Abstract
Background
This study aimed to describe the efficacy of hysteroscopy in the management of women with the persistent gestational trophoblastic disease (PGTD)/GTN to reduce the need for chemotherapy.
Materials and methods
This prospective, single-arm, clinical trial study was recruited in an educational referral hospital between September 2018 and September 2019. Totally, 30 participants with a history of hydatidiform mole that was managed by uterine evacuation and developed low risk persistent gestational trophoblastic disease were recruited. Hysteroscopy was performed for removal of persisted trophoblastic tissue. Serum beta-hCG titer was measured before and 7 days after the procedure.
Results
The mean ± SD age of the participants was 31.4 ± 4.6 years. There was a significant difference (p = 0.06) between that mean ± SD of beta-hCG titer before (8168.4 ± 1758) and after (2648.8 ± 5888) hysteroscopy. Only two (6.6%) cases underwent chemotherapy due to no drop in the beta-hCG titer.
Conclusion
Hysteroscopy may play a significant role in the management of GTN, although it requires validation in larger prospective randomized studies and longer follow-up.
Similar content being viewed by others
Introduction
Hydatidiform mole [1] also known as molar pregnancy occurs by placental pathology of androgenetic origin [2]. This phenomenon happens with abnormal hyperproliferation of the placental villi and hydropic degeneration [3]. HM belongs to the gestational trophoblastic diseases (GTD) as the most common pathologies and could locally invade the uterus with potential metastasis [2]. HM is a premalignant condition and categorized as complete and partial either. Malignant disease is referred to as gestational trophoblastic neoplasia (GTN) [4].
The incidence of HM varies from 66 to 121 per 100,000 pregnancies in North America, and Europe whereas Asia, Latin America, and the Middle East report a higher rate (23 to 1299 per 100,000 pregnancies) [5]. Two well-known risk factors of HM are maternal age and previous hydatidiform mole [6] as the chance of repeating is 10-20 folds more than the general population [7].
The common features are vaginal bleeding, uterine enlargement, pelvic pain, hyperemesis as well as hyperthyroidism, pregnancy-induced hypertension, and ovarian theca lutein cyst as less or late features [8]. History taking, physical examination, beta-hCG titer, chest radiograph, and ultrasound findings are routine diagnostic evaluation [9]. Treatment involves evacuating the uterus by uterine suction or surgical curettage [10].
Fifteen percent of complete hydatidiform moles will progress to a malignant transformation that is called gestational trophoblastic neoplasia (GTN) and consequently, need further treatment based on the stage of the disease or risk group. A persistent positive beta-hCG titer helps us to detect the development of GTN in the follow-up period [11]. The standard types of treatment available in GTN are surgery, chemotherapy, and radiation therapy. New methods of treatment are being tested as clinical trials to find better options and lower the potential complications of chemoradiotherapy. Second curettage was accepted as an alternative to chemotherapy for non-metastatic and low-grade GTN for patients who have intrauterine disease, although, it might not reduce the need for chemotherapy in persisted cases [12] and may develop intrauterine adhesions which cause infertility [1].
Hysteroscopy resection under the direct vision was suggested for removing the residual of trophoblastic tissue with fewer complications than curettage [1]. This study aimed to assess whether hysteroscopy in GTN could reduce the need for further chemotherapy.
Materials and methods
Study overview
This prospective, single-arm, clinical trial study was carried out in an educational referral hospital affiliated to Tehran University of Medical Sciences between September 2018 and September 2019. All participants with a history of hydatidiform mole were recruited. Lab data such as renal, liver and thyroid function test, complete blood count (CBC), and electrolytes was obtained. Indeed, beta-hCG titer was measured as a baseline.
An abdominopelvic ultrasound was performed to find any evidence of invasive mole, exclude a coexisting pregnancy, and look for possible metastatic disease. Chest radiography was ordered for all patients.
In the participants who desired to preserve fertility, uterine evacuation was performed. After dilatation, the molar tissue was evacuated with suction cannula 9 gauge and the clinician was performed a sharp curettage by curette at the end of the procedure.
