Abstract
Parasites cause illnesses with broad spectrum of symptoms from mild to severe, and are responsible for a significant number of outbreaks in the world. Current anti-parasitic drugs are toxic and have significant side effects. Nano-carriers are believed to obviate the limitations of conventional drugs via decreasing side effects and increasing target delivery and drug permeability with a controlled prolonged release of a drug. Solid lipid nanoparticles (SLNs) are lipid nanoparticles (LNPs), which have frequently been practiced. Suitable release rate, stability, and target delivery make SLNs a good alternative for colloidal carriers. SLNs are supposed to have great potential to deliver natural products with anti-parasitic properties. Nanoparticles have employed to improve stability and capacity loading of SLNs, during recent years. This review describes development of SLNs, the methods of preparation, characterization, and loaded drugs into SLNs in parasitic diseases. In addition, we summarize recent development in anti-parasitic SLNs-loaded drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Nanotechnology is a wide study area, which covers broad range of fields such as food, medicine, electronics, computer, communication, transportation, energy, and environment [1,2,3]. Advanced progress in nanotechnology has been led to control and use of materials at a nano-metric dimensions [4]. Actually, the main feature of nano materials is their dimension, which is smaller than 100 nm [4]. The main application of nanotechnology in biomedicine is designing and developing nano-carriers to sufficiently and specifically deliver and release therapeutic agents [5, 6]. Actually, nanomedicine employs nanotechnology, biomedical, and pharmaceutical sciences for either diagnosis or delivery purposes [7, 8] to increase and decrease effectiveness and toxicity, respectively [9, 10].
Colloidal particles are solid nano-carriers, composed from synthetic and natural polymers with sizes between 10 and 1000 nm, which could be an alternative for liposomes colloidal carriers [11]. Most of the therapeutic agents are conjugated to nanoparticles (NPs) to alter pharmacokinetic (PK) and/or pharmacodynamics (PD) properties of drugs [6, 12, 13]. Furthermore, many nano-drug formulations have been approved in clinical trials, so far [14, 15]. The types of NPs in approved and investigational drugs are polymeric, liposomal, nanocrystal formulations, inorganic NPs, micelles, metals/metal oxides, proteins, and dendrimers [16,17,18]. The majority of employed NPs, which have already been proven, are liposomes and polymers [14, 17]. Liposomes are small solid particles, suspended in a fluid phase, with a significant role in smart drug delivery with excellent efficiency [19]. The successful delivery of drugs depends on the sustained release of their contents and their stability in nanometer size [20, 21]. Due to the size, safety, ability to encapsulate various drugs, biocompatibility, and excellent modulation, liposomal colloidal drug carriers are good alternatives as a drug transporter compared to the expensive polymers [22]. Solid lipid nanoparticles (SLNs) are member of lipid nanoparticles, which due to their various therapeutic applications, are alternative carriers for traditional colloidal nanoparticles.
Parasites including protozoa and helminths, are widely reported in the world, and are responsible for gastrointestinal disorders, malnutrition, anemia, allergies, and etc. The main transmission routes of parasites are ingestion of contaminated food and water or through vectors (Table 1) [23,24,25]. Efficient treatment is a critical challenge facing with a broad range of medical and veterinary important parasites. The chemical drugs used for parasitic diseases are mostly expensive and toxic, with side effects and drug resistance [26,27,28]. Therefore, developing new efficient drugs for treatment of parasitic diseases has been practiced. Accordingly, nanotechnology has been incorporated in pharmaceutics to develop effectual drug delivery system for various parasitic diseases such as toxoplasmosis [29, 30], leishmaniasis [31,32,33,34,35,36], malaria [37,38,39,40], and trypanosomiasis [41]. Encapsulation of conventional drugs into nano-carriers such as lipid nanoparticles provides the possibility to develop new drugs with higher efficiency than common drugs with a low toxicity to host cells. In this review the general aspects, preparation methods, and characterization techniques of SLNs are explored. The current herbal and chemical antiparasitic agents are summarized and their combination with SLNs are reviewed. In addition, we comprehensively discuss the current development of nanodrugs for parasitic diseases.
2 General aspects of SLNs (structure, application, and characterization)
In last decades, several colloidal carrier systems such as emulsions, liposomes and polymeric micro, and nanoparticles have been developed [42,43,44]. Among carrier systems, SLNs as an alternative carrier system to traditional colloidal carriers, are attracting major attention for various therapeutic applications [42, 45]. At the early 90’s decade, SLNs were offered as an alternative carrier to colloidal drug carriers [46]. The size of SLNs as a sub-micron colloidal vehicle, are ranging from 50 to 1000 nm [44]. The large surface area, higher stability, and high drug loading properties, which improve efficacy of pharmaceuticals, are the most important advantages of SLNs [47]. In addition, SLNs have better performance in controlling the release kinetics compared to liquid lipid, which makes them more beneficial for intravenous applications [48]. The lipid matrix structure of solids (which is made of physiological lipids) reduces toxicity of SLNs and improves the absorption of water-insoluble drugs in the intestine [49, 50]. SLNs are comprised of a solid core of a high melting point lipid surrounded by phospholipids as a layer of safer surfactant [51, 52]. The lipids in SLNs include: (1) partial glycerides (2) saturated monoacid triglycerides (3) fatty acids, and (4) waxes. The toxicity profiling of SLNs is important for both production and application of such carrier system. According to the encapsulation location of drug compounds, SLNs have three different structures, which are categorized based on their preparation methods: (1) Drug-enriched shell model, in which NPs are prepared by a hot homogenization process. (2) Drug-enriched core model, which leads to supersaturation of the active drug based on cooling the nanoemulsion methods, and (3) homogenous matrix model that NPs are prepared by the cold homogenization process [53] (Fig. 1).
The toxicity profile is important for the generation and application of SLN systems [54, 55]. Toxicological profile should be evaluated before pre-clinical and clinical studies using in vitro and in vivo assays [56].
It has been reported that SLNs could be a target carrier for variety of drugs [57, 58]. The advantages of SLNs such as stability, biodegradable, and small size suggest them capable for delivering drugs to the liver [59]. Actually, because of the high saturation solubility and rapid dissolution rate, SLNs can accelerate the early stages of drug action [53] (Fig. 2).
Recent research has shown various potential administrations of SLNs such as oral route, brain, parenteral, ophthalmic, topical, and transdermal delivery, and carrying gene vector [49, 59,60,61,62]. The other advantage of SLNs is the modulation of drug release profiles [42]. Drug release from SLNs depends on the factors such as particle size, surfactant concentration, polymorphic state of SLNs, and temperature [48, 63]. Solid matrix of SLNs contains well-tolerated ingredients that protect active ingredients against chemical degradation. In addition, due to the initially burst of released drug, SLNs can prolong drug release time and minimize the burst due to increasing the solubility of the drug in the water phase, temperature, surfactant, and concentration [64, 65].
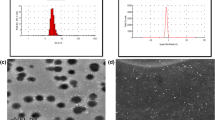
A variety of methods have been developed for characterization of SLNs. Evaluation of particle size, crystallinity size, distribution kinetics (zeta potential), lipid polymorphism, coexistence of micelles liposome, drug nanoparticles shape, drug release, and surface morphology are measured using various methods such as transmission electron microscopy (TEM), scanning electron microscopy (SEM) [66], scanning tunneling microscopy (STM), freeze fracture electron microscopy (FFEM), atomic force microscopy (AFM), photon correlation spectroscopy (PCS), and dynamic light scattering (DLS) [67]. In addition, the entrapped therapeutic agent volume can be characterized by UV, visible spectrophotometer, and high-pressure liquid chromatography (HPLC) [68].
The location of the therapeutic agent in the SLNs can be effective on its release, as well. For instance, the rate of drug release, which is located in the shell of the SLNs, is faster than the therapeutic agent that is located in the lipid nucleus. The properties and efficacy of SLNs were evaluated by in vivo and ex vivo assays, such as evaluation of drug loading and entrapment efficiency (EE) [69], assessment of the percentage of drug release [70], pharmacokinetic studies [71], determination of particle size [72], animal studies [73], evaluation of polydispersity index (PDI) [74], zeta potential (ZP) [75], thermogravimetric analysis (TG) [76], and cell toxicity by methyl-thiazolyl-tetrazolium (MTT) colorimetric assay [77].
3 Preparation of SLNs
Many techniques are available for the preparation of SLNs [78, 79]. The suitable preparation technique is chosen based on the particle size and availability of technique, which improve drug loading and successful encapsulation of therapeutic agent. SLNs are prepared from lipid, emulsifier, and water/solvent. The preparation of SLNs requires a precursor such as emulsion, micro-emulsions, and micellar solutions. The most common techniques employed for emulsions are hot homogenization, melt dispersion [80], phase inversion temperature (PIT) [81], and solvent evaporation-diffusion from emulsions [82]. Microemulsion dilution and microemulsion cooling techniques are common techniques for microemulsions [83], while coacervation method [84] is common in micellar solutions. Some of other techniques such as membrane contactor technique [85], spray-drying, spray-congealing [86] and electrospray are based on a particular instrument. However, high shear homogenization, hot and cold homogenization, ultra-sonication or homogenization, emulsification/evaporation, microemulsion, double emulsion method, and solvent evaporation/diffusion from emulsions are reported as the most common preparation techniques of SLNs formulation for anti-parasitic drugs [87,88,89].
Apart from conventional preparation methods, recent innovated technologies are described for preparation of liposomes, such as freeze drying of monophase solutions method, microfluidic channel method, membrane contactor method, dense gas techniques, green technology [90]. Among the new methods, green technologies have many benefits in biomedical research. Actually, the process of development of synthetic nanomaterials could be expensive, with less feasibility, which can produce environmental harmful substances [91]. In this regard, applications of green technologies had been led to 7% decrease in production of toxic materials such as hydrochloric acid (Hcl), trichloroethylene, and methyl isobutyl ketone, only during a decade from 2003 to 2014 [92]. Green technologies have been incorporated to synthesize lipid nanoparticles. Tocosome, a novel drug delivery system, which was firstly described by Mozafari et al. [93], is a bioactive carrier. This carrier is a product of a modified and improved heating method, which is known as “Mozafari method” [94]. Although green technologies have been tried for some parasitic diseases such as malaria [95, 96], the application of green technologies to prepare lipid NPs for parasitic diseases are rare and needs further consideration (Table 2).
4 Herbal and natural polymer components loaded into SLNs
Herbal medicine has been developed as a remedy for diseases along with human evolution [106, 107]. Over the time, because of the advantages of herbal medicines, applications of this approach have been developed [7, 108]. Currently, herbal compounds are incorporated with a nanostructured system to improve molecular size, increase bioavailability and biocompatibility, and decrease probable toxicity of the compounds [10, 109,110,111]. Indeed, nanotechnology can reduce side effects and increase target delivery of the herbal products [112,113,114]. In recent years, SLNs have taken attention by the researchers in drug delivery area [115] to enhance the efficacy [116,117,118] and improve oral bioavailability [119] of conventional herbal medicine. Furthermore, SLNs are most stable vehicles for plant extracts, which have shown higher antioxidant activity [120].
