Abstract
Our objective is to show a feasible approach to the hysteroscopic procedures when the cervical canal has a diameter smaller than the lesion. Our study is designed as a case series and illustration of the surgical hysteroscopic technique. A group of patients (n = 37) underwent office hysteroscopy in Regional Reference Center for Hysteroscopy Service at Palagi Hospital, Florence, Italy, to see and treat an endometrial polyp with unfavorable cervical conditions between January 2019 and December 2019. An office hysteroscopy in outpatient setting with vaginoscopic approach was performed in women with unfavorable cervical conditions. Fiber-based 3.5-mm hysteroscope, with 5F electrosurgery unit and 5F bipolar electrode, was used to perform the cervicoplasty in order to enlarge the cervical canal from internal to external os, following by the removal of the endometrial polyp with the excision of the base only without slicing. After 90 days, a follow-up hysteroscopy was performed. The procedure was performed successfully in 89.2% of patients.
The surgical technique of cervicoplastic allows to perform an operative procedure without analgesia/sedation or anesthesia or blind cervical dilation, reducing the risk of complications and costs. Furthermore, cervicoplasty allowed the removal en bloc of the endocavitary lesion in all cases. At the follow-up hysteroscopy, the cervical passage was straight and smooth, without lesions repaired in all patients. Cervicoplasty is a technique which allows to perfume an ease and comfortable hysteroscopic procedure even in patients with unfavorable cervical canal. Due to the widening of the diameter of the cervical canal, intracavitary lesions are removed intact resulting in an optimal pathological evaluation.
Similar content being viewed by others
Background
Hysteroscopic surgery is commonly used to manage and treat different gynecological pathologies. Modern hysteroscopic technologies are available to combine the possibility to explore the uterine cavity and also treat surgically the disease (“see-and-treat-approach”).
A tortuous conformation of cervical canal, as well as stenosis or adhesions, might represent an obstacle in outpatient gynecological procedures where an easy and comfortable access of the uterine cavity is necessary. In addition, the cervical canal is pivotal not only for the access into the endometrial cavity but also for the removal of a large intracavitary neoformation, or for embryo transfer during in vitro fertilization [1, 2].
Cervical stenosis may be congenital or secondary to cervical trauma, infection, cancer, radiation, conization, or postmenopausal atrophy with a still undefined prevalence or incidence [3]. In a series of 31,052 office hysteroscopies, Bettocchi et al. identified cervical stenosis in 32.7% of cases, with a major prevalence in postmenopausal women than in reproductive age women (70.1% vs 29.9%), being the combined stenosis of both external and internal cervical os the most common form [4].
The diameter of the cervical canal and the age of patients influence the perception of pain during the procedure, affecting feasibility and acceptability of the surgical technique [5, 6]. Currently, cervical dilatation is the most used method to treat cervical stenosis by the use of Hegar uterine dilatator [7] in an inpatient setting and the use of anesthesia with consequences on patient outcomes and hospital costs.
In this context, a hysteroscopic technique that allows to expand the cervical canal in an outpatient procedure might be useful in large intracavitary neoformation.
Material and methods
The study was designed as a retrospective case series. Data were collected from a group of women (n = 37) undergoing hysteroscopy with unfavorable cervical conditions, namely, a lesion bigger than the cervical diameter, a previous conization, or a stenotic or tortuous cervical canal. Surgery was performed by using a fiber-based 3.5-mm hysteroscope (Versascope, Gynecare, Ethicon, Inc., Somerville, NJ, USA) in order to remove an endometrial polyp. The excision of the polyp was made at the base of the lesion so that it was removed intact. All the procedures were performed in an office setting, without analgesia/sedation or anesthesia, between January 2019 and December 2019, in the Regional Reference Center for Hysteroscopy, Palagi Hospital, Florence. The patients were followed up with a hysteroscopy after 90 days from the procedure. The study was approved by the local IRB.
Surgical technique is explained by a video reporting a successful office hysteroscopy of a 35-year-old woman, para 0 with a large polyp.
Patients
The mean age of the study population was 47.8 ± 13.62 years (range 31–77), and 13 (35.1%) patients were in the postmenopausal age. The mean body mass index was 25.6 ± 6.1 kg/m2 (range 20.4–43.3). Eight (21.6%) women were nulliparous. Three patients had a previous cervical conization. The main characteristics of the patients are shown in Table 1.
