Abstract
Background
Despite the global increase in older employees, workplace physical activity interventions (WPAIs) for this target group have not yet been sufficiently developed. The major drawback of existing WPAIs is low adherence due to lack of time or limited motivation. A novel approach could be to integrate tailored neuromotor and strength exercises into everyday working tasks to prevent the functional decline of older employees at the workplace without needing much additional time for training. This approach was tested in the present study by evaluating the proof-of-concept of a novel WPAI based on the Lifestyle-integrated Functional Exercise (LiFE) program integrated into a working environment (wLiFE55 +).
Methods
The proof-of-concept of wLiFE55 + was quantified within a 4-week pre-post exercise intervention study by measuring (1) feasibility including adherence, activity frequency, adverse events and acceptance (integrability of wLiFE55 + activities, perceived improvement and safety, satisfaction, physical demand, personal trainer session, intervention content) and (2) pre-to-post changes in neuromotor function (12-Level Balance Scale, 12-LBS; Community Balance and Mobility Scale, CBM), strength (60sec Chair Stand Test), and PA (1-week activity monitoring). For statistical analysis, the median and interquartile range (IQR) were computed. For pre-to-post changes, Wilcoxon signed-rank tests with effect size (r) were also performed.
Results
Seventeen older employees (mean age 59 years, 8 female) were included of which fifteen completed the study. The intervention adherence was 100%, and the activity adherence was 58% (9 out of 12 maximum possible wLiFE55 + activities implemented). Depending on the specific activity, the frequency of practice ranged between 25–75% of the days of the intervention period, and single wLiFE55 + activities were practiced between one and three times per day. No adverse events occurred, and acceptance was high. Pre-to-post increases with medium effect sizes were found for neuromotor function (CBM, 12-LBS) and specific PA variables (total sedentary time, sedentary bouts > 30 min).
Conclusion
The results of the study highlight the feasibility of wLiFE55 + in a work setting with older employees. The pre-to-post increases observed in neuromotor measures and reductions in sedentary time suggest that wLiFE55 + may counteract the age-related functional decline in older employees and justifies future studies in this field. The next steps are program adjustments to boost exercise frequency and evaluating wLiFE55 + in a randomized controlled trial.
Similar content being viewed by others
Background
Population aging and older retirement age mean that more older employees (i.e., those aged 55 years and older [1, 2]) will remain in the workforce [3, 4]. An aging population means an aging workforce, making it essential for companies to recruit and retain older employees to meet their personnel requirements [5]. However, older employees face an age-related functional decline, and their physical work capacity is up to 50% lower [6]. Decreasing physical capacities include muscular strength and endurance [7] and neuromotor function (balance, agility, flexibility and coordination) [8,9,10,11].
Physical inactivity contributes to age-related functional decline [12, 13]. Without sufficient training, muscular strength decreases by approximately 10–15% per decade [14]. Maintaining muscle strength is important for health, as it is positively associated with metabolic function [15], and is fundamental for carrying out daily activities [16]. Neuromotor function decreases by 10% per decade [17], which can result in mobility impairments and falls. Neuromotor function is also positively associated with neurocognitive health [18].
Physical activity (PA) is a powerful tool for preventing age-related functional decline and maintaining strength and neuromotor function [19]. However, only 23% of adults comply with PA guidelines, and compliance continues to decline with age [20]. It is therefore particularly important to encourage people to stay physically active as they grow older. This also applies to PA at work. Therefore, companies must offer workplace physical activity interventions (WPAI) for older employees. The WPAI for older employees needs to specifically address the domains of strength and neuromotor function to counteract age-related decline [21]. A systematic review reported only a small number of WPAI for older employees. Most of these interventions focused on aerobic exercise. The authors explicitly called for the development of programs with strength and neuromotor training. Furthermore, all WPAIs were carried out in addition to work. These additional interventions require employees to take extra time outside their regular tasks, i.e. in exercise courses. However, these interventions are generally not seamlessly integrated into the work environment and are perceived as optional add-ons. Therefore, these treatments may be ineffective in the long run due to low adherence [22]. To maximize adherence, new WPAI tools to motivate older adults to adopt more physically active lifestyles in the workplace are needed.
One highly promising alternative approach is the Lifestyle-integrated Functional Exercise (LiFE) program, which integrates specific exercises for improving strength and neuromotor function into everyday activities while considering behavioral change to foster long-term adherence through habit formation [23, 24]. LiFE integrates short exercise bouts into everyday life for older adults (60 +), making it feasible without requiring additional time for an exercise program [25]. Previous studies [22] have shown successful integration with greater adherence to LiFE (64% of participants) than to additional training (53%) due to the high degree of ‘personalization’ of the integrated activities. A recent review paper [25] shows evidence that LiFE improves the physical capacity of various target populations. The most relevant studies for the present topic are related to the adapted aLiFE for young retired seniors [19, 24, 26,27,28]. The exercises as well as the behavioral change techniques have been adjusted for this younger target population [24]. Studies have demonstrated the feasibility of aLiFE [19, 26, 27] and its effects on specific physical capacity measures such as balance and mobility [24] and the use of technology [27]. However, to the best of our knowledge, aLiFE has not been transferred to a workplace setting yet.
Previous WPAI studies of older employees have not focused on integrating exercise into workplace routines [29]. Work commonly occupies almost half of the waking hours of older employees and therefore provides a large ‘time bank’ for offering multiple opportunities to integrate exercises into daily routines at the workplace [30]. Integrating PA to improve strength and neuromotor function in the work environment could be a promising strategy for employees in an office setting, as this group has little PA during work and could therefore particularly benefit from such training. The primary objectives of this study were 1) to develop a wLiFE55 + intervention by adapting aLiFE for the working environment and for a target group of older employees and 2) to assess the feasibility of the newly developed wLiFE55 + program. The secondary objectives included exploring pre-post-intervention changes in neuromotor function, strength, and PA patterns after 4 weeks of wLiFE55 + training.
Methods
The development and feasibility testing of the wLiFE55 + program were based on the framework for adapting public health interventions [31]. Stage 1 involved (a) community assessment, (b) expert consultation, and (c) adaptation of aLiFE to develop wLiFE55 +. Stage 2 included feasibility testing of wLiFE55 + in a pilot study.
Stage 1: development of the wLiFE55 + program
(a) Community assessment
Community assessment included (i) assessing organizational capacity to implement the program and (ii) need assessment. (i) To assess the organizational capacity required to implement the program and how recruitment should proceed, a meeting was held with the person responsible for the sports program (PB) and the person responsible for occupational health management (KM) at the University of Konstanz. The organization (University of Konstanz) expressed the capacity and need for wLiFE55 + and supported participant recruitment using flyers, mailing lists (newsletter), and a webpage. (ii) For need assessments, the first author (YR) and second author (DP) carried out literature research in the field of WPAI [32,33,34] and identified environmental and situational cues for integrating the wLiFE55 + activities into an office environment (see Table 1, appendix). The results of the need assessment were incorporated in stage (c).
