Abstract
Background
While growing evidence suggests a relationship between migraine and cardiovascular disease, the genetic evidence for a causal relationship between migraine and cardiovascular disease is still scarce. Investigating the causal association between migraine and cardiovascular disease is vital.
Methods
We carried out a bidirectional Mendelian randomization (MR) study including discovery samples and replication samples using publicly available genome-wide association study (GWAS) summary datasets and stringent screening instrumental variables. Four different MR techniques—Inverse variance weighted (IVW), MR ‒Egger, weighted median, and weighted mode—as well as various sensitivity analyses—Cochran’s Q, IVW radial, leave-one-out (LOO), and MR-PRESSO—were utilized to investigate the causal relationship between cardiovascular disease and migraine.
Results
The protective causal effects of genetically predicted migraine on coronary artery disease (OR, 0.881; 95% CI 0.790–0.982; p = 0.023) and ischemic stroke (OR, 0.912; 95% CI 0.854–0.974; p = 0.006) were detected in forward MR analysis but not in any other cardiovascular disease. Consistently, we also discovered protective causal effects of coronary atherosclerosis (OR, 0.865; 95% CI 0.797–0.940; p = 0.001) and myocardial infarction (OR, 0.798; 95% CI 0.668–0.952; p = 0.012) on migraine in reverse MR analysis.
Conclusion
We found a potential protective effect of migraine on coronary artery disease and ischemic stroke and a potential protective effect of coronary atherosclerosis and myocardial infarction on migraine. We emphasised epidemiological and genetic differences and the need for long-term safety monitoring of migraine medications and future research to improve cardiovascular outcomes in migraine patients.
Similar content being viewed by others
Introduction
Migraine, a prevalent and long-term condition, is generally identified by repeated incapacitating bouts of headaches along with other associated symptoms, including aura [1]. The typical clinical features of this neurological disorder include unilateral, throbbing headache attacks accompanied by nausea, vomiting, photophobia, and phonophobia [2]. It affects at least 1 billion people globally, posing a significant socioeconomic burden [3].
Co-morbidity between migraine and cardiovascular disease (CVD) are becoming increasingly common. As the leading cause of death worldwide and the cause of the highest mortality and disability globally, CVD has been posing an increasingly health and social burden as the world’s population aging [4]. The guidelines on preventing CVD issued by the European Society of Cardiology (ESC) in 2021 suggest that migraine with aura should be factored into the assessment of CVD risk [5].
Numerous cohort studies and meta-analyses have established correlations between migraine and various CVDs, including stroke, coronary artery disease (CAD), myocardial infarction (MI), atrial fibrillation (AF), and cardiovascular death [3, 6,7,8]. Although much progress has been made in preventing CVDs, the potential interactions with migraine remain unclear due to the complexity and diversity of factors contributing to CVDs. It might be implied by a positive causal association that the prevention of migraine could reduce CVD risk, and novel pathways and therapeutic targets for CVD risk reduction may be identified. In contrast, it might be inferred by an inverse causal association that CVD risk could be increased by therapeutics modifying migraine liability, such as anti-CGRP antibodies, CGRP (receptor) mAbs, and triptans [9,10,11]. Therefore, establishing causality between liability to migraine and CVD would have clinical significance. However, most of the previous studies were conducted at the individual level rather than at the summary level, which is susceptible to confounding factors.
Mendelian randomization (MR), a statistical method that uses exposure-related single nucleotide polymorphisms (SNPs) as instrumental variables, was utilized by neurologists and cardiologists to investigate the potential causal association between exposures and outcomes [12]. MR analysis, which is based on the principle of random assignment of alleles at meiosis, ensures that MR methods are independent of the external factors that confound observational epidemiological studies [13].
We utilized MR data from extensive genome-wide association studies (GWASs) of migraine [14,15,16] and CVD [17,18,19,20,21,22,23] to explore the potential causal association between migraine and CVD. Establishing the causal association between these factors and implementing preventive strategies may therefore emphasize the value of migraine patients being screened for CVD, which may offer fresh perspectives on cardiovascular disease treatment.
Methods
Study design
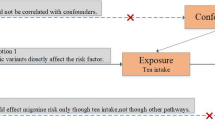
In this study, we conducted a bidirectional MR study to determine whether migraine and CVD are causally related. SNPs were utilized as instrumental variables (IVs) to estimate the causal effect of exposure on outcomes. In MR analysis, three key assumptions should be followed: 1). Exposure should strongly correlate with IVs; 2). There will be no correlation between IVs and any potentially confounding factors that may impact the outcome and exposure; and 3). IVs cannot affect outcomes through any means other than exposure but can only affect outcomes through exposure [24] (Fig. 1). Due to the ethical approval and informed consent that had already been obtained from each of the initial studies, any further ethical reviews were not needed.