Artemisinin, an extract of the Artemisia annua, is one of the well-known herbal extract in medicine, which has been prescribed for malaria treatment for a long time. To increase efficiency and decrease side effects, artemisinin-based combination therapies (ACTs) have recently been developed for treatment of malaria. Many studies have employed SLNs formulation as a carrier for antimalarial drugs such as artemisinin [121]. In this regard, artemisinin and its derivatives (artesunate, artemether, dihydroartemisinin) are combined with other commercial drugs [122, 123]. Currently, combination therapy is preferred over monotherapy for malaria treatment [124]. For example, Attama et al. [38] employed SLNs to encapsulate two antimalarial drugs, artemether and lumefantrine, as the first-line treatment for malaria. In this regard, artemether and lumefantrine were loaded into the lipid nanoparticle to decrease side effects, enhance bioavailability, and overcome the pharmacokinetic mismatches. In addition, SLNs were labeled with coumarin 6 to indicate cellular uptake of encapsulated antimalarial drugs in Plasmodium-infected cells. The results of in vivo tests revealed high parasitemia clearance after oral administration with lower side effect, suggesting SLNs formulation as a promising technique to increase efficiency of combination therapy for malaria. Dwivedi et al. [39], loaded another derivations of artemisinin, arteether (ART), into SLNs for oral prescribtion. To evaluate the efficacy of ART-SLNs formulation, the entrapment efficiency was calculated using high-performance liquid chromatography (HPLC) method. The cytotoxicity effects of ART were evaluated out using MTT assay on J774A.1 cell line that the results showed a cell viability over 90%. Omwoyo et al. [37], loaded dihydroartemisinin (DHA), a derivative of artemisinin, into SLNs to evaluate anti-malaria efficacy, and to overcome limitations of this component including poor water-solubility and poor pharmacokinetic profile. The SLNs-loaded DHA was prepared based on single-emulsion solvent evaporation and high-speed homogenization methods, with size range of range from 150 to 500 nm. Stability and sustained release of drug were up to 90 days and over 20 h, respectively. Moreover, IC50 was 0.25 ng/ml with 97.24% chemo-suppression at 2 mg/kg/day, which were evaluated by in vitro and in vivo assays, respectively. Eventually, the released results using in vitro and in vivo assays showed that SLNs formulation was excellent for clinical practices.
Recently, numerous reports represented a ressistance agaist artemisinin [125,126,127,128]. Luteolin as a bioactive component can be utilized to eradicate artemisinin-resistant P. falciparum [129]. Luteolin is able to disrupt the life cycle of the parasite by preventing the fatty acid biosynthesis, which prevents the formation of new organelles and development of young trophozoite (ring stage) [130, 131]. Because of excellent biocompatibility of luteolin, this compound has been loaded into SLN-polyethylene glycol (PEG) using heat homogenization, cold homogenization, and hot-microemulsion ultrasonic methods [40]. Accordingly, luteolin encapsulated by SLN with further PEG modification showed an improvement of relative bioavailability, with decreased distribution and clearance of the component.
T. gondii is another prevalent human-infecting protozoa, which is the considered as a target for development of new treatment. Nemati et al. [30] developed neem oil-SLNs (NeO-SLNs) using double emulsification method and evaluated its anti-Toxoplasma activity. The results of this study showed that SLNs, as a liposomal carrier for NeO, prolonged extract release with an acceptable anti-Toxoplasma activity and cell cytotoxicity.
Chitosan (CS) is a natural biopolymer material composed of N-acetyl-d-glucosamine and d-glucosamine units with interesting properties and numerous pharmaceutical applications, which has been widely employed in the drug delivery area [132, 133]. In recent years, novel formulation against microbial agents with natural origins and nontoxic compounds have attracted the attention of many researchers [134]. The CS is a new delivery system, which has been widely studied as a coating material for different nanoparticles including SLNs [135, 136]. CS -coated SLN was successfully formulated to treat several diseases [22, 137, 138]. The anti-effects CS against Leishmania, Trichomonas, Plasmodium and Toxoplasma has previously been reported [139]. In this regard, Teimouri et al. [140] showed that CS was highly effective against T. gondii, and in a nanoformulation can be used as an alternative natural medicine in the treatment of toxoplasmosis. The results of in vitro and in vivo experiments showed 100% mortality of tachyzoites of RH strain and growth inhibition rates of tachyzoites in peritoneal of mice. CS exhibited significant effects on P. berghei, as well [141]. The results of in vivo and in vitro experiments showed that different concentrations of chitosan have potential antimalarial activity. To overcome the efflux of chloroquine (CQ) from the parasite's acidic digestive vacuole, nanoparticle chloroquine (NCQ) was employed. CS encapsulated nanochloroquine attenuated P. berghei infection in male Swiss mice, while the nanoformulation showed more potency to protect DNA damage, oxidative stress, and inflammation in infected mice [141]. The antiparasitic activity of chitosan was also highlighted on T. gallinae trophozoites. Accordingly, CS concentrations showed high mortality rate in treated trophozoites compared to control group. In addition, CS inhibited the viability of T. gallinae trophozoites [142, 143]. However, few studies have been conducted on combination of CS with SLN in parasitic infections. Additionally, several studies have been shown that CS has in vitro antileishmanial activity with 50% (EC50) against promastigotes and amastigotes forms of L. infantum, L. amazonensis, L. chagasi, L. major, L. tropica, and L. mexicana [144,145,146,147]. Moreover, recent findings reported that chitosan and its derivatives represented therapeutic and vaccine purposes in the treatment and prevention of both cutaneous and visceral leishmaniasis. Therefore, commercial chitosan is suggested to be an appropriate candidate for further studies on treatment of cutaneous and visceral leishmaniasis. In a study by Jain, et al. [36], the CS-coated SLNs was employed as an immunoadjuvant chemotherapy for Leishmania infection. The combination of SLNs with CS, as natural polymer, loaded with amphotericin B (AmB), induced activation of macrophages, which provoked immune responses such as tumor necrosis factor (TNF) α and interleukin (IL) 12 against leishmaniasis. SLNs preparation was performed using solvent emulsification-evaporation method and the cytotoxic studies in mice revealed suitable safety profile. The result indicated that AmB-SLNs as a safe and effective drug delivery system can be useful in anti-Leishmania therapy and immunotherapy field.
5 The therapeutic efficacy of antiparasitic drugs loaded into SLNs
In order to improve the therapeutic properties and increase the effectiveness of commercial antiparasitic drugs, many studies have applied SLNs as suitable carriers to transfer therapeutic agents, such as praziquantel [98, 101], paromomycin (PM) [29, 32, 34, 35], nitazoxanide (NTZ) [148], tanespimycin (17-AAG) [31], and AmB [32, 36, 149] in parasitic diseases.
5.1 Protozoa
Available data indicates side effects, toxicity, and resistant to commercial drugs in different parasitic protozan infections [150, 151]. To overcome the limitations of available chemical drugs for parasitic protozoan infections, the lipid-based formulations were suggested to enhance drug bioavailability and efficacy [152, 153]. Parvez et al. [32], developed and designed a drug-carrier system to decrease drug toxicity and improve bioavailability of AmB and PM against visceral leishmaniasis (VL), as orally administered dual drug SLNs (DDSLNs). For this purpose, the SLNs were modified with a dextrin composition, 2-hydroxypropyl-β-cyclodextrin (HPCD), which was incorporated with AmB and PM. The in vitro and in vivo tests were performed in mouse macrophage cells (J774) and L. donovani-infected BALB/c mice, respectively. As a results, DDSLNs decreased drug toxicity and side effects and enhanced the efficacy, compared to liposomal forms. In addition, the HPCD modification improved the uptake of SLNs by the infected macrophages and inhibited intracellular amastigote growth [32]. Moreover, vitamin B12-stearic acid (VBS), which was coated with AmB-loaded SLNs (VBS-AmB-SLNs), were prepared by double emulsion, solvent evaporation, and thermal-sensitive hydrogel methods to improve bioavailability for oral delivery and enhance the absorption potency of AmB [33]. Accordingly, the results of anti-leishmanial activity and cellular uptake revealed an enhanced efficacy up to 94% with the low toxicity percentage on cell lines. Actually, the most desirable rout to absorb drugs in the drug delivery system is the oral delivery, but the oral absorption of AmB is 0.2–0.9%, and nanoformulations can increase absorption and efficacy of the drug [33].
It was suggested that modulation of heat shock protein 90 (Hsp90) can inhibit the growth of Leishmania spp [154]. Actually, it was reported that 17-N-allylamino-17-demethoxygeldanamycin (17-AAG; tanespimycin) is an hsp90 inhibitor [155]. Pires et al. [31] developed a novel generation of anti-Leishmania agents by loading SLNs on tanespimycin (17-AAG, tanespimycin) using a double emulsion method with a particle size of about 104.3 ± 1.2 to improve the therapeutic effects of the drug. The findings showed a remarkable drug internalization, which seems to be potentially important delivery systems for elimination of intracellular Leishmania [154]. However, some drawbacks like the poor aqueous solubility and low stability have been limited usage of tanespimycin. Kharaji, et al. [34] developed a novel delivery systems against L. major and L. tropica using PM sulfate. The results of toxicity assays represented that PM-SLN formulation with smaller size and lower dose was safe with slight toxicity compared to larger size and higher dose of PM-SLN with enhanced effectiveness. Additionally, the results of SYTO green staining and fluorescent microscope imaging showed a decreased number of leishman-bodies in infected THP1 cells treated with PM-SLN. According to the results of in vitro analysis of IC50 and EC50 of PM-SLN formulation, this formulation was suggested for using in the treatment of the cutaneous leishmaniasis. Furthermore, Heidari‐Kharaji et al. [35], employed PM-SLN formulation against L. major in infected BALB/c mice and reported no significant toxicity in laboratory animals. In addition, the levels of cytokines including IL-4, gamma interferon (IFN-γ), and nitric oxide (NO) were evaluated. The results suggested that PM-SLN formulation is effective and safe with great drug delivery properties, which can reduce proliferation of L. major parasites in infected mice. In addition, Khosravi et al. [29], developed mannosylated SLNs containing PM (PM-SLN-M) and evaluated the anti-protozoa activity on acute toxoplasmosis. The results proposed high anti intracellular T. gondii activity with low cell toxicity in higher dosage than PM (Table 3).
5.2 Helminths
5.2.1 Classification of anthelmintic drugs based on the mechanism of action
Helminths are multicellular microorganisms with a complex body structure and organ systems (e.g., muscular, nervous, digestive, and reproductive). They can involve the liver, blood, intestine, and other tissues in human hosts [156]. From the clinical point of view, helminths are phylogenetically divided into three classes: cestodes or tapeworms, nematodes or roundworms, and trematodes or flatworms, with worldwide distribution [157].
Anthelminthic drugs destruct cell structure, integrity, metabolism, and neuromuscular coordination, which result in damage and the expulsion of worm from host intestine [158, 159]. Anthelminthic agents are generally classified into three groups: anticestodal, antinematodal, and antitrematodal drugs. Anthelmintic drugs may interfere with the carbohydrate metabolism, inhibit respiratory enzymes, and block neuromuscular action of helminths, and make them susceptible to the host's immune cells [160, 161]. Anthelminthic agents are generally classified into three groups: anticestodal, antinematodal, antitrematodal drugs.