(b) Expert consultation
Experts from sports science (MS, YR, DP), occupational health (SVM, GMS), occupational safety (RE, BW), and the occupational healthcare industry (FB, CK, BH) were consulted to discuss the adaptations for transferring the aLiFE concept to the new setting and target population. During joint meetings, it was discussed how the (i) aLiFE concept can be transferred to an office setting, (ii) what environmental (e.g., staple documents, set aside bin) and situational (e.g., enter the date in the calendar, phone call with colleague cues are relevant for incorporating wLiFE55 + activities into an office setting, and (iii) how to achieve an adequate training intensity to fulfill the ACSM criteria [9]. The experts decided that the aLiFE activities, designed for retired people (aged 60 +), are sufficiently challenging for older employees (aged 55 +) and meet the ACSM criteria for strength and balance exercises in terms of task challenge and progression. The exercises from aLiFE were retained for wLiFE55 +. In contrast, the environmental and situational cues had to be adapted because aLiFE has not been designed for a workplace setting. However, the behavioral change concept of aLiFE was retained [19].
(c) Adaptation of aLiFE to develop wLiFE55+
aLiFE is a variant of the LiFE program and has been specially developed for younger older people after retirement [24]. aLiFE served as the basis for the development of wLiFE55 +. aLiFE has been designed based on the ACSM guidelines for neuromotor function and strength training [9]. The aLiFE program targets age-related functional decline related to strength and neuromotor function by integrating personalized activities into daily routines [22] using established behavior change techniques [19]. The aLiFE activities were retained for wLiFE55 + as they have sufficient task challenge for older employees. However, because aLiFE was not developed as a WPAI, the program lacks the corresponding environmental and situational cues needed to integrate activities into daily routines at the workplace. These were added in the course of the adaptation (Table 1). For each activity, the participant manual was supplemented with information about situations offering opportunities for integration exercises into the working environment (Table 1). Based on the environmental and situational cues, the wLiFE55 + activities were subdivided into three categories: 1) on the way to work/ on the way home, 2) in the office, and 3) during the break.
Stage 2: feasibility pilot study
Study design and setting
A pilot study conducted at the University of Konstanz from March to July 2022 aimed to test the feasibility of wLiFE55 +. This study included a 4-week intervention with a pre-to-post design involving four personal trainer sessions at the workplace.
Study population
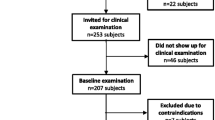
A convenient sample of 34 employees was recruited via flyer. The inclusion criteria were a minimum age of 55 years and current employment status. The exclusion criteria were having such diseases where exercise was contraindicated, attending organized exercise classes more than twice a week or exercising more than two hours each week. The participants provided written informed consent that was approved by the ethics committee of the University of Konstanz (ethical approval number: IRB23KN07-005w, date of approval: 12 July 2023). The study design is presented in Fig. 1. Eight participants were not eligible due to these inclusion and exclusion criterias.
Study procedures
Assessments
The pretest and post-assessments were conducted at the University of Konstanz, except for the ambulatory daily PA assessment. All measurements were validated and selected for the wLiFE55 + target group.
Administering the intervention
After the pretest, participants received the wLiFE55 + manual (see participant manual summary in the Supplementary file 1) and met a personal trainer (holding sports science degrees) for a 1.5-h session (see personal trainer session checklist in the Supplementary file 2). During this first session, the personal trainer (a) introduced the wLiFE55 + trainer by the use of the wLiFE55 + manual, (b) evaluated the ability and opportunities for wLiFE55 + activities using the Daily Routine Chart (see Supplementary file 3), (c) assessed the level of difficulty for each activity using the wLiFE55 + Assessment Tool (wLAT55 +) (see Supplementary file 4), (d) discussed goal setting about short- and long term fitness goals, (e) implemented up to four activites (neuromotor function, strength, and PA) linked to specific environmental and situational cues in the working environment, such as working tasks, situations or places, using the Daily Routine Chart (see Supplementary file 3) and the Activity Planner (see Supplementary file 5).
In the 2nd, 3rd and 4th training sessions, the personal trainer (a) clarified any questions related to the wLiFE55 + program, (b) reviewed the wLiFE55 + activities commenced previously, the Activity Planner, (c) taught ways of making the program more effective (upgrading wLiFE55 + activities), (d) implemented up to four wLiFE55 + activities and (e) developed plans for embedding the wLiFE55 + activities into the daily routine. Personal trainers motivated participants and supported adjusting wLiFE55 + activities over three follow-up sessions based on preferences. wLiFE55 + activities were documented in the Activity Planner with details on how, when, and where to perform them, aligning with HAPA (Health Action Process Approach) model recommendations, specifically adjusted to the LiFE concept [19]. The HAPA model served to enrich habit formation theory because of its emphasis on motivational and volitional factors during behavior change. For the planning procedure, participants used implementation intentions [35] by writing the environmental and situational cue followed by the wLiFE55 + activity in if–then sentences (e.g., “If I turn on my computer, then I do the tandem stand”). The integration of behavior change techniques including HAPA into the LiFE program is explained in Boulton, Hawley-Hague [19] and was also used in wLiFE55 + . Intrinsic motivation is another beneficial factor for long-term maintenance PA behavior [36]. Therefore, wLiFE55 + fulfills three psychological needs (autonomy, competence, and connectedness) by empowering participants to independently manage their training and become their own LiFE trainers [37].
Measurements
Participant characteristics
For the descriptive data, a self-developed questionnaire asked for personal data such as weight, height, education, profession, current working situation, and job satisfaction.
Feasibility measures obtained during intervention:
-
Adherence: Drop-out rate, intervention adherence and activity adherence.
-
o
Drop-out rate: Percentage of those who dropped out of the intervention.
-
o
Intervention adherence: Number of participants in the personal trainer sessions.
-
o
Activity adherence: Number of wLiFE55 + activities integrated during the intervention in daily life. During each session, a maximum of 4 wLiFE55 + activities could be integrated, for a total of 16.
-
o
-
Frequency of practice: Number of wLiFE55 + activities per day and percentage of days for each activity reported by the participant in the ‘Activity Planner‘.
-
o
Daily frequency practice: For each activity, frequency per day, the data were summed and divided through all days the participants executed the activity.
-
o
Weekly percentage of practice days during the intervention: For each activity, the percentage of days in which the activity was performed was divided by the total days in the intervention’s duration.
-
o
-
Muscle soreness: pain in the muscles after training
-
Adverse events: included self-reported pain and accidents during the intervention.
Feasibility measures obtained post-intervention:
-
Acceptability of wLiFE55 + activities: defined as integrability, perceived improvement, satisfaction with progress, perceived safety, and physical demands of wLiFE55 + activities using a 6-point Likert scale. Each question was followed by an open-ended question to explain the given ratings.
-
Acceptability of the wLiFE55 + program: overall reported acceptability, using a 6-point Likert-scale. Each question was followed by an open-ended question to explain the given ratings.
-
Activity preferences: three favorite wLiFE55 + activities.
Exploratory pre-post measures of subjective assessments:
The Activities-Specific Balance Confidence-Scale (ABC-D) [38] was used to assess fall-associated self-efficacy. The normal and complex activity scores were calculated. The International Physical Activity Questionnaire (IPAQ) measures movement behavior and categorizes it into different activities, such as profession, transport, household, and leisure time [39]. We used the IPAQ to calculate the walking activity time, moderate activity time, vigorous activity time, and total PA activity time.