Data sources
First, two meta-analyses focused on migraine, collectively analyzing data from 873,341 [15] and 554,569 [14] individuals, which we used as a discovery sample and replication sample for positive MR, respectively. Additionally, two large publicly accessible GWAS datasets, which include 484,598 and 463,010 participants of European ancestry, provide summary-level statistics on migraine in the reverse MR.
In the GWAS meta-analysis [15] of migraine, which was utilized in forward discovery MR, SNPs were also identified using a strict genome-wide significance threshold. A total of 123 SNPs were identified using a strict genome-wide significance threshold in the initial set, and 23 SNPs (rs10128028, rs11578492, rs56019088, rs6693567, rs7564469, rs950570, rs73138150, rs12653216, rs11957829, rs10866704, rs74434374, rs11248546, rs200314499, rs12295710, rs566673, rs4842676, rs75002882, rs28929474, rs34914463, rs1285294, rs111404218, rs1507220, and rs4403550) were excluded due to evidence of linkage disequilibrium. As a result, a total of 100 SNPs were retained for subsequent analytical evaluation.
In the GWAS meta-analysis [14] of migraine, which was utilized in forward replication MR, SNPs were identified using a strict genome-wide significance threshold. From the initial set of 73 SNPs, eight were excluded due to evidence of linkage disequilibrium. The excluded SNPs were rs4704232, rs12936464, rs75002882, rs7093087, rs1268083, rs6693567, rs4278348, and rs1026332. Consequently, a total of 65 SNPs were retained for subsequent analytical evaluation.
Then, we utilized a number of summary-level statistics of CVD, including migraine [16, 22], atrial fibrillation (AF) [19], coronary atherosclerosis (CA) [22], coronary artery disease (CAD) [17], heart failure (HF) [18], hypertension [22], myocardial infarction (MI) [16], transient ischemic attack (TIA) [23], peripheral artery disease (PAD) [21], stroke and its subtype [20]. Except for two meta-analyses [14, 15], all GWAS data were obtained from the IEU GWAS database [25]. Table 1 provides an overview of all the summary-level statistics utilized in this study.
Instrumental variable selection
To identify genetic IVs that met these three MR assumptions, a series of quality control procedures were performed [12]. For SNPs that showed a strong association with exposure, a genome-wide significance threshold of P < 5 × 10− 8 was applied for initial screening. If SNPs did not satisfy the threshold, the P value requirement was loosened to < 5 × 10− 6 following protocols from prior MR studies. Due to the limited number of SNPs, the significance thresholds for large artery atherosclerosis ischemic stroke, small vessel ischemic stroke, and transient ischemic attack were relaxed to 5 × 10− 5 in the reverse replication MR. Additionally, to address the effects of linkage disequilibrium among the SNPs, a clumping process was conducted using an R2 < 0.001 and a clumping distance of greater than 10,000 kb. Furthermore, traits related to SNPs were examined after the clumping process. Palindromic SNPs possessing intermediate allele frequencies were removed by harmonizing the exposure and outcome datasets to ensure that SNPs matched on the identical effect allele for both. None of the single SNPs demonstrated any correlation with the relevant confounding factors. The F-statistic of the selected SNPs was calculated using the formula F = β2/se2 to avoid weak IV bias (F < 10) for our MR analysis study [26]. After the filtering protocol described above, these stringently screened SNPs served as the final IVs for subsequent MR analysis.
Mendelian randomization analysis
The causal association between migraine and CVD was evaluated using four MR analysis methods. The inverse variance-weighted (IVW) method was used to determine the causal relationship between exposure and outcome due to having the highest statistical validity, while the MR‒Egger, weighted median, and weighted mode methods were utilized as additional MR methods [12]. The MR‒Egger regression intercept can be utilized to measure horizontal pleiotropy, which provides a conservative estimate of causality but with decreased statistical accuracy [27]. The weighted median method can be utilized to offer an unbiased estimation when up to 50% of the IVs are invalid [28]. The weighted mode method can be applied to evaluate the robustness of MR results [29].
In addition, a series of sensitivity analyses were performed to assess heterogeneity and pleiotropy. Cochran’s Q test was utilized to quantify the heterogeneity associated with IVW and MR‒Egger regression [29]. P > 0.05 indicated no significant heterogeneity among the IVs. The IVW radial method was then used to examine instrumental variables with significant heterogeneity contributions [30]. The MR-Pleiotropy Residual Sum and Outlier (PRESSO) global test was utilized to detect potential horizontal pleiotropy [27]. If necessary, the results were recalculated after the exclusion of outliers. P > 0.05 suggested an absence of pleiotropy in IVs, thus fulfilling a key assumption.