5.2.1.1 Disrupting the metabolism
Benzimidazoles (BZD) such as albendazol (ABZ), mebendazol, thiabendazol, and tricolabendazol are a group of therapeutic agents, employed for a broad spectrum of helminths (E. vermicularis (pinworm), T. trichiura (whipworm), A. lumbricoides (common roundworm), Ancylostoma duodenale (common hookworm), Necator americanus (American hookworm), which mainly inhibit tubulin polymerization [162]. Benzimidazoles acts by interfering with carbohydrate metabolism and inhibiting polymerization of microtubules, which led to damage of cytoplasmic microtubules and impaired uptake of glucose via the larval and adult stages of the parasites [163].
Mebendazole inhibits glucose absorption in nematodes and cestodes, resulting in a significant consumption of parasite glycogen [164]. Niclosamide is an anthelmintic drug which is used to treat tapeworms and inhibits coupling of oxidative phosphorylation reactions and the electron transport, which impairs ATP synthesis [165]. Clorsulon is a compound belonging to the benzenesulphonamide family, which is recommended for treatment and control of adult liver flukes, F. hepatica [166]. Clorsulon affects the glycolytic pathway and nervous system of the parasite, resulting in inhibition of phosphoglycerate kinase [167]. Bithionol is an antibacterial, anthelmintic, and anti-algae agent, which had been practiced for treatment of fascioliasis and paragonimiasis before commercializing praziquantel. Bithionol interferes in ATP production and oxidative phosphorylation, which prevents formation of ATP in parasites [164].
5.2.1.2 Frustrating the nervous and muscular system
Imidazothiazoles are a group of anthelminthic drugs, which target neurotransmitters. Imidazothiazoles are nicotinic anthelmintic that act as acetylcholine receptors of nematodes and lead to flaccid paralysis of helminth via neuromuscular depolarizing blockade through stimulation of ganglion-like structures in nematodes muscle cells, and expelling by the normal peristaltic movements of the host intestine [168]. Piperazine is a common drug against nematodes, which through gamma-aminobutyric acid mimicking (GABA) affects chlorine (Cl) channels. The activity of piperazine depends on the inhibition of neuromuscular transmission (succinate production) in the parasite, hyperpolarizing of the nerve membrane, and paralysis of the helminths [169]. Some anthelmintic drugs act rapidly and selectively on neuromuscular transmission of nematodes. Levamisole, pyrantel, and morantel target nicotinic acetylcholine receptors of nematode muscle and cause spastic paralysis [170]. These drugs increase the flow of cations that leads to a rigid paralysis [171]. Pyrantel pamoate has been known as a broad-spectrum anthelmintic drug, which is prescribed for ascariasis, enterobiasis, and hookworm infections. This drug is a depolarizing neuromuscular-blocking agent, which paralyzes helminths by causing acetylcholine release and inhibiting cholinesterase [159].
5.2.1.3 Cell and membrane integrity destruction
Some of anthelmintic drugs destruct the integrity of protective layers and paralyze helminths with leakage of intracellular Ca2+. For example, praziquantel (PZQ) leads to tegumental impair and paralytic muscular of cestodes, resulting in death and deportation [172]. PZQ is broadly prescribed for hydatid cyst, neurocysticercosis, clonorchiosis, opisthorchosis, and schistosomiasis [173]. Following treatment with PZQ, tegument is disrupted due to significant influx of Ca2+ in the worms and increasing the calcium uptake of the parasite [174]. Diethylcarbamazine is a drug of choice against filiariasis, loiasis, and tropical eosinophilia, which immobilizes microfilariae and alters surface structure of the parasites. Furthermore, this drug displaces microfilariae from tissues to increase the contact between the parasites and immune system (Table 4).
5.2.2 The therapeutic efficacy of anthelmintic drugs loaded into SLNs
Several classes of anthelminthic agents have been developed, so far. Some drugs are specifically prescribed for a class of helminths. For example, drug of choice for schistosomiasis and tapeworms is praziquantel, while mebendazole and ABZ are the first line drugs prescribed for soil-transmitted helminths, and diethylcarbamazine and ivermectin are prescribed for filarial infections [175].
The site of absorption for anti-helminthic drugs in gastrointestinal tract is different [176]. It was evidenced that mebendazole is accumulated in the intestine and is used for treating large intestinal roundworms such as Ascarids, hookworms, and whipworms [177]. Although most of the drugs are absorbed from the intestinal tract, pyrantel pamoate, a drug of choice for pinworm infection, ascariasis, hookworm infection, and trichostrongilosis, is accumulated in the intestinal lumen [159]. Shortcomings of current anthelmintic drugs are poor water-solubility, low bioavailability, rapid degradation, and clearance factor [178]. Therefore, nanomedicine and conventional therapy have been incorporated for target delivery and reducing anthelminthic resistant [179, 180]. Nanoparticles with high surface to volume ratio provide higher surface area, resulting in reducing the size, increasing the surface area, as well as increase in the dissolution rate of the particles [181]. In addition, employing suitable carrier can overcome the solubility and bioavailability limitations of conventional drugs. It is supposed that gastrointestinal helminths use lipid droplets from digestive fluid to utalize it in their methabolic activity and produce energy [103]. This fact makes SLNs as an excellent lipid carrier for the delivery of anthelmintic drug agents such as: ABZ [99, 103, 105, 182], PZQ [101, 102, 183], and albendazole sulfoxide (ABZS) [99, 100, 104].
Ivermectin and nitazoxanide (NTZ) are effective anthelminthic drugs, which are widely employed for trichinosis [148]. However, drug resistant is expected for these drugs in the future, which arises the emergency for developing new and stable biocompatible therapeutic agents. In this regard, Hassan et al. [148] developed SLNs-loaded nitazoxanide (NTZ-SLNs) to increase the capture efficacy and drug release rates using modified thin film hydration technique for treatment of intestinal and muscular phase of trichinosis in murine host. The histopathological assessments demonstrated that ivermectin only affected the muscular phase, while NTZ-SLNs significantly killed Trichinella larvae in both intestinal and muscular phases, indicating increased efficacy of the drugs after combination with SLNs [148]. In addition, thin-film hydration is one of the most commonly used methods for liposome preparation [184]. ABZ is a benzimidazole, which has been widely prescribed for parasitic infections. The efficacy of ABZ has been evaluated against ascariasis, trichuriasis, strongyloidiasis, enterobiasis, and hookworm infection. The mechanism of action of ABZ is suggested to be via decreasing ATP formation and blocking glucose uptake in different stages of helminth’s life cycle. One of the significant advantages of ABZ, is the solubility of this drug in lipid formulation that leads to improve bioavailability and suitable loading capacity of the drug in the SLNs [103]. Sharma et al. [103] developed a ABZ-loaded SLNs (SLN-A) formulation against the intestinal parasitic worm, Haemonchus contortus, to enhance the effectivness of ABZ based on evaluation of the motility and mobility assay (AMMA) of adult helminths. In this study, double emulsion technique was used to produce SLNs. This formulation was developed to reduce the needed dosage and side effects of the drug. Dispersion ultrasonic emulsion and nano-emulsion methods were used for preparation of drug-loaded SLNs and drug-free SLNs [103]. Hydatidosis or hydatid disease is caused by the larval stages of cestode (tapeworm) of the genus Echinococcus with serious public health problems. Benzimidazole derivatives (albendazole, thiabendazole, and mebendazole) are the currently administrated drug of choice for echinococcosis. Among BZDs, ABZ, as a lipophilic anthelmintic drug, is an effective drug against cystic echinococcosis (CE). However, the conventional drugs have shown systemic side effects. In this regard, a study was designed on ABZ and ABZ sulfoxide (SO)-loaded SLNs formulation to increase drug permeation across the hydatid cyst membrane [100]. Micro emulsification and high shear homogenization methods were used to prepare SLNs. The particle size of prepared formulations showed < 180 nm, and ABZ-SLNs and ABZSO-SLNs showed fast release, and higher permeability and efficacy compared to conventional drug. Hydatid cysts are classified as fertile and infertile cysts. Actually, fertile cysts contain the germinal layer with the brood capsules and protoscoleces, but the germinal layer of infertile cysts is without protoscoleces. Therefore, diffusion of drugs into the cyst layers may led to increased drugs efficacy [185]. Rafiei et al. [99], investigated ultrastructural changes of ABZ and ABZSO and their SLNs-loaded in fertile and infertile hydatid cysts. They micro-emulsification and high shear homogenization methods were engaged to produce lipid nanoparticles. The findings showed higher efficacy of ABZ and ABZSO SLNs-loaded in fertile and small cysts [99]. Toxocariasis is caused by T. canis and T. catis, causative agents of visceral larva migrants (VLM) and ocular toxocariasis (OT). ABZ is one of the choice drug in treatment toxocariasis, as well. In this regard, Kudtarkar et al. [105], engaged lipid nanoparticles to prepare SLNs using phase inversion temperature method. The mean particle size of ABZ-SLN was ranged of 116 ± 3.51 nm to 168.3 ± 3.92 nm. The anthelmintic efficacy of ABZ-SLN was evaluated in mice infected with T. canis larvae. The ABZ-SLN formulations showed effective drug delivery and therapeutic effect at both low (50 mg/kg) and high (100 mg/kg). Furthermore, the results showed, reduction in larvae count in vital organs of mice. Abedi et al. [182], designed a magnetic SLNs-loaded ABZ as an antiparasitic drug. They modified the drug delivery system area in ABZ-SLN formulation. ABZ-magnetic SLNs (MSLNPs) were composed of (Fe3O4) NPs as the core and stearic acid as shell, were engaged as carriers to increase the efficient delivery of ABZ.
Although the limitations such as poor solubility in water, low absorption through the gastrointestinal tract (GIT), and need for large dosage have been reported [186], PZQ is a frontline drug for parasitic infections and the drug of choice for the schistosomiasis chemotherapy [187]. However, chemotherapy with PZQ is not effective in high endemic areas [186], and the efficiancy of PZQ is low during oral administration. Therefore, nanoformulation of this drug was practiced to overcome these limitations. Souza et al. [98], evaluated the intestinal permeability, toxicity, and effectiveness of PZQ-SLNs against adult S. mansoni. The preparation method of SLNs was high-shear homogenization and micro-emulsification. S. mansoni was cultured in HepG2 cell line and the adult worms were incubated with SLNs, PZQ-SLNs and free PZQ. PZQ-SLNs were typically spherical shape with a size range between 500 and 1000 nm, and PZQ-loaded SLNs formulation killed the parasites in short time with low cell toxicity against HepG2 cells compared to the free PZQ. Therefore, the PZQ-loaded SLNs were suggested as a promising treatment strategy for the schistosomiasis control program. Similar to previous study, Radwan et al. [97], fabricated a novel PZQ-SLNs formulation to enhance bioavailability and antischistosomal efficacy of PZQ against murine S. mansoni infection [97]. In this study, SLN formulations were prepared by micro emulsification and high shear homogenization techniques and the particle sizes of SLNs ranged between 87.32 and 302.3 nm. As results, the number of worms were significantly reduced at 14 days after treatment with SLNs-PZQ in S. mansoni-infected mice treated with SLNs-PZQ compared to control group. Moreover, a significant reduction in the percentages of total mature eggs was observed after SLNs-PZQ treatment. The results of pharmacokinetic assessment of PZQ and SLNs-PZQ in normal and S. mansoni-infected mice showed enhanced PZQ bioavailability in the S. mansoni-infected groups, as well. Xie, et al. [102], developed a modification with loading PZQ into hydrogenated castor oil-SLNs in order to enhance the therapeutic efficacy of the drug against dogs infected with E. granulosus. The nanoparticle size was 263.00 ± 11.15 nm, and the preparation methods were hot homogenization and ultrasonication techniques. The hydrogenated castor oil (HCO) was loaded into SLNs to induce the therapeutic efficacy of PZQ. In this study, the E. granulosus-infected dogs were treated with a low dose of 0.5 mg/kg compared to the high dose of 5 mg/kg, which is prescribed in clinical application, revealing an enhanced pharmacological activity of PZQ by SLNs. Andrade et al. [101] developed SLNs via high-cut homogenization method for the loading of PZQ for the treatment of S. mansoni infections. Analysis of SEM microscopy showed that PZQ-loaded SLNs were typically spherical with a size range between 500 and 1000 nm. The in vitro investigation on adult worms of S. mansoni showed that PZQ-loaded SLNs has great parasiticidal properties (Table 5).
