Abstract
Background
Fixed severe hyperkyphotic deformities spread over more than five vertebral levels represent a therapeutic challenge, especially when the deformity apex is located at the thoraco-lumbar junction, thus requiring a huge amount of correction. The aim of this article is to describe an innovative all-posterior corrective technique based on multilevel non-contiguous thoracic pedicle subtraction ostoeotomy (PSO).
Materials and methods
A retrospective review of three patients with fixed severe thoracic hyperkyphosis (a deformity angle of over 70°) with a thoraco-lumbar apex (between T11 and L1) treated by simultaneous two-level thoracic PSO and thoraco-lumbar posterior fusion was performed. Radiographic and clinical records were evaluated pre-operatively, post-operatively and at last follow-up (after a minimum of 2 years). Each variable was presented as mean ± SD (standard deviation). Statistical analyses were performed using paired t-tests (P value < 0.05 was considered significant).
Results
The mean local deformity angle decreased by 75% (from 81.3° ± 2.1° to 20.7° ± 1.4°, p < 0.001), the post-operative thoracic kyphosis decreased by 46% (from 61.4° ± 2.4° to 33.2° ± 0.9°, p < 0.001) and the sagittal vertical axis decreased by 73% (from 14.7 cm ± 0.8 cm to 3.9 cm ± 0.3 cm, p < 0.001). No differences were observed in the radiological results between post-operative values and those at the final follow-up. The average Oswestry Disability Index (ODI) score reduced from 65.7 ± 1.8 pre-operatively to 17.3 ± 1.7 at last follow-up (p < 0.001). No neurological, mechanical nor infective complication occurred.
Conclusions
The presented technique, although technically demanding, proved to be a safe and effective alternative for the management of fixed severe thoraco-lumbar junction hyperkyphotic deformities.
Level of evidence: IV
TRIAL REGISTRATION Retrospectively registered
Similar content being viewed by others
Introduction
Fixed severe hyperkyphotic deformities spread over more than five vertebral levels are complex to treat due to the amount of correction required, which varies depending upon the angular value and the localization of the apex of the deformity. The most challenging situation is when the apex of the kyphosis is located at the thoraco-lumbar junction because the maximal correction is required at this site [1].
In the presence of severe deformities, the huge amount of angular correction, over 70°, that is needed remains complex to obtain, even by performing aggressive tricolumnar osteotomies [2]. Pedicle subtraction osteotomy (PSO) and bone disc bone osteotomy (BDBO) are capable of guaranteeing maximal angular corrections of 35° and 55°, respectively [3]. Vertebral column resection (VCR) represents the most powerful spinal osteotomy; it allows tremendous corrective angles but encompasses a high rate of neurological and mechanical complications and should therefore be reserved for biplanar severe fixed deformities in which the spine must not only be shortened but also translated [4].
The authors have therefore speculated that the treatment of these severe deformities should be accomplished by means of two simultaneous PSOs performed non-contiguously, permitting adequate corrective potential alongside excellent intraoperative control and healing potential of the osteotomy sites, thus resulting in a low rate of neurological and mechanical complications.
The aim of this article is to describe a posterior one-stage technique based on multilevel non-contiguous thoracic PSO for severe (a deformity angle of over 70°) fixed rounded kyphotic deformities at the thoraco-lumbar junction, including the correction and complication rates at a minimum of 2 years’ follow-up in three adult patients.
Materials and methods
Study sample
A retrospective review of patients over 18 years old with fixed severe thoracic hyperkyphosis (a deformity angle of over 70°) with a thoraco-lumbar apex (between T11 and L1) treated by simultaneous two-level thoracic PSO and thoraco-lumbar posterior fusion was performed. Follow-up evaluations were performed post-operatively, at 12 months and up to the final follow-up at 28.7 ± 2.5 months.
Informed consents for participation in the study and for the publication of clinical images were obtained from each patient.
Data collection
Included patients were all affected by severe fixed thoracic hyperkyphosis with a thoraco-lumbar apex (between T11 and L1). Anterior bony fusion at the apex of the deformity was present in each case and documented by pre-operative CT scan. Fulcrum supine radiographs were taken in all cases to confirm the irreducibility of the deformity.