All these analyses were performed using R software (version 4.3.2) with the R packages TwoSample MR (version 0.5.8), MR-PRESSO (version 1.0), and RadialMR (version 1.1).
Results
Effects of migraine on CVD
The MR results of migraine patients on CVD are listed in Fig. 2. In the discovery MR study, the IVW method revealed that genetically determined migraine was associated with CAD (OR = 0.881, 95% CI: 0.790–0.982, p = 0.023) (Figure S1)and ischemic stroke (OR = 0.912, 95% CI: 0.854–0.974, p = 0.006) (Figure S2). However, we did not find a significant correlation between migraine and AF, CA, MI, HF, hypertension, any stroke, cardioembolic ischemic stroke, small vessel ischemic stroke, large artery atherosclerotic ischemic stroke, TIA or PAD. Similar results to those of the IVW method were obtained using MR‒Egger analyses, the weighted median, and the weighted mode. Additionally, we obtained similar results in the replication MR study, demonstrating the reliability of the results (Fig. 3).
Effects of CVD on migraine
To further explore the causal association between migraine and CVD, a reverse MR study was performed with CVD as the exposure and migraine as the outcome (Fig. 4). Specifically, in the reverse discovery MR study, the IVW method showed that genetic CA (OR = 0.865, 95% CI: 0.797–0.940 p = 0.001) (Figure S3) and MI (OR = 0.798, 95% CI: 0.668–0.952, p = 0.012) (Figure S4)had a protective causal effect on migraine. However, we did not find a causal relationship between CVDs and migraine in the replication samples (Fig. 5). This could be a consequence of the limited number of IVs, which leads to insufficient statistical validity.
Discussion
Migraine and cardiovascular disease (CVD) are prominent public health problems worldwide [31]. Many studies have reported the epidemiological overlap between migraine and CVD [32, 33]. Although, previous epidemiological studies have found an increased risk of CVD in patients with migraine, the evidence for a causal relationship between migraine and CVD is scarce. In our Mendelian randomization (MR) study, a potentially protective effect of migraine on the risk of coronary artery disease (CAD) and ischemic stroke was identified. According to the reverse MR analysis, coronary atherosclerosis (CA) and myocardial infarction (MI) potentially led to a decreased risk of migraine. This is the most comprehensive MR article currently available to evaluate the causal association between migraine and CVD. However, the potentially protective effects of migraine and CVD on each other are unexpected given the existing epidemiologic research, but are consistent with previous studies from a genetic perspective.
Many epidemiological studies report an increased risk of CVD in migraineurs [6, 32, 34,35,36,37,38]. Large meta-analysis of case-control studies and observational cohort studies also reports increased risk of CVD in migraineurs [8, 39]. However, epidemiological studies of migraine-associated CVD risk have some inherent limitations. First, many observational studies about migraine and CVD are based on case‒control and cross-sectional designs, which are ambiguous in terms of chronology, preventing the inference of transparent causal associations. Second, a variety of confounding factors, such as the drugs utilized for acute and prophylactic treatment of migraine and CGRP receptor antagonists, will be susceptible in the observational studies by affecting CVD. Third, the difference of diagnostic criteria utilized in some observational studies may reduce the reliability of the results. In addition, our MR study is a mechanism-only study, targeting the signaling pathways and genetics of migraine and CVD, without incorporating confounding factors such as the external environment.