6 Future perspective
Together with emerging drugs for a broad spectrum of communicable and non-communicable diseases, nanoscience and nanotechnology are developed. Nanoparticles or nanoscale materials are popular due to their applications in drug delivery, which have led to a dramatically increase in the number of clinical trials of nanomedicine incorporated drugs. Actually, specific drug delivery reduces systemic toxicity and nonspecific distribution, and overcomes limitations of conventional drugs. Despite recent progress in drug delivery systems based on nanomaterials in the treatment of parasites, this subject still remains as a priority of research. However, few clinical trials employed SLN-based formulations as a vehicle for the treatment of the parasite infections, therefore, there is an essential requirement for expanding nanodrugs for parasitic diseases. In addition, together with advances in herbal medicine, SLNs formulation seems to be an alternative technique to either improve specific delivery or decrease toxic effects of herbal extracts or their components.
Application of SLNs formulation in vaccines seems to be another target in future research. It was suggested that incorporation of SLNs with adjuvants can improve the immune responses during vaccination. Importantly, SLNs increase contact surface and control the release of loaded contents. Therefore, regarding the rapid degradation of adjuvants in the body, a combination of the lipid components of SLNs with adjuvants may deliberate degradation of adjutant with long lasting exposure to the immune system, which lead to more efficient immunogenicity.
Although nanotechnology and its applications in nanodrug formulation is rapidly being progressed, the gap between developed and less-developed countries is widening. The lack of resources and technologies in less-income countries decreases the capability of these regions to effectually participate in designing nanotechnology-based drugs for their needs. Apart from the lack of infrastructures in poor countries, the target for effective therapy is also different. The main challenge for less-developed countries is forceful actions against infectious diseases, while the most of developed and commercialized nano-formulated drugs are against non-communicable diseases, which is the main problem in wealth countries. Therefore, the following ways are suggested to increase the chance of designing and prescribing of nanodrugs in less-developed countries. (1) Fabricating cost effective nano-formulated drugs with low maintenance costs, high stability, and high effectiveness to generally decrease the health costs for poor countries. (2) Efficient participation of nongovernment organizations (NGOs) to invest and provide resources for designing and fabrication of effective nanodrugs. (3) The use of low cost materials such as herbal extracts and green technologies in order to decrease the cost for designing novel nanodrugs against infectious diseases. (4) Although there are single studies synthesizing and employing nanodrugs in poor regions, it seems that establishing a headquarter organization to functionally support researches and studies for new technologies, increases the chance of poor regions to access to the nanodrugs and employ them in their challenges.
References
Thiruvengadam M, Rajakumar G, Chung IM. Nanotechnology: current uses and future applications in the food industry. 3 Biotechnology. 2018;8(1):74. https://doi.org/10.1007/s13205-018-1104-7.
Nasrollahzadeh M, Sajadi SM, Sajjadi M, Issaabadi Z. Chapter 4-Applications of nanotechnology in daily life. In: Nasrollahzadeh M, Sajadi SM, Sajjadi M, Issaabadi Z, Atarod M, editors. Interf Sci Technol, vol. 28. Amsterdam: Elsevier; 2019. p. 113–43. https://doi.org/10.1016/B978-0-12-813586-0.00004-3.
Neme K, Nafady A, Uddin S, Tola YB. Application of nanotechnology in agriculture, postharvest loss reduction and food processing: food security implication and challenges. Heliyon. 2021;7(12):e08539. https://doi.org/10.1016/j.heliyon.2021.e08539.
Jeevanandam J, Barhoum A, Chan YS, Dufresne A, Danquah MK. Review on nanoparticles and nanostructured materials: history, sources, toxicity and regulations. Beilstein J Nanotechnol. 2018;9:1050–74. https://doi.org/10.3762/bjnano.9.98.
Zdrojewicz Z, Waracki M, Bugaj B, Pypno D, Cabała K. Medical applications of nanotechnology. Postep Hig Med Doswiad (Online). 2015;69:1196–204. https://doi.org/10.5604/17322693.1177169.
Havel H, Finch G, Strode P, Wolfgang M, Zale S, Bobe I, Youssoufian H, Peterson M, Liu M. Nanomedicines: from bench to bedside and beyond. AAPS J. 2016;18(6):1373–8. https://doi.org/10.1208/s12248-016-9961-7.
Bonifácio BV, Silva PB, Ramos MA, Negri KM, Bauab TM, Chorilli M. Nanotechnology-based drug delivery systems and herbal medicines: a review. Int J Nanomed. 2014;9:1–15. https://doi.org/10.2147/ijn.s52634.
Nemati S, Shalileh F, Mirjalali H, Omidfar K. Toward waterborne protozoa detection using sensing technologies. Front Microbiol. 2023;14:1118164. https://doi.org/10.3389/fmicb.2023.1118164.
Mirza AZ, Siddiqui FA. Nanomedicine and drug delivery: a mini review. Int Nano Lett. 2014;4(1):1–7.
Watkins R, Wu L, Zhang C, Davis RM, Xu B. Natural product-based nanomedicine: recent advances and issues. Int J Nanomed. 2015;10:6055.
Barratt G. Colloidal drug carriers: achievements and perspectives. Cell Mol Life Sci. 2003;60(1):21–37. https://doi.org/10.1007/s000180300002.
Ventola CL. The nanomedicine revolution: part 1: emerging concepts. Peer Rev J Formular Manag. 2012;37(9):512–25.
Havel HA. Where are the nanodrugs? an industry perspective on development of drug products containing nanomaterials. AAPS J. 2016;18(6):1351–3. https://doi.org/10.1208/s12248-016-9970-6.
Caster JM, Patel AN, Zhang T, Wang A. Investigational nanomedicines in 2016: a review of nanotherapeutics currently undergoing clinical trials. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2017. https://doi.org/10.1002/wnan.1416.
Bobo D, Robinson KJ, Islam J, Thurecht KJ, Corrie SR. Nanoparticle-based medicines: a review of FDA-approved materials and clinical trials to date. Pharmaceut Res. 2016;33(10):2373–87. https://doi.org/10.1007/s11095-016-1958-5.
Stanberry LR, Simon JK, Johnson C, Robinson PL, Morry J, Flack MR, Gracon S, Myc A, Hamouda T, Baker JR Jr. Safety and immunogenicity of a novel nanoemulsion mucosal adjuvant W805EC combined with approved seasonal influenza antigens. Vaccine. 2012;30(2):307–16. https://doi.org/10.1016/j.vaccine.2011.10.094.
Ventola CL. Progress in nanomedicine: approved and investigational nanodrugs. Peer-Rev J Formul Manag. 2017;42(12):742–55.
Gregory AE, Titball R, Williamson D. Vaccine delivery using nanoparticles. Front Cell Infect Microbiol. 2013;3:13. https://doi.org/10.3389/fcimb.2013.00013.
Weers JG. Colloidal particles in drug delivery. Curr Opin Colloid Interf Sci. 1998;3(5):540–4. https://doi.org/10.1016/S1359-0294(98)80030-7.
Nagati V, Tenugu S, Pasupulati AK. Chapter 4-Stability of therapeutic nano-drugs during storage and transportation as well as after ingestion in the human body. In: Das Talukdar A, Dey Sarker S, Patra JK, editors. Advances in nanotechnology-based drug delivery systems. Amsterdam: Elsevier; 2022. p. 83–102. https://doi.org/10.1016/B978-0-323-88450-1.00020-X.
Patra JK, Das G, Fraceto LF, Campos EVR, Rodriguez-Torres MdP, Acosta-Torres LS, Diaz-Torres LA, Grillo R, Swamy MK, Sharma S, Habtemariam S, Shin H-S. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnol. 2018;16(1):71. https://doi.org/10.1186/s12951-018-0392-8.
Baek J-S, Cho C-W. Surface modification of solid lipid nanoparticles for oral delivery of curcumin: improvement of bioavailability through enhanced cellular uptake, and lymphatic uptake. Eur J Pharmaceut Biopharmaceut. 2017;117:132–40. https://doi.org/10.1016/j.ejpb.2017.04.013.
WHO. Global report on antimalarial efficacy and drug resistance: 2000–2010. WHO; 2010. p. 2023.
Murray CJL, Rosenfeld LC, Lim SS, Andrews KG, Foreman KJ, Haring D, Fullman N, Naghavi M, Lozano R, Lopez AD. Global malaria mortality between 1980 and 2010: a systematic analysis. Lancet. 2012;379(9814):413–31.
Taghipour A, Javanmard E, Rahimi HM, Abdoli A, Matin S, Haghbin M, Olfatifar M, Mirjalali H, Zali MR. Prevalence of intestinal parasitic infections in patients with diabetes: a systematic review and meta-analysis. Int Health. 2023. https://doi.org/10.1093/inthealth/ihad027.
Liu LX, Weller PF. Antiparasitic drugs. New Engl J Med. 1996;334(18):1178–84. https://doi.org/10.1056/nejm199605023341808.
Katz M. Adverse metabolic effects of antiparasitic drugs. Rev Infect Dis. 1982;4(4):768–70. https://doi.org/10.1093/4.4.768.
Farahmandian I, Arfaa F, Jalali H, Reza M. Comparative studies on the evaluation of the effect of new anthelminthics on various intestinal helminthiasis in Iran. Effects of anthelminthics on intestinal helminthiasis. Chemotherapy. 1977;23(2):98–105. https://doi.org/10.1159/000221977.
Khosravi M, Mohammad Rahimi H, Doroud D, Mirsamadi ES, Mirjalali H, Zali MR. In vitro evaluation of mannosylated paromomycin-loaded solid lipid nanoparticles on acute toxoplasmosis. Front Cell Infect Microbiol. 2020;10:33.