Exploratory pre-post-measures of objective assessment:
Neuromotor function: We used the 12-Level-Balance Scale (12-LBS) to asses static balance. It is an extended version of the 8-Level Balance Scale (8-LBS) [23]. The 12-LBS is a series of static standing positions with increasing difficulty, which is achieved by a) a reduction in the support area, b) sensory handicaps (eyes closed), and c) additional cognitive tasks (see Supplementary file 6). The participants had to complete a balance task for 30 s without support or to perform a reactive step or arm movement before progressing to the next task. The highest balance test performed successfully was rated (maximum score: 12 points). Similarly, the Community Balance Mobility Scale (CBM) was used to assess balance and mobility through 13 items, including unilateral stance, tandem walking, 180° tandem pivot, lateral foot scooting, hopping forward, crouch and walk, lateral dodging, walking and looking, running with controlled stop, forward to backward walking, walk, look and carry, descending stairs, and step-up 1 × step [40]. Except for unilateral stance, all CBM items evaluate dynamic balance. Each item was rated based on standardized instructions and scoring guidelines (range 0–5 points), with a maximum possible score of 96 points.
Strength: The 60sec Chair Stand Test (60CST) was utilized to assess lower extremity strength by measuring the number of times participants could stand up and sit down on a chair (45 cm height) without arms within 60 s [41]. For this purpose, the total number of repetitions is presented. To avoid ceiling effects, we chose the 12-LBS, CBM, and 60CST as measuring instruments to challenge the higher performance level of older employees.
PA: PA was monitored using the Move 3 accelerometer (move III, movisens GmbH, Karlsruhe, Germany) [42], which was worn on the high wrist. The sensor wear time was recorded, and the PA was categorized before the first and after the fourth personal trainer session. The sensor was removed during water immersion and overnight periods. PA variables were computed with DataAnalyzer (Movisens GmBH, Karlsruhe, Germany, version 1.13.7) and R (software package, version 2023.06.0 + 421). The sensor wear time encompassed the total minutes worn daily (from waking to bedtime). The following PA variables were categorized: activity-related (standing time, PA time, sit-to-stand transfers, steps) and sedentary-related (sedentary time, sedentary bouts > 20 min, > 30 min, and > 60 min and their counts).
Activity-related PA variables: The standing time was extracted from activity class 9 (standing) in DataAnalyzer, and the daily minutes were totaled. PA activity time encompassed the sum of activity classes 4 (slope up), 5 (jogging), 6 (slope down), and 7 (walking) from DataAnalyzer, with daily PA minutes. The step count was derived from the DataAnalyzer daily data. Sit-to-stand transfers were calculated when transitioning from activity class 8 (sitting) to either 9 (standing) or 2 (PA).
Sedentary-related PA variables: Sedentary time was classified as activity class 8 (sitting/lying), and sedentary bouts were calculated and separated into bouts of > 20 min, > 30 min and > 60 min. The total time and the number of each sedentary bout were calculated.
Statistical analysis
Participant characteristics were reported using measures of central tendency (mean, median) and dispersion (SD = standard deviation, IQR = interquartile range), and were analyzed with the JASP Team (2023) (version 0.16.3). Pre-to-post changes were explored using the Wilcoxon signed-rank test because the data was not normally distributed. The effect size (r) for the Wilcoxon test is given by the match rank biserial correlation. The effect size (r) is calculated as the Z statistic divided by the square root of the sample size (N) (Z\(\sqrt N\)) [43]. The effects were interpreted as small (r = 0.1), medium (r = 0.3), or large (r = 0.5). A p-value less than 0.05 was considered significant, and a p-value greater than 0.05 was considered not significant. Additionally, a subanalysis was performed for low functioning participants for pre-to-post changes based on the median split.
Results
Thirty-four older employees were screened for eligibility, and 17 were included (Fig. 1). Two participants dropped out after the baseline assessment, reportedly because of no interest or lack of time. No outcome analyses were conducted for these two participants. No adverse events were reported in the study. Fifteen participants completed the study and were included in the analysis.
Descriptive data
The sample comprised older employees aged 55–68 years (Table 2). Baseline balance and mobility function were high (CBM score 8 points above the reference value [44]). Strength, as measured by the 60CST, ranged between 30 and 63 repetitions. Sedentary behavior (620 min/day) was greater than that reported in a literature review (approximately 600 min/day) [45]. The baseline steps (9262 steps per day) were in the range of a “somewhat active” (7500–9999 steps/day) group [46].
On average, the participants had a high level of education, and most (80%) were permanently employed. The majority (67%) worked in flextime. The participants worked in the following professional fields: technical professions (n = 5), administrative professions (n = 9), and healthcare professions (n = 3). On average, they worked 34.1 (± 9.4) hours per week and spend 3.6 (± 1.5) days in the office and 1.4 (± 1.5) days working from home. Nine participants worked in a single office, and eight participants worked in a two-person office or multiroom office. On average, participants tended to be satisfied with their job, with few having concerns about job change (see Supplementary file 7).
Adherence
All participants included in the analysis (n = 15) showed 100% intervention adherence. Of a maximum possible 16 wLiFE55 + activities, participants carried out an average of 9 wLiFE55 + activities (± 1.5, range 7–12) during the intervention, corresponding to a mean activity adherence of 57% (range: 44–75%). wLiFE55 + strength activities were most frequently implemented (mean = 3.7 ± 1, range 2–5), followed by wLiFE55 + neuromotor activities (mean = 3.3 ± 0.7, range 2–5) and PA (mean = 2.2 ± 0.7, range 1–3).
Frequency of practice
Participants included in the analysis (n = 15) most frequently implemented lunging for the strength module, one-leg stand and tandem walk for the neuromotor module, and walking faster for the PA module, while least frequently implementing toe and heel standing and walking, stepping and changing direction, and sitting less (Table 3).
The weekly frequency of practice ranged between 25 and 75% days/week depending on the activity. For wLiFE55 + activities implemented by more than three participants, the highest frequencies were reported for tightening muscles (strength module), one-leg stand (neuromotor function module) and break up sitting (PA module), and the lowest frequencies were reported for toe standing and walking, square stepping, leaning, hopping or jumping and walking longer. (Table 3).
The daily frequency of practice ranged between 1 and 2.99 times per day depending on the activity. The highest frequencies were reported for sit-to-stand (strength module), stepping over objects (neuromotor function module), and sit less (PA module), and the lowest frequencies were reported for toe/ heel standing and walking, square stepping, hopping or jumping, leaning and walking longer. (Table 3).
Muscle soreness
Four participants reported muscle soreness after beginning the intervention, but none reported worsening pain or prolonged exercise-related symptoms from the wLiFE55 + activities.
Acceptability of wLiFE55 + activities
Participants included in the analysis (n = 14) found it rather easy to integrate wLiFE55 + activities into their commutes. They perceived it more challenging to integrate them into daily work routines and non-work-related activities (Table 4). Most of the participants perceived some intervention-related improvements in neuromotor function, strength, and PA. Most felt safe when performing unsupervised wLiFE55 + activities and found it physically demanding. There was moderate or strong consensus for all items.