Patient demographics, the aetiology of the deformity and data on prior surgical treatments were collected by reviewing the medical records.
Operative time, blood loss, length of stay, and intra- and post-operative complications were recorded.
The deformity angle (used to evaluate the local spinal kyphosis angle, defined as the Cobb angle from the upper endplate of the proximal junctional normal vertebra to the lower endplate of the distal junctional normal vertebra) and the T1–T12 thoracic kyphosis (TK) and L1–S1 lumbar lordosis (LL) angles were measured on pre- and post-operative full-length standing radiographs. The C7 plumbline (C7PL)/central sacral vertical line (CSVL) and sagittal vertical axis (SVA) were used to assess coronal and sagittal imbalance. The pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), PI–LL mismatch (PI-LL) and GAP score [5] were used to evaluate the spinopelvic balance.
The sagittal deformity angular ratio (S-DAR) [6] was used pre-operatively to evaluate the radius of curvature of the deformity, and was calculated by dividing the deformity angle by the number of vertebral bodies in the deformed area.
Osteotomy healing was assessed in all cases with a CT scan performed at the 1-year follow-up evaluation.
The Oswestry Disability Index (ODI) was administered pre-operatively and at last follow-up.
Surgical planning and technique
Surgery was planned based on pre-operative full standing antero-posterior and lateral X-rays of the entire column and on CT scan; these guided the decision regarding the location of the osteotomies and the desired corrective angle, the fusion area, and eventually the need to obtain patient-specific guides for screw insertion.
The first osteotomy was always planned at the apex of the deformity, while the second was always planned at three levels above in order to maintain at least three pairs of screws between the two osteotomies. The degree of correction for each osteotomy was accurately measured on the 3D CT scan reconstruction.
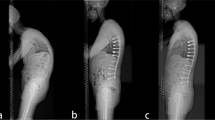
Regarding the fusion area, the lower instrumented vertebra (LIV) was the sagittal stable vertebra according to the definition by Cho et al. [7]. The fusion was eventually extended distally in the presence of documented disc degeneration at the level below the planned LIV (Fig. 1). The upper instrumented vertebra was T3 in all cases.
In the presence of an altered posterior anatomy (related to previous surgeries) with the presence of posterior spinal fusion mass, customized guides (Myspine, Medacta International SA, Castel San Pietro, Switzerland) for the placement pedicle screws were developed (Fig. 2); otherwise, the freehand technique was used.
The patient was placed prone on an Allen table; neurophysiologic monitoring with somatosensory-evoked potentials and trans-cranial motor-evoked potentials was used in all cases. After a standard posterior midline approach with longitudinal skin incision, careful subperiosteal exposure of the spinous processes and laminae was performed; when customized guides were used (in two cases), care was taken not to remove bone to avoid altering the contact points of the guides. Each guide was then placed on the corresponding vertebra and firmly held; then, after checking the contact surfaces, lateral and contralateral awls were used to prepare the entry point, and a 2.5 mm drill was used to prepare the pathway for the screws in the pedicle [8]. Finally, after tapping, polyaxial screws of an appropriate length and diameter were inserted according to the planned model. When customized guides were not needed (in one case), a freehand technique was used [9].
Screws were placed at all levels, except for those in planned osteotomies. The screw position was checked with a fluoroscope.
Then, the first thoracic PSO was performed as planned, at the apex of the deformity (T12 in two cases, T11 in one case). Laminectomy was performed at the level of the osteotomy and at the adjacent levels, one above and one below, to prevent buckling of the spinal cord during the correction manoeuvre; the pedicles were visualized and drilled to maintain orientation. The ribs at the level of the osteotomy were carefully exposed (3–4 cm) and removed, disarticulating the costotransverse joints bilaterally (Fig. 3). The bone was all saved for later fusion. Then, careful dissection of the lateral vertebral body wall was carried out bilaterally.
After positioning dural retractors to optimize the visualization of the vertebral body, two osteotomes were positioned superior and inferior with respect to the pedicle, and the desired osteotomy angle was checked under fluoroscope guidance (Fig. 4). A temporary rod was placed on the opposite side to the first surgeon to prevent sudden collapsing of the spine and possible translation while completing the osteotomy. Then, lateral vertebral body wall cuts were made with straight osteotomes in a precise wedge according to the desired degree of closure.