Nemati S, Mohammad Rahimi H, Hesari Z, Sharifdini M, Jalilzadeh Aghdam N, Mirjalali H, Zali MR. Formulation of Neem oil-loaded solid lipid nanoparticles and evaluation of its anti-Toxoplasma activity. BMC Complement Med Therap. 2022;22(1):1–11.
Pires VC, Magalhães CP, Ferrante M, de Souza RJ, Nguewa P, Severino P, Barral A, Veras PST, Formiga FR. Solid lipid nanoparticles as a novel formulation approach for tanespimycin (17-AAG) against Leishmania infections: preparation, characterization and macrophage uptake. Act Trop. 2020;211:105595.
Parvez S, Yadagiri G, Gedda MR, Singh A, Singh OP, Verma A, Sundar S, Mudavath SL. Modified solid lipid nanoparticles encapsulated with amphotericin B and paromomycin: an effective oral combination against experimental murine visceral leishmaniasis. Sci Rep. 2020;10(1):1–14.
Singh A, Yadagiri G, Parvez S, Singh OP, Verma A, Sundar S, Mudavath SL. Formulation, characterization and in vitro anti-leishmanial evaluation of amphotericin B loaded solid lipid nanoparticles coated with vitamin B12-stearic acid conjugate. Mater Sci Eng C. 2020;117: 111279.
Kharaji MH, Doroud D, Taheri T, Rafati S. Drug targeting to macrophages with solid lipid nanoparticles harboring paromomycin: an in vitro evaluation against L. major and L. tropica. AAPS Pharm Sci Tech. 2016;17(5):1110–9.
Heidari-Kharaji M, Taheri T, Doroud D, Habibzadeh S, Badirzadeh A, Rafati S. Enhanced paromomycin efficacy by solid lipid nanoparticle formulation against Leishmania in mice model. Parasit Immunol. 2016;38(10):599–608.
Jain V, Gupta A, Pawar VK, Asthana S, Jaiswal AK, Dube A, Chourasia MK. Chitosan-assisted immunotherapy for intervention of experimental leishmaniasis via amphotericin B-loaded solid lipid nanoparticles. Appl Biochem Biotechnol. 2014;174(4):1309–30.
Omwoyo WN, Melariri P, Gathirwa JW, Oloo F, Mahanga GM, Kalombo L, Ogutu B, Swai H. Development, characterization and antimalarial efficacy of dihydroartemisinin loaded solid lipid nanoparticles. Nanomed Nanotechnol Biol Med. 2016;12(3):801–9.
Attama AA, Kenechukwu FC, Onuigbo EB, Nnamani PO, Obitte N, Finke JH, Pretor S, Müller-Goymann CC. Solid lipid nanoparticles encapsulating a fluorescent marker (coumarin 6) and antimalarials–artemether and lumefantrine: evaluation of cellular uptake and antimalarial activity. Eur J Nanomed. 2016;8(3):129–38.
Dwivedi P, Khatik R, Khandelwal K, Shukla R, Paliwal SK, Dwivedi AK, Mishra PR. Preparation and characterization of solid lipid nanoparticles of antimalarial drug arteether for oral administration. J Biomater Tissue Eng. 2014;4(2):133–7.
Kamarullah W, Indrajaya E, Emmanuella J. potency of luteolin with solid lipid nanoparticle (sln)-polyethylene glycol (peg) modification for artemisinin-resistant Plasmodium falciparum infection. Indonesian J Trop Infect Dis. 2018;7(3):80–6.
Volpedo G, Costa L, Ryan N, Halsey G, Satoskar A, Oghumu S. Nanoparticulate drug delivery systems for the treatment of neglected tropical protozoan diseases. J Venom Animal Toxin Includ Trop Dis. 2019;25:e144118. https://doi.org/10.1590/1678-9199-jvatitd-1441-18.
Müller RH, Mäder K, Gohla S. Solid lipid nanoparticles (SLN) for controlled drug delivery—a review of the state of the art. Eur J Pharmaceut Biopharmaceut. 2000;50(1):161–77. https://doi.org/10.1016/s0939-6411(00)00087-4.
Lu H, Zhang S, Wang J, Chen Q. A review on polymer and lipid-based nanocarriers and its application to nano-pharmaceutical and food-based systems. Front Nutr. 2021;8:783831. https://doi.org/10.3389/fnut.2021.783831.
Nicolas J, Mura S, Brambilla D, Mackiewicz N, Couvreur P. Design, functionalization strategies and biomedical applications of targeted biodegradable/biocompatible polymer-based nanocarriers for drug delivery. Chem Soc Rev. 2013;42(3):1147–235. https://doi.org/10.1039/c2cs35265f.
Guimarães D, Cavaco-Paulo A, Nogueira E. Design of liposomes as drug delivery system for therapeutic applications. Int J Pharmaceut. 2021;601:120571. https://doi.org/10.1016/j.ijpharm.2021.120571.
Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev. 2013;65(1):36–48. https://doi.org/10.1016/j.addr.2012.09.037.
Jacob S, Nair AB, Shah J, Gupta S, Boddu SHS, Sreeharsha N, Joseph A, Shinu P, Morsy MA. Lipid nanoparticles as a promising drug delivery carrier for topical ocular therapy-an overview on recent advances. Pharmaceutics. 2022. https://doi.org/10.3390/pharmaceutics14030533.
Dhiman N, Awasthi R, Sharma B, Kharkwal H, Kulkarni GT. Lipid nanoparticles as carriers for bioactive delivery. Front Chem. 2021;9:580118. https://doi.org/10.3389/fchem.2021.580118.
Uner M, Yener G. Importance of solid lipid nanoparticles (SLN) in various administration routes and future perspectives. Int J Nanomed. 2007;2(3):289–300.
Satapathy S, Patro CS. Solid lipid nanoparticles for efficient oral delivery of tyrosine kinase inhibitors: a nano targeted cancer drug delivery. Adv Pharmaceut Bull. 2022;12(2):298–308. https://doi.org/10.34172/apb.2022.041.
Mishra V, Bansal KK, Verma A, Yadav N, Thakur S, Sudhakar K, Rosenholm JM. Solid lipid nanoparticles: emerging colloidal nano drug delivery systems. Pharmaceutics. 2018. https://doi.org/10.3390/pharmaceutics10040191.
Pink DL, Loruthai O, Ziolek RM, Wasutrasawat P, Terry AE, Lawrence MJ, Lorenz CD. On the structure of solid lipid nanoparticles. Small. 2019;15(45):e1903156. https://doi.org/10.1002/smll.201903156.
Ghasemiyeh P, Mohammadi-Samani S. Solid lipid nanoparticles and nanostructured lipid carriers as novel drug delivery systems: applications, advantages and disadvantages. Res Pharmaceut Sci. 2018;13(4):288–303. https://doi.org/10.4103/1735-5362.235156.
Sharma S, Parveen R, Chatterji BP. Toxicology of nanoparticles in drug delivery. Curr Pathobiol Rep. 2021;9(4):133–44. https://doi.org/10.1007/s40139-021-00227-z.
Khan I, Saeed K, Khan I. Nanoparticles: properties, applications and toxicities. Arab J Chem. 2019;12(7):908–31. https://doi.org/10.1016/j.arabjc.2017.05.011.
Inglut CT, Sorrin AJ, Kuruppu T, Vig S, Cicalo J, Ahmad H, Huang HC. Immunological and toxicological considerations for the design of liposomes. Nanomaterials (Basel, Switzerland). 2020. https://doi.org/10.3390/nano10020190.
Wong HL, Bendayan R, Rauth AM, Li Y, Wu XY. Chemotherapy with anticancer drugs encapsulated in solid lipid nanoparticles. Adv Drug Deliv Rev. 2007;59(6):491–504. https://doi.org/10.1016/j.addr.2007.04.008.
Din FU, Aman W, Ullah I, Qureshi OS, Mustapha O, Shafique S, Zeb A. Effective use of nanocarriers as drug delivery systems for the treatment of selected tumors. Int J Nanomed. 2017;12:7291–309. https://doi.org/10.2147/ijn.s146315.
Lingayat VJ, Zarekar NS, Shendge RS. Solid lipid nanoparticles: a review. Nanosci Nanotech Res. 2017;4(2):67–72.
Satapathy MK, Yen TL, Jan JS, Tang RD, Wang JY, Taliyan R, Yang CH. Solid lipid nanoparticles (slns): an advanced drug delivery system targeting brain through bbb. Pharmaceutics. 2021. https://doi.org/10.3390/pharmaceutics13081183.
Manjunath K, Venkateswarlu V. Pharmacokinetics, tissue distribution and bioavailability of clozapine solid lipid nanoparticles after intravenous and intraduodenal administration. J Control Rel. 2005;107(2):215–28. https://doi.org/10.1016/j.jconrel.2005.06.006.
Martins SM, Sarmento B, Nunes C, Lúcio M, Reis S, Ferreira DC. Brain targeting effect of camptothecin-loaded solid lipid nanoparticles in rat after intravenous administration. Eur J Pharmaceut Biopharmaceut. 2013;85(3):488–502. https://doi.org/10.1016/j.ejpb.2013.08.011.
Wang X, Chen H, Luo Z, Fu X. Preparation of starch nanoparticles in water in oil microemulsion system and their drug delivery properties. Carbohydr Polym. 2016;138:192–200. https://doi.org/10.1016/j.carbpol.2015.11.006.
Zur Mühlen A, Schwarz C, Mehnert W. Solid lipid nanoparticles (SLN) for controlled drug delivery–drug release and release mechanism. Eur J Pharmaceut Biopharmaceut. 1998;45(2):149–55. https://doi.org/10.1016/s0939-6411(97)00150-1.
Mehnert W, Mäder K. Solid lipid nanoparticles: production, characterization and applications. Adv Drug Deliv Rev. 2001;47(2–3):165–96. https://doi.org/10.1016/s0169-409x(01)00105-3.
Dikmen G, Guney G, Genc L. Characterization of solid lipid nanoparticles containing caffeic acid and determination of its effects on MCF-7 cells. Recent Patents Anti-Cancer Drug Discov. 2015;10(2):224–32. https://doi.org/10.2174/1574892810666150115124413.
Guillot A, Couffin AC, Sejean X, Navarro F, Limberger M, Lehr CM. Solid phase extraction as an innovative separation method for measuring free and entrapped drug in lipid nanoparticles. Pharmaceut Res. 2015;32(12):3999–4009. https://doi.org/10.1007/s11095-015-1761-8.
Venishetty VK, Parikh N, Sistla R, Ahmed FJ, Diwan PV. Application of validated RP-HPLC method for simultaneous determination of docetaxel and ketoconazole in solid lipid nanoparticles. J Chromatogr Sci. 2011;49(2):136–41. https://doi.org/10.1093/chrsci/49.2.136.
Lv Y, He H, Qi J, Lu Y, Zhao W, Dong X, Wu W. Visual validation of the measurement of entrapment efficiency of drug nanocarriers. Int J Pharmaceut. 2018;547(1):395–403. https://doi.org/10.1016/j.ijpharm.2018.06.025.
Berry MR, Likar MD. Statistical assessment of dissolution and drug release profile similarity using a model-dependent approach. J Pharmaceut Biomed Anal. 2007;45(2):194–200. https://doi.org/10.1016/j.jpba.2007.05.021.