Acceptability of the wLiFE55 + program
Participants rated wLiFE55 + as good, highly recommended it to a friend or colleague and were willing to continue the program in the future (Table 5). Many participants found it ‘rather helpful’ to learn wLiFE55 + in a group with others. They were quite satisfied with their results from the wLiFE55 + program. Participants enjoyed the personal trainer sessions and found the instructions and exchanges very helpful. Repeated practice of wLiFE55 + activities and discussing specific activity situations with the personal trainer were rated as helpful. Theoretical content about the wLiFE55 + program was found to be useful, while the ‘if–then’ sentences for planning the wLiFE55 + activities were perceived only as ‘rather helpful ‘.
Activity preferences
Stair climbing was the most frequently mentioned as the favorite activity, followed by one-leg stand and tandem-walk. Square stepping, hopping, jumping and walking faster were not among the favorite wLiFE55 + activities. (Fig. 2).
Exploratory pre-post measures of subjective assessments
Balance confidence did not change from pre to post. The descriptive IPAQ results and small effect sizes (r = -0.162-0.385) indicated increased PA, although the difference was not significant (p = 0.255-0.616). (Table 6).
Exploratory pre-post measures of objective assessments for the total sample
For neuromotor function, the descriptive 12-LBS and CBM results and medium effect sizes (12-LBS: r = -0.600, CBM: r = -0.667) indicated increased neuromotor performance, with significance for CBM (p = 0.030).
For strength, the descriptive 60CST results increased with a medium effect size (r = -0.462).
The results for activity-related PA, standing time, PA, and steps suggested increased activity-related PA with small effect sizes (r = -0.209-0.429). The results of the repetitions from sit-to-stand transfers and small effect size (r = -0.538) indicated increased sit-to-stand transfers per day.
For sedentary-related PA, the descriptive sedentary behavior results and medium effect size (r = 0.516) indicated reduced sedentary time. For sedentary bouts > 20 min, > 30 min and > 60 min, the descriptive sedentary time decreased from pre to post, with medium effect sizes (r = 0.560-0.736). The number of sedentary bouts > 20 min, > 30 min, and > 60 min decreased with small to medium effect sizes (r = -0.055-0.648), with a significant difference for sedentary bouts > 60 min (p = 0.040). (Table 7).
Exploratory pre-post measures of objective assessments for low-function participants
Subanalysis revealed a statistically significant difference in neuromotor function (12-LBS: r = -1.00; p = 0.026, CBM: r = 0.857; p = 0.047) and strength (60CST: r = 1.00; p = 0.036) between the low functioning participants in the pre-post comparison, with improvements from pretest to posttest. For PA, sit-to-stand transfer increased significantly (p = 0.016) with a large effect size (r = 1.000) (see Supplementary file 8).
Discussion
This study indicates the feasibility of wLiFE55 + , as shown by measures of adherence and acceptance. Successful recruitment of the target population and overall positive feedback highlight the potential of wLiFE55 + as an innovative WPAI. For each wLiFE55 + domain (i.e. strength, neuromotor function, PA), several wLiFE55 + activities were integrated into commutes, during work, and daily life. Furthermore, our results suggest significant intervention-related pre-post increases in neuromotor function and PA parameters related to sedentary behavior. Participants with low baseline performance will benefit from wLiFE55 + .
Adherence
High drop-out rates (22%) have been reported for WPAIs using exercise approaches conducted in addition to working hours [47]. With wLiFE55 + , the drop-out rate is much lower (12%), less time is required for training, and integration into everyday activities is easier.
Intervention adherence (100%) was greater than that for other WPAIs, for which adherence rates ranging from 57–99% have been reported [48]. We realized that the participants appreciated the personal trainer sessions, which is consistent with other studies [49]. These intervention sessions not only motivated our participants, but also provided flexibility by allowing rescheduling to avoid conflicts with other appointments. The results suggest that one-on-one personal training is an effective method for changing attitudes and increasing the amount of PA [50].
The average activity adherence was 58% with 9 wLiFE55 + activities out of 16 implemented. Participants could decide on the number of wLiFE55 + activities according to their time capacity. The mean activity adherence for the three domains (3.7–2.2 wLiFE55 + activities/per week) in our study was lower than that in previous LiFE studies summarized in reviews (4.9 wLiFE55 + activities/per week) [22, 25, 51]. In contrast to all previous LiFE studies, our target population was younger, not retired, and relatively healthy. Therefore, our participants’ subjective need to integrate wLiFE55 + activities may have been lower than that reported in previous studies in older, more impaired target populations.
Frequency of practice
A higher frequency of practice is generally associated with greater effects [52]. Unlike structured training programs using multiple sets and rest intervals for counting the frequency of practice [53], wLiFE55 + integrates activities into daily routines, resulting in repetitions throughout the week.
Similar to aLiFE, neuromotor activities were practiced most frequently by the majority of participants, followed by strength activities and PA. Participants may have prioritized neuromotor activities due to perceived deficits, while their relatively high baseline PA status may have reduced interest in further increasing activity levels. According to previous studies, time constraints and employment status may explain the lower practice frequency among retired participants [22]. Nevertheless, our exploratory analysis suggested that even with reduced implementation, wLiFE55 + positively impacts physical capacity in our employed population.
Muscle soreness
Challenging exercises are associated with numerous positive effects [54]. Only a few participants reported muscle soreness after starting the intervention. This disappeared during the study, suggesting that wLiFE55 + activities did not overtax the participants. Muscle soreness is a common training effect for untrained individuals [55, 56].
Acceptability of the wLiFE55 + activities
The integrability of wLiFE55 + activities varied with the environment. Commuting had the highest integrability, likely due to lower stress, less observation, and ample space for wLiFE55 + activities. However, integrability was lower in the workplace and daily life, possibly due to time constraints and cognitive demands [57]. The acceptance of wLiFE55 + activities differed by domain. Participants perceived the most improvement in strength and PA, whereas assessing neuromotor function was less popular. Whenever participants executed wLiFE55 + activities they felt safe and rated the wLiFE55 + activities as physically demanding. This justifies further investments in the development of wLiFE55 + .
Previous studies have shown that an employee’s setup at work affects their movements at work, such as walks to the coffee machine [58]. Therefore, differences in workplaces may also affect the integration of the wLiFE55 + activities. Such influence may be measured in future studies by systematically analyzing the workplace configuration [59].
Acceptability of the wLiFE55 + program
Participants showed good acceptance of the wLiFE55 + program. A "good" rating indicates successful intervention development, and opinions on learning the program in a group varied, possibly due to individual preferences. Personalized approaches offering both individual- and group-based LiFE training may enhance acceptance [60,61,62]. The high enjoyment levels during personal trainer sessions and nonsupervised LiFE training highlight the intervention's potential for older employees.
The results show that the use of personal trainers sessions is very important for the high acceptability and adherence of the wLiFE55 + program. On the same note, personal trainer sessions may also pose some challenges for its practical implementation including costs and lost working time for the company (if the personal training sessions take place during working hours). In a previous LiFE study, some personal trainer sessions were replaced by telephone calls after a few weeks [63], which may reduce the costs. The use of a group program with one personal trainer session for several participants may also be an option for more cost-effective implementation [63].
Activity preferences
Three of the most favorably rated exercises are from the neuromotor function module, indicating a greater acceptance of neuromotor training among older employees. These wLiFE55 + activities can be performed in limited space without causing sweating. The participants found the neuromotor exercises to be novel, and their motivation to improve may have been high due to the challenges shown in the pretest. In the strength module, stair climbing was the preferred activity, likely because it can be easily incorporated into daily life.