It is currently unclear to which extent the genetic roots of migraine and CVD overlap and contribute to the coincidence of CVD. There is debate about how migraine and CVD interact to each other in genetic level. The GWAS data for migraine used in our discovery study identified 123 risk loci [15], including 86 previously unknown ones, with the new loci encompassing genes encoding recent migraine-specific drug targets such as Calcitonin gene-related peptide (CALCA/CALCB) and serotonin 1 F receptor (HTR1F). However, in their analysis, the migraine risk alleles neither consistently increased nor consistently decreased the risk of CAD, but migraine dominant variants in the CAD GWAS, at a p-value of less than 1e-5, there were eight variants, one with the same direction of effect and seven with the opposite direction of effect, with a p-value of 0.07. This could mean overall that the opposite direction effect is greater than the same direction effect for migraine and CAD. Besides, the paper by Bendik et al. [40] in 2017 identified the shared genetic risk between migraine and CAD that the index SNPs at two (in KCNK5and AS3MT) of the three loci (PHACTR1, KCNK5and AS3MT) had opposite effect directions in migraine and CAD. A genetic risk score study for coronary disease based on the UK Biobank revealed that an increased genetic predisposition to CAD was inversely associated with migraine headaches [41]. At the same time, this study suggests that, in addition to the LRP1, PHACTR1, and FHL5 loci, there might be a rather extensive opposing genetic component between CAD and migraine. This further suggests that the mechanisms involved influence critical and delicate homeostatic features of vascular biology in opposite ways. A genetic study analyses using summary statistics from GWAS studies identified that known migraine loci also revealed novel associations with opposite risk alleles [42]. Specifically, these associations were found for all stroke, ischemic stroke, and small vessel stroke at rs55928386 (HTRA1); for large artery stroke at rs11172113 (LRP1); and for all stroke and ischemic stroke at rs1535791 and rs4942561 (both LRCH1). The focus of these studies has been on prioritizing the identification of shared gene loci and the quantification of genetic correlations, but we are explicitly concerned with the identification of causality, in which case we aim to minimize the effects of pleiotropy. Although we cannot conclude that future larger-scale GWAS will never find some specific loci for migraine with aura, we can assume that the opposite effect between migraine and CAD and ischemic stroke in our research.
The opposite epidemiological and genetic effects of migraine and CAD might indicate that there are mediating factors which reverse the direction of the effect estimates. We hypothesized that migraine may influence CVD through mediating factors. Diabetes might be a potential mediator, as migraine reduces the risk of developing type 2 diabetes in women with migraine [43]. Since diabetes is a known risk factor for CA and CAD, migraine reduces the risk factors for CA and CAD. Alcohol consumption could also be a potential mediator, as an MR study showed that the genetic liability to migraine is inversely associated with alcohol consumption [44], which is a causal risk factor for CVD. Genotypes of APOB or PCSK9 related to higher LDL-C levels which is the risk factor for CVD have shown an inverse association with migraine according to GWAS summary data [45]. However, the combination of confounding and overcontrol of protective mediators could influence not only the disease but also the medication taken by participants in the observational study, which could reverse the direction of the effect estimates [46].
Based on our MR results, we hypothesize that CGRP might be the potential biological mechanism that points to migraine as a protective factor for CAD. Migraine onset involves the release of large amounts of Calcitonin gene-related peptide (CGRP). CGRP receptors are located not only in the central and peripheral nervous system, but also in the cardiovascular system [47]. Simultaneously, CGRP is a potent vasodilator that functions through receptors on the endothelium to stimulate the production of nitric oxide (NO). This helps regulate blood flow and prevent ischemic damage, thereby providing a protective effect on the cardiovascular system. CGRP promotes coronary vasodilation and is involved in the formation of new blood vessels in response to ischemic insults [48]. This might explain the reason why migraine as a protective factor for CAD in our MR results. Some studies have also suggested that the protective effect of CGRP against ischemia [49], particularly in the context of brain ischemia, might reduce the extent of the infarct zone and protect against cerebral vasospasm [50]. The studies are consistent with our MR results and might be a potential pathway for migraine as an ischemic stroke. The effect of MI to reduce the risk of migraine is difficult to explain the potential mechanism. Because of the age-specific variability in the migraine and MI populations and the fact that epidemiologically migraine usually precedes MI, it is difficult to find additional paper that would support the effect of MI to reduce the risk of migraine occurrence. We speculate that this result may be due to the small number of SNPs included in the GWAS used for exposure and outcome, which may have contributed to the lack of robustness of the results. In the future, larger GWAS databases could give a more detailed explanation of MI and migraine.
Migraine and CVD are both genetically and environmentally regulated disorders. It has been suggested that 40–60% of the clinical presentation of migraine is determined by genetic factors, with the remainder being determined by non-genetic endogenous and exogenous risk modifiers and triggers [2]. This could mean that the influence of the external environment may be greater than that brought about by genes.
