Abstract
Background
Vulvar cancer is a rare gynecological malignancy that primarily affects women of postmenopausal age. Treatment is mainly surgical, particularly for vulvar squamous cell carcinoma, the most prevalent histotype. In patients with unifocal tumors with a maximum diameter of <4 cm, in the absence of suspected inguinal lymph nodes, sentinel lymph node (SLN) biopsy is recommended. The use of a radioactive tracer is mandatory; the use of the vital blue dye is optional.
Results
Two patients diagnosed with vulvar squamous cell carcinoma (FIGO IB stage) underwent bilateral radical vulvectomy, SLN search and removal, and bilateral inguinal lymphadenectomy at the Cannizzaro Hospital Operative Unit of Obstetrics and Gynecology Department (Catania, Italy). Three milliliters of indocyanine green (ICG) 0.5 mg/mL was administered in 3 peritumoral injections under general anesthesia to screen the SLN. The images were acquired using an intraoperative infrared camera system, which allowed intraoperative visualization of the SLN. An SLN was identified for each patient. The lymph nodes examined by the pathologist were negative for metastatic localization of the disease. However, patients underwent bilateral inguinofemoral lymphadenectomy, as this procedure is not currently codified as a gold standard for the detection of SLN in vulvar cancer. All the lymph nodes removed were negative for the localization of vulvar carcinoma metastases.
Conclusions
The potential of the administration of indocyanine green (ICG) allows the execution of SLN biopsy, avoiding the multiple administrations of radiocolloid in the pre-operative phase, painful for the patient, elimination, and exposure to radioactivity. Therefore, while requiring standardization of the methodology and a large-scale application, this procedure could open a new surgical management perspective in patients with early-stage vulvar cancer.
Similar content being viewed by others
Introduction
Vulvar cancer accounts for approximately 3–5% of all gynecological neoplasms, with an annual incidence of 1–2 in 100,000 women, [1]. In recent decades, vulvar cancer incidence has risen by 4.6% every 5 years. Every year, about 6190 new cases are expected [2, 3]. Historically, the incidence peak has been around 70 years of age. However, the incidence of vulvar squamous cell carcinoma (vSCC) has been shown to have affected younger women in recent years [4, 5].
vSCC has a combined clinical, surgical, and pathological staging system based on American Joint Committee on Cancer and the International Federation of Gynecology and Obstetrics (FIGO), 2009 [6]. Lymph node involvement is the most relevant prognostic predictor. Radical vulvectomy with bilateral inguinofemoral lymphadenectomy is defined as the gold standard for treating patients with vulvar squamous cell carcinoma (vSCC).
However, up to two thirds of vulvar squamous cell carcinoma (vSCC) patients who underwent inguinofemoral lymphadenectomy subsequently experience lymphedema [7,8,9]. Given that <30% of patients with FIGO stage I or II vulvar cancer have positive lymph nodes, lymphadenectomy is not ideal for most patients [10,11,12]. It was preferred to replace the demolitive surgical approach with wide excision of the vulvar lesion and sentinel lymph node biopsy. The abovementioned procedure, which is more conservative, has an efficacy comparable to the previous one but reduced morbidity in the early stage cases [13, 14]. For the research and identification of the sentinel lymph node, the gold standard uses a combination of radioccolloids and blue dye. However, the radioactive tracers cannot provide real-time visual guidance, and the blue dye cannot be seen through the skin. Recently, there has been a growing interest in using the fluorescent dye, indocyanine green (ICG). It is a tricarbocyanine dye, which fluoresces in the near-infrared spectrum when illuminated with 806-nm light. The fluorescent light is then captured through a video camera that allows viewing of the indocyanine green (ICG) in the spectrum of visible light. Besides, indocyanine green (ICG), being soluble in water and binding to albumin, is particularly suitable for mapping the lymphatic tracts and lymph nodes [15]. Therefore, the indocyanine green (ICG) can be used for sentinel lymph node detection in open, laparoscopic, or robotic surgery. In oncological gynecology, this method was applied for the first time in 2010 by Furukawa in cervical cancer using a portable video camera for open surgery (PDE; Hamamatsu Photonics, Hamamatsu, Japan) [16]. Subsequently, the search for sentinel lymph nodes with indocyanine green (ICG) has become the gold standard in the initial cases of endometrial and cervical cancer, mainly by laparoscopic and robotic methods. With the introduction of the SPY Portable Handheld Imager (SPY-PHI) © Stryker imaging system for open surgery and based on our clinical experience, we have evaluated the possibility of performing the SLN search procedure with indocyanine green (ICG) in early-stage vulvar cancer.