Exploratory pre-post measures of subjective assessments
The limited effects observed for balance confidence are related to ceiling effects, as shown by the high baseline values.
Exploratory pre-post measures of objective assessments for the total sample
The large effect size and significant improvement observed in CBM performance may suggest a clinically relevant effect on balance and mobility performance for older employees. These findings are consistent with previous LiFE studies [24, 25] Our participants already had a very good balance and mobility, as indicated by a CBM score of 81.7 points (normal value 50–59 years: 77 points; 60–69 years: 65 points) [44]. Nevertheless, our findings suggest that the wLiFE55 + program could further improve balance for these participants.
The medium effect (r = 0.462) observed in the 60CST may suggest a training effect induced by wLiFE55 + . This result is in line with short-term strength exercises of 4 weeks [64], and greater improvement in strength performance can be expected for long-term interventions (12 weeks) [65].
For activity-related PA, each variable increased, leading to the assumption that PA improved with increasing wLiFE55 + activities. The participants showed, on average, a 10 min longer standing and PA time for the posttest. The number of steps increased, including the wLiFE55 + activities for PA.
For sedentary-related PA, each variable decreased. The total sedentary time, as well as the sedentary bouts > 20 min, > 30 min, and > 60 min, decreased significantly which is consistent with the activity preferences for break-up sitting and sitting less [66].
Based on our proof-of-concept study, the majority of participants seem to benefit from wLiFE55 + . On the same note, few participants may not benefit from the intervention for specific outcomes such as strength or sedentary behavior. A responder analysis needs to be conducted in a larger study.
Exploratory pre-post measures of objective assessments: low function participants
The analyzed dose–response relationship between baseline performance and improvement through the wLiFE55 + program showed that low function participants improved significantly in neuromotor function (12-LBS and CBM), strength, and PA for sit-to-stand transfers. Compared to the total sample, the effects were greater in all domains, and the improvement became significant in the 12-LBS, 60CST and sit-to-stand transfer. Participants with low function, in particular, benefited from the wLiFE55 + activities, which is consistent with previous literature [67]. Further analysis is necessary to determine the optimal doses for improving physical capacity and activity [68].
Refinement of wLiFE55+
Based on the pilot study, we propose four major refinement suggestions for items with two points below the maximum score in the acceptance questionnaire. First, the wLiFE55 + program will be shortened for wLiFE55 + activities with the lowest frequency. Toe walking and heel walking for the strength module, and stepping and changing direction for the neuromotor function module will be excluded. For the PA module, no wLiFE55 + activity was excluded, as it consisted of only four wLiFE55 + activities. Second, for the category integrability, we wanted to improve the integration of wLiFE55 + activities into daily work routines. Therefore, we will use qualitative data to better understand the difficulties of the participants (published separately). Third, for the two categories of perceived improvement and satisfaction with progress for the three domains, we propose increasing the difficulty of the wLiFE55 + activities and increasing the duration of the intervention. Fourth, for helpfulness learning wLiFE55 + in a group, we suggest developing a mixed design of group sessions and individual personal trainer sessions consistent with previous results [69].
Strategies to maintain motivation
One option for future wLiFE55 + studies is the integration of a digital approach that allows participants to track their progress and record their goals. The feasibility of such an approach for implementing aLiFE in retired seniors has been previously demonstrated [70] and might be translatable to wLiFE55 + . Digital technology may foster visualization of the participant’s current level of performance, setting goals, and allow objective assessment of their progress by activity tracking. A smartphone app may allow participants to document their wLiFE55 + activities and progress via a special app. Studies have shown that visualizing progress, for example, through progress bars, can increase participants' motivation and promote health-promoting behavioral changes [71,72,73]. An app may also foster participant-trainer interaction. Personalized attention allows us to address individual needs and progress and support participants during the intervention [19, 69, 74].
Another strategy for boosting motivation could be gamification. In this context, there is the possibility of introducing elements such as point systems or leaderboards to further motivate participants and encourage long-term participation. These approaches have already been shown to be effective, especially in older adults [75, 76].
Collaborations with health insurance companies and their bonus programs may offer participants a financial incentive for long-term participation in wLiFE55 + . In summary, several options exist to further develop wLiFE55 + to foster participant motivation and achieve sustainable implementation of our training program.
Adaptation
Future studies could adapt wLiFE55 + to different work environments such as manufacturing. Upper body exercises could be established, as work in production sometimes requires good upper limb strength [77]. In general, adaptations of the wLiFE55 + to other jobs should be based on a structured framework to determine the exact needs of workers in their workplace [31].
Limitations
Our study used a convenient sample of university employees who possess a high education level and flexibility in organizing work. The findings may not apply to older employees in different occupations and working conditions [78]. The convenience sample including a small number of participants limits the generalizability of our findings. To overcome these limitations, the next step involves consecutively recruiting larger samples of older employees from a broader range of working contexts to investigate the effects of wLiFE55 + . The feasibility of personal trainer sessions in real life scenarios (e.g., companies) needs to be proven.
However, the present sample was sufficient for testing the initial feasibility of the wLiFE55 + program. Although the short intervention period allowed us to assess the acceptability of wLiFE55 + and identify areas for further development, longer interventions are necessary to evaluate behavior change and adoption of the program [31]. The implementation of numerous wLiFE55 + activities within a short timeframe may have overwhelmed some participants, but it also helped us identify the most accepted wLiFE55 + activities within the target population. Longer intervention periods would allow participants to establish habits of their preferred activities and progressively increase the difficulty level for optimal task challenges. As we lacked a control group, we cannot draw definitive conclusions about the effectiveness of wLiFE55 + . For the pilot study we deliberately did not use a control group due to the exploratory, hypothesis-generating nature of the study. The aim was not to prove the effects of wLiFE55 + . Additionally, the subanalysis low functioning sample was small. Nonetheless, our findings suggest that individuals with lower functional performance may benefit more and could be the focus of future studies.
Impact and application for future research
Our study shows the successful development of a new innovative WPAI specifically designed for counteracting the functional decline of older employees by carrying out strength and neuromotor exercises. To the best of our knowledge, it is the first WPAI program integrating exercise into daily routines at the workplace. The high level of adherence and acceptance supports the success of the wLiFE55 + intervention development.
As we gave the participants a choice of exercises, we were able to identify the most suitable exercises (e.g. climbing stairs, one-leg stand, tandem walk) building the basis for future studies. Our findings highlight the importance of a personal trainer in the context of program acceptance. This finding should be incorporated into the further development of wLiFE55 + . To reduce the costs of a personal trainer, the wLiFE55 + program may be examined in a group format, previously developed for retired adults [63]. Using such a format, older employees could exchange ideas on the best ways to integrate training in the workplace.
Based on our pilot study, the next step is evaluating the effectiveness of wLiFE55 + within a follow-up study including a longer intervention period and a consecutively recruited sample. We would like to address the following questions in the next study: Can the wLiFE55 + program significantly improve neuromotor function, strength and PA in comparison to other WPAIs such as exercise courses? Can long-term effects be achieved? Can the wLiFE55 + program be transferred to other working environments? Can the wLiFE55 + program reduce the number of days employees are absent from work? The transfer of wLiFE55 + to people with a low level of education is another future field of research.
