient underwent left high inguinal orchiectomy under spinal anaesthesia. The pathological assessment demonstrated the presence of malignant spindle cells with moderate nuclear pleomorphism and areas of haemorrhage, necrosis, and hyalinization within the tumour, stage PT1bN0Mx. The tumour was positive for SMA, h-Caldesmon, and Desmin, whereas negative for S-100 and CD117 (Fig. 2). The tumour was categorised as FNCLCC grade 1 with ENNEKING staging 1A. The postoperative follow-up showed no complications.
The postoperative period was uneventful and the patient was discharged on the next postoperative day. At 4 weeks and 3 months post-operatively, the patient was doing well with no evidence of local recurrence or distant metastasis.
3 Discussion
Leiomyosarcoma of the testis is believed to arise from undifferentiated smooth muscle cells of mesenchymal origin, such as blood vessels, seminiferous tubules, and tunica [5]. Primary leiomyosarcoma of the testis is a rare malignancy and only a handful of cases have been reported till now [6, 7]. These tumours are seen between the fourth and seventh decades, and the mean age of presentation is 50 years [8]. These patients present with a painless testicular mass and vague discomfort in the inguinoscrotal region. Scrotal ultrasound is usually performed, and it shows a hypoechoic and well-circumscribed mass, with or without calcification. Tumour markers such as HCG, AFP, and LDH are usually within normal limits [8]. Similarly, our case also presented with a painless testicular mass with normal serum tumour markers. Previous history of radiotherapy and the use of anabolic steroids are commonly identified risk factors for testicular leiomyosarcoma in patients less than 50 years old [9, 10]. In contrast, our patient did not have any such history of radiation or use of anabolic steroids.
Abdallah et al., in their literature review of 31 cases [11], reported that age at presentation varied significantly, with a mean age of 50.7 years and ranged from as early as 8 months to 78 years [8, 12] The tumour size ranged from 2 to 10 cm, with no preference for tumour laterality. Among 31 patients, 28 had normal serum markers except two had raised LDH and one patient had raised B-HCG levels. Of the 31 patients, 24 remained disease-free on long-term follow-up. One patient developed a local recurrence and six patients developed distant metastasis. Local recurrence was treated by local wide excision with or without radiotherapy. Retroperitoneal metastasis was treated by radiotherapy, and visceral metastasis was treated by chemotherapy alone.
Testicular tumours in the elderly population usually occur without any pre-existing risk factors. There are several differentials of leiomyosarcoma in elderly population. The incidence of GCTs in men older than 60 years of age is extremely low, with the exception of spermatocytic seminomas, a distinct GCT generally associated with a benign course. Spermatocytic seminoma is associated with distinctive clinical and pathological characteristics. They are not associated with a history of cryptorchidism, have a negative tumour marker profile, and are almost never associated with metastasis [13]. Other differentials include primary testicular lymphoma (PTL), an uncommon disease seen in 1–9% of all testicular neoplasms. However, it is the most common malignancy in men older than 50 years of age. DLBCL is the most common type, with anthracycline-based chemotherapy as the cornerstone of the treatment [14]. Sometimes, tumours occurring in the para-testicular region may be clinically indistinguishable from primary testicular tumours. They usually appear as scrotal masses with or without hydrocele. Only 30% of these are malignant, with liposarcoma being the most frequent, followed by leiomyosarcoma. Both of these tumours are found mainly in elderly males [15].
So far, ten cases of primary testicular leiomyosarcoma in septuagenarians have been reported (Table 1). As seen in leiomyosarcoma in the younger population, there is no side predilection, and the size of the tumour also falls within a similar range. But 3 out of 11 cases, including ours, had metastasis at presentation. This translates into 27.27% of the cases. Although the numbers are lower, still, this is a significant observation. Treatment has been high inguinal orchidectomy in the majority of cases, and the presence of localised disease on histopathology translated into good long-term outcomes. Our patient did not have any findings suggestive of metastatic disease.
Due to the disease's rarity, specific histopathological criteria are lacking. Histologic grade is considered the most important prognostic factor and is predictive of cancer-specific survival and distant metastasis. The AJCC Staging System and the French Federation of Cancer Centres Sarcoma Group (FNCLCC) grading scheme are two examples. The AJCC system grades range from G1 (well-differentiated) to G4 (undifferentiated). A more widely recommended staging system, FNCLCC, is based on three parameters: mitotic rates, differentiation, and necrosis [16].
Testicular leiomyosarcomas have a better prognosis and lower metastatic potential compared to extra-testicular leiomyosarcomas. High inguinal orchidectomy is considered the ideal treatment of choice. However, the need for RPLND is not well documented, and therefore it is reserved for patients with enlarged retroperitoneal nodes on imaging [17, 18]. The need for adjuvant treatment, such as chemotherapy and radiation, is decided on a case-to-case basis and no guidelines have been formulated for the same. Adjuvant treatment has been used in patients with positive surgical margins or when a local recurrence is contemplated [19, 20].