Shah VP, Midha KK, Dighe S, McGilveray IJ, Skelly JP, Yacobi A, Layloff T, Viswanathan CT, Cook CE, McDowall RD. Analytical methods validation: bioavailability, bioequivalence and pharmacokinetic studies. Conference report. Eur J Drug Metab Pharmacokinet. 1991;16(4):249–55. https://doi.org/10.1007/bf03189968.
Arvaniti EC, Juenger MCG, Bernal SA, Duchesne J, Courard L, Leroy S, Provis JL, Klemm A, De Belie N. Determination of particle size, surface area, and shape of supplementary cementitious materials by different techniques. Mater Struct. 2015;48(11):3687–701. https://doi.org/10.1617/s11527-014-0431-3.
Kakkar D, Dumoga S, Kumar R, Chuttani K, Mishra AK. PEGylated solid lipid nanoparticles: design, methotrexate loading and biological evaluation in animal models. Med Chem Commun. 2015;6(8):1452–63. https://doi.org/10.1039/C5MD00104H.
Danaei M, Dehghankhold M, Ataei S, Hasanzadeh Davarani F, Javanmard R, Dokhani A, Khorasani S, Mozafari MR. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics. 2018. https://doi.org/10.3390/pharmaceutics10020057.
Xu R. Progress in nanoparticles characterization: sizing and zeta potential measurement. Particuology. 2008;6(2):112–5. https://doi.org/10.1016/j.partic.2007.12.002.
Pang LSK, Saxby JD, Chatfield SP. Thermogravimetric analysis of carbon nanotubes and nanoparticles. J Phys Chem. 1993;97(27):6941–2. https://doi.org/10.1021/j100129a001.
Melo MN, Pereira FM, Rocha MA, Ribeiro JG, Junges A, Monteiro WF, Diz FM, Ligabue RA, Morrone FB, Severino P, Fricks AT. Chitosan and chitosan/PEG nanoparticles loaded with indole-3-carbinol: characterization, computational study and potential effect on human bladder cancer cells. Mater Sci Eng C. 2021;124:112089. https://doi.org/10.1016/j.msec.2021.112089.
Esposito E, Sguizzato M, Drechsler M, Mariani P, Carducci F, Nastruzzi C, Cortesi R. Progesterone lipid nanoparticles: Scaling up and in vivo human study. Eur J Pharmaceut Biopharmaceut. 2017;119:437–46. https://doi.org/10.1016/j.ejpb.2017.07.015.
Ravani L, Esposito E, Bories C, Moal VL, Loiseau PM, Djabourov M, Cortesi R, Bouchemal K. Clotrimazole-loaded nanostructured lipid carrier hydrogels: thermal analysis and in vitro studies. Int J Pharmaceut. 2013;454(2):695–702. https://doi.org/10.1016/j.ijpharm.2013.06.015.
Patil H, Kulkarni V, Majumdar S, Repka MA. Continuous manufacturing of solid lipid nanoparticles by hot melt extrusion. Int J Pharmaceut. 2014;471(1):153–6. https://doi.org/10.1016/j.ijpharm.2014.05.024.
Carbone C, Tomasello B, Ruozi B, Renis M, Puglisi G. Preparation and optimization of PIT solid lipid nanoparticles via statistical factorial design. Eur J Med Chem. 2012;49:110–7. https://doi.org/10.1016/j.ejmech.2012.01.001.
Nabi-Meibodi M, Vatanara A, Najafabadi AR, Rouini MR, Ramezani V, Gilani K, Etemadzadeh SMH, Azadmanesh K. The effective encapsulation of a hydrophobic lipid-insoluble drug in solid lipid nanoparticles using a modified double emulsion solvent evaporation method. Colloid Surface B Biointerfaces. 2013;112:408–14. https://doi.org/10.1016/j.colsurfb.2013.06.013.
Kotmakçı M, Akbaba H, Erel G, Ertan G, Kantarcı G. Improved method for solid lipid nanoparticle preparation based on hot microemulsions: preparation, characterization, cytotoxicity, and hemocompatibility evaluation. AAPS Pharm Sci Tech. 2017;18(4):1355–65. https://doi.org/10.1208/s12249-016-0606-z.
Battaglia L, Gallarate M, Cavalli R, Trotta M. Solid lipid nanoparticles produced through a coacervation method. J Microencapsul. 2010;27(1):78–85. https://doi.org/10.3109/02652040903031279.
Charcosset C, El-Harati A, Fessi H. Preparation of solid lipid nanoparticles using a membrane contactor. J Control Releas. 2005;108(1):112–20. https://doi.org/10.1016/j.jconrel.2005.07.023.
Passerini N, Gavini E, Albertini B, Rassu G, Di Sabatino M, Sanna V, Giunchedi P, Rodriguez L. Evaluation of solid lipid microparticles produced by spray congealing for topical application of econazole nitrate. J Pharm Pharmacol. 2009;61(5):559–67. https://doi.org/10.1211/jpp.61.05.0003.
Souto EB, Doktorovova S, Zielinska A, Silva AM. Key production parameters for the development of solid lipid nanoparticles by high shear homogenization. Pharmaceut Develop Technol. 2019;24(9):1181–5. https://doi.org/10.1080/10837450.2019.1647235.
Nair AB, Shah J, Al-Dhubiab BE, Jacob S, Patel SS, Venugopala KN, Morsy MA, Gupta S, Attimarad M, Sreeharsha N, Shinu P. Clarithromycin solid lipid nanoparticles for topical ocular therapy: optimization, evaluation and in vivo studies. Pharmaceutics. 2021. https://doi.org/10.3390/pharmaceutics13040523.
Pooja D, Tunki L, Kulhari H, Reddy BB, Sistla R. Optimization of solid lipid nanoparticles prepared by a single emulsification-solvent evaporation method. Data Brief. 2016;6:15–9. https://doi.org/10.1016/j.dib.2015.11.038.
Maleki G, Bahrami Z, Woltering EJ, Khorasani S, Mozafari MR. A review of patents on “Mozafari Method” as a green technology for manufacturing bioactive carriers. Biointerface Res Appl Chem. 2023;13:1.
Nasrollahzadeh M, Sajjadi M, Sajadi SM, Issaabadi Z. Chapter 5-Green nanotechnology. In: Nasrollahzadeh M, Sajadi SM, Sajjadi M, Issaabadi Z, Atarod M, editors. An introduction to green nanotechnology, vol. 28. Elsevier; 2019. p. 145–98.
Kumar A. Improving secondary metabolite production in tissue cultures. Plant Biol Biotechnol. 2015;8:397–406.
Mozafari MR, Javanmard R, Raji M. Tocosome: novel drug delivery system containing phospholipids and tocopheryl phosphates. Int J Pharmaceut. 2017;528(1–2):381–2. https://doi.org/10.1016/j.ijpharm.2017.06.037.
Mozafari MR. Nanoliposomes: preparation and analysis. Method Mol Biol (Clifton, NJ). 2010;605:29–50. https://doi.org/10.1007/978-1-60327-360-2_2.
Mohammadi L, Pal K, Bilal M, Rahdar A, Fytianos G, Kyzas GZ. Green nanoparticles to treat patients with Malaria disease: an overview. J Molr Struct. 2021;1229:129857.
Rahman K, Khan SU, Fahad S, Chang MX, Abbas A, Khan WU, Rahman L, Haq ZU, Nabi G, Khan D. Nano-biotechnology: a new approach to treat and prevent malaria. Int J Nanomed. 2019;14:1401–10. https://doi.org/10.2147/ijn.s190692.
Radwan A, El-Lakkany N, William S, El-Feky G, Al-Shorbagy M, Saleh S, Botros S. A novel praziquantel solid lipid nanoparticle formulation shows enhanced bioavailability and antischistosomal efficacy against murine S. mansoni infection. Parasite Vectors. 2019. https://doi.org/10.1186/s13071-019-3563-z.
de Souza AL, Andreani T, de Oliveira RN, Kiill CP, dos Santos FK, Allegretti SM, Chaud MV, Souto EB, Silva AM, Gremião MP. In vitro evaluation of permeation, toxicity and effect of praziquantel-loaded solid lipid nanoparticles against Schistosoma mansoni as a strategy to improve efficacy of the schistosomiasis treatment. Int J Pharm. 2014;463(1):31–7. https://doi.org/10.1016/j.ijpharm.2013.12.022.
Rafiei A, Soltani S, Ramezani Z, Abbaspour MR, Jelowdar A, Kahvaz MS. Ultrastructural changes on fertile and infertile hydatid cysts induced by conventional and solid lipid nanoparticles of albendazole and albendazole sulfoxide. Compr Clin Pathol. 2019;28(4):1045–53.
Soltani S, Rafiei A, Ramezani Z, Abbaspour MR, Jelowdar A, Kahvaz MS. Evaluation of the hydatid cyst membrane permeability of albendazole and albendazole sulfoxide-loaded solid lipid nanoparticles. Jundishapur J Natural Pharmaceut Product. 2017;12:2.
Andrade LN, Marques C, Barbosa T, Santos R, Chaud MV, da Silva CF, Corrêa CB, Amaral RG, de Souza NR, Gonsalves JKM. Praziquantel-loaded solid lipid nanoparticles: production, physicochemical characterization, release profile, cytotoxicity and in vitro activity against Schistosoma mansoni. J Drug Deliv Sci Technol. 2020;58: 101784.
Xie S, Pan B, Shi B, Zhang Z, Zhang X, Wang M, Zhou W. Solid lipid nanoparticle suspension enhanced the therapeutic efficacy of praziquantel against tapeworm. Int J Nanomed. 2011;6:2367.
Sharma S, Goel V, Kaur P, Gadhave K, Garg N, Singla LD, Choudhury D (2021) Bioinspired dual-functional solid lipid nanoformulations for targeted drug delivery and sustained release for enhancement of potency of albendazole, an antihelminthic drug. bioRxiv:2021.2007.2024.453620; 2021. https://doi.org/10.1101/2021.07.24.453620.
Ahmadnia S, Moazeni M, Mohammadi-Samani S, Oryan A. In vivo evaluation of the efficacy of albendazole sulfoxide and albendazole sulfoxide loaded solid lipid nanoparticles against hydatid cyst. Exp Parasitol. 2013;135(2):314–9.
Kudtarkar A, Shinde U, Bharkad G, Singh K. Solid lipid nanoparticles of albendazole for treatment of Toxocara canis infection: in-vivo efficacy studies. Nanosci Nanotechnol Asia. 2017;7(1):80–91.
Petrovska BB. Historical review of medicinal plants’ usage. Pharmacog Rev. 2012;6(11):1–5. https://doi.org/10.4103/0973-7847.95849.
Tucakov J. Healing with plants–phytotherapy. Beograd Cult. 1971;8:180–90.
Mohammad Rahimi H, Khosravi M, Hesari Z, Sharifdini M, Mirjalali H, Zali MR. Anti-toxoplasma activity and chemical compositions of aquatic extract of Mentha pulegium L. and Rubus idaeus L.: an in vitro study. Food Sci Nutr. 2020;8(7):3656–64. https://doi.org/10.1002/fsn3.1648.