Conclusion
This pilot study demonstrated the feasibility of using wLiFE55 + to improve health-related factors in older adults, including neuromotor function, strength, and PA. The development stages of wLiFE55 + were successful and involved community access, expert consultations, and the creation of a participant manual. The pilot study showed significant improvements in these factors after a 4-week intervention. The positive feedback from participants justifies the continuation of wLiFE55 + as a supplementary WPAI for older employees. This study addresses previous shortcomings in integrated WPAIs by targeting the needs of older employees and achieving high adherence. This study represents an important step toward preventing functional decline and serves as a basis for future evaluation and implementation of wLiFE55 + .
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Abbreviations
- PA:
-
Physical Activity
- WPAI:
-
Workplace Physical Activity Intervention
- LiFE:
-
Lifestyle-integrated Functional Exercise
- aLiFE:
-
adapted Lifestyle-integrated Functional Exercise for young retired seniors
- wLiFE55 + :
-
workLiFE55 +
- ACSM:
-
American College of Sports Medicine
- wLAT55 + :
-
wLiFE55 + Assessment Tool
- HAPA:
-
Health Action Process Approach
- ABC-D:
-
Activities-Specific Balance Confidence-Scale
- IPAQ:
-
International Physical Activity Questionnaire
- 12-LBS:
-
12-Level Balance Scale
- 8-LBS:
-
8-Level Balance Scale
- CBM:
-
Community Balance and Mobility Scale
- 60CST:
-
60sec Chair Stand Test
- IQR:
-
Interquartile Range
- BMI:
-
Body Mass Index
References
Merom D, Stanaway F, Gebel K, Sweeting J, Tiedemann A, Mumu S, et al. Supporting active ageing before retirement: a systematic review and meta-analysis of workplace physical activity interventions targeting older employees. BMJ Open. 2021;11(6): e045818.
Söderbacka T, Nyholm L, Fagerström L. Workplace interventions that support older employees’ health and work ability-a scoping review. BMC Health Serv Res. 2020;20:1–9.
Dvořáková Z. The aging workforce and early retirement. AGING. 2022.
National Academies of Sciences, Engineering, and Medicine; Commitee on Population; Commitee on Understanding the Aging Workforce and Employment at Older Ages. Understanding the aging workforce: Defining a research agenda. Becker T, Fiske ST, editors. Washington (DC): National Academies Press (US); 2022.
Sippli K, Schmalzried P, Rieger MA, Voelter-Mahlknecht S. Challenges arising for older workers from participating in a workplace intervention addressing work ability: a qualitative study from Germany. Int Arch Occup Environ Health. 2021;94(5):919–33.
Ilmarinen J, Rantanen J. Promotion of work ability during ageing. Am J Ind Med. 1999;Suppl 1:21–3.
Ostchega Y, Dillon CF, Lindle R, Carroll M, Hurley BF. Isokinetic leg muscle strength in older americans and its relationship to a standardized walk test: data from the national health and nutrition examination survey 1999–2000. J Am Geriatr Soc. 2004;52(6):977–82.
Fujiyama H, Hinder MR, Schmidt MW, Garry MI, Summers JJ. Age-related differences in corticospinal excitability and inhibition during coordination of upper and lower limbs. Neurobiol Aging. 2012;33(7):1484 e1-14.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59.
Kenny GP, Yardley JE, Martineau L, Jay O. Physical work capacity in older adults: Implications for the aging worker. Am J Ind Med. 2008;51(8):610–25.
Marques NR, Hallal CZ, Spinoso DH, Crozara LF, Morcelli MH, Karuka AH, et al. Age-related alterations in the activation of trunk and lower limb muscles during walking. J Back Musculoskelet Rehabil. 2016;29(2):295–300.
Milanović Z, Pantelić S, Trajković N, Sporiš G, Kostić R, James N. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging. 2013:8:549–56.
Shur N, Creedon L, Skirrow S, Atherton P, MacDonald I, Lund J, et al. Age-related changes in muscle architecture and metabolism in humans: The likely contribution of physical inactivity to age-related functional decline. Ageing Res Rev. 2021;68: 101344.
Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006;61(10):1059–64.
Ihalainen JK, Inglis A, Makinen T, Newton RU, Kainulainen H, Kyrolainen H, et al. Strength Training Improves Metabolic Health Markers in Older Individual Regardless of Training Frequency. Front Physiol. 2019;10:32.
Granacher U, Gollhofer A, Hortobagyi T, Kressig RW, Muehlbauer T. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: a systematic review. Sports Med. 2013;43(7):627–41.
Bauman A, Merom D, Bull FC, Buchner DM, Singh MAF. Updating the Evidence for Physical Activity: Summative Reviews of the Epidemiological Evidence, Prevalence, and Interventions to Promote “Active Aging.” Gerontologist. 2016;56:S268–80.
Brustio PR, Magistro D, Ivaldi S, Caglio MM, Rabaglietti E, Liubicich ME. Neuromotor training in older women living in long-term care setting: a pilot study. Geriatr Nurs. 2015;36(5):361–6.
Boulton E, Hawley-Hague H, French DP, Mellone S, Zacchi A, Clemson L, et al. Implementing behaviour change theory and techniques to increase physical activity and prevent functional decline among adults aged 61–70: The PreventIT project. Prog Cardiovasc Dis. 2019;62(2):147–56.
Finger JD, Mensink G, Lange C, Manz K. Gesundheitsfördernde körperliche Aktivität in der Freizeit bei Erwachsenen in Deutschland. J Health Monit. 2017;2:37–44.
Granacher U, Wick C, Rueck N, Esposito C, Roth R, Zahner L. Promoting balance and strength in the middle-aged workforce. Int J Sports Med. 2010;32(1):35–44.
Weber M, Belala N, Clemson L, Boulton E, Hawley-Hague H, Becker C, et al. Feasibility and Effectiveness of Intervention Programmes Integrating Functional Exercise into Daily Life of Older Adults: A Systematic Review. Gerontology. 2018;64(2):172–87.
Clemson L, Fiatarone Singh MA, Bundy A, Cumming RG, Manollaras K, O’Loughlin P, et al. Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): randomised parallel trial. BMJ. 2012;345: e4547.
Schwenk M, Bergquist R, Boulton E, Van Ancum JM, Nerz C, Weber M, et al. The Adapted Lifestyle-Integrated Functional Exercise Program for Preventing Functional Decline in Young Seniors: Development and Initial Evaluation. Gerontology. 2019;65(4):362–74.
Hezel N, Körbi C, Wolf M, Adams M, Jansen C-P, Labudek S, et al. The Lifestyle-integrated Functional Exercise (LiFE) program and its modifications: a narrative review. German Journal of Exercise and Sport Research. 2021;51(4):416–29.
Mikolaizak AS, Taraldsen K, Boulton E, Gordt K, Maier AB, Mellone S, et al. Impact of adherence to a lifestyle-integrated programme on physical function and behavioural complexity in young older adults at risk of functional decline: a multicentre RCT secondary analysis. Bmj Open. 2022;12(10).