4 Conclusion
Elderly testicular leiomyosarcoma is a rare malignancy and usually not associated with any pre-existing risk factors like exposure to radiation or use of anabolic steroids. Treatment is high inguinal orchidectomy and is curative if detected early, and long-term oncological outcomes are encouraging.
Availability of data and materials
Not applicable.
References
Albers P, Albrecht W, Algaba F, Bokemeyer C, Cohn-Cedermark G, Horwich A et al (2005) Guidelines on testicular cancer. Eur Urol 48:885–894
Gaddam SJ, Chesnut GT (2022) Testicle cancer. In: StatPearls. Treasure Island (FL): StatPearls Publishing
Siegel RL, Miller KD, Jemal A (2020) Cancer statistics, 2020. CA Cancer J Clin 70(1):7–30
Berney D, Warren A, Verma M et al (2008) Malignant germ cell tumors in the elderly: a histopathological review of 50 cases in men aged 60 years or over. Mod Pathol 21:54–59
Arul P, Akshatha C (2016) Testicular leiomyoma masquerading as lymphoma. J Med Soc 30:176–178
Giridhar V, Kumar PB, Natarajan K, Hegde P (2011) Testicular leiomyosarcoma with metastasis. Indian J Urol 27:278–279
Moona MS, Fatima D, Turezbek A (2011) Primary testicular leiomyosarcoma. J Pak Med Assoc 61(10):1014–1016
Wakhlu A, Chaudhary A (2004) Massive leiomyosarcoma of the testis in an infant. J Pediatr Surg 39(7):e16–e17
Siraj F, Sharma S, Rai CB, Vasudeva P (2018) Primary high grade testicular leiomyosarcoma: a rare malignancy in a young male. Turk J Urol 44(2):178–181
Froeher M, Fischer R, Leike S, Hakenberg OW, Noack B, Wirth MP (1999) Intratesticular leiomyosarcoma in a young man after high doping with oral Turinabol: a case report. Cancer 86:1571–1575
Abdallah H, Dergamoun H, Hachem F, Boughaleb A, Al Sayegh H, Nouini Y (2021) Testicular leiomyosarcoma: a case report and literature review. Int J Surg Case Rep 83:105996
Hmida W, Mallat F, Othmen MB, Ben Ahmed K, Chavey S, Mestiri S, Abdallah AB, Mosbah F (2014) Primary intratesticular leiomyosarcomain a 78-year-old male. Int J Case Rep Images 5(10):717–722
Gigantino V, La Mantia E, Franco R, Cecere S, Rossetti S, Di Napoli M, Pisano C, Berretta M, Galzerano A, Botti G, Pignata S, Facchini G (2013) Testicular and testicular adnexa tumors in the elderly. Anticancer Drugs 24(3):228–236
Zucca E, Conconi A, Mughal TI, Sarris AH, Seymour JF, Vitolo U et al (2003) Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the International Extranodal Lymphoma Study Group. J Clin Oncol 21:20–27
Varzaneh FE, Verghese M, Shmookler BM (2002) Paratesticular leiomyosarcoma in an elderly man. Urology 60:1112
Zagars GK, Ballo MT, Pisters PW, Pollock RE, Patel SR, Benjamin RS et al (2003) Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: an analysis of 1225 patients. Cancer 97(10):2530–2543
Singh R, Chandra A, O’Brien TS (2004) Primary intratesticular leiomyosarcoma in a mixed race man: a case report. Clin Pathol 57:1319–1320
Wang X, Chen Z, Qiu S, Cao D, Jin K, Li J, Chen B, Lei H, Huang Y, Bao Y, Yang L, Liu L, Wei Q (2021) Clinical characteristics and prognostic factors of testicular sarcoma: a population-based study. Front Oncol 11:614093
Rajkomar K, Mundy I (2007) Leiomyosarcoma of the scrotum—a rare tumour. N Z Med J 120:U2835
Ballo MT, Zagars GK, Pisters PW et al (2001) Spermatic cord sarcoma: outcome, patterns of failure and management. J Urol 166:1306–1310
Acknowledgements
None.
Funding
No external funding received.
Author information
Authors and Affiliations
Contributions
BJ and RG had reviewed literature and written the case report. AK was the primary surgeon involved in treating the patient. RM and SC were involved in formulation of paper and review. SKR was involved in review of literature. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Consent taken from the patient for publication of this case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Competing interests
No competing interest among the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Joshi, B., Goel, R., Kumar, A. et al. Leiomyosarcoma presenting as unilateral painless testicular mass in a septuagenarian: a case report with review of the literature. Afr J Urol 28, 57 (2022). https://doi.org/10.1186/s12301-022-00325-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-022-00325-3