Abstract
Background
Unintentional falls are common among the elderly and given the expected increase of the aging population, these falls contribute to a high number of admissions to the emergency department. Relatively low-energy trauma mechanisms can lead to serious injuries in the elderly, with contributing factors being comorbidities, medication use and degenerative abnormalities.
Case presentation
A 94-year-old female suffered an unintentional fall at home. Upon arrival of the ambulance at her house she was hemodynamically stable and mobilized to the gurney with assistance. During primary survey at the emergency department, her blood pressure and oxygen saturation decreased, she was not able to move her legs anymore and lost consciousness. A full-body CTA was performed, which showed a fracture through the vertebral body of L2 with significant dislocation and a large active bleeding of the corpus, extending to the retroperitoneum and the epidural space. Despite resuscitation, her vital signs deteriorated and given the severe abnormalities on CTA, it was decided to discontinue further treatment, after which she deceased. The performed CTA and an x-ray from 2016 suggested diffuse idiopathic skeletal hyperostosis, which might have contributed to the severity and instability of the vertebral fracture. Mobilization after the fall might have increased the dislocation of the fracture. The use of oral anticoagulants worsened the subsequent bleeding and the extension to the epidural space caused the paralysis of the legs.
Conclusions
It is important to be aware of the possible serious consequences of unintentional falls in the elderly population and to provide strict immobilization of the spinal column until proper imaging.
Similar content being viewed by others
Background
Unintentional falls are common in the elderly population, with an incidence of 33% of the people aged 65 years or older, representing 105,000 elderly visiting the emergency department each year in the Netherlands [1]. Subsequently, falls are the leading cause of injury-related death in the elderly and contribute to high numbers of hospital admissions [2]. Moreover, given the expected increase of elderly in the general population, the health care-related costs continue to expand [3]. Previous studies emphasize how relatively low-energy trauma mechanisms in the elderly can lead to severe injuries. Contributing factors to the severity of the injuries are degenerative abnormalities, comorbidities, and medication use [4, 5]. Vertebrae, wrists, and hips are most frequently affected. Vertebral fragility fractures occur more often in women, and are associated with an increased level of morbidity and mortality [6, 7]. The majority of these fractures are located between the tenth thoracic and fourth lumbar vertebra [8]. In addition to degenerative conditions that increase with age, such as osteoporosis, other conditions can cause the spine to be more prone to fracture, such as ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis [9].
We report the case of a fall in a 94-year-old in which the severity of initial injury was underestimated compared to the eventual outcome in the emergency department.
Case presentation
A 94-year-old female was presented at the emergency department after an unwitnessed fall at home. She still lived on her own and mobilized inside her apartment with help of a walking aid. Her medical history reports congestive heart failure, atrial fibrillation, and hypercholesterolemia, for which she used a beta-blocker, an ACE-inhibitor, a coumarin derivative, and a statin. Furthermore, in 2011, she had been diagnosed with hyperuricemia and gout, for which she received allopurinol.
The ambulance reported that at the time of their arrival, the patient was conscious. She had fallen when she was alone at home, and her family was able to reach her by phone after one hour. There was no (witnessed) loss of consciousness; however, she suffered from retrograde amnesia and there was suspected head injury. Due to the initial estimation of a low-energy fall, the patient walked to the gurney with assistance of the ambulance nurses; however, after she started complaining of back pain, it was decided to immobilize the spine by transporting her in a vacuum mattress. During transport to the hospital, blood pressure decreased down to 90/50 mmHg, which initially responded to a fluid challenge with 500 ml of Ringer’s lactate. At the emergency department, she underwent a trauma survey according to the principles of the Advanced Trauma and Life Support. Upon arrival, her blood pressure was normal (112/59 mmHg) with tachycardia (137/min), tachypnea (30/min), and she was fully conscious (GCS 15). Within a few minutes, oxygen saturation and blood pressure significantly decreased to 90% and 82/41 mmHg respectively, whereupon a non-rebreathing mask with 15 L oxygen was applied and fluid resuscitation was started using 2 L Ringer’s lactate under pressure. Blood pressure remained low and her consciousness decreased. Plain radiographs of the chest and pelvis showed no abnormalities that could explain a hypovolemic shock. Laboratory findings showed a decreased hemoglobin of 4.4 mmol/L with an INR of 6.0. Prothrombin Complex Concentrate, vitamin K, and tranexamic acid were administered to attenuate blood loss and two units of packed red blood cells were given. Focused Assessment with Sonography in Trauma (FAST) did not show intra-abdominal free fluid. Neurological examination showed a complete paralysis of the lower extremities. A full-body computed tomography angiography (CTA) scan was performed, which showed a completely unstable Chance-type fracture through both the vertebral body and posterior complex of L2, with significant anterior distraction resulting in hyperlordosis. In addition, a large active bleeding was seen, extending to the retroperitoneum and the epidural space (Fig. 1). The extent of the retroperitoneal hematoma caused a mass effect with ventral dislocation of the right kidney (Fig. 2). In addition, a significant calcification of the anterior ligament of the spine was observed (Fig. 1). No intracerebral or intrathoracic post-traumatic abnormalities were detected.