Taraldsen K, Mikolaizak AS, Maier AB, Mellone S, Boulton E, Aminian K, et al. Digital Technology to Deliver a Lifestyle-Integrated Exercise Intervention in Young Seniors-The PreventIT Feasibility Randomized Controlled Trial. Front Digit Health. 2020;2:10.
Zhang W, Schwenk M, Mellone S, Paraschiv-Ionescu A, Vereijken B, Pijnappels M, et al. Complexity of Daily Physical Activity Is More Sensitive Than Conventional Metrics to Assess Functional Change in Younger Older Adults. Sensors. 2018;18(7):20–32.
Schaller A, Stassen G, Baulig L, Lange M. Physical activity interventions in workplace health promotion: objectives, related outcomes, and consideration of the setting-a scoping review of reviews. Front Public Health. 2024;12:1353119.
Holtermann A, Straker L, Lee IM, Stamatakis E, van der Beek AJ. Workplace physical activity promotion: why so many failures and few successes? The need for new thinking. Br J Sports Med. 2021;55(12):650–1.
Escoffery C, Lebow-Skelley E, Udelson H, Boing EA, Wood R, Fernandez ME, et al. A scoping study of frameworks for adapting public health evidence-based interventions. Transl Behav Med. 2019;9(1):1–10.
Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta-analysis of workplace physical activity interventions. Am J Prev Med. 2009;37(4):330–9.
Dugdill L, Brettle A, Hulme C, McCluskey S, Long A. Workplace physical activity interventions: a systematic review. Int J Workplace Health Manag. 2008;1(1):20–40.
Hamilton K, Fraser E, Hannan T. Habit-based workplace physical activity intervention: a pilot study. Occup Med. 2019;69(7):471–4.
Gollwitzer PM. Implementation intentions: strong effects of simple plans. Am Psychol. 1999;54(7):493.
Teixeira PJ, Carraça EV, Markland D, Silva MN, Ryan RM. Exercise, physical activity, and self-determination theory: a systematic review. Int J Behav Nutr Phys Act. 2012;9:1–30.
Kramer F, Labudek S, Jansen CP, Nerz C, Fleig L, Clemson L, et al. Development of a conceptual framework for a group-based format of the Lifestyle-integrated Functional Exercise (gLiFE) programme and its initial feasibility testing. Pilot Feasibility Stud. 2020;6:6.
Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28-34.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Gordt K, Mikolaizak AS, Taraldsen K, Bergquist R, Van Ancum JM, Nerz C, et al. Creating and validating a shortened version of the community balance and mobility scale for application in people who are 61 to 70 years of age. Phys Ther. 2020;100(1):180–91.
McDonald O, Perraton L, Osadnik C. Validity and clinical applicability of the 60-second sit-to-stand test in people with acute exacerbations of COPD. Respir Med. 2023:107264.
Giurgiu M, Bussmann JB, Hill H, Anedda B, Kronenwett M, Koch ED, et al. Validating accelerometers for the assessment of body position and sedentary behavior. Journal for the Measurement of Physical Behaviour. 2020;3(3):253–63.
Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2.
Zbarsky K, Parsley D, Clegg H. Community Balance & Mobility Scale (CB&M): age-related reference values. Physiother Canada. 2010;62(suppl): e8.
Harvey JA, Chastin SF, Skelton DA. How sedentary are older people? A systematic review of the amount of sedentary behavior. J Aging Phys Act. 2015;23(3):471–87.
Tudor-Locke C, Schuna JM Jr, Barreira TV, Mire EF, Broyles ST, Katzmarzyk PT, et al. Normative steps/day values for older adults: NHANES 2005–2006. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2013;68(11):1426–32.
Genin PM, Dessenne P, Finaud J, Pereira B, Dutheil F, Thivel D, et al. Effect of Work-Related Sedentary Time on Overall Health Profile in Active vs. Inactive Office Workers. Front Public Health. 2018;6:279.
Hulls PM, Richmond RC, Martin RM, Chavez-Ugalde Y, de Vocht F. Workplace interventions that aim to improve employee health and well-being in male-dominated industries: a systematic review. Occup Environ Med. 2022;79(2):77–87.
Mazzetti SA, Kraemer WJ, Volek JS, Duncan ND, Ratamess NA, Gomez A, et al. The influence of direct supervision of resistance training on strength performance. Med Sci Sports Exerc. 2000;32(6):1175–84.
McClaran SR. The effectiveness of personal training on changing attitudes towards physical activity. J Sports Sci Med. 2003;2(1):10.
Burton E, Lewin G, Clemson L, Boldy D. Effectiveness of a lifestyle exercise program for older people receiving a restorative home care service: a pragmatic randomized controlled trial. Clin Interv Aging. 2013;8:1591–601.
Schoenfeld BJ, Ogborn D, Krieger JW. Effects of resistance training frequency on measures of muscle hypertrophy: a systematic review and meta-analysis. Sports Med. 2016;46(11):1689–97.
Suchomel TJ, Nimphius S, Bellon CR, Stone MH. The importance of muscular strength: training considerations. Sports Med. 2018;48:765–85.
Søgaard K, Sjøgaard G. Physical activity as cause and cure of muscular pain: evidence of underlying mechanisms. Exerc Sport Sci Rev. 2017;45(3):136.
Liu Cj, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane database of systematic reviews. 2009(3).
Miles M, Clarkson P. Exercise-induced muscle pain, soreness, and cramps. J Sports Med Phys Fitness. 1994;34(3):203–16.
van As S, Veling H, Beckers DG, Earle F, McMaster S, Kompier MA, et al. The impact of cognitive work demands on subsequent physical activity behavior. J Exp Psychol Appl. 2022;28(3):629.
Rubichi S, Pellicano A. Does the Simon effect affect movement execution? Eur J Cogn Psychol. 2004;16(6):825–40.
Rassia ST, Hay S, Beresford A, Baker NV, editors. Movement dynamics in office environments. In: 3rd CIB International Conference on Smart and Sustainable Built Environments, Delft, Netherlands, 2009. Proceedings of SASBE 2009.
Bredahl TVG, Særvoll CA, Kirkelund L, Sjøgaard G, Andersen LL. When intervention meets organisation, a qualitative study of motivation and barriers to physical exercise at the workplace. Sci World J. 2015;1:518–61.
Lawton R, Mceachan R, Jackson C, West R, Conner M. Intervention fidelity and effectiveness of a UK worksite physical activity intervention funded by the Bupa Foundation. UK Health promotion international. 2014;30(1):38–49.
Reicherzer L, Kramer-Gmeiner F, Labudek S, Jansen C-P, Nerz C, Nystrand MJ, et al. Group or individual lifestyle-integrated functional exercise (LiFE)? A qualitative analysis of acceptability. BMC Geriatr. 2021;21:1–12.
Jansen CP, Nerz C, Labudek S, Gottschalk S, Kramer-Gmeiner F, Klenk J, et al. Lifestyle-integrated functional exercise to prevent falls and promote physical activity: Results from the LiFE-is-LiFE randomized non-inferiority trial. Int J Behav Nutr Phys Act. 2021;18(1):115.
Del Vecchio A, Casolo A, Negro F, Scorcelletti M, Bazzucchi I, Enoka R, et al. The increase in muscle force after 4 weeks of strength training is mediated by adaptations in motor unit recruitment and rate coding. J Physiol. 2019;597(7):1873–87.