The apex of the wedge was at the cortical anterior vertebral body wall, which was carefully violated with a sharp osteotome to obtain the desired corrective angle. The bony wedge was then removed. The same procedure was performed on the opposite side. Thoracic roots were preserved in all cases. All soft tissues and osseous elements were carefully removed from the anterior portion of the dura to prevent any compression of the neural elements anteriorly during osteotomy closure (Fig. 5).
PSO closure was then performed by gentle compression across temporary rods and by adjusting the Allen bed frame to reduce the kyphosis.
The same procedure was repeated on the other thoracic vertebra (T8 in two cases, T7 in one case) to achieve proper correction of the deformity (Figs. 6, 7).
Then, the temporary rods on the right side were removed and gently replaced with a pre-bent 5.5 mm titanium rod; the same procedure was performed on the left side. After placing the definitive rods (Fig. 8), segmentary compression was applied to the screws and rods to achieve bone-to-bone closure.
Careful decortication of the posterior spinal elements of the instrumented vertebrae was followed by apposition of allograft bone. A subfascial (Fig. 9) drain was placed and a standard suture was performed.
Early mobilization out of bed started on post-operative day 1. For the first 12 weeks after surgery, a thoracic lumbar sacral orthosis (TLSO) to restrict spinal movements and facilitate initial bone graft fusion was prescribed.
Patient characteristics
Three patients (two females and one male) were included. The average age was 42.6 (range 30–52) years. Patient characteristics are summarized in Table 1. According to PI, the Roussouly morphotype of all patients was 4 [10].
Statistical analysis
Each variable was presented as mean ± SD (standard deviation). Statistical analyses were performed using paired t-tests (SPSS version 17.0). Normality was assumed, and a P value < 0.05 was considered significant.
Results
The mean operating time was 305 ± 56 min, and the mean blood loss was 1982 ± 976 ml. Intra-operatively, the surgical planning regarding the fusion area was respected in all the cases; there was no need to extend the instrumentation proximally or distally due to the pulling out of screws during a corrective manoeuvre at the most cephalad and caudal levels. Intra-operatively, an accidental durotomy was observed in one case during the laminectomy at the T12 level, with a transient reduction of somatosensory-evoked potentials and trans-cranial motor-evoked potentials in both lower limbs. The dural lesion was sutured and sealed with fibrin glue. Somatosensory-evoked potentials and trans-cranial motor-evoked potentials spontaneously returned to baseline values in approximately 25 min with the administration of steroids and blood products, and the procedure was completed. No reduction in somatosensory- and motor-evoked potentials was observed during osteotomy closure in any of the cases. All the patients were neurologically intact after surgery. Patients were discharged after an average length of stay of 9.7 ± 3.1 days. Significant results were achieved in the sagittal plane (Table 2). In detail, the mean local deformity angle decreased by 75% (from 81.3° ± 2.1° to 20.7° ± 1.4°, p < 0.001), the post-operative TK decreased by 46% (from 61.4° ± 2.4° to 33.2° ± 0.9°, p < 0.01) and the sagittal vertical axis decreased by 73% (from 14.7 cm ± 0.8 cm to 3.9 cm ± 0.3 cm, p < 0.01). No significant change was noted in spinopelvic parameters; however, the GAP score showed a significant improvement (from 10.7 ± 1.5 to 7.3 ± 1.5, p < 0.05).
The average C7PL/CSVL remained at a physiological value of 1.4 cm ± 0.2 cm; there was no difference with respect to the pre-operative value (n.s.).
No differences were observed in the radiological results between post-operative values and those obtained at final follow-up.
The average Oswestry Disability Index (ODI) score reduced from 65.7 ± 1.8 pre-operatively to 17.3 ± 1.7 at the last follow-up (p < 0.01).
At the 1-year FU, the CT scan showed complete healing of the osteotomies in all cases. No cases of infection, progression of the deformity, proximal or distal junction pathology, or pulling out of screws were recorded up to the final FU.