In the follow-up period, patients were visited every week and the beta-hCG was measured by cobas analyzer for free beta subunit by ECL (Electrochemiluminescence). The standard created by International Federation of Gynecologists and Obstetricians (FIGO) for GTN diagnosis are as follow [13]:
-
1-
Beta- hCG plateau four values ± 10% recorded over a 3-week duration.
-
2-
Elevated beta-hCG level more than 10% of three values recorded over a 2-week duration.
-
3-
Detectable beta-hCG for more than 6 months after evacuation.
In the case of GTN, after staging by FIGO [14], hysteroscopy was performed by a surgeon with 15-year experience in the field of hysteroscopy, with 26 F KARL STORZ bipolar resectoscope fitted with an 8-mm cutting loop. Saline was used to distend the uterine cavity by controlling the amount of fluid (by means of Hysteroflator). We set the pomp on the least pressure that was 150 mmHg to minimize the cell spread via the fallopian tube. As in GTN, the uterus is similar to pregnancy; it is very prone to be traumatized with any manipulation. By using the loop without current as the curettage, all trophoblastic tissues were removed by gentle motions with minimal trauma application. Indeed, no misoprostol or prostaglandins were used for cervical preparing. Seven days after the procedure, beta-hCG was evaluated again.
Primary outcome was the evaluation of the change in serum beta-hCG levels after 1 and 7 days (a 10 log reduction regarding the primary levels). Secondary outcome was assessing the endometrial cavity for any remaining tissue 7 days after the procedure by transvaginal ultrasound (TVS) (Siemens probe, by a same radiologist who performed the first TVS). If beta-hCG had a plateaued or non-decreasing trend (<a 10 log reduction), the patients were candidate for chemotherapy. All the participants followed by measuring beta-hCG levels for 6 months until the levels would be undetectable.
Ethical statements
All participants sign the written informed consent. The oncologist explained the potential pros and cons of hysteroscopic resection and the advantages and disadvantages of chemotherapy as an alternative treatment. The study had been approved by TUMS ethics committee (Reference Number: 27546-30-03-94). It was registered in Iranian Registry of Clinical Trials (IRCT), (Reference Number: IRCT201601222576N11, 8/2016). This trial was conducted according to the principles of the Helsinki Declaration.
Inclusion and exclusion criteria
Inclusion criteria were the history of hydatidiform mole that beta-hCG titer in the follow-up did not reach negative value after uterine evacuation or the detecting molar tissue in the uterus by ultrasound. They were all eager to participate in the study. Exclusion criteria were patients who preferred chemotherapy instead of hysteroscopy or had unstable vital signs.
Statistical analysis
Data analysis was conducted by means of STATA version 14. (StataCorp, College Station, TX, USA). The Mann-Whitney U test was used for data analysis. P value less than 0.05 was considered significant. A CONSORT guideline was used for reporting the results.
Results
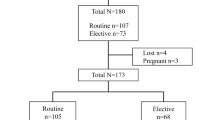
Totally, 287 participants with confirmed pathology of molar pregnancy underwent uterine evacuation. In the follow-up, 41 (14.2%) cases of GTN were enrolled (Fig. 1). After a complete evaluation and a consultation by an oncologist, 7 women withdrew from the study and prefer to receive conventional chemotherapy. All participants who assessed using FIGO criteria for GTN staging were non-metastatic (stage 1) and also all cases were low risk GTN using prognostic scoring and anatomic staging systems of FIGO [15]. In 30 patients, the mean ± SD age was 31.4 ± 4.6 years. The mean ± SD of baseline and discharge beta-hCG was 8168.4 ± 1758 and 2648.8 ± 5888 (p = 0.06) respectively.
In ultrasound evaluation 7 days after the hysteroscopy, no persistent tissue in the uterus was reported in the cases. In the follow-up, two patients received chemotherapy after hysteroscopy due to increased beta-hCG titer.
The age, gravidity, baseline, and discharge beta-hCG titer of two groups (who need chemotherapy or not) is listed in Table 1.