Indeed, differences in migraine between genders, which as the non-genetic endogenous, have been reported in the literature, such as higher CGRP plasma levels in women than in men [51], the cardiovascular benefits of CGRP, that may be strongly influenced by female sex hormones [52], and the possible interaction between CGRP and female sex hormones [53]. In addition, differences in gene expression occur in populations of different ages. For example, certain genes associated with migraine may have different expression levels in younger people, whereas their expression may be reduced or increased in older people [54]. Furthermore, not only does non-genetic endogenous influence the relationship between migraine and CVD, but also non-genetic exogenous. There are always dilemmas in the treatment of migraine and CVD in that medications such as NSAIDs, anti-CGRP antibodies, CGRP (receptor) monoclonal antibodies (mAbs), and triptans for migraine treatment or preventative medication can increase the risk of CVD as a side effect. NSAIDs combined with caffeine are often utilized as a first-line acute treatment for migraine [55]. However, chronic use or overuse of NSAIDs has been associated with a higher risk of venous thromboembolism and AF and may promote the conversion of episodic to chronic migraine [56, 57]. Calcitonin gene-related peptide receptor (CGRP receptor), a neuropeptide released by the trigeminal nerve, plays a crucial role in migraine pathophysiology [2]. In addition, while small-molecule antagonists of the CGRP receptor have been proven to be effective treatment options for migraine patients [58,59,60], blocking the vasodilatory effects of CGRP during ongoing (silent or transient) cerebral and cardiac ischemia could potentially lead to larger infarcts [10]. The subcutaneous administration of CGRP (receptor) mAbs, a relatively new preventative treatment for migraine, has been reported to increase the development of hypertension and worsen preexisting hypertension in the postmarketing setting [11]. Moreover, triptans are safe for most migraine patients but should be avoided in those with atherosclerotic diseases, such as coronary artery disease (CAD), stroke, and PAD, due to the risk of coronary artery vasoconstriction [61]. Therefore, our results highlight the importance of long-term clinical safety monitoring of migraine medications at the genetic level and the need for future research to focus on improving cardiovascular prognosis in migraine patients.
This study utilized large-exposure and outcome GWASs to conduct MR analysis to infer a causal association between migraine and CVDs. The major advantage of this study is the application of a robust MR design that minimizes reverse causality and confounding factors associated with traditional observational research. However, this study has several limitations. First, no subgroup analysis of migraine was performed, as summary statistics rather than raw data were utilized in the meta-analysis. Second, the GWAS cases in this study were all of European ancestry, so further studies are needed to determine whether the results of this study can be generalized to other human populations. Third, the sample sizes of some datasets were not large enough, resulting in insufficient statistical power in the replication MR. Therefore, a GWAS database with a larger sample size may be needed in the future for additional validation. Fourth, the study populations of migraine and cardiovascular disease may differ significantly in age and gender composition. However, sex and age information was not included in the GWAS database we used, which made it challenging to conduct more detailed analyses. In addition, a potential limitation is the overlap of participants in both the exposure and outcome datasets, as well as between the GWAS for migraine and CVDs, which could introduce sample overlap bias and lead MR estimates towards observational estimates, although the true proportion of overlap is likely very small and difficult to quantify. Finally, we found a potential protective effect of migraine on CAD and ischemic stroke, and we also found that CA and MI reduce the risk of migraine. We particularly emphasize the importance of long-term clinical safety monitoring of migraine medications at the genetic level and the need for future studies to focus on improving cardiovascular prognosis in migraine patients.
Conclusion