Our experience
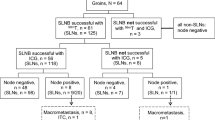
A total of 165 patients underwent surgery for a vulvar squamous cell carcinoma (vSCC) at the Cannizzaro Hospital Operative Unit of Obstetrics and Gynecology Department (Catania, Italy) between 2006 and 2019. From electronic databases and medical records, clinical and pathological characteristics (age, FIGO stage, tumor size, surgery, margin status, inguinal lymph node status, recurrence incidence, and follow-up) were collected. All cases were classified based on the 2009 FIGO staging (Table 1) [17].
Patients with tumors smaller than 2 cm and <1 mm of stromal invasion were treated only by local radical excision to achieve disease-free margins. Patients with midline lesions with >2 cm tumors were treated by radical vulvectomy and bilateral inguinofemoral lymphadenectomy with separate incisions. Patients with tumors located more than 1 cm from the midline were treated with ipsilateral inguinal lymphadenectomy, frozen section, and possible contralateral lymphadenectomy. Inguinal lymphadenectomy was not performed in patients with early-stage tumors (FIGO stage IA with stromal invasion <1 mm) and in very elderly patients (≥80 years) with multiple comorbidities [18].
Based on our experience and according to The European Society of Gynaecological Oncology (ESGO) guidelines, we decided to treat two patients with vulvar squamous cell carcinoma (vSCC), FIGO stage IB with radical vulvectomy, sentinel lymph node search, and removal with indocyanine green (ICG) subsequent bilateral inguinofemoral lymphadenectomy.
Characteristics of the patients
At the Gynecology and Obstetrics Department of the Cannizzaro Hospital (Catania, Italy), two patients diagnosed with vulvar squamous cell carcinoma (vSCC) were operated by administration of indocyanine green (ICG), which aided in exploration and removal of sentinel lymph nodes. Both patients have been diagnosed with FIGO IB stage vulvar neoplasm. The first patient, aged 85 years, menarche at the age of 13, physiological menopause, and a remote medical history characterized by arterial hypertension in medical therapy, consulted with us after the onset of vulvar itching and burning for about 2 years, which has intensified over the last 3 months. The patient was then subjected to a gynecological examination with evidence of a vulvar region transformed into a tumor, approximately 4 cm in diameter, with bilateral involvement of large and small lips. She was then subjected to vulvar biopsy, with histological results of “well-differentiated fragments of squamous verrucous carcinoma” on an outpatient basis. The second clinical case concerned a 71-year-old patient with a past medical history marked by arterial hypertension and type II diabetes mellitus under medical treatment. The patient came to our attention by finding a vulvar lesion of about 3 cm affecting the large and small right lip. She had undergone vulvar biopsy at another hospital, with histological results of “moderately differentiated, invasive squamous carcinoma fragments.” Both patients underwent a preoperative workup with clinical evaluation of the lesion and computed tomography (CT) scan of the complete abdomen and groin without signs of suspected lesions due to secondary heteroplastic processes.
Intraoperative imaging system
The SPY Portable Handheld Imager (SPY-PHI) © Stryker was used as the intraoperative imaging device. This device uses SPY fluorescence imaging technology to visually assess blood circulation in blood vessels and associated tissue perfusion during surgery. The design of SPY-PHI makes the device versatile, enabling the operator to frame the operating field and use the acquired images in real-time, integrating fluorescence signal data with white light images in real-time. The SPY Portable Handheld Imaging System Camera, with integrated optics and cables for real-time fluorescence imaging in visible light and near-infrared, is ideal for open surgery.
Intraoperative detection of the sentinel lymph node
The fluorescent agent was administered to patients placed in the lithotomy position under general anesthesia. Indocyanine green (ICG) prepared with a 25-mg vial of green indocyanine green (ICG) (Pulsion Medical Systems AG, Munich, Germany) diluted in 50 mL of water for injections (B. Braun Medical) was used, resulting in a concentration of 0.5 mg/mL. Injection of 1 ml per quadrant was administered in the three quadrants around the vulvar lesion (Fig. 1). After the injection, the infrared camera, equipped with a movable arm, was placed in front of the patient to detect transcutaneous fluorescence during surgery. Subsequently, the SLN was localized based on the fluorescence intensity. The intraoperative fluorescence detection camera system was used to open, identify, and remove the SLN and the vulvectomy of the groin. After the excision, the capture of the residual lymphatic pathway could be seen bilaterally through the infrared camera. Additionally, all SLNs were subject to ex vivo imaging due to the presence of fluorescence. The excised SLNs were sent to pathological anatomy and processed according to the standard SLN protocol [19].