Discussion
The presented technique, although technically demanding, resulted in an acceptable average time and blood loss. These results were superior with respect to the main case series dealing with single-level PSO reported in the literature [11], but were equal or inferior to the rare case series available in the literature that deal with two-level PSO adopted for the treatment of anklylosing spondylitis, which involves a first PSO at the thoraco-lumbar junction (T12 or L1) and another one performed at the lumbar caudal level [12,13,14].
The technique proved to be really efficient at preventing intraoperative neurologic impairment, with no case showing a motor-evoked potential reduction during resections and during corrective manoeuvres with osteotomy closure. This finding is related, in the authors’ opinion, to some technical issues. First, planning the second osteotomy three levels above the deformity apex and adopting temporary rods permits three pairs of screws to be maintained between the two osteotomies, resulting in strong fixation without the risk of sagittal translation of the portion of the spine between the two osteotomies, which represents the major risk factor for neurological impairment in thoracic PSO [11, 15]. Secondarily, respecting the thoracic nerve roots, especially in the apical-level osteotomy (T11 and T12 in all four cases), lowers the risk of spinal cord ischaemia according to Lau et al. [16]. Finally, the adoption of a wide laminectomy at least one level above and one below the osteotomy site proved to be crucial in preventing spinal cord kinking and compression after bony resections and osteotomy closure.
The technique proved to be really efficient at reducing a deformity angle of up to 75%, thus re-establishing a physiological sagittal alignment, with a reduction of the SVA to within 5 cm in all the patients evaluated. This finding may be explained by the characteristics of the analysed cohort, in which the deformity apex was located at the thoraco-lumbar junction. This permits the first osteotomy to be performed at the T12 or T11 level, where the corrective potential of the thoracic PSO is maximal, and the second to be performed at the T7 or T8 level, where the corrective power remains remarkable [15]. The obtained correction rate is quite impressive and is in line with those reported by authors who performed more aggressive corrective procedures, such as vertebral column resection (VCR), which has, up to now, been considered the gold standard in the treatment of fixed kyphotic deformities for which the amount of correction required exceeds the correction capability of a single PSO [17,18,19,20,21,22]. Differently from the case series dealing with VCR [17,18,19,20,21,22], we did not observe any major complication in the presented case series.
The absence of significant changes in spinopelvic parameters can be explained by the fact that these patients had a thoraco-lumbar deformity (with a thoracic apex in all cases) and not a lumbosacral deformity. Therefore, the osteotomies and the corrective manoeuvres were performed with the aim to reduce the hyperkyphosis in the thoracic spine, and not to gain lordosis in the lumbosacral junction. Despite that, the GAP score showed a significant improvement, mainly because of the powerful reduction of the global sagittal imbalance that the technique made it possible to achieve.
Regarding the healing at osteotomy sites, the CT scan performed at the 1-year FU demonstrated excellent healing of all six osteotomies. This finding may be explained by the wide bony contact that is achieved with a PSO, unlike a VCR, in which an anterior cage or mesh is required to avoid spinal cord kneeling, thus lowering the biological healing potential of the spine [17,18,19,20,21,22]. Another explanation for the excellent healing potential of the presented technique is the presence of the rib cage in the thoracic tract. Yang et al. [23] found that thoracic PSOs had a lower non-union rate, resulting in fewer late mechanical complications compared to lumbar PSOs, which was assumed to be because the greater motion of lumbar vertebrae compared to thoracic vertebrae—which are additionally sustained by the rigid rib cage—may contribute to an increased rate of pseudarthrosis and rod rupture in the lumbar spine.