Obeid MA, Al Qaraghuli MM, Alsaadi M, Alzahrani AR, Niwasabutra K, Ferro VA. Delivering natural products and biotherapeutics to improve drug efficacy. Therapeut Deliv. 2017;8(11):947–56. https://doi.org/10.4155/tde-2017-0060.
Lam PL, Wong WY, Bian Z, Chui CH, Gambari R. Recent advances in green nanoparticulate systems for drug delivery: efficient delivery and safety concern. Nanomedicine (Lond). 2017;12(4):357–85. https://doi.org/10.2217/nnm-2016-0305.
Jafarpour Azami S, Mohammad Rahimi H, Mirjalali H, Zali MR. Unravelling Toxoplasma treatment: conventional drugs toward nanomedicine. World J Microbiol Biotechnol. 2021;37(3):48. https://doi.org/10.1007/s11274-021-03000-x.
Yadav D, Suri S, Choudhary AA, Sikender M, Hemant BN, Beg NM. Novel approach: Herbal remedies and natural products in pharmaceutical science as nano drug delivery systems. Int J Pharm Tech. 2011;3(3):3092–116.
Singh RP, Singh SG, Naik H, Jain D, Bisla S. Herbal excipients in novel drug delivery system. Int J Compr Pharm. 2011;2:1–7.
Gunasekaran T, Haile T, Nigusse T, Dhanaraju MD. Nanotechnology: an effective tool for enhancing bioavailability and bioactivity of phytomedicine. Asian Pacific J Trop Biomed. 2014;4:S1–7. https://doi.org/10.12980/APJTB.4.2014C980.
Kheradmandnia S, Vasheghani-Farahani E, Nosrati M, Atyabi F. Preparation and characterization of ketoprofen-loaded solid lipid nanoparticles made from beeswax and carnauba wax. Nanomed Nanotechnol Biol Med. 2010;6(6):753–9.
Sutthanut K, Lu X, Jay M, Sripanidkulchai B. Solid lipid nanoparticles for topical administration of Kaempferia parviflora extracts. J Biomed Nanotechnol. 2009;5(2):224–32. https://doi.org/10.1166/jbn.2009.1026.
Dasam JM, Natarajan J, Karri V, Wadhwani AD, Antony J. Targeting efficacy of simvastatin for hormone-dependent carcinomas through solid lipid nanoparticles. J Nanomed Nanotechnol. 2016;7(6):1–7.
Shewale PB, Patil RA, Hiray YA. Antidepressant-like activity of anthocyanidins from Hibiscus rosa-sinensis flowers in tail suspension test and forced swim test. Indian J Pharmacol. 2012;44(4):454.
Vijayanand P, Jyothi V, Aditya N, Mounika A. Development and characterization of solid lipid nanoparticles containing herbal extract: in vivo antidepressant activity. J Drug Deliv. 2018;2018:2908626. https://doi.org/10.1155/2018/2908626.
Campos DA, Madureira AR, Sarmento B, Gomes AM, Pintado MM. Stability of bioactive solid lipid nanoparticles loaded with herbal extracts when exposed to simulated gastrointestinal tract conditions. Food Res Int. 2015;78:131–40. https://doi.org/10.1016/j.foodres.2015.10.025.
Rajwar TK, Pradhan D, Halder J, Rai VK, Kar B, Ghosh G, Rath G. Opportunity in nanomedicine to counter the challenges of current drug delivery approaches used for the treatment of malaria: a review. J Drug Target. 2023;31(4):354–68. https://doi.org/10.1080/1061186x.2022.2164290.
Mutabingwa TK. Artemisinin-based combination therapies (ACTs): best hope for malaria treatment but inaccessible to the needy! Act Trop. 2005;95(3):305–15. https://doi.org/10.1016/j.actatropica.2005.06.009.
Eastman RT, Fidock DA. Artemisinin-based combination therapies: a vital tool in efforts to eliminate malaria. Nat Rev Microbiol. 2009;7(12):864–74. https://doi.org/10.1038/nrmicro2239.
Baden L, Catteruccia F, Diabaté A, Donini C, Nosten F, O’Neill S, Osier F, Phyo AP, White N. Malaria-epidemiology, treatment, and prevention. New Engl J Med. 2023;388(5): e9. https://doi.org/10.1056/NEJMp2216703.
Yasri S, Wiwanitkit V. Artemisinin resistance: an important emerging clinical problem in tropical medicine. Int J Physiol Pathophysiol Pharmacol. 2021;13(6):152–7.
Ye R, Hu D, Zhang Y, Huang Y, Sun X, Wang J, Chen X, Zhou H, Zhang D, Mungthin M, Pan W. Distinctive origin of artemisinin-resistant Plasmodium falciparum on the China-Myanmar border. Sci Rep. 2016;6:20100. https://doi.org/10.1038/srep20100.
Fola AA, Feleke SM, Mohammed H, Brhane BG, Hennelly CM, Assefa A, Crudal RM, Reichert E, Juliano JJ, Cunningham J, Mamo H, Solomon H, Tasew G, Petros B, Parr JB, Bailey JA. Plasmodium falciparum resistant to artemisinin and diagnostics have emerged in Ethiopia. Nat Microbiol. 2023;8(10):1911–9. https://doi.org/10.1038/s41564-023-01461-4.
Greenwood B. Artemisinin-resistant and hrp-negative malaria parasites in Africa. New Engl J Med. 2023;389(13):1162–4. https://doi.org/10.1056/NEJMp2309142.
Miean KH, Mohamed S. Flavonoid (myricetin, quercetin, kaempferol, luteolin, and apigenin) content of edible tropical plants. J Agricult Food Chem. 2001;49(6):3106–12. https://doi.org/10.1021/jf000892m.
Tasdemir D, Lack G, Brun R, Rüedi P, Scapozza L, Perozzo R. Inhibition of Plasmodium falciparum fatty acid biosynthesis: evaluation of fabg, fabz, and fabi as drug targets for flavonoids. J Med Chem. 2006;49(11):3345–53. https://doi.org/10.1021/jm0600545.
Lehane AM, Saliba KJ. Common dietary flavonoids inhibit the growth of the intraerythrocytic malaria parasite. BMC Res Not. 2008;1(1):26. https://doi.org/10.1186/1756-0500-1-26.
Goy RC, Britto Dd, Assis OBG. A review of the antimicrobial activity of chitosan. Polímeros. 2009;19:241–7.
No HK, Park NY, Lee SH, Meyers SP. Antibacterial activity of chitosans and chitosan oligomers with different molecular weights. Int J Food Microbiol. 2002;74(1–2):65–72. https://doi.org/10.1016/s0168-1605(01)00717-6.
Stan D, Enciu A-M, Mateescu AL, Ion AC, Brezeanu AC, Stan D, Tanase C. Natural compounds with antimicrobial and antiviral effect and nanocarriers used for their transportation. Front Pharmacol. 2021;12:25.
Mikušová V, Mikuš P. Advances in chitosan-based nanoparticles for drug delivery. Int J Mol Sci. 2021. https://doi.org/10.3390/ijms22179652.
Shin GH, Kim JT. Observation of chitosan coated lipid nanoparticles with different lipid compositions under simulated in vitro digestion system. Food Hydrocolloid. 2018;84:146–53. https://doi.org/10.1016/j.foodhyd.2018.05.052.
Wang J-y, Wang Y, Meng X. Chitosan nanolayered cisplatin-loaded lipid nanoparticles for enhanced anticancer efficacy in cervical cancer. Nanoscale Res Lett. 2016;11(1):524. https://doi.org/10.1186/s11671-016-1698-9.
Liu H, Li Y, Zhang X, Shi M, Li D, Wang Y. Chitosan-coated solid lipid nano-encapsulation improves the therapeutic antiairway inflammation effect of berberine against COPD in cigarette smoke-exposed rats. Can Respirat J. 2022;2022:8509396. https://doi.org/10.1155/2022/8509396.
Kong M, Chen XG, Xing K, Park HJ. Antimicrobial properties of chitosan and mode of action: a state of the art review. Int J Food Microbiol. 2010;144(1):51–63. https://doi.org/10.1016/j.ijfoodmicro.2010.09.012.
Teimouri A, Azami SJ, Keshavarz H, Esmaeili F, Alimi R, Mavi SA, Shojaee S. Anti-Toxoplasma activity of various molecular weights and concentrations of chitosan nanoparticles on tachyzoites of RH strain. Int J Nanomed. 2018;13:1341–51. https://doi.org/10.2147/ijn.s158736.
Teimouri A, Haghi AM, Nateghpour M, Farivar L, Hanifian H, Mavi SA, Zare R. Antimalarial efficacy of low molecular weight chitosan against Plasmodium berghei infection in mice. J Vector Borne Dis. 2016;53(4):312–6.
Tavassoli M, Imani A, Tajik H, Moradi M, Pourseyed S. Novel in vitro efficiency of chitosan biomolecule against Trichomonas gallinae. Iran J Parasitol. 2012;7(1):92–6.
Yarahmadi M, Fakhar M, Ebrahimzadeh MA, Chabra A, Rahimi-Esboei B. The anti-giardial effectiveness of fungal and commercial chitosan against Giardia intestinalis cysts in vitro. J Parasit Dis. 2016;40(1):75–80. https://doi.org/10.1007/s12639-014-0449-z.
Parvez S, Yadagiri G, Karole A, Singh OP, Verma A, Sundar S, Mudavath SL. Recuperating biopharmaceutical aspects of amphotericin b and paromomycin using a chitosan functionalized nanocarrier via oral route for enhanced anti-leishmanial activity. Front Cell Infect Microbiol. 2020;10:24.
Riezk A, Van Bocxlaer K, Yardley V, Murdan S, Croft SL. Activity of amphotericin b-loaded chitosan nanoparticles against experimental cutaneous leishmaniasis. Molecules. 2020. https://doi.org/10.3390/molecules25174002.
Haddad A, Delavari M, Arbabi M, Gardeshmeydani I, Salmani A. Evaluation of anti-leishmaniasis activity of curcumin-loaded chitosan nanoparticles on Leishmania major and L. infantum in vitro. FEYZ. 2021;25(4):1040–6.
Riezk A, Raynes JG, Yardley V, Murdan S, Croft SL. Activity of Chitosan and its derivatives against Leishmania major and Leishmania mexicana in vitro. Antimicrob Agents Chemother. 2020. https://doi.org/10.1128/aac.01772-19.
Hassan MM, Abd El-Rahman EM, Abd El-Hamed EF, Abdel Fattah AS, Harb OA, Mohamed SAEN, Sarhan MH. The impact of nitazoxanide loaded on solid lipid nanoparticles on experimental trichinellosis. Zagazig Univ Med J. 2021;27(6):1074–84. https://doi.org/10.21608/zumj.2019.16531.1480.
Singh A, Mishra A, Chaudhary R, Kumar V. Role of herbal plants in prevention and treatment of parasitic diseases. J Sci Res. 2020;64:50–8.
Capela R, Moreira R, Lopes F. An overview of drug resistance in protozoal diseases. Int J Mol Sci. 2019. https://doi.org/10.3390/ijms20225748.
Monzote L, Siddiq A. Drug development to protozoan diseases. Open Med Chem J. 2011;5:1–3. https://doi.org/10.2174/1874104501105010001.