Results
Two sentinel lymph nodes were removed, one for each treated patient using a near-infrared fluorescence (NIRF) camera, and fluorescence detection after injection of indocyanine green (ICG). In the first clinical case, the sentinel lymph node (SLN) was contralateral to the left paramedian vulvar lesion (Fig. 2). The failure to identify the SLN in the left inguinal area, homolaterally to the site of more significant development of the vulvar lesion, was due to the 15-min wait between the administration of the ICG and the viewing of fluorescence through a near-infrared fluorescence (NIRF) camera. In fact, 30 min after the start of the procedure, it was possible to locate the lymphatic pathway and the SLN in the right inguinal area (Fig. 3). The sentinel node was found in the deep inguinal area. As per standard protocol, the removed SLN, subjected to definitive histological examination, was negative for metastatic localization.
In the second clinical case, the SLN was detected 30 min after the administration of indocyanine green (ICG) and subsequent visualization with near-infrared fluorescence (NIRF) camera. The SLN was identified in the right inguinal area, homolaterally to the vulvar lesion (Figs. 3 and 4). After removing the two SLNs, both were subjected to ex vivo visualization with near-infrared fluorescence (NIRF) camera and exhibited bright fluorescence (Fig. 5). The sentinel nodes were found in the deep inguinal area. As per standard protocol, the removed SLNs, subjected to definitive histological examination, were negative for metastatic localization. All inguinal lymph nodes removed during the surgical procedures gave negative results for the localization of metastases.
Discussion
Intraoperative detection of sentinel lymph node (SLN) in vulvar squamous cell carcinoma (vSCC) by peritumor administration of indocyanine green (ICG) and near-infrared fluorescence (NIRF) camera has numerous advantages. This procedure replaced the standard procedure for administering a radioactive tracer, which, according to The European Society of Gynaecological Oncology (ESGO) guidelines, has been mandatory and could prevent patients with early-stage vulvar cancer from experiencing peritumoral injection associated discomfort before surgery [18]. Additionally, the superficial localization of most inguinal lymph nodes may allow for transcutaneous lymphatic mapping in the groin. Finally, a significant proportion of tumors are located near or in the midline. The transcutaneous lymphatic mapping could also help determine the size and number of SLNs comparable to lymphoscintigraphy when using a radioactive tracer.
In the two treated patients, the waiting time between injection of the indocyanine green (ICG) tracer and viewing by a SPY Portable Handheld Imager (SPY-PHI) camera was approximately 30 min. This duration, considered acceptable for the intraoperative management of the patient, permits gradual visualization, in real-time, of the lymphatic pathway of tumor drainage and the easy localization of the SLN by transcutaneous route, or, if the thickness of the adipose tissue is excessive and the patient’s BMI> 25 after incision of the groin homolaterally to the vulvar lesion. The limitation of this procedure could be related to the fact that near-infrared fluorescence (NIRF) imaging has a maximum penetration depth of approximately 5 mm in the tissue (fat) [20]. Therefore, the detectability of SLNs in patients with higher BMIs can be difficult. In our experience, which consisted of only two clinical cases treated, we did not notice any differences in latency time between injection of the indocyanine green (ICG) tracer and visualization of the SLN. Furthermore, our experience has allowed us to find a correspondence between the absence of metastatic localization between the resected sentinel lymph node and the inguinofemoral lymph nodes removed in bilateral inguinal lymphadenectomy. This could open up a new view for the application of intraoperative imaging in real-time given by the indocyanine green (ICG) tracer’s use in early-stage vulvar cancer. While requiring further large-scale studies and standardization of the procedure, this method has numerous advantages compared to the administration of a radiotracer alone.
Conclusions
The preliminary data in our possession, therefore, has the objective of defining guidelines to be applied on a large scale regarding the dosage of indocyanine green (ICG) to be used in peritumoral initiation as well as defining the standard waiting time to be able to perform visualization of the sentinel lymph node (SLN), data, to date, not present in the literature. Our experience provides us with information that seems to be encouraging in this sense. It opens up the possibility of a different intraoperative surgical management of early-stage vulvar cancer.