Transverse (A), coronal (B), and sagittal (C, D) plane CT slices of the vertebral bleeding. A, B Active bleeding toward the retroperitoneum with a larger hematoma on the right side, but active contrast extravasation on both sides. C Active bleeding extending to the epidural space. D CT slice with bone window setting showing substantial dislocation of the fracture and extensive calcification of the anterior ligament of the spine
After CT imaging, her blood pressure kept decreasing despite resuscitation with in total 3 L of Ringer’s lactate and two units of packed red blood cells. The family was called, and it was decided to make a do-not-resuscitate decision. Given the age, prolonged duration of hypovolemia and subsequent hypoperfusion of the brain, in combination with the neurological and CTA findings, further treatment was discontinued. The patient deceased several minutes after discontinuation of treatment. Figure 3 presents a global timeline of events.
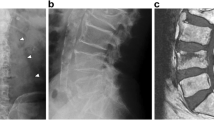
The exact origin of the bleeding is difficult to pinpoint, and this degree of bleeding is rare in case of a vertebral fracture. Based on the CT images, no further injury to the abdominal aorta, inferior vena cava, or the lumbar arteries was observed. The location of the bleeding most likely concerned the cancellous bone of the vertebrae, and the severity most probably has been increased by the high INR due to anticoagulant use. In addition, signs of extensive calcifications of the anterior ligament suspected of diffuse idiopathic skeletal hyperostosis were seen on both CT and previous conventional lumbar spine imaging in 2016 (Fig. 4).
Discussion
The number of elderly presenting to the emergency department after a fall is expected to increase by 47% until 2050 [1]. Moreover, 5209 of the Dutch people aged 65 and older died due to an unintentional fall in 2021 [10]. Because of its major impact on healthcare and healthcare costs, the Dutch Association of Clinical Geriatrics composed a guideline to improve fall prevention in patients living at home or in chronic care facilities [11]. The present case report describes a fatal outcome after a sustained L2 fracture due to a fall. The detrimental outcome was not expected in this initially ambulant patient with low back pain after the low-energy fall.
The high incidence of vertebral fragility fractures in elderly is mainly due to osteoporosis. In addition, ankylosing spine diseases like ankylosing spondylitis (AS) and diffuse idiopathic skeletal hyperostosis (DISH) cause the spine to be prone to highly unstable fractures [9]. In contrast to AS, DISH occurs at an older age and particularly affects the spine instead of the sacroiliac joints. Ossification of the anterior longitudinal ligaments and enthuses, as seen in this case, lead to decreased mobility until eventually complete ankylosis occurs [12, 13]. As a consequence, even minor trauma can cause fracture with high risk of instability and additional neurological deficit [14]. The prevalence of DISH in the Netherlands is approximately 17% in patients older than 50 years of age, and it is associated with obesity, type 2 diabetes, and increased life expectancy [15, 16]. The patient in this case suffered from dyslipidemia, hyperuricemia, and gout, all related to DISH [15]. A systematic review by Westerveld et al. showed that in case of DISH and AS, delay of diagnosis often occurs and awareness for the condition is highly important, as fracture instability can cause neurological deterioration after transfers or manipulation, which was also observed in the current case [14]. The Dutch guideline on acute traumatic vertebral fractures states that immobilization is necessary in any suspected thoracolumbar fracture (indicated by back pain or neurological deficit), or in case of a dangerous mechanism of injury (e.g., falls from > 3 m of height, high speed motor vehicle collisions) or known risk factors (including osteoporosis or an ankylotic spine) [17]. The patient was immobilized in a vacuum mattress after she reported back pain while walking to the gurney. Unfortunately, the diagnosis of DISH was unknown since no further tests were done after the suggestion of DISH on the radiographs in 2016, and therefore she was not immobilized immediately.