In conclusion, we found a potential protective effect of migraine on coronary artery disease and ischemic stroke, and we also found that coronary atherosclerosis and myocardial infarction reduce the risk of migraine. We also emphasize epidemiological and genetic differences and the importance of long-term clinical safety monitoring of migraine medications at the genetic level and the need for future studies to focus on improving cardiovascular prognosis in migraine patients. In addition, it must be emphasized that further research is required to confirm the final result.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- MR:
-
Mendelian randomization
- GWAS:
-
Genome-wide association study
- IVW:
-
Inverse variance weighted
- LOO:
-
Leave-one-out
- ESC:
-
European Society of Cardiology
- CVD:
-
Cardiovascular disease
- CAD:
-
Coronary artery disease
- MI:
-
Myocardial infarction
- AF:
-
Atrial fibrillation
- CA:
-
Coronary atherosclerosis
- HF:
-
Heart failure
- TIA:
-
Transient ischemic attack
- PAD:
-
Peripheral artery disease
- SNP:
-
Single nucleotide polymorphisms
- IV:
-
Instrumental variable
- PRESSO:
-
MR-Pleiotropy Residual Sum and Outliers
- NHANES:
-
National Health and Nutrition Examination Survey
- CGRP:
-
Calcitonin gene-related peptide receptor
References
Ashina M, Migraine. Ropper AH (eds) (2020) N Engl J M(ed). ;383(19):1866–76
Ferrari MD, Goadsby PJ, Burstein R, Kurth T, Ayata C, Charles A et al (2022) Migraine Nat Rev Dis Primers 8(1):2
Kalkman DN, Couturier EGM, El Bouziani A, Dahdal J, Neefs J, Woudstra J et al (2023) Migraine and cardiovascular disease: what cardiologists should know. Eur Heart J 44(30):2815–2828
Evans MA, Sano S, Walsh K (2020) Cardiovascular Disease, Aging, and Clonal Hematopoiesis. Annu Rev Pathol Mech Dis 15(1):419–438
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M et al (2021) 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J 42(34):3227–3337
Adelborg K, Szépligeti SK, Holland-Bill L, Ehrenstein V, Horváth-Puhó E, Henderson VW et al (2018) Migraine and risk of cardiovascular diseases: Danish population based matched cohort study. BMJ. ;k96
Chen D, Willis-Parker M, Lundberg GP (2020) Migraine headache: is it only a neurological disorder? Links between migraine and cardiovascular disorders. Trends Cardiovasc Med 30(7):424–430
Schurks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T (2009) Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ 339(oct27 1):b3914–b3914
MaassenVanDenBrink A, Reekers M, Bax WA, Ferrari MD, Saxena PR (1998) Coronary side-effect potential of current and prospective Antimigraine Drugs. Circulation 98(1):25–30
MaassenVanDenBrink A, Meijer J, Villalón CM, Ferrari MD, Wiping Out CGRP (2016) Potential Cardiovascular risks. Trends Pharmacol Sci 37(9):779–788
De Vries Lentsch S, Van Der Arend BWH, Maassen VanDenBrink A, Terwindt GM (2022) Blood Pressure in Patients With Migraine Treated With Monoclonal Anti-CGRP (Receptor) Antibodies: A Prospective Follow-up Study. Neurology [Internet]. Oct 25 [cited 2024 Apr 18];99(17). https://www.neurology.org/doi/https://doi.org/10.1212/WNL.0000000000201008
Richmond RC, Davey Smith G (2022) Mendelian randomization: concepts and scope. Cold Spring Harb Perspect Med 12(1):a040501
Davies NM, Holmes MV, Davey Smith G (2018) Reading mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. ;k601
Choquet H, Yin J, Jacobson AS, Horton BH, Hoffmann TJ, Jorgenson E et al (2021) New and sex-specific migraine susceptibility loci identified from a multiethnic genome-wide meta-analysis. Commun Biol 4(1):864
Hautakangas H, Winsvold BS, Ruotsalainen SE, Bjornsdottir G, Harder AVE, Kogelman LJA et al (2022) Genome-wide analysis of 102,084 migraine cases identifies 123 risk loci and subtype-specific risk alleles. Nat Genet 54(2):152–160
Dönertaş HM, Fabian DK, Fuentealba M, Partridge L, Thornton JM (2021) Common genetic associations between age-related diseases. Nat Aging 1(4):400–412
Mbatchou J, Barnard L, Backman J, Marcketta A, Kosmicki JA, Ziyatdinov A et al (2021) Computationally efficient whole-genome regression for quantitative and binary traits. Nat Genet 53(7):1097–1103
Shah S, Henry A, Roselli C, Lin H, Sveinbjörnsson G, Fatemifar G et al (2020) Genome-wide association and mendelian randomisation analysis provide insights into the pathogenesis of heart failure. Nat Commun 11(1):163
Nielsen JB, Thorolfsdottir RB, Fritsche LG, Zhou W, Skov MW, Graham SE et al (2018) Biobank-driven genomic discovery yields new insight into atrial fibrillation biology. Nat Genet 50(9):1234–1239
Malik R, Chauhan G, Traylor M, Sargurupremraj M, Okada Y, Mishra A et al (2018) Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet 50(4):524–537