No adverse events during the hysteroscopy such as uterine perforation, volume overload, hemorrhage, or pulmonary emboli happened. In 6 months follow-up after the procedure, all 28 patients were checked routinely and none of them required salvage chemotherapy during this period.
Discussion
Due to the possible side effects of chemotherapy in women in the fertility age, new treatment modalities have been suggested to manage GTN. We assess the role of hysteroscopic resection without electrical current for GTN management. The results of this study showed that hysteroscopic resection could treat 93.3% of the patients and only 2 cases (6.6%) needed further chemotherapy. This method was performed in a study by Rein et al. in 95 patients with non-molar retained products of conception who underwent hysteroscopy or D&C [1].
The standard treatment for HM is uterine evacuation, but the repeated procedure in the cases of persistent tissue may be associated with complications such as uterine perforation and synechiae [16]; however, in the present study due to direct visualization of uterine cavity and border of the trophoblastic tissues, there was no perforation or Asherman syndrome after 6 months follow-up.
On the other hand, the uterus in GTD is prone to be traumatized by any manipulation. We used an electro loop to be easily handled to catch the remaining tissue without electro current to minimize the trauma.
Faivre et al. also reported a lower rate of adhesion after hysteroscopic resection of residual trophoblastic tissues. They used hysteroscopy for removing residual trophoblastic tissue in 50 patients and reported 100% complete evacuation of the uterus with minimal complication [17].
In another study, patients with low-risk gestational trophoblastic neoplasia underwent repeat uterine evacuation and revealed that 83% did not require further chemotherapy [18]. Indeed, second curettage for low risk non metastatic GTN was performed in 64 patients and reported 40% cure after second curettage. They also observed surgical failure in 59% [19]. In contrast, in the present study, no complication was reported.
In the other study by Pezeshki et al., 544 patients underwent second uterine evacuation for low risk GTN, while 67% cured but third evacuation was performed in 28 patients and at last, 27% of cases needed chemotherapy [20].
This study had some limitations. First, the study had selection bias because it is a single-arm study. Due to the ethical concern, we could not include a control group with second curettage because it was assumed that D&C may increase risk of perforation or adhesion or incomplete evacuation due to the blind nature of D&C. Second, the sample size was limited. So, larger multicentric, randomized studies with follow-up protocol and control group (may be D&C or chemotherapy group) is crucial. The strengths of the study were the novelty in using resection without electrical current and the 6-month follow-up period.
Conclusion
Hysteroscopy with non-electrical current may be a safe method to manage GTN to minimize the need for chemotherapy in the selected patients.
Availability of data and materials
All data analyzed during this study are included in this published article as a supplementary file.
Abbreviations
- GTN:
-
Gestational trophoblastic neoplasia
- PGTD:
-
Persistent gestational trophoblastic disease
- D&C:
-
Dilatation & curettage
- HM:
-
Hydatidiform mole
- GTN:
-
Gestational trophoblastic neoplasia
- SD:
-
Standard deviation
- CBC:
-
Complete blood count CT: computed tomography
- MRI:
-
Magnetic resonance imaging
- ECL:
-
Electrochemiluminescence
- IRCT:
-
Iranian Registry of Clinical Trials
- TVS:
-
Transvaginal sonography
- FIGO:
-
International Federation of Gynecologists and Obstetricians
References
Rein DT, Schmidt T, Hess AP, Volkmer A, Schondorf T, Breidenbach M (2011) Hysteroscopic management of residual trophoblastic tissue is superior to ultrasound-guided curettage. J Minim Invasive Gynecol 18(6):774–778
Candelier JJ (2016) The hydatidiform mole. Cell Adhes Migr 10(1-2):226–235
Candelier JJ (2015) Complete hydatidiform mole. Med Sci 31(10):861–868