Results
Technique
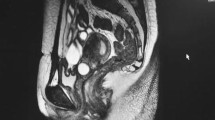
A vaginoscopic approach using a fiber-based 3.5-mm hysteroscope was used. A 5F Gynecare Versapoint2 electrosurgery unit and 5F bipolar electrode Versapoint Twizzle (Gynecare, Menlo Park, CA) were inserted. Localizing the internal os, a lateral cut was performed for all the length of the cervical canal until the external os for each side. The maximum depth of lateral cutting is 2.1 mm for each side, assuming that the angle of cut is 45° with a 3-mm length of the electrode, with a possible maximum enlargement of 6 mm for each side (Video 1). The polyp was excised at the base, and with a tenaculum, we proceed to the transport through the cervical canal. Patients did not experience pain during the procedure. No abnormal bleeding occurred during the surgical procedure. After 90 days, a hysteroscopy was done to assess the cervical canal. We found an intact cervical canal with no signs of damage or injury (Fig. 1).
Additional file 1: Video 1. Cervicoplasty (attached as e-mail as requested).
Case series
The procedure was successfully performed in 89.2% of the patients (33/37). The failure of the technique was in one patient with previous conization, since no external cervical os were detectable. In other three cases, the polyp needed to be sliced in order to be removed. The procedure time varied between 2 and 4 min. In all patients who performed the hysteroscopy (36/37, 97.3%), the followed up hysteroscopy showed a normal mucosal surface in the cervical canal.
Discussion
In an outpatient setting, office hysteroscopy for the removal of endocavitary neoformations, such as polyps or small myomas, is occasionally hampered by cervical stenosis or the large dimension of the lesion. Moreover, the size of the intracavitary neoformation is pivotal for the success and the duration of the procedure, being related to the diameter of the cervical canal [8,9,10]. Our surgical technique may be adopted in patients with a large diameter polyp in an office setting, providing the enlargement of the cervical canal.
Indeed, the size of endocavitary neoformation is not the only factor that influences the feasibility of the procedure, but there are some additional elements like texture, position, form, and planting base of neoformation that might influence the success of outpatient operative hysteroscopy; in addition, also in successful circumstances, all these factors could cause a prolonged operation time that affects patient’s compliance [11, 12]. A factor that can, also, influence the feasibility of an office hysteroscopy is the hysteroscopist’s experience and the instrument size which is crucial for determining the reduction of pain during an office vaginoscopic hysteroscopy, while the type of uterine distension medium is less important in the perception of pain. Smaller diameter of the instruments are associated to less pain for infertile patients with a vaginoscopic approach and the training level of the gynecologist is crucial in perceived pain especially when the indication of hysteroscopy is primary infertility [13]. The patency of the cervical canal is an important factor. If the cervical canal is wide, the instrument can be angled leading to an easier maneuver and extraction. On the other hand, when the canal is narrow, the procedure might fail or be associated with prolonged duration and increase in the pain VAS score. In an observational study on office hysteroscopic procedures, the majority of women experienced no discomfort in all pathologic conditions treated except for endometrial polyps larger than the internal cervical os, in which women experienced low or moderate pain [14]. The introduction of innovative hysteroscopic tissue removal system, such as Trueclear 5C, fragments the polyps in small-size fragments that are immediately captured to do a pathological diagnosis [11] providing adequate tissue for pathological diagnosis despite the effects of tissue fragmentation [15]. The outpatient cervicoplasty could make easier the extraction of neoformations. This technique allows a low learning curve for new surgical operator, the transport of removed neoformations in bigger fragments or even en bloc with a reduced operative time, more comprehensive histological response due to a minor thermal damage, less patient discomfort, and increased success rate of the office operative hysteroscopy in an outpatient setting.
The present surgical technique has several strengths: the isthmic mucosa is thin, smooth, and has no large caliber arterial vessels; the bipolar electrode on the small vessels allows a safe state of coagulation avoiding important blood loss; and the neighboring organs are preserved from lateral cervical cutting. The bladder is forward, the rectum is behind the cervical canal, and the ureter is lateral, which is generally located 15 mm laterally to the isthmic margin and 10 mm above side the vaginal fornix.