Abbreviations
- BMI:
-
Body mass index
- CT:
-
Computed tomography
- ESGO:
-
European Society of Gynaecological Oncology
- ICG:
-
Indocyanine green
- NIRF:
-
Near-infrared fluorescence
- SLN:
-
Sentinel lymph node
- SPY-PHI:
-
SPY portable handheld imager
- vSCC:
-
Vulvar squamous cell carcinoma
References
Weinberg D, Gomez-Martinez RA (2019) Vulvar cancer. Obstet Gynecol Clin N Am 46:125–135. https://doi.org/10.1016/j.ogc.2018.09.008
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics. CA Cancer J Clin 67:7–30. https://doi.org/10.3322/caac.21387
American Cancer Society (2018) Cancer facts & figures 2018. American Cancer Society
Zweizig S, Korets S, Cain JM (2014) Key concepts in management of vulvar cancer. Best Pract Res Clin Obstet Gynaecol 28:959–966. https://doi.org/10.1016/j.bpobgyn.2014.07.001
Hampl M, Deckers-Figiel S, Hampl JA et al (2008) New aspects of vulvar cancer: changes in localization and age of onset. Gynecol Oncol 109:340–345. https://doi.org/10.1016/j.ygyno.2008.01.041
Pecorelli S (2009) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet 105:103–104. https://doi.org/10.1016/j.ijgo.2009.02.012
Gaarenstroom KN, Kenter GG, Trimbos JB et al (2003) Postoperative complications after vulvectomy and inguinofemoral lymphadenectomy using separate groin incisions. Int J Gynecol Cancer 13:522–527. https://doi.org/10.1046/j.1525-1438.2003.13304.x
Rouzier R, Haddad B, Dubernard G et al (2003) Inguinofemoral dissection for carcinoma of the vulva: effect of modifications of extent and technique on morbidity and survival. J Am Coll Surg 196:442–450. https://doi.org/10.1016/s1072-7515(02)01895-1
De Hullu JA, Hollema H, Lolkema S et al (2002) Vulvar carcinoma. The price of less radical surgery. Cancer 95:2331–8. https://doi.org/10.1002/cncr.10969
Hassanzade M, Attaran M, Treglia G et al (2013) Lymphatic mapping and sentinel node biopsy in squamous cell carcinoma of the vulva: systematic review and meta-analysis of the literature. Gynecol Oncol 130:237–245. https://doi.org/10.1016/j.ygyno.2013.04.023
Johann S, Klaeser B, Krause T et al (2008) Comparison of outcome and recurrence-free survival after sentinel lymph node biopsy and lymphadenectomy in vulvar cancer. Gynecol Oncol 110:324–328. https://doi.org/10.1016/j.ygyno.2008.04.004
Hacker NF, Berek JS, Lagasse LD et al (1983) Management of regional lymph nodes and their prognostic influence in vulvar cancer. Obstet Gynecol 61:408–412
Howland J (1988) Preventing automobile injury: new findings from evaluative research. Auburn House Publishing Company, pp 163–196
Francis JA, Eiriksson L, Dean E et al (2019) No. 370 management of squamous cell cancer of the vulva. J Obstet Gynaecol Can 41:89–101. https://doi.org/10.1016/j.jogc.2018.07.004
Levinson K, Mahdi H, Escobar P (2013) Feasibility and optimal dosage of indocyanine green fluorescence for sentinel lymph node detection using robotic single site instrumentation: preclinical study. J Minim Invasive Gynecol 20:691–696. https://doi.org/10.1016/j.jmig.2013.03.013
Furukawa N, Oi H, Yoshida S et al (2010) The usefulness of photodynamic eye for sentinel lymph node identification in patients with cervical cancer. Tumori 96:936–940
Hacker NF (2009) Revised FIGO staging for carcinoma of the vulva. Int J Gynecol Obstet 105:105–106. https://doi.org/10.1016/j.ijgo.2009.02.011
Pecorino B, Scibilia G, Ferrara M et al (2020) Prognostic factors and surgical treatment in vulvar carcinoma: single center experience. J Obstet Gynaecol Res 46:1871–1878. https://doi.org/10.1111/jog.14368
de Hullu JA, Hollema H, Piers DA et al (2000) Sentinel lymph node procedure is highly accurate in squamous cell carcinoma of the vulva. J Clin Oncol 18:2811–6. https://doi.org/10.1200/jco.2000.18.15.2811
Vahrmeijer AL, Hutteman M, van der Vorst JR et al (2013) Image-guided cancer surgery using near- infrared fluorescence. Nat Rev Clin Oncol 10:507–518. https://doi.org/10.1038/nrclinonc.2013.123
Acknowledgements
Not applicable
Funding
This research did not receive any funding from the public, commercial, or not-profit sectors.
Author information
Authors and Affiliations
Contributions
The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Written informed consent for publication was obtained.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Scollo, P., Ferrara, M., Pecorino, B. et al. Indocyanine green fluorescence imaging, sentinel lymph node mapping in patients with vulvar cancer: peritumoral injection dosage and waiting times in our experience. Gynecol Surg 18, 4 (2021). https://doi.org/10.1186/s10397-021-01085-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10397-021-01085-8