Lumbar fractures combined with severe bleeding are discussed in a number of studies. One retrospective study and three prior case reports showed accompanying lumbar artery bleeding on angiography [18,19,20,21]. In all cases, selective embolization was performed successfully. In our case, no further angiography examination was performed after initial CTA imaging, due to the agreement to discontinue further treatment. The CT-scan showed no clear image suggesting a rupture of any lumbar artery, despite the more difficult assessment due to the large hemorrhage. As shown in Fig. 1C, the bleeding extended to the epidural space causing a spinal epidural hematoma (SEH) with subsequent paralysis of the legs. Traumatic SEH occurs in between 0.5 and 1.7% of all spinal injuries, but the incidence increases to 9% in patients affected by ankylosing spondylitis or rheumatoid arthritis [22]. A retrospective case series by Tamburelli et al. investigated 7 consecutive patients with SEH. Like the patient in our case, 5 patients used oral anticoagulants and 2 were affected by DISH or AS [23]. In contrast to the patients in the case series of Tamburelli et al., the vital signs of the patient in our case deteriorated very rapidly and she died in the emergency department after discontinuing further treatment. This was most probably caused by the extension of the bleeding to the retroperitoneum and the subsequent hypovolemic shock. The use of coumarin derivates with an increased INR evidently contributed to the extensive blood loss.
In conclusion, this case report and literature review has emphasized the severity of a fall in elderly, especially in case of an ankylotic spine, as it may lead to serious neurological failure. Moreover, the use of anticoagulants contributed to the severe outcome and given its frequent use in the elderly population, one should be aware of the severe consequences. Strict spinal immobilization until proper imaging, CTA and complementary angiography should be low-threshold considerations in these patients. Apart from the co-morbidities contributing to the course of this case, morbidity and mortality are generally high in elderly who fall and this frail population is expected to increase in the future [1,2,3].
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- AS:
-
Ankylosing spondylitis
- CT:
-
Computed tomography
- CTA:
-
Computed tomography angiography
- DISH:
-
Diffuse idiopathic skeletal hyperostosis
- SEH:
-
Spinal epidural hematoma
References
VeiligheidNL. Dutch Injury Surveillance System (Letsel Informatie Systeem) 2011–2021 [04–08–2023]. Available from: https://www.veiligheid.nl/sites/default/files/2022-09/Infographic%20feiten%20en%20cijfers%20valongevallen%2065-plussers%202021.pdf.
Rau CS, Lin TS, Wu SC, Yang JC, Hsu SY, Cho TY, et al. Geriatric hospitalizations in fall-related injuries. Scand J Trauma Resusc Emerg Med. 2014;22:63.
Hartholt KA, van der Velde N, Looman CW, van Lieshout EM, Panneman MJ, van Beeck EF, et al. Trends in fall-related hospital admissions in older persons in the Netherlands. Arch Intern Med. 2010;170(10):905–11.
Galet C, Zhou Y, Eyck PT, Romanowski KS. Fall injuries, associated deaths, and 30-day readmission for subsequent falls are increasing in the elderly US population: a query of the WHO mortality database and National Readmission Database from 2010 to 2014. Clin Epidemiol. 2018;10:1627–37.
Pasquetti P, Apicella L, Mangone G. Pathogenesis and treatment of falls in elderly. Clin Cases Miner Bone Metab. 2014;11(3):222–5.
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353(9156):878–82.
Oudshoorn C, Hartholt KA, Zillikens MC, Panneman MJ, van der Velde N, Colin EM, et al. Emergency department visits due to vertebral fractures in the Netherlands, 1986–2008: steep increase in the oldest old, strong association with falls. Injury. 2012;43(4):458–61.