Sakaue S, Kanai M, Tanigawa Y, Karjalainen J, Kurki M, Koshiba S et al (2021) A cross-population atlas of genetic associations for 220 human phenotypes. Nat Genet 53(10):1415–1424
Neale lab [Internet] [cited 2024 Apr 23]. UK Biobank. http://www.nealelab.is/uk-biobank
Introduction | R7 | FinnGen Public Documentation [Internet] (2022) [cited 2024 Apr 23]. https://finngen.gitbook.io/documentation/v/r7/
Skrivankova VW, Richmond RC, Woolf BAR, Yarmolinsky J, Davies NM, Swanson SA et al (2021) Strengthening the reporting of Observational studies in Epidemiology using mendelian randomization: the STROBE-MR Statement. JAMA 326(16):1614
Browse the IEU OpenGWAS project [Internet] [cited 2024 Apr 25]. https://gwas.mrcieu.ac.uk/datasets/
Burgess S, Thompson SG, CRP CHD Genetics Collaboration (2011) Avoiding bias from weak instruments in mendelian randomization studies. Int J Epidemiol 40(3):755–764
Bowden J, Davey Smith G, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44(2):512–525
Bowden J, Davey Smith G, Haycock PC, Burgess S (2016) Consistent estimation in mendelian randomization with some Invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314
Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan N, Thompson J (2017) A framework for the investigation of pleiotropy in two-sample summary data mendelian randomization. Stat Med 36(11):1783–1802
Bowden J, Spiller W, Del Greco MF, Sheehan N, Thompson J, Minelli C et al (2018) Improving the visualization, interpretation and analysis of two-sample summary data mendelian randomization via the Radial plot and radial regression. Int J Epidemiol 47(4):1264–1278
Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP et al Heart Disease and Stroke Statistics—2020 Update: A Report From the American Heart Association. Circulation [Internet]. 2020 Mar 3 [cited 2024 May 12];141(9). https://www.ahajournals.org/doi/https://doi.org/10.1161/CIR.0000000000000757
Liu H, Zhang S, Gong Z, Zhao W, Lin X, Liu Y et al Association between migraine and cardiovascular disease mortality: a prospective population-based cohort study
Kurth T, Rist PM (2023) Migraines and cardiovascular disease: mechanisms and methodological challenges. Nat Rev Cardiol 20(12):791–792
Kurth T, Rist PM, Ridker PM, Kotler G, Bubes V, Buring JE (2020) Association of Migraine with Aura and other risk factors with Incident Cardiovascular Disease in Women. JAMA 323(22):2281
Rist PM, Buring JE, Cook NR, Kurth T (2023) Contribution of Migraine to Cardiovascular Disease Risk Prediction. J Am Coll Cardiol 81(23):2246–2254
Li L, Schulz UG, Kuker W, Rothwell PM (2015) Age-specific association of migraine with cryptogenic TIA and stroke: Population-based study. Neurology 85(17):1444–1451
Kwon MJ, Choi HG, Kim YH, Kim JH, Rim HT, Lee HS et al (2023) A higher probability of subsequent stroke and ischemic heart disease in migraine patients: a longitudinal follow-up study in Korea. J Headache Pain 24(1):98
Siao WZ, Su CH, Kuan YH, Tsai TH, Huan KH, Lee CY (2022) Risk of peripheral artery disease and stroke in migraineurs with or without aura: a nationwide population-based cohort study. Int J Med Sci 19(7):1163–1172
Sacco S, Ornello R, Ripa P, Tiseo C, Degan D, Pistoia F et al (2015) Migraine and risk of ischaemic heart disease: a systematic review and meta-analysis of observational studies. Euro J Neurol 22(6):1001–1011
Winsvold BS, Bettella F, Witoelar A, Anttila V, Gormley P, Kurth T et al (2017) Shared genetic risk between migraine and coronary artery disease: A genome-wide analysis of common variants. Yao YG, editor. PLoS ONE. ;12(9):e0185663
Ntalla I, Kanoni S, Zeng L, Giannakopoulou O, Danesh J, Watkins H et al (2019) Genetic risk score for Coronary Disease identifies predispositions to Cardiovascular and Noncardiovascular diseases. J Am Coll Cardiol 73(23):2932–2942
Daghlas I, Sargurupremraj M, Danning R, Gormley P, Malik R, Amouyel P et al (2022) Migraine, Stroke, and cervical arterial dissection: Shared Genetics for a Triad of Brain disorders with vascular involvement. Neurol Genet 8(1):00
Fagherazzi G, El Fatouhi D, Fournier A, Gusto G, Mancini FR, Balkau B et al (2019) Associations between Migraine and Type 2 diabetes in women: findings from the E3N cohort study. JAMA Neurol 76(3):257
Yuan S, Daghlas I, Larsson SC (2022) Alcohol, coffee consumption, and smoking in relation to migraine: a bidirectional mendelian randomization study. Pain 163(2):e342–e348
Hong P, Han L, Wan Y (2024) Mendelian randomization study of lipid metabolism characteristics and migraine risk. Eur J Pain. ;ejp.2235.