Moreover, cervicoplasty reduces the trauma on the cervical channel during the extraction of the big lesions, reducing the incidence of long-term sequela on the cervical patency and myometrium strength [16,17,18].
Recently, a hysteroscopic technique has been published to treat a narrow cervical canal when ET or intrauterine insemination failed due to cervical factor. A similar technique was used in the past for some cases of ART [19, 20]. A resectoscopic cervical shaving in general anesthesia and after cervical dilatation was performed, followed by ET in a second time; in all four cases, ET was feasible and successful without preterm delivery. Another study used a hysteroscopic surgery in infertile women as safe and effective treatment for cervical stenosis [21]. Our technique, conversely, is performed without sedation or anesthesia.
Finally, our technique which might help for colposcopic follow-up in patients who had undergo conization for cervical pathology and had developed a stenotic cervical is not performable. The incidences of stenosis after conization are hard to compare because definitions vary greatly and, also, it depends on the surgical technique. Hasegawa et al. reported that premenopausal and postmenopausal patients with a prior laser cone biopsy had an incidence of cervical stenosis between 8.3 and 59.1%, respectively [22]. Houlard et al. suggested to adopt other surgical options other than conization in the management of cervical pathology when patient age exceeds 40 years [23]. Some studies underline the risk of undetected cervical or endometrial neoplasms in patients with cervical stenosis after conization [24].
Conclusion
Cervicoplasty is an effective, painless, and safe hysteroscopic procedure that might help gynecologists in hysteroscopic surgeries when the intracavitary lesion exceeds the cervical canal caliber, especially in an outpatient setting. This procedure reduces discomfort of the patient, cutting down the operative time and increasing operative feasibility.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Brown, J., Buckingham, K., Abou-Setta, A.M. and Buckett, W. (2010) Ultrasound versus ‘clinical touch’ for catheter guidance during embryo transfer in women. Cochrane Database Syst Rev Issue 1. Art. No.: CD006107.
Mahajan N, Gupta I (2011) Use of Versapoint to refashion the cervical canal to overcome unusually difficult embryo transfers and improve in-vitro fertilization-embryo transfer outcome: a case series. J Hum Reprod Sci 4(1):12–16
Wood MA, Kerrigan KL, Burns MK, Glenn TL, Ludwin A, Christianson MS, Bhagavath B, Lindheim SR (2018) Overcoming the challenging cervix: identification and techniques to access the uterine cavity. Obstet Gynecol Surv 73(11):641–649
Bettocchi S, Bramante S, Bifulco G et al (2016) Challenging the cervix: strategies to overcome the anatomic impediments to hysteroscopy: analysis of 31,052 office hysteroscopies. Fertil Steril 105:16–17. https://doi.org/10.1016/j.fertnstert.2016.01.030
Cicinelli E (2010) Hysteroscopy without anesthesia: review of recent literature, J minim invasive Gynecol.; 17. https://doi.org/10.1016/j.jmig.2010.07.003
Troia L, Darino I, Regini C, Vellucci FL, Orlandini C, Razzi S, Severi FM, Luisi S (2019) Factors affecting pain perception in outpatient hysteroscopy. European Gynecology and Obstetrics 1(1):39–42
Christianson M, Barker M, Lindheim S (2008) Overcoming the challenging cervix: techniques to access the uterine cavity. J Low Genit Tract Dis 12:24
Rovira Pampalona J, Degollada Bastos M, Mancebo Moreno G, Ratia Garcia E, Buron Pust A, Mateu Pruñonosa JC, Guerra Garcia A, Carreras Collado R, Bresco TP (2015) Outpatient hysteroscopic polypectomy: bipolar energy system (Versapoint®) versus mechanical energy system (TRUCLEAR system®)—preliminary results. Gynecol Obstet Investig 80(1):3–9
Hamerlynck TW, Schoot BC, van Vliet HA, Weyers S (2015) Removal of endometrial polyps: hysteroscopic morcellation versus bipolar resectoscopy, a randomized trial. Minim Invasive Gynecol 22(7):1237–1243