Khurana B, Sheehan SE, Sodickson A, Bono CM, Harris MB. Traumatic thoracolumbar spine injuries: what the spine surgeon wants to know. Radiographics. 2013;33(7):2031–46.
Hunter T, Forster B, Dvorak M. Ankylosed spines are prone to fracture. Can Fam Physician. 1995;41:1213–6.
Statistics Netherlands (Centraal Bureau van de Statistiek). Dutch causes of death statistics (‘Doodsoorzakenstatistiek’) CBS Statline2021. Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/7052_95/table?fromstatweb . Cited 2023 August 8.
Dutch Association of Clinical Geriatrics (NVKG). Dutch Guideline ‘Fall prevention in the elderly’ (Richtlijn ‘Preventie van valincidenten bij ouderen’): Richtlijnendatabase.nl; 2017. Available from: https://richtlijnendatabase.nl/richtlijn/preventie_van_valincidenten_bij_ouderen/startpagina_-_preventie_van_valincidenten.html . Cited 04–08–2023.
Belanger TA, Rowe DE. Diffuse idiopathic skeletal hyperostosis: musculoskeletal manifestations. J Am Acad Orthop Surg. 2001;9(4):258–67.
Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007;369(9570):1379–90.
Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18(2):145–56.
Kiss C, Szilagyi M, Paksy A, Poor G. Risk factors for diffuse idiopathic skeletal hyperostosis: a case-control study. Rheumatology (Oxford). 2002;41(1):27–30.
Westerveld LA, van Ufford HM, Verlaan JJ, Oner FC. The prevalence of diffuse idiopathic skeletal hyperostosis in an outpatient population in The Netherlands. J Rheumatol. 2008;35(8):1635–8.
Nederlandse Orthopaedische Vereniging (NOV). Dutch Guideline “Acute traumatic vertebral fractures” (Richtlijn “Acute Traumatische Wervelletsels”) 2019. Available from: https://richtlijnendatabase.nl/richtlijn/acute_traumatische_wervelletsels/startpagina_-_acute_traumatische_wervelletsels.html . Cited 2024 January 29.
Eun JP, Oh YM. Traumatic lumbar artery rupture after lumbar spinal fracture dislocation causing hypovolemic shock: an endovascular treatment. Br J Neurosurg. 2015;29(5):742–4.
Morita S, Tsuji T, Fukushima T, Yamagiwa T, Otsuka H, Inokuchi S. Arterial embolization of an extrapleural hematoma from a dislocated fracture of the lumbar spine: a case report. Scand J Trauma Resusc Emerg Med. 2009;17:27.
Sofocleous CT, Hinrichs CR, Hubbi B, Doddakashi S, Bahramipour P, Schubert J. Embolization of isolated lumbar artery injuries in trauma patients. Cardiovasc Intervent Radiol. 2005;28(6):730–5.
Di Meglio L, Rodà GM, Arrichiello A, Gurgitano M, Carrafiello G, Angileri SA. Lifesaving embolization in a massive lumbar artery bleeding: Interventional radiology management. Radiol Case Rep. 2021;16(10):3113–6.
Caron T, Bransford R, Nguyen Q, Agel J, Chapman J, Bellabarba C. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976). 2010;35(11):E458–64.
Tamburrelli FC, Meluzio MC, Masci G, Perna A, Burrofato A, Proietti L. Etiopathogenesis of traumatic spinal epidural hematoma. Neurospine. 2018;15(1):101–7.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
R.P., M.v.W. and J.T.B. contributed to conceptualization and design. Data acquisition and collection were performed by R.P. and S.G.. R.P. and M.v.W. wrote the first draft, whereafter all authors provided feedback on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was obtained from the next of kin of the deceased patient for writing this case report and the use of accompanying images.
Consent for publication
Written informed consent was obtained from the next of kin of the deceased patient for publication of this case report and accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ploumen, R.A.W., van Wezenbeek, M.R., Willems, P.C.P.H. et al. How a broken vertebra can lead to a fatal hemorrhage: a case report. Int J Emerg Med 17, 24 (2024). https://doi.org/10.1186/s12245-024-00594-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-024-00594-5