Kalepu S, Manthina M, Padavala V. Oral lipid-based drug delivery systems—an overview. Acta Pharmaceut Sin B. 2013;3(6):361–72. https://doi.org/10.1016/j.apsb.2013.10.001.
Nakmode D, Bhavana V, Thakor P, Madan J, Singh PK, Singh SB, Rosenholm JM, Bansal KK, Mehra NK. Fundamental aspects of lipid-based excipients in lipid-based product development. Pharmaceutics. 2022. https://doi.org/10.3390/pharmaceutics14040831.
Wiesgigl M, Clos J. Heat shock protein 90 homeostasis controls stage differentiation in Leishmania donovani. Mol Biol Cell. 2001;12(11):3307–16. https://doi.org/10.1091/mbc.12.11.3307.
Petersen A, Campos TA, Dantas D, Rebouças JS, da Silva JC, de Menezes JPB, Formiga FR, de Melo JV, Machado G, Veras PST. Encapsulation of the HSP-90 chaperone inhibitor 17-AAG in stable liposome allow increasing the therapeutic index as assessed, in vitro, on Leishmania (L) amazonensis amastigotes-hosted in mouse cba macrophages. Front Cell Infect Microbiol. 2018;8:303. https://doi.org/10.3389/fcimb.2018.00303.
Neva FA, Brown HW. Basic clinical parasitology; 1994.
Sepulveda MS, Kinsella JM. Helminth collection and identification from wildlife. J Vis Exp. 2013;82:e51000. https://doi.org/10.3791/51000.
Martin RJ. Modes of action of anthelmintic drugs. Vet J. 1997;154(1):11–34. https://doi.org/10.1016/S1090-0233(05)80005-X.
Lloyd AE, Honey BL, John BM, Condren M. Treatment options and considerations for intestinal helminthic infections. J Pharm Technol. 2014;30(4):130–9. https://doi.org/10.1177/8755122514533667.
Giordani C, Marin G, Pérez D, Soraci A, Errecalde J. Mechanism of action of drugs with activity against multicellular parasites. Parazitologiya. 2017;51:294–316.
Fissiha W, Kinde MZ. Anthelmintic resistance and its mechanism: a review. Infect Drug Resist. 2021;14:5403–10. https://doi.org/10.2147/idr.s332378.
McCracken RO, Taylor DD. Biochemical effects of thiabendazole and cambendazole on Hymenolepis diminuta (cestoda) in vivo. J Parasitol. 1983;69(2):295–301. https://doi.org/10.2307/3281226.
Pham K, Mertelsmann A, Mages K, Kingery JR, Mazigo HD, Jaka H, Kalokola F, Changalucha JM, Kapiga S, Peck RN, Downs JA. Effects of helminths and anthelmintic treatment on cardiometabolic diseases and risk factors: a systematic review. PLOS Negl Trop Dis. 2023;17(2):e0011022. https://doi.org/10.1371/journal.pntd.0011022.
Frayha GJ, Smyth JD, Gobert JG, Savel J. The mechanisms of action of antiprotozoal and anthelmintic drugs in man. Gen Pharmacol Vascul Syst. 1997;28(2):273–99. https://doi.org/10.1016/S0306-3623(96)00149-8.
Chen W, Mook RA Jr, Premont RT, Wang J. Niclosamide: beyond an antihelminthic drug. Cell Signal. 2018;41:89–96. https://doi.org/10.1016/j.cellsig.2017.04.001.
Castro-Hermida JA, González-Warleta M, Martínez-Sernández V, Ubeira FM, Mezo M. Current challenges for fasciolicide treatment in ruminant livestock. Trend Parasitol. 2021;37(5):430–44. https://doi.org/10.1016/j.pt.2020.12.003.
Mukherjee N, Mukherjee S, Saini DP, Roy P, Babu S. Phenolics and terpenoids; the promising new search for anthelmintics: a critical review. Mini Rev Med Chem. 2015. https://doi.org/10.2174/1389557515666150227114824.
Charvet CL, Guégnard F, Courtot E, Cortet J, Neveu C. Nicotine-sensitive acetylcholine receptors are relevant pharmacological targets for the control of multidrug resistant parasitic nematodes. Int J Parasitol Drugs Drug Resist. 2018;8(3):540–9. https://doi.org/10.1016/j.ijpddr.2018.11.003.
Page SW. Chapter 10-Antiparasitic drugs. In: Maddison JE, Page SW, Church DB, editors. Small animal clinical pharmacology. 2nd ed. Edinburgh: W.B. Saunders; 2008. p. 198–260. https://doi.org/10.1016/B978-070202858-8.50012-9.
Holden-Dye L, Walker RJ. Anthelmintic drugs and nematicides: studies in Caenorhabditis elegans. London: WormBook; 2014. p. 1–29. https://doi.org/10.1895/wormbook.1.143.2.
Beech RN, Skuce P, Bartley DJ, Martin RJ, Prichard RK, Gilleard JS. Anthelmintic resistance: markers for resistance, or susceptibility? Parasitology. 2011;138(2):160–74. https://doi.org/10.1017/s0031182010001198.
Thomas CM, Timson DJ. The mechanism of action of praziquantel: can new drugs exploit similar mechanisms? Curr Med Chem. 2020;27(5):676–96. https://doi.org/10.2174/0929867325666180926145537.
Eissa MM, El-Azzouni MZ, El-Khordagui LK, Abdel Bary A, El-Moslemany RM, Abdel Salam SA. Single oral fixed-dose praziquantel-miltefosine nanocombination for effective control of experimental schistosomiasis mansoni. Parasite Vectors. 2020;13:1–12.
Gnanasekar M, Salunkhe AM, Mallia AK, He YX, Kalyanasundaram R. Praziquantel affects the regulatory myosin light chain of Schistosoma mansoni. Antimicrob Agents Chemother. 2009;53(3):1054–60. https://doi.org/10.1128/aac.01222-08.
Kabatende J, Barry A, Mugisha M, Ntirenganya L, Bergman U, Bienvenu E, Aklillu E. Safety of praziquantel and albendazole coadministration for the control and elimination of schistosomiasis and soil-transmitted helminths among children in rwanda: an active surveillance study. Drug Saf. 2022;45(8):909–22. https://doi.org/10.1007/s40264-022-01201-3.
Lifschitz A, Lanusse C, Alvarez L. Host pharmacokinetics and drug accumulation of anthelmintics within target helminth parasites of ruminants. N Z Vet J. 2017;65(4):176–84. https://doi.org/10.1080/00480169.2017.1317222.
Eskandari M, Asgharzadeh F, Askarnia-faal MM, Naimi H, Avan A, Ahadi M, Vossoughinia H, Gharib M, Soleimani A, Naghibzadeh N, Ferns G, Ryzhikov M, Khazaei M, Hassanian SM. Mebendazole, an anti-helminth drug, suppresses inflammation, oxidative stress and injury in a mouse model of ulcerative colitis. Sci Rep. 2022;12(1):10249. https://doi.org/10.1038/s41598-022-14420-6.
Li P, Rios Coronado PE, Longstaff XRR, Tarashansky AJ, Wang B. Nanomedicine approaches against parasitic worm infections. Adv Healthc Mater. 2018;7(13): e1701494. https://doi.org/10.1002/adhm.201701494.
Paredes AJ, Llabot JM, Sanchez Bruni S, Allemandi D, Palma SD. Self-dispersible nanocrystals of albendazole produced by high pressure homogenization and spray-drying. Drug Develop Industr Pharm. 2016;42(10):1564–70.
Fontana F, Figueiredo P, Zhang P, Hirvonen JT, Liu D, Santos HA. Production of pure drug nanocrystals and nano co-crystals by confinement methods. Adv Drug Deliv Rev. 2018;131:3–21.
Barbosa EJ, Löbenberg R, de Araujo GLB, Bou-Chacra NA. Niclosamide repositioning for treating cancer: challenges and nano-based drug delivery opportunities. Eur J Pharmaceut Biopharmaceut. 2019;141:58–69.
Abidi H, Ghaedi M, Rafiei A, Jelowdar A, Salimi A, Asfaram A, Ostovan A. Magnetic solid lipid nanoparticles co-loaded with albendazole as an anti-parasitic drug: sonochemical preparation, characterization, and in vitro drug release. J Mol Liq. 2018;268:11–8.
Mishra A, Vuddanda PR, Singh S. Intestinal lymphatic delivery of praziquantel by solid lipid nanoparticles: formulation design, in vitro and in vivo studies. J Nanotechnol. 2014;2014:8.
Xiang B, Cao D-Y. Preparation of drug liposomes by thin-film hydration and homogenization. In: Lu W-L, Qi X-R, editors. Liposome-based drug delivery systems. Berlin: Springer; 2017. p. 1–11. https://doi.org/10.1007/978-3-662-49231-4_2-1.
Skuhala T, Trkulja V, Runje M, Vukelic D, Desnica B. Albendazolesulphoxide concentrations in plasma and hydatid cyst and prediction of parasitological and clinical outcomes in patients with liver hydatidosis caused by Echinococcus granulosus. Croatian Med J. 2014;55(2):146–55. https://doi.org/10.3325/cmj.2014.55.146.
Norbury LJ, Shirakashi S, Power C, Nowak BF, Bott NJ. Praziquantel use in aquaculture—current status and emerging issues. Int J Parasitol Drugs Drug Resist. 2022;18:87–102. https://doi.org/10.1016/j.ijpddr.2022.02.001.
Coeli R, Baba EH, Araujo N, Coelho PMZ, Oliveira G. Praziquantel treatment decreases Schistosoma mansoni genetic diversity in experimental infections. PLoS Negl Trop Dis. 2013;7(12): e2596.
Partridge GJ, Rao S, Woolley LD, Pilmer L, Lymbery AJ, Prestidge CA. Bioavailability and palatability of praziquantel incorporated into solid–lipid nanoparticles fed to yellowtail kingfish Seriola lalandi. Compar Biochem Physiol Part C Toxicol Pharmacol. 2019;218:14–20.
de Almeida AE, Souza ALR, Cassimiro DL, Gremião MPD, Ribeiro CA, Crespi MS. Thermal characterization of solid lipid nanoparticles containing praziquantel. J Therm Analys Calorimetr. 2012;108(1):333–9.
Acknowledgements
The authors thank all members of the Foodborne and Waterborne Diseases Research Center for their collaborations.
Funding
This project was financially supported by Shahid Beheshti University of Medical Sciences, Tehran, Iran with grant number: 43007082.
Author information
Authors and Affiliations
Contributions
Conceived and designed: HM and SA. Data gathering and literature review: MM PK. Illustrations and graphics: SN. Writing the manuscript: SN. Reviewing and editing the manuscript: HM. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in this study were in accordance with the ethical standards (IR.SBMU.RIGLD.REC.1402.007) released by the Ethical Review Committee of the Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran. As well, the study was approved by the ethics committee/institutional review board of the Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nemati, S., Mottaghi, M., Karami, P. et al. Development of solid lipid nanoparticles-loaded drugs in parasitic diseases. Discover Nano 19, 7 (2024). https://doi.org/10.1186/s11671-023-03955-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11671-023-03955-w