Noventa M, Ancona E, Quaranta M, Vitagliano A, Cosmi E, D’Antona D, Gizzo S (2015) Intrauterine morcellator devices: the icon of hysteroscopic future or merely a marketing image? A systematic review regarding safety, efficacy, advantages, and contraindications. Reprod Sci 22(10):1289–1296
Ceci O, Franchini M, Cannone R, Giarrè G, Bettocchi S, Fascilla FD, Cicinelli E (2019) Office treatment of large endometrial polyps using truclear 5C: feasibility and acceptability. Obstet Gynaecol Res 45(3):626–633
Li C, Dai Z, Gong Y, Xie B, Wang B (2017) A systematic review and meta-analysis of randomized controlled trials comparing hysteroscopic morcellation with resectoscopy for patients with endometrial lesions. Int J Gynaecol Obstet 136:6–12
Pluchino N, Ninni F, Angioni S, Artini P, Araujo VG, Massimetti G, Genazzani AR, Cela V (2010) Office vaginoscopic hysteroscopy in infertile women: effects of gynecologist experience, instrument size, and distention medium on patient discomfort. J Minim Invasive Gynecol 17(3):344–350
Bettocchi S, Ceci O, Di Venere R et al (2002) Advanced operative office hysteroscopy without anaesthesia: analysis of 501 cases treated with a 5 Fr. Bipolar electrode. Hum Reprod 17:2435–2243
Franchini M, Zolfanelli F, Gallorini M, Giarrè G, Fimiani R, Florio P (2015) Hysteroscopic polypectomy in an office setting: specimen quality assessment for histopathological evaluation. Eur J Obstet Gynecol Reprod Biol 189:64–67
Mannini L, Sorbi F, Ghizzoni V, Masini G, Fambrini M, Noci I (2016) Spontaneous unscarred uterine rupture at 15 weeks of pregnancy: a case report. Ochsner J 16(4):545–547
Sorbi F, Sisti G, Pieralli A, Di Tommaso M, Livi L, Buccoliero AM, Fambrini M (2013) Cervicoisthmic choriocarcinoma mimicking cesarean section scar ectopic pregnancy. J Res Med Sci 18(10):914–917
Sisti G, Nasioudis D, Kanninen T, Sorbi F, Fambrini M. (2015) Risk factors for development of isthmocele following cesarean section. Minerva Ginecol. Aug;67(4):301-306.
Noyes N, Licciardi F, Grifo J, Krey L, Berkeley A (1999) In vitro fertilization outcome relative to embryo transfer difficulty: a novel approach to the forbidding cervix. Fertil Steril 72:261–265
Pabuccu R, Ceyhan ST, Onalan G, Goktolga U, Ercan CM, Selam B (2005) Successful treatment of cervical stenosis with hysteroscopic canalization before embryo transfer in patients undergoing IVF: a case series. J Minim Invasive Gynecol 12:436–438
Lin YH, Hwang JL, Huang LW, Seow KM, Chen HJ, Tzeng CR (2013) Efficacy of hysteroscopic cervical resection for cervical stenosis. J Minim Invasive Gynecol 20:836–841
Hasegawa K, Torii Y, Kato R et al (2016) The problems of cervical conization for postmenopausal patients. Eur J Gynaecol Oncol 37:327–331
Houlard S, Perrotin F, Fourquet F, Marret H, Lansac J, Body G (2002) Risk factors for cervical stenosis after laser cone biopsy. Eur J Obstet Gynecol Reprod Biol 104:144–147
Penna C, Fambrini M, Fallani MG, Pieralli A, Scarselli G, Marchionni M (2005) Laser CO2 conization in postmenopausal age: risk of cervical stenosis and unsatisfactory follow-up. Gynecol Oncol 96(3):771–775
Acknowledgments
Not applicable.
Funding
The authors declare no funding.
Author information
Authors and Affiliations
Contributions
SC, VD, and FP designed the study; SC, CC, DP, FS, and KLA collected, analyzed, and interpreted the data; SC, EC, and GG were the surgeons responsible for and provided the patient recruitment; CC, DP, and FS prepared the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We have received the ethics approval and the consent from the patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Calzolari, S., Comito, C., Pavone, D. et al. Extending cervicoplastic surgery: an alternative technique to overcome the limitation of office hysteroscopy. Gynecol Surg 17, 8 (2020). https://doi.org/10.1186/s10397-020-01076-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10397-020-01076-1