Van Zwieten A, Tennant PWG, Kelly-Irving M, Blyth FM, Teixeira-Pinto A, Khalatbari-Soltani S (2022) Avoiding overadjustment bias in social epidemiology through appropriate covariate selection: a primer. J Clin Epidemiol 149:127–136
Sohn I, Sheykhzade M, Edvinsson L, Sams A (2020) The effects of CGRP in vascular tissue - classical vasodilation, shadowed effects and systemic dilemmas. Eur J Pharmacol 881:173205
Aubdool AA, Thakore P, Argunhan F, Smillie SJ, Schnelle M, Srivastava S et al (2017) A novel α-Calcitonin gene-related peptide Analogue protects against end-organ damage in experimental hypertension, Cardiac Hypertrophy, and Heart failure. Circulation 136(4):367–383
Chai W, Mehrotra S, Jan Danser AH, Schoemaker RG (2006) The role of calcitonin gene-related peptide (CGRP) in ischemic preconditioning in isolated rat hearts. Eur J Pharmacol 531(1–3):246–253
Zhai L, Sakurai T, Kamiyoshi A, Ichikawa-Shindo Y, Kawate H, Tanaka M et al (2018) Endogenous calcitonin gene-related peptide suppresses ischemic brain injuries and progression of cognitive decline. J Hypertens 36(4):876–891
Raffaelli B, Storch E, Overeem LH, Terhart M, Fitzek MP, Lange KS et al (2023) Sex Hormones and Calcitonin Gene–Related Peptide in Women With Migraine: A Cross-sectional, Matched Cohort Study. Neurology [Internet]. Apr 25 [cited 2024 Jul 22];100(17). https://www.neurology.org/doi/https://doi.org/10.1212/WNL.0000000000207114
Gangula PRR, Wimalawansa SJ, Yallampalli C (2002) Sex steroid hormones Enhance Hypotensive effects of Calcitonin Gene-related peptide in aged female Rats1. Biol Reprod 67(6):1881–1887
Gupta S, Villalón CM, Mehrotra S, De Vries R, Garrelds IM, Saxena PR et al (2007) Female sex hormones and rat Dural Vasodilatation to CGRP, Periarterial Electrical Stimulation and Capsaicin. Headache 47(2):225–235
De Boer I, Van Den Maagdenberg AMJM, Terwindt GM (2019) Advance in genetics of migraine. Curr Opin Neurol 32(3):413–421
Robbins MS (2021) Diagnosis and management of Headache: a review. JAMA 325(18):1874
Schmidt M, Christiansen CF, Mehnert F, Rothman KJ, Sorensen HT (2011) Non-steroidal anti-inflammatory drug use and risk of atrial fibrillation or flutter: population based case-control study. BMJ 343(jul04 1):d3450–d3450
Ungprasert P, Srivali N, Wijarnpreecha K, Charoenpong P, Knight EL (2015) Non-steroidal anti-inflammatory drugs and risk of venous thromboembolism: a systematic review and meta-analysis. Rheumatology 54(4):736–742
Goadsby PJ, Dodick DW, Ailani J, Trugman JM, Finnegan M, Lu K et al (2020) Safety, tolerability, and efficacy of orally administered atogepant for the prevention of episodic migraine in adults: a double-blind, randomised phase 2b/3 trial. Lancet Neurol 19(9):727–737
Tassorelli C, Nagy K, Pozo-Rosich P, Lanteri-Minet M, Sacco S, Nežádal T et al (2024) Safety and efficacy of atogepant for the preventive treatment of episodic migraine in adults for whom conventional oral preventive treatments have failed (ELEVATE): a randomised, placebo-controlled, phase 3b trial. Lancet Neurol 23(4):382–392
Pozo-Rosich P, Ailani J, Ashina M, Goadsby PJ, Lipton RB, Reuter U et al (2023) Atogepant for the preventive treatment of chronic migraine (PROGRESS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 402(10404):775–785
Sacco S, Harriott AM, Ayata C, Ornello R, Bagur R, Jimenez-Ruiz A et al (2023) Microembolism and other Links between Migraine and Stroke: clinical and pathophysiologic update. Neurology 100(15):716–726
Acknowledgements
We are grateful to the referenced studies or consortiums contributing open-access datasets for the analysis.
Funding
The study was supported by the National Natural Science Foundation of China (Grant No. 81960421), the Yunnan Talents Support Program (Grant No. XDYC-MY-2022-0064), and the Yunnan Provincial Department of Education Scientific Research Fund Project [2024J0261].
Author information
Authors and Affiliations
Contributions
XR D, CD L and TF K created the concept and design of this study. XL D designed and painted the figures in this study. M Z provided knowledge about cardiovascular disease and migraine. GR Z, XY Z, N T, GC L and B L were responsible for the statistical analysis. XR D and CD L drafted, revised, and edited the manuscript. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The data used in this MR analysis were entirely from previously reported summary data. Therefore, neither patient consent nor ethical approval was necessary for the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Duan, X., Du, X., Zheng, G. et al. Causality between migraine and cardiovascular disease: a bidirectional Mendelian randomization study. J Headache Pain 25, 130 (2024). https://doi.org/10.1186/s10194-024-01836-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-024-01836-w