Vassilakos P, Riotton G, Kajii T (1977) Hydatidiform mole: two entities. A morphologic and cytogenetic study with some clinical consideration. Am J Obstet Gynecol 127(2):167–170
Altieri A, Franceschi S, Ferlay J, Smith J, La Vecchia C (2003) Epidemiology and aetiology of gestational trophoblastic diseases. Lancet Oncol 4(11):670–678
Lurain JR (2010) Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol 203(6):531–539
Sand PK, Lurain JR, Brewer JI (1984) Repeat gestational trophoblastic disease. Obstet Gynecol 63(2):140–144
Akinlaja O, McKendrick R, Mashak Z, Nokkaew M (2016) Incidental finding of persistent hydatidiform mole in an adolescent on Depo-Provera. Case Rep Obstet Gynecol 2016:6075049
Sasaki S (2003) Clinical presentation and management of molar pregnancy. Best Pract Res Clin Obstet Gynaecol 17(6):885–892
Padron L, Rezende Filho J, Amim Junior J, Sun SY, Charry RC, Maesta I et al (2018) Manual compared with electric vacuum aspiration for treatment of molar pregnancy. Obstet Gynecol 131(4):652–659
Wolfberg AJ, Berkowitz RS, Goldstein DP, Feltmate C, Lieberman E (2005) Postevacuation hCG levels and risk of gestational trophoblastic neoplasia in women with complete molar pregnancy. Obstet Gynecol 106(3):548–552
Lima LLA, Padron L, Camara R, Sun SY, Rezende JF, Braga A (2017) The role of surgery in the management of women with gestational trophoblastic disease. Rev Col Bras Cir 44(1):94–101
Kohorn EI (2001) The new FIGO 2000 staging and risk factor scoring system for gestational trophoblastic disease: description and critical assessment. Int J Gynecol Cancer 11(1):73–77
Kohorn EI (2002) Negotiating a staging and risk factor scoring system for gestational trophoblastic neoplasia. A progress report. J Reprod Med 47(6):445–450
Ngan HY, Bender H, Benedet JL, Jones H, Montruccoli GC, Pecorelli S et al (2003) Gestational trophoblastic neoplasia, FIGO 2000 staging and classification. Int J Gynaecol Obstet 83(Suppl 1):175–177
Thomson AJA, Jason AB, Deans R, Kingston A, Vancaillie TGB (2009) The management of intrauterine synechiae. Curr Opin Obstet Gynecol 21(4):335–341
Faivre E, Deffieux X, Mrazguia C et al (2009) Hysteroscopic management of residual trophoblastic tissue and reproductive outcome: a pilot stu. J Minim Invasive Gynecol 16(4):487–490
Yarandi F, Jafari F, Shojaei H, Izadi-Mood N (2014) Clinical response to a second uterine curettage in patientswith low-risk gestational trophoblastic disease: a pilot study. J Reprod Med 59(11-12):566–570
Osborne RJFV, Schink JC et al (2016) Second Curettage for Low-Risk Nonmetastatic Gestational Trophoblastic Neoplasia. Obstet Gynecol 128(3):535–542
Pezeshki MHB, Silcocks P, Everard JE, Coleman J, Gillespie AM, Tidy J, Coleman RE (2004) The role of repeat uterine evacuation in the management of persistent gestational trophoblastic disease. Gynecol Oncol 95(3):423–429
Acknowledgements
The authors would like to thanks the staff of perinatology clinic of Woman Hospital for their support and help our patients to fill the questionnaires.
Funding
There is no funding for this study.
Author information
Authors and Affiliations
Contributions
F.D.T: Project development. S.S.S: Project development. F.Y: Project development. E.S: Data collection. M.F: Data collection. Z.S: Data collection. M (Mahsa).G: Manuscript writing. M (Marjan).G: Data management, manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the participants in the study were asked to fill informed consent for participation in the study .The study was approved by the ethical committee of Tehran University of Medical Sciences.
Consent for publication
All the participants were informed about publication of data anonymously, and they signed the informed consent.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tanha, F.D., Sede, S.S., Yarandi, F. et al. Does hysteroscopy in women with persistent gestational trophoblastic disease reduce the need for chemotherapy? A prospective, single-arm, clinical trial pilot study. Gynecol Surg 18, 12 (2021). https://doi.org/10.1186/s10397-021-01094-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10397-021-01094-7