The adoption of simultaneous double PSOs has rarely been described in the literature. Obeid et al. [24] reported the adoption of two adjacent apical PSOs in a single session with a modification to the standard PSO technique, represented by the resection of the discs above each osteotomized vertebra, for the treatment of a thoraco-lumbar fixed severe kyphotic deformity. The described technique, although fascinating, may be related in the authors’ opinion to a high risk of pseudarthrosis at the osteotomy sites, and presents the drawback of not being appliable in cases in which the anterior annulus is calcified or ossified. Most of the case series dealing with simultaneous PSOs refer to patients affected by ankylosing spondylitis treated with two lumbar PSOs or with a lumbar and a thoracic PSO, with excellent correction rates and the avoidance of major complications [12,13,14]. The adoption of a double simultaneous thoracic PSO has been reported by Lau et al. [16] and O'Shaughnessy [15], but their case series were extremely heterogeneous in terms of patients and deformity characteristics. The case series presented here does not come without limitations. First, its small sample size and the retrospective nature of the study are clear limitations. Secondly, it deals with a heterogeneous cohort of patients in terms of the aetiology of the deformity (congenital and iatrogenic).
In conclusion, although technically demanding, simultaneous two-level non-contiguous thoracic pedicle subtraction osteotomy is a powerful technique which, with its high corrective potential in the sagittal plane alongside its very low complication rate, may be particularly suitable for the treatment of fixed severe hyperkyphosis in adults with the apex located at the thoraco-lumbar junction.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Change history
22 December 2022
A Correction to this paper has been published: https://doi.org/10.1186/s10195-022-00679-y
References
Macagno AE, O’Brien MF (2006) Thoracic and thoracolumbar kyphosis in adults. Spine (Phila Pa 1976). https://doi.org/10.1097/01.brs.0000236909.26123.f8
Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P, Ames C, Smith JS, Shaffrey CI, Glassman S, Farcy JP, Lafage V (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery. https://doi.org/10.1227/NEU.0000000000000182o
Kose KC, Bozduman O, Yenigul AE, Igrek S (2017) Spinal osteotomies: indications, limits and pitfalls. EFORT Open Rev 2:73–82. https://doi.org/10.1302/2058-5241.2.160069
Lenke LG, Newton PO, Sucato DJ, Shufflebarger HL, Emans JB, Sponseller PD, Shah SA, Sides BA, Blanke KM (2013) Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0b013e318269fab1
Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstück F, Pérez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A (2017) Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Jt Surg Am 99:1661–1672. https://doi.org/10.2106/JBJS.16.01594
Bin Wang X, Lenke LG, Thuet E, Blanke K, Koester LA, Roth M (2016) Deformity angular ratio describes the severity of spinal deformity and predicts the risk of neurologic deficit in posterior vertebral column resection surgery. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000001547
Cho KJ, Lenke LG, Bridwell KH, Kamiya M, Sides B (2009) Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0b013e31819e28ed
Watanabe K, Lenke LG, Matsumoto M, Harimaya K, Kim YJ, Hensley M, Stobbs G, Toyama Y, Chiba K (2010) A novel pedicle channel classification describing osseous anatomy. Spine (Phila Pa 1976) 35:1836–1842. https://doi.org/10.1097/brs.0b013e3181d3cfde
Faldini C, Viroli G, Fiore M, Barile F, Manzetti M, Di Martino A, Ruffilli A (2021) Power-assisted pedicle screws placement: Is it as safe and as effective as manual technique? Narrative review of the literature and our technique. Musculoskelet Surg. https://doi.org/10.1007/s12306-021-00714-x
Sebaaly A, Gehrchen M, Silvestre C, Kharrat K, Bari TJ, Kreichati G, Rizkallah M, Roussouly P (2020) Mechanical complications in adult spinal deformity and the effect of restoring the spinal shapes according to the Roussouly classification: a multicentric study. Eur Spine J 29:904–913. https://doi.org/10.1007/s00586-019-06253-1
Xu H, Zhang Y, Zhao Y, Zhang X, Xiao S, Wang Y (2015) Radiologic and clinical outcomes comparison between single- and two-level pedicle subtraction osteotomies in correcting ankylosing spondylitis kyphosis. Spine J 15:290–297. https://doi.org/10.1016/j.spinee.2014.09.014