Pedersen MT, Vorup J, Nistrup A, Wikman JM, Alstrøm JM, Melcher P, et al. Effect of team sports and resistance training on physical function, quality of life, and motivation in older adults. Scand J Med Sci Sports. 2017;27(8):852–64.
Copeland JL, Ashe MC, Biddle SJ, Brown WJ, Buman MP, Chastin S, et al. Sedentary time in older adults: a critical review of measurement, associations with health, and interventions. Brit J Sport Med. 2017;51(21):1539.
Kraemer WJ, Fragala MS. Personalize it: program design in resistance training. ACSM’s Health & Fitness Journal. 2006;10(4):7–17.
Fyfe JJ, Hamilton DL, Daly RM. Minimal-dose resistance training for improving muscle mass, strength, and function: A narrative review of current evidence and practical considerations. Sports Med. 2022;52(3):463–79.
Reicherzer L, Kramer-Gmeiner F, Labudek S, Jansen CP, Nerz C, Nystrand MJ, et al. Group or individual lifestyle-integrated functional exercise (LiFE)? A qualitative analysis of acceptability. BMC Geriatr. 2021;21(1):93.
Taraldsen K, Mikolaizak AS, Maier AB, Mellone S, Boulton E, Aminian K, et al. Digital technology to deliver a lifestyle-integrated exercise intervention in young seniors—the preventIT feasibility randomized controlled trial. Frontiers in Digital Health. 2020;2: 563688.
Eichhorn D, Ott I. Nudging im Unternehmen: den Weg für gesunde Entscheidungen bereiten: Institut für Arbeit und Gesundheit der Deutschen Gesetzlichen Unfallversicherung (IAG); 2019.
Fishbach A, Hofmann W. Nudging self-control: A smartphone intervention of temptation anticipation and goal resolution improves everyday goal progress. Motivation Science. 2015;1(3):137.
Ledderer L, Kjær M, Madsen EK, Busch J, Fage-Butler A. Nudging in Public Health Lifestyle Interventions: A Systematic Literature Review and Metasynthesis. Health Educ Behav. 2020;47(5):749–64.
Lindelöf N, Karlsson S, Lundman B. Experiences of a high-intensity functional exercise programme among older people dependent in activities of daily living. Physiother Theory Pract. 2012;28(4):307–16.
Allam A, Kostova Z, Nakamoto K, Schulz PJ. The effect of social support features and gamification on a Web-based intervention for rheumatoid arthritis patients: randomized controlled trial. J Med Internet Res. 2015;17(1): e3510.
Hamari J, Koivisto J. “Working out for likes”: An empirical study on social influence in exercise gamification. Comput Hum Behav. 2015;50:333–47.
da Silva NC, Ricci F, de Castro VR, Lima ACR, do Carmo Lopes ER, de Salvo Mauad LD, et al. Effects of workplace upper extremity resistance exercises on function and symptoms of workers at a tertiary hospital: a randomized controlled trial protocol. BMC Musculoskelet Disord. 2022;23(1):119.
Joyce K, Pabayo R, Critchley JA, Bambra C. Flexible working conditions and their effects on employee health and wellbeing. Cochrane Database Syst Rev. 2010;17(2):1–88.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the AFF Young Scholar Fund of the University of Konstanz. The content of this paper is solely the responsibility of the authors.
Author information
Authors and Affiliations
Contributions
YR developed the concept and design, was responsible for study management, statistical analysis, interpretation of data, and prepared the manuscript. DP was involved in study management and data acquisition. MS was responsible for funding acquisition, development of concept and design, interpretation of data and preparation of manuscript. All authors contributed to interpretation of data, drafting the article, and final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Participants provided written informed consent. The study protocol was approved by the ethics committee of the University of Konstanz.
Consent for publication
All the patients who provided their case reports provided consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
11556_2024_356_MOESM1_ESM.docx
Supplementary Material 1: Supplementary File 1. Short description of the participant manual. The participant manual is currently available in German and serves as a guide for participants during the program. It is handed out to participants at the first training session. It explains the scope of the wLiFE55+ program and offers strategies for seamless integration into everyday working life. The first section of the manual focuses on the key aspects of the program, particularly the concepts of habit formation and activity integration. As the wLiFE55+ program aims for long-term implementation, the importance of setting personal goals is also clear. In the following chapters "Neuromotor Function","Strength" and "Physical Activity", the importance of these components for the health of the target group is discussed, and the effect of targeted activities is illustrated. The principles of wLiFE55+ are presented and the individual activities (neuromotor function: e.g., tandem stand, strength: e.g., squat, physical activity: e.g., interrupting sitting phases) are described and illustrated in detail. The participant manual is designed to help participants organize their training independently. Each chapter therefore offers strategies for recognizing situations, selecting suitable activities, and adjusting the intensity accordingly. For example, the chapter on balance shows how participants can optimize their balance training by making small adjustments (e.g., reducing the support surface). Supplementary File 2. Checklist personal trainer session for teaching the wLiFE55+ program to the study participants during 4 personal trainer sessions at the workplace. Supplementary File 3. Daily Routine chart. Supplementary File 4. wLiFE55+ assessment tool (version March 2022; adapted version of the aLAT [24]). Supplementary File 5. Activity Planner. Supplementary File 6. The extension process from the Short Physical Performance Battery (SPPB) to the 8-Level-Balance-Scale (8-LBS) to the 12-Level-Balance-Scale (12-LBS) to assess static balance for older employees. The SPPB includes three balance performance items (Romberg stand, semi-tandem stand, tandem stand; each with eyes open for 10 sec) with a maximum score of 4 points. The 8-LBS is an extension of the SPPB [23]. The 8-LBS performed in previous standing positions (Romberg stand, semi-tandem stand and tandem stand) for a longer time (30 sec instead of 10 sec) and with two different conditions (eyes open, eyes closed). In addition, a fourth standing position (one-leg stand on the preferred leg) is used. This is performed with eyes open, eyes closed, and eyes closed with an additional cognitive distractor. The 8-LBS has a maximum score of 8 points. The 12-LBS is an extension of the 8-LBS. The one-leg stand on the nonpreferred leg was added and performed with all three conditions (eyes open, eyes closed, eyes closed with an additional cognitive distractor). The 12-LBS has a maximum score of 12 points. This extension process was performed to avoid ceiling effects, as older employees show a better static balance than do retired seniors. Supplementary File 7. Descriptive data for working situation items (n=17).Notes. Self-developed questionnaire with items regarding working situation-related data. The questionnaire data for two participants were missing. Supplementary File 8. Exploratory pre-post measures for objective assessment of low function participants. Notes. The data are presented as the medians and interquartile range (IQR). 12-LBS= 12-Level Balance Scale; CBM=Community balance and mobility scale; 60CST= 60sec Chair Stand Test. Supplementary File 9. Exploratory pre-post measures for objective assessment
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ritter, Y., Pfister, D., Steckhan, G.M. et al. The work Lifestyle-integrated Functional Exercise program for preventing functional decline in employees aged 55 years and older: development and initial evaluation. Eur Rev Aging Phys Act 21, 21 (2024). https://doi.org/10.1186/s11556-024-00356-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-024-00356-5