Abstract
Background
Non-steroidal anti-inflammatory drugs (NSAIDs) are considered first-line medications for acute migraine attacks. However, the response exhibits considerable variability among individuals. Thus, this study aimed to explore a machine learning model based on the percentage of amplitude oscillations (PerAF) and gray matter volume (GMV) to predict the response to NSAIDs in migraine treatment.
Methods
Propensity score matching was adopted to match patients having migraine with response and nonresponse to NSAIDs, ensuring consistency in clinical characteristics and migraine-related features. Multimodal magnetic resonance imaging was employed to extract PerAF and GMV, followed by feature selection using the least absolute shrinkage and selection operator regression and recursive feature elimination algorithms. Multiple predictive models were constructed and the final model with the smallest predictive residuals was chosen. The model performance was evaluated using the area under the receiver operating characteristic (ROCAUC) curve, area under the precision-recall curve (PRAUC), balance accuracy (BACC), sensitivity, F1 score, positive predictive value (PPV), and negative predictive value (NPV). External validation was performed using a public database. Then, correlation analysis was performed between the neuroimaging predictors and clinical features in migraine.
Results
One hundred eighteen patients with migraine (59 responders and 59 non-responders) were enrolled. Six features (PerAF of left insula and left transverse temporal gyrus; and GMV of right superior frontal gyrus, left postcentral gyrus, right postcentral gyrus, and left precuneus) were observed. The random forest model with the lowest predictive residuals was selected and model metrics (ROCAUC, PRAUC, BACC, sensitivity, F1 score, PPV, and NPV) in the training and testing groups were 0.982, 0.983, 0.927, 0.976, 0.930, 0.889, and 0.973; and 0.711, 0.648, 0.639, 0.667,0.649, 0.632, and 0.647, respectively. The model metrics of external validation were 0.631, 0.651, 0.611, 0.808, 0.656, 0.553, and 0.706. Additionally, a significant positive correlation was found between the GMV of the left precuneus and attack time in non-responders.
Conclusions
Our findings suggest the potential of multimodal neuroimaging features in predicting the efficacy of NSAIDs in migraine treatment and provide novel insights into the neural mechanisms underlying migraine and its optimized treatment strategy.
Similar content being viewed by others
Introduction
Migraine is the second leading cause of disability among all age groups worldwide, and the leading cause of disability among women aged 15 to 49 [1, 2]. At present, the pathophysiological mechanisms underlying migraine remain unclear. Migraine is accompanied by various clinical symptoms and can be induced by multiple factors. This suggested that migraine has complex neuropathological mechanisms, possibly leading to a far less satisfactory treatment for migraine management [3,4,5]. Although some studies have proposed and developed more specific treatment strategies for migraine, non-steroidal anti-inflammