Abstract
Background
This retrospective medium-term follow-up study compares the outcomes of medial fixed-bearing unicompartmental knee arthroplasty (mUKA) using a cemented metal-backed (MB) or an all-polyethylene (AP) tibial component.
Materials and methods
The database of our institution was mined for primary mUKA patients implanted with an MB or an AP tibial component (the MB-UKA and AP-UKA groups, respectively) from 2015 to 2018. We compared patient demographics, patient-reported outcome measures (PROMs), and motion analysis data obtained with the Riablo™ system (CoRehab, Trento, Italy). We conducted propensity-score-matching (PSM) analysis (1:1) using multiple variables.
Results
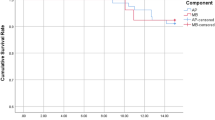
PSM analysis yielded 77 pairs of MB-UKA and AP-UKA patients. At 5 years, the physical component summary (PCS) score was 52.4 ± 8.3 in MB-UKA and 48.2 ± 8.3 in AP-UKA patients (p < 0.001). The Forgotten Joint Score (FJS-12) was 82.9 ± 18.8 in MB-UKAs and 73.4 ± 22.5 in AP-UKAs (p = 0.015). Tibial pain was reported by 7.8% of the MB-UKA and 35.1% of the AP-UKA patients (p < 0.001). Static postural sway was, respectively, 3.9 ± 2.1 cm and 5.4 ± 2.3 (p = 0.0002), and gait symmetry was, respectively, 92.7% ± 3.7 cm and 90.4% ± 5.4 cm (p = 0.006). Patient satisfaction was 9.2 ± 0.8 in the MB-UKA and 8.3 ± 2.0 in the AP-UKA group (p < 0.003).
Conclusions
MB-UKA patients experienced significantly better 5-year static sway and gait symmetry outcomes than AP-UKA patients. Although the PROMs of the two groups overlapped, MB-UKA patients had a lower incidence of tibial pain, better FJS-12 and PCS scores, and were more satisfied.
Similar content being viewed by others
Introduction
Osteoarthritis of the knee (KOA) is highly prevalent on a global scale and is the primary cause of musculoskeletal disability. It limits physical and work activity, affects quality of life, and involves elevated healthcare expenses [1,2,3]. When conservative approaches prove ineffective, surgical intervention, in the form of partial or total knee replacement, becomes necessary. Both procedures are common in developed countries, and their prevalence is expected to rise substantially in the future [2, 4]. Unicompartmental knee arthroplasty (UKA) has garnered increasing popularity in recent times, as multiple studies have indicated that it is less invasive, involves a shorter duration of surgery, provides a wider range of motion, offers greater pain relief, enables a quicker return to daily activities and sports, and is less expensive than total knee arthroplasty (TKA) [5,6,7,8,9,10,11].
In about 90% of cases, UKA is performed on the medial tibiofemoral joint [12, 13]. Among the decisions to be made in the surgical approach to UKA are the implant fixation method (cemented or uncemented), the design (mobile or fixed bearing), and the placement (conventional or robotic).
In fixed-bearing UKA, the tibial component is usually either all polyethylene (AP) or metal backed (MB). Whereas the former component is thicker, ensuring preservation of the bone stock for eventual surgical revision, and is associated with a lower implant cost [14, 15], the latter provides greater flexibility during surgery and allows for separate bearing replacement [16]. However, an MB component has potential issues with wear on the backside of the interface [17], greater bone loss in case of implant failure [18], and a higher cost [19]. Two studies have found that AP components provide slightly better functional outcomes than MB components [16, 20], whereas biomechanical studies have demonstrated greater stress and strain on the proximal tibial cancellous bone in patients with AP components [19, 21, 22]. Elevated tibial bone strain and microdamage have been suggested as factors that contribute to unexplained pain and suboptimal outcomes [23, 24]. Whereas one study has described better functional outcomes with an MB than with an AP tibial component at medium-term follow-up [25], other studies, including a meta-analysis, have found no discernible differences in functional outcomes between them [14, 24, 26,27,28].
In recent years, instrumented motion analysis has increasingly been used to gain an objective and quantitative description of an individual’s motor functions and abilities [29,30,31]. This method plays a key role in the evaluation of pathological conditions, compensatory motor strategies, and the monitoring of improvement during rehabilitation. It also offers a more sensitive and objective means of assessment compared to the ordinal scoring used in “semiquantitative” clinical scales [32]. Critically, instrumented motion analysis allows the kinematic and kinetic parameters of human movements to be determined and musculoskeletal functions to be assessed in a quantitative manner. Consequently, it has found numerous applications in clinical assessments, rehabilitation, sports, and even diagnostics [33].
Since the turn of the new millennium, technological advances in motion measurement techniques have facilitated the assessment of body segment kinematics through wearable inertial sensors that are miniaturized inertial measurement units (IMUs), which quantify three-dimensional linear acceleration and angular velocity with respect to the axes of a sensor-embedded frame of reference [34].
In the coming years, these devices are expected to see ever-wider clinical utilization through integration into various devices designed specifically for clinical interventions (particularly rehabilitation), thus extending beyond research and motor function assessment. Several companies have incorporated IMUs into video-game-based rehabilitation systems such as the Riablo™ system (CoRehab, Trento, Italy) [35]. This trend reflects the growing awareness of the potential of wearable inertial devices to enhance clinical interventions and rehabilitation.
The aim of this study was to determine whether there is a difference in medium-term functional outcome scores, health-related quality of life (HRQL) scores, and static postural sway, mobility, and gait symmetry between medial UKA (mUKA) patients implanted with an MB or an AP tibial component.
Materials and methods
Patient selection
Following approval by the institutional review board, the database of the Orthopedic Department of IRCCS Sacro Cuore-Don Calabria Hospital (Negrar di Valpolicella, Italy) was mined for all primary mUKAs performed from 2015 to 2018. There were 653 such procedures, 342 involving an MB and 311 involving an AP tibial component.
The data collected included demographics, body mass index (BMI), medical history, American Society of Anesthesiologists (ASA) class, operative time, length of hospital stay, any revision surgeries or complications, clinical outcomes, and patient satisfaction.
Indications of surgery
All mUKAs were performed on patients with primary KOA of the medial compartment who, after a 3-month conservative treatment including physical therapy, intra-articular cortisone injections, rest, and anti-inflammatory medications, still experienced substantial pain. After a review of their medical history, a physical examination, and a preoperative radiographic assessment, these patients were considered eligible for mUKA [36].
Inclusion and exclusion criteria
We enrolled all the patients with a 5-year follow-up who met the classic mUKA selection criteria described by Kozinn and Scott in 1989 [37], i.e., a preoperative mechanical axis deformity of less than 10° in varus or 5° in valgus and a flexion contracture of less than 15°. Further criteria were an intact/competent anterior cruciate ligament, an intact lateral compartment, patellofemoral changes of no greater than grade II or III according to the Albach classification [38], and trochlear wear up to grade IV, provided it presented a central distribution [39].
Patients with primary lateral KOA, a history of complex knee surgery, significant trauma, inflammatory arthropathy, ataxia or neurological disease, psychiatric disorders (or who were in treatment), symptomatic KOA in the contralateral knee, and those who had required bilateral UKA or mUKA revision for aseptic loosening or infection during follow-up were excluded.
All patients provided their signed informed consent.
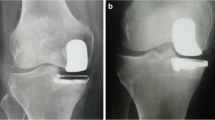
Surgical procedure
All patients received the Link Sled® fixed-bearing prosthesis (LINK, Hamburg, Germany) with an MB or an AP cemented tibial component. All procedures were performed under spinal anesthesia associated with an adductor canal nerve block. A tourniquet was used in all cases. Surgeries were performed through an 8- to 10-cm limited medial midvastus approach without lateral patellar subluxation using a Link Mitus® ART (anatomic reconstruction technique) instrument set for minimally invasive surgery. The tibial cut was performed first to remove 5 mm of thickness from the most degraded portion of the plateau. The sagittal inclination was set according to the native tibial slope. Femoral preparation was performed by removing the cartilage layer with a saw blade. The femoral component was oriented according to the condyle anatomy. The aim of the procedure was to achieve an equal flexion–extension gap and to restore normal leg alignment. All implants were cemented. A suction drain was placed in all patients and removed the day after surgery.
Rehabilitation protocol
Patients initiated rehabilitation on the first postoperative day. They engaged in a daily 90-min session with a physiotherapist in the morning and in an additional 90-min session without supervision in the afternoon. Immediate weight-bearing was prescribed. Crutches were indicated for the first month. Upon discharge, typically between day 3 or 4. The discharge was mutually agreed upon by the orthopedist, physiotherapist, internal medicine specialist, and patient, taking into consideration the clinical condition and attainment of short-term rehabilitation goals.
Clinical outcomes
Key preoperative and postoperative variables were collected by qualified personnel of the Orthopedic Department. Patients were assessed preoperatively and then at 12 months and 5 years with five major patient-reported outcome measures (PROMs): the Knee Society Function Score (KSFS), the Knee Society Knee Score (KSKS) [40], and the Oxford Knee Society (OKS) Score [41, 42] as well as the physical component summary (PCS) and mental component summary (MCS) of the Short Form 36 Health Survey (SF-36), which measures HRQL [43].
At 5 years, we assessed the Forgotten Joint Score-12 (FJS-12) [44], patient satisfaction (ranging from 1, not satisfied, to 10, completely satisfied), the presence of tibial pain (particularly under the prosthetic tibial plateau) on the Numerical Rating Scale (NRS), and static postural sway, mobility, and gait symmetry, the latter three measures using the RiabloTM system.
Static postural sway and gait symmetry
The RiabloTM device is an adaptive system comprising multiple IMUs and a force platform, all wirelessly connected to a computer. It has been developed to enhance conventional rehabilitation programs by directing users while performing prescribed physical exercises through a video interface. Each IMU weighs 20 g. IMUs operate on the wireless Bluetooth™ communication protocol and have a sampling frequency of 50 Hz [35]. The sensors are held in place with elastic bands. We employed three bands, which were attached (i) to the chest at the level of the mammillary line, and (ii) at the mid-thigh, and (iii) at mid-tibial level on the affected or the healthy limb, depending on the exercise. Data collected from five distinct exercises were then analyzed by the system to provide information on static postural sway, mobility, and gait symmetry:
-
1.
The Timed Up & Go Test was used to assess the time the subject took to rise from a chair (seat height, 46 cm), walk a distance of 3 m, pivot, and return to a seated position in the chair [45].
-
2.
The Sit-to-Stand Test, a practical test frequently employed as a measure of functional performance, was applied to assess the time required to move from a seated to a standing position a given number of times or to record the repetitions executed in a given time interval [46].
-
3.
The Figure-of-8 Test was employed to evaluate walking proficiency in a single task: walking in a figure-of-8 pattern. Curved trajectories are key to navigating the figure-of-8 pattern, since the transition from a linear to a bending path and the adjustment of body movements in clockwise and counterclockwise directions replicates walking in everyday situations [47].
-
4.
The Half-Turn Test has been incorporated into evaluations of mobility and balance for older individuals [48]. We used it to assess the ability to execute a swift and efficient turn. Participants were asked to take a few steps and then rapidly turn about to face the opposite direction. We measured the number of steps required to complete the 180° turn.
-
5.
The Alternate Step Test, a version of the stool stepping task and one of the tests of the Berg Balance Scale [48], assesses coordinated weight shifting and serves as an indicator of lateral stability. Patients were required to rapidly mount a step measuring 18 cm in height and 40 cm in depth alternately with the left and the right unshod foot. We measured the time taken to accomplish eight steps.
Postural sway was evaluated using the Riablo™ stabilometric platform, where two pressure matrices, each fitted with 160 pressure sensors, record weight in a gradual manner. The maximum weight the pressure board can bear is 200 kg between the matrices. The platform communicates with the software through a Bluetooth protocol.
Statistical analysis
Data analysis was performed using Microsoft Excel (2019) in conjunction with the XLSTAT resource pack (XLSTAT Premium, Addinsoft, New York, NY, USA). A propensity-score-matching (PSM) analysis was employed to minimize variations in known covariates between the cohorts [49], since several retrospective arthroplasty studies have used this type of analysis to minimize selection bias [8, 27, 50,51,52,53,54,55,56,57]. The two patient groups were matched one-to-one by an optimal matching algorithm [58]. The algorithm identifies matched samples with the smallest average absolute distance across all matched pairs. This technique, regarded as an optimal method to evaluate differences between treatment groups, was applied to mitigate the impact of potential confounding variables [59]. Patients were considered suitable for matching if the propensity score discrepancy between the groups fell within the caliper radius of 0.01 × sigma. The strength of the association and 95% confidence intervals were determined. The variables on which the two groups were harmonized included gender and ASA class (categorical data), age, BMI, preoperative KSFSs, KSKSs, and the OKS, PCS, and MCS scores (quantitative data).
The Shapiro–Wilk test was applied to determine whether the data had a normal distribution. Calculated mean values and standardized mean differences (SMDs) were also obtained for all continuous data. A non-parametric test, the Mann–Whitney test for unpaired data, and the Wilcoxon signed-rank test for paired data were employed to evaluate significant differences in continuous variables between the groups. Categorical data were analyzed using the chi-square test. Discrepancies between the MB and AP groups were assessed by comparing the SMD before and after matching. A group was regarded as imbalanced for a particular covariate if the SMD exceeded 0.2 [49]. A significance level of p < 0.05 was considered statistically significant.
Results
The search of the institutional database yielded 653 mUKAs with a 5-year follow-up; of these, 342 had used an MB component (MB-UKAs) and 311 an AP component (AP-UKAs). A total number of 136 MB-UKAs and 124 AP-UKAs met the study criteria. PSM analysis successfully matched 77 pairs of patients for gender, age, BMI, ASA class and preoperative KSFSs, KSKSs, and OKS, PCS, and MCS scores.
Demographics
Before PSM analysis, the two groups (136 MB-UKA and 124 AP-UKA patients) showed an imbalance in terms of BMI (the SMD was 0.82) and age, which was significantly different (p = 0.010). After PSM analysis, where patients were matched 1:1, we had two similar groups devoid of significantly different preoperative, perioperative, and postoperative features (Table 1).
Clinical outcomes
Before PSM analysis, the two groups were imbalanced in terms of KSFSs, with an SMD of 0.30. After PSM analysis, there were no residual significant differences. The preoperative KSFSs, KSKSs, and OKS, PCS, and MCS scores were not significantly different either before or after matching (Table 2).
After matching, the PCS score at 12 months was 51.8 ± 7.6 (range 29–62) in MB-UKA and 49.1 ± 9.2 (range 27–69) in AP-UKA patients (p = 0.032). At 5 years, it was 52.4 ± 8.3 (range 26–66) and 48.2 ± 8.3 (range 24–59), respectively (p < 0.001).
The FJS-12 score at 5 years was 82.9 ± 18.8 (range 42–100) in MB-UKA subjects and 73.4 ± 22.5 (range 32–100) in AP-UKA subjects (p = 0.015).
Tibial pain at 5 years was reported by 7.8% of MB-UKA and 35.1% of AP-UKA patients (p < 0.001).
Satisfaction at 5 years was 9.2 ± 0.8 (range 8–10) in MB-UKA patients and 8.3 ± 2.0 (range 4–10) in AP-UKA patients (p < 0.003).
Static postural sway, mobility, and gait symmetry
Static postural sway at 5 years was 3.9 ± 2.1 cm (range 0.60–10.30) in the MB-UKA group and 5.4 ± 2.3 cm (range 1.1–10.5) in the AP-UKA group (p = 0.0002) (Table 3).
Gait symmetry at 5 years was 92.7% ± 3.7 (range 86.2–100) in MB-UKA and 90.4% ± 5.4 (range 79.3–99.9) in AP-UKA patients (p = 0.006).
Discussion
The main finding of this study was that patients who underwent UKA with an MB component reported better static postural sway and gait symmetry at 5 years than those who underwent UKA with an AP component.
At the same time point, the AP patients also reported a significantly higher prevalence of tibial pain; they had significantly worse FJS-12 and PCS scores and were significantly less satisfied with their outcome. There were no other significant differences in the functional measures analyzed.
To the best of our knowledge, this is the first study to use a motion analysis system to compare the functional outcomes of UKA patients implanted with different tibial components.
Novel motion measurement systems that are developed to provide an objective description and quantitative assessment of patient motor functions and abilities always require validation. Several IMU-based techniques have been devised to track lower-limb joint movement, but only a few have been compared to stereophotogrammetry, the gold standard. The sensitivity and accuracy of the Riablo™ system, used in this study, have been validated by Leardini and co-workers [35]. In particular, the authors compared knee and chest angular measurements with the corresponding gait measures. They demonstrated that the IMU-based Riablo™ system makes minimal errors when measuring joint rotations, even in self-worn conditions. The authors concluded that the system is suitable for use in routine lower-limb joint rehabilitation, in patients who have received orthopedic treatment, and in those recovering from injury. The device has also been used as an aid to improve conventional rehabilitation in patients with neurological conditions [60, 61].
The advantages of these devices include cost-effectiveness compared to gait analysis equipment, a compact size and light weight, and the elimination of constraints related to the testing environment, extending it beyond the confines of the laboratory [34].
Wearable inertial devices for human motion analysis find widespread application in several areas. These include gait analysis (which is further subdivided into upright gait stability or dynamic balance assessment, measurement of spatio-temporal variables of gait, and evaluation of lower limb joint kinematics during gait); stabilometry (focusing on static balance assessment); instrumented clinical tests; assessment of upper-body mobility; monitoring of daily life activities; and evaluation of tremors [33].
At 5 years, the groups showed significantly different FJS-12 scores. The higher scores of the MB-UKA patients were comparable to those published by Longo et al. [62]. The lower FJS-12 scores of the AP-UKA patients may be related to the higher incidence of tibial pain in this group, possibly as a consequence of the greater proximal tibial strain, which has also been demonstrated in those patients compared to MB-UKA patients in a biomechanical study [63].
The finding that well-aligned AP-UKA implants involved greater bone deformation than misaligned MB-UKA implants [22] suggests that greater tibial bone strain and microdamage may contribute to component loosening [64] or unexplained pain [23], which may be the cause of the lower satisfaction and FJS-12 and PCS scores of our AP group. Clearly, pain could also affect the gait patterns and the ability to stand upright for a prolonged period, as shown by Riablo™ analysis.
Several studies have measured the postoperative functional scores of MB-UKA and AP-UKA patients.
Koh and colleagues found no significant differences in clinical and radiological outcomes at 2 years, including the Knee Society Score (KSS) and the Western Ontario McMaster University Osteoarthritis Index (WOMAC) scores [14].
In addition, a randomized study by Hutt et al. reported no differences in the Knee Osteoarthritis Outcome Score (KOOS) at a mean follow-up of 6.4 years [16].
We also failed to find significant differences in the KSKSs, the KSFSs, and the OKS and MCS scores, of which the latter measures HRQL (SF-36 score).
This finding contrasts with a retrospective study by Scott and co-workers, who reported no significant differences in SF-12 and PCS scores between 173 MB and 82 AP patients at 5 years [24]. Another study found better KSSs and KOOSs and lower pain in MB-UKA than in AP-UKA patients at a follow-up of more than 10 years as well as no significant differences in knee range of motion [65]. Lee et al., employing PSM, did not report any statistically significant differences between MB-UKA and AP-UKA patients in terms of outcomes, quality of life, or 10-year implant survival [27].
The main strength of our study is that all procedures were performed by highly experienced surgeons working at a specialized, high-volume knee prosthetic surgery center. All patients followed identical preoperative protocols, underwent the same implantation procedure, and followed a standardized rehabilitation protocol. The meticulous application of stringent inclusion and exclusion criteria, ensuring a highly homogeneous patient cohort, and the application of PSM, which—though yielding a limited number of patient pairs—effectively minimized confounding factors, are additional strengths.
The study’s limitations include, first of all, its retrospective design, since PSM minimized but clearly could not rule out selection bias. Patient number and follow-up duration are also limited.
Our findings demonstrate by movement analysis that MB-UKA provides greater stability and gait symmetry, even though both tibial components ensure good functional outcomes. Further studies are needed to establish which component provides better clinical results in the short, medium, and long term.
Conclusions
At 5-year follow-up the static sway and gait symmetry demonstrated significant differences in between fixed-bearing AP and MB tibial components. Despite nearly overlapping functional outcomes, the MB-UKA group suffered less tibial pain, had better FJS-12 and PCS scores, and was more satisfied than the AP-UKA group.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- mUKA:
-
Medial unicompartmental knee arthroplasty
- MB:
-
Metal-backed
- AP:
-
All-polyethylene
- PROMs:
-
Patient-reported outcome measures
- PSM:
-
Propensity score matching
- PCS:
-
Physical component summary
- FJS-12:
-
Forgotten Joint Score-12
- NRS:
-
Numeric Rating Scale
- KOA:
-
Osteoarthritis of the knee
- UKA:
-
Unicompartmental knee arthroplasty
- TKA:
-
Total knee arthroplasty
- IMU:
-
Inertial measurement unit
- HRQL:
-
Health-related quality of life
- BMI:
-
Body mass index
- ASA:
-
American Society of Anesthesiologists
- KSFS:
-
Knee Society Function Score
- KSKS:
-
Knee Society Knee Score
- OKS:
-
Oxford Knee Society
- MCS:
-
Mental component summary
- SF:
-
Short Form
- SMD:
-
Standardized mean difference
- SD:
-
Standard deviation
- KSS:
-
Knee Society Score
- WOMAC:
-
Western Ontario McMaster University Osteoarthritis Index
- KOOS:
-
Knee Osteoarthritis Outcome Score
References
Bindawas SM, Vennu V, Auais M (2015) Health-related quality of life in older adults with bilateral knee pain and back pain: data from the Osteoarthritis Initiative. Rheumatol Int 35:2095–2101
Hooper G, Lee A, Rothwell A, Frampton C (2014) Current trends and projections in the utilisation rates of hip and knee replacement in New Zealand from 2001 to 2026. N Z Med J 127:82–93
Piovan G, Screpis D, Natali S, Iacono V, Baldini M, Farinelli L et al (2022) Simultaneous bilateral total knee arthroplasty in elderly: are there factors that can influence safety and clinical outcome? Adv Orthop. https://doi.org/10.1155/2022/1989822
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg 89:780–785
Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW (2012) Unicompartmental versus total knee arthroplasty database analysis. Clin Orthop Relat Res 470(1):84–90
Noticewala MS, Geller JA, Lee JH, Macaulay W (2012) Unicompartmental knee arthroplasty relieves pain and improves function more than total knee arthroplasty. J Arthroplasty 27(8):99–105
Witjes S, Gouttebarge V, Kuijer PPFM, van Geenen RCI, Poolman RW, Kerkhoffs GMMJ (2016) Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med. https://doi.org/10.1007/s40279-015-0421-9
De Berardinis L, Senarighi M, Ciccullo C, Forte F, Spezia M, Gigante AP (2022) Fast-track surgery and telerehabilitation protocol in unicompartmental knee arthroplasty leads to superior outcomes when compared with the standard protocol: a propensity-matched pilot study. Knee Surg Relat Res. https://doi.org/10.1186/s43019-022-00173-z
Mercurio M, Gasparini G, Familiari F, Castioni D, Galasso O (2022) Outcomes of bi-unicompartmental versus total knee arthroplasty for the treatment of medial and lateral knee osteoarthritis: a systematic review and meta-analysis of comparative studies. Indian J Orthop. 56(6):963–972
Wu LP, Mayr HO, Zhang X, Huang YQ, Chen YZ, Li YM (2022) Knee scores of patients with non-lateral compartmental knee osteoarthritis undergoing mobile, fixed-bearing unicompartmental knee and total knee arthroplasties: a randomized controlled trial. Orthop Surg 14:73–87
Xi G, Wang HH, Li H, Zhang M (2022) Short-term outcomes of Oxford unicompartmental knee arthroplasty with coronal subluxation of the knee: a retrospective case–control study. J Orthop Traumatol. https://doi.org/10.1186/s10195-022-00626-x
van der List JP, McDonald LS, Pearle AD (2015) Systematic review of medial versus lateral survivorship in unicompartmental knee arthroplasty. Knee. https://doi.org/10.1016/j.knee.2015.09.011
D’Amario F, De Berardinis L, Zanon G, Qordja F, Vitale U, Gigante AP (2024) First Italian experience with the Oxinium metal-backed fixed-bearing medial Journey II unicompartmental knee system: promising short-term outcomes of 145 cases. J Clin Med. https://doi.org/10.3390/jcm13051303
Koh IJ, Suhl KH, Kim MW, Kim MS, Choi KY, In Y (2017) Use of all-polyethylene tibial components in unicompartmental knee arthroplasty increases the risk of early failure. J Knee Surg 30:807–815
Gioe TJ, Bowman KR (2000) A randomized comparison of all-polyethylene and metal-backed tibial components. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-200011000-00015
Hutt JRB, Farhadnia P, Massé V, Lavigne M, Vendittoli P-A (2015) A randomised trial of all-polyethylene and metal-backed tibial components in unicompartmental arthroplasty of the knee. Bone Jt J 97(6):786–792
Nouta KA, Verra WC, Pijls BG, Schoones JW, Nelissen RGHH (2012) All-polyethylene tibial components are equal to metal-backed components: Systematic review and meta-regression. Clin Orthop Relat Res. https://doi.org/10.1007/s11999-012-2582-2
Rouanet T, Combes A, Migaud H, Pasquier G (2013) Do bone loss and reconstruction procedures differ at revision of cemented unicompartmental knee prostheses according to the use of metal-back or all-polyethylene tibial component? Orthop Traumatol Surg Res 99:687–692
Small SR, Berend ME, Ritter MA, Buckley CA, Rogge RD (2011) Metal backing significantly decreases tibial strains in a medial unicompartmental knee arthroplasty model. J Arthroplasty 26:777–782
Heyse TJ, Khefacha A, Peersman G, Cartier P (2012) Survivorship of UKA in the middle-aged. Knee 19(5):585–591. https://doi.org/10.1016/j.knee.2011.09.002
Scott CEH, Eaton MJ, Nutton RW, Wade FA, Evans SL, Pankaj P (2017) Metal-backed versus all-polyethylene unicompartmental knee arthroplasty: Proximal tibial strain in an experimentally validated finite element model. Bone Joint Res 6(1):22–30. https://doi.org/10.1302/2046-3758.61.BJR-2016-0142.R1
Danese I, Pankaj P, Scott CEH (2019) The effect of malalignment on proximal tibial strain in fixed-bearing unicompartmental knee arthroplasty: a comparison between metal-backed and all-polyethylene components using a validated finite element model. Bone Jt Res 8:55
Simpson DJ, Price AJ, Gulati A, Murray DW, Gill HS (2009) Elevated proximal tibial strains following unicompartmental knee replacement—a possible cause of pain. Med Eng Phys 31:752–757
Scott CEH, Wade FA, Bhattacharya R, MacDonald D, Pankaj P, Nutton RW (2016) Changes in bone density in metal-backed and all-polyethylene medial unicompartmental knee arthroplasty. J Arthroplasty 31:702–709
van der List JP, Kleeblad LJ, Zuiderbaan HA, Pearle AD (2017) Mid-term outcomes of metal-backed unicompartmental knee arthroplasty show superiority to all-polyethylene unicompartmental and total knee arthroplasty. HSS J 13:232–240
Valentini R, De Fabrizio G, Piovan G, Stasi A (2014) Unicondylar knee prosthesis: our experience. Acta Biomed 85:91–96
Lee M, Cheng D, Chen J, Liow L, Lo NN, Yeo SJ (2021) No difference in functional outcomes, quality of life and survivorship between metal-backed and all-polyethylene tibial components in unicompartmental knee arthroplasty: a 10-year follow-up study. Knee Surg Sports Traumatol Arthrosc 29:3368–3374
Costa GG, Lo Presti M, Grassi A, Agrò G, Cialdella S, Mosca M et al (2020) Metal-backed tibial components do not reduce risk of early aseptic loosening in unicompartmental knee arthroplasty: a systematic review and meta-analysis. J Knee Surg 33:180–189
Perry J, Burnfield JM, Cabico LM (2010) Gait analysis: normal and pathological function. Slack Inc., West Deptford
Cappozzo A, Della Croce U, Leardini A, Chiari L (2005) Human movement analysis using stereophotogrammetry. Part 1: theoretical background. Gait Posture. https://doi.org/10.1016/j.gaitpost.2004.01.010
Lanotte F, Shin S, O’Brien M, Jayaraman A (2023) Validity and reliability of a commercial wearable sensor system for measuring spatiotemporal gait parameters in a post-stroke population: the effects of walking speed and asymmetry. Physiol Meas. https://doi.org/10.1088/1361-6579/aceecf
Kirtley C (2006) Clinical gait analysis: theory and practice. Churchill Livingstone, Oxford
Iosa M, Picerno P, Paolucci S, Morone G (2016) Wearable inertial sensors for human movement analysis. Expert Rev Med Devices. https://doi.org/10.1080/17434440.2016.1198694
Kavanagh JJ, Menz HB (2008) Accelerometry: A technique for quantifying movement patterns during walking. Gait Posture. https://doi.org/10.1016/j.gaitpost.2007.10.010
Leardini A, Lullini G, Giannini S, Berti L, Ortolani M, Caravaggi P (2014) Validation of the angular measurements of a new inertial-measurement-unit based rehabilitation system: comparison with state-of-the-art gait analysis. J Neuroeng Rehabil. https://doi.org/10.1186/1743-0003-11-136
Rodríguez-Merchán EC, Gómez-Cardero P (2018) Unicompartmental knee arthroplasty: current indications, technical issues and results. EFORT Open Rev 3:363–373
Kozinn S, Scott R (1989) Unicondylar knee arthroplasty. J Bone Joint Surg Am 71:145–150
Ahlbäck S (1968) Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 277:7–72
Lee M, Huang Y, Chong HC, Ning Y, Lo NN, Yeo SJ (2016) Predicting satisfaction for unicompartmental knee arthroplasty patients in an Asian population. J Arthroplasty 31:1706–1710
Insall J, Dorr L, Scott R, Scott W (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br 80:63–69
Luger M, Schopper C, Krottenthaler ES, Mahmoud M, Heyse T, Gotterbarm T et al (2023) Not all questions are created equal: the weight of the Oxford Knee Scores questions in a multicentric validation study. J Orthop Traumatol. https://doi.org/10.1186/s10195-023-00722-6
Ware JJ, Sherbourne C (1992) The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med Care. https://doi.org/10.1097/00005650-199206000-00002
Sansone V, Fennema P, Applefield RC, Marchina S, Ronco R, Pascale W et al (2020) Translation, cross-cultural adaptation, and validation of the Italian language Forgotten Joint Score-12 (FJS-12) as an outcome measure for total knee arthroplasty in an Italian population. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-019-2985-2
Podsiadlo JD, Richardson S(1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x
Csuka M, Mccarty DJ (1985) Simple method for measurement of lower extremity muscle strength. Am J Med. https://doi.org/10.1016/0002-9343(85)90465-6
Hess R, Brach J, Piva S, VanSwearingen J (2010) Walking skill can be assessed in older adults: validity of the Figure-of-8 Walk Test. Phys Ther 90:89–99
Berg K, Wood-Dauphinée S, Williams JI, Gayton D (1989) Measuring balance in the elderly: preliminary development of an instrument. Physiother Can 41:304–311
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46:399–424
Plantz MA, Sherman AE, Kadakia AR (2020) A propensity score-matched analysis comparing outpatient and short-stay hospitalization to standard inpatient hospitalization following total ankle arthroplasty. J Orthop Surg Res. https://doi.org/10.1186/s13018-020-01793-5