Zhong W, Chen Z, Zeng Y, Sun C, Li W, Qi Q, Guo Z (2019) Two-level osteotomy for the corrective surgery of severe kyphosis from ankylosing spondylitis: a retrospective series. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0000000000003095
Zhang HQ, Huang J, Guo CF, Liu SH, Tang MX (2014) Two-level pedicle subtraction osteotomy for severe thoracolumbar kyphotic deformity in ankylosing spondylitis. Eur Spine J 23:234–241. https://doi.org/10.1007/s00586-013-2867-5
Charles YP, Ntilikina Y, Collinet A, Steib JP (2020) Combined percutaneous and open instrumentation for thoracolumbar kyphosis correction by two-level pedicle subtraction osteotomy in ankylosing spondylitis. Eur J Orthop Surg Traumatol 30:939–947. https://doi.org/10.1007/s00590-020-02631-4
O’Shaughnessy BA, Kuklo TR, Hsieh PC, Yang BP, Koski TR, Ondra SL (2009) Thoracic pedicle subtraction osteotomy for fixed sagittal spinal deformity. Spine (Phila Pa 1976) 34:2893–2899. https://doi.org/10.1097/BRS.0b013e3181c40bf2
Lau D, Haddad AF, Fury MT, Deviren V, Ames CP (2021) Multilevel pedicle subtraction osteotomy for correction of severe rigid adult spinal deformities: a case series, indications, considerations, and literature review. Oper Neurosurg. https://doi.org/10.1093/ons/opaa430
Dalle Ore CL, Ames CP, Deviren V, Lau D (2018) Outcomes following single-stage posterior vertebral column resection for severe thoracic kyphosis. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.07.209
Saifi C, Laratta JL, Petridis P, Shillingford JN, Lehman RA, Lenke LG (2017) Vertebral column resection for rigid spinal deformity. Glob Spine J. https://doi.org/10.1177/2192568217699203
Cho W, Lenke LG, Blanke KM, O’Shaughnessy BA, Dorward IG, Koester LA, Sides BA, Baldus CR (2015) Predicting kyphosis correction during posterior-only vertebral column resection by the amount of spinal column shortening. Spine Deform. https://doi.org/10.1016/j.jspd.2014.06.006
Zhang XS, Zhang YG, Wang Z, Chen C, Wang Y (2010) Correction of severe post-traumatic kyphosis by posterior vertebra column resection. Chin Med J (Engl). https://doi.org/10.3760/cma.j.issn.0366-6999.2010.06.008
Wang Y, Zhang Y, Zhang X, Huang P, Xiao S, Wang Z, Liu Z, Liu B, Lu N, Mao K (2008) A single posterior approach for multilevel modified vertebral column resection in adults with severe rigid congenital kyphoscoliosis: a retrospective study of 13 cases. Eur Spine J. https://doi.org/10.1007/s00586-007-0566-9
Lenke LG, O’Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM (2009) Posterior vertebral column resection for severe pediatric deformity: Minimum two-year follow-up of thirty-five consecutive patients. Spine (Phila Pa 1976). https://doi.org/10.1097/BRS.0b013e3181b53cba
Yang BP, Ondra SL, Chen LA, Hee SJ, Koski TR, Salehi SA (2006) Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine 5:9–17. https://doi.org/10.3171/spi.2006.5.1.9
Obeid I, Boissière L, Vital JM, Bourghli A (2014) Osteotomy of the spine for multifocal deformities. Eur Spine J. https://doi.org/10.1007/s00586-014-3660-9
Acknowledgements
Not applicable.
Funding
No funding was received for this study by the National Institutes of Health (NIH), Wellcome Trust, Howard Hughes Medical Institute (HHMI), or others.
Author information
Authors and Affiliations
Contributions
CF and AR conceived the study and revised the paper; FB, GV and MM drafted the manuscript and collected and interpreted the data; FB, GV and GG participated in planning and revising the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval consent to participate
The study was approved by the institutional review board of our hospital (Ethics Committee of Area Vasta Emilia Centro, Regione Emilia-Romagna (CE-AVEC). All patients signed an informed consent on the use of their hospitalization data for scientific purposes.
Competing interests
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The given and the family names of the authors have been corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Faldini, C., Barile, F., Viroli, G. et al. Multilevel non-contiguous thoracic pedicle subtraction osteotomy for fixed rounded hyperkyphotic deformity of the thoraco-lumbar junction with anterior bony fusion: technical note. J Orthop Traumatol 23, 47 (2022). https://doi.org/10.1186/s10195-022-00665-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-022-00665-4