Matsunaga-Myoji Y, Fujita K, Tabuchi Y, Mawatari M (2023) Propensity score-matched comparison of physical activity and quality of life between revision total hip arthroplasty and primary total hip arthroplasty. J Orthop 40:23–28
Domb BG, Bheem R, Monahan PF, Rosinsky PJ, Maldonado DR, Meghpara MB et al (2021) Minimum five-year outcomes of hip resurfacing: propensity-score matched against total hip arthroplasty control groups. J Arthroplasty 36:2012–2015
Yeung MHY, Fu H, Cheung A, Kwan VCW, Cheung MH, Chan PK et al (2023) Robotic arm-assisted unicondylar knee arthroplasty resulted in superior radiological accuracy: a propensity score-matched analysis. Arthroplasty. https://doi.org/10.1186/s42836-023-00210-6
Yoo JD, Huh MH, Shin YS (2023) Risk of revision in UKA versus HTO: a nationwide propensity score-matched study. Arch Orthop Trauma Surg 143:3457–3469
Yamamoto K, Nakajima A, Sonobe M, Akatsu Y, Yamada M, Nakagawa K (2023) A comparative study of clinical outcomes between cruciate-retaining and posterior-stabilized total knee arthroplasty: a propensity score-matched cohort study. Cureus. https://doi.org/10.7759/cureus.45775
Harada S, Hamai S, Shiomoto K, Hara D, Fujii M, Ikemura S et al (2021) Patient-reported outcomes after primary or revision total hip arthroplasty: a propensity score-matched Asian cohort study. PLoS ONE. https://doi.org/10.1371/journal.pone.0252112
De Berardinis L, Senarighi M, Farinelli L, Qordja F, Gallo A, Spezia M et al (2023) In primary total hip arthroplasty, the direct anterior approach leads to higher levels of creatine kinase and lower levels of C-reactive protein compared to the posterolateral approach: a propensity score matching analysis of short-term follow-up data. J Orthop Surg Res. https://doi.org/10.1186/s13018-023-04084-x
Rosenbaum PR (1989) Optimal matching for observational studies source. J Am Stat Assoc. https://doi.org/10.2307/2290079
Austin PC (2009) Some methods of propensity-score matching had superior performance to others: results of an empirical investigation and Monte Carlo simulations. Biom J 51:171–184
Ghoshchi SG, De Angelis S, Morone G, Panigazzi M, Persechino B, Tramontano M et al (2020) Return to work and quality of life after stroke in Italy: a study on the efficacy of technologically assisted neurorehabilitation. Int J Environ Res Public Health 17:1–12
Lupo A, Cinnera A, Pucello A, Iosa M, Coiro P, Personeni S et al (2018) Effects on balance skills and patient compliance of biofeedback training with inertial measurement units and exergaming in subacute stroke: a pilot randomized controlled trial. Funct Neurol 33:131–136
Longo UG, De Salvatore S, Candela V, Berton A, Casciaro C, Sciotti G et al (2021) Unicompartmental knee arthroplasty: minimal important difference and patient acceptable symptom state for the forgotten joint score. Medicina (Lithuania). https://doi.org/10.3390/medicina57040324
Scott CEH, Eaton MJ, Nutton RW, Wade FA, Pankaj P, Evans SL et al (2013) Proximal tibial strain in medial unicompartmental knee replacements. Biomech Study Implant Des. https://doi.org/10.1302/0301-620X.95B10.31644
Bruni D, Akkawi I, Iacono F, Raspugli GF, Gagliardi M, Nitri M et al (2013) Minimum thickness of all-poly tibial component unicompartmental knee arthroplasty in patients younger than 60 years does not increase revision rate for aseptic loosening. Knee Surg Sports Traumatol Arthrosc 21:2462–2467
Sessa V, Celentano U (2021) Unicompartmental knee arthroplasty: all-poly versus metal-backed tibial component—a long-term follow-up study. Int Orthop 45:3063–3068
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization, CZ, GP, and LDB; methodology, LDB, GP, and MS; validation, DS, APG, and SN; formal analysis, LP, DS, and APG; writing—original draft preparation, LDB, MS, and GP; writing—review and editing, APG, LP, and CZ; supervision, CZ. The author(s) read and approved the final manuscript. All authors have given final approval of the version to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Verona and Rovigo—Italy. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Piovan, G., De Berardinis, L., Screpis, D. et al. Metal-backed or all-poly tibial components: which are better for medial unicompartmental knee arthroplasty? A propensity-score-matching retrospective study at the 5-year follow-up. J Orthop Traumatol 25, 24 (2024). https://doi.org/10.1186/s10195-024-00765-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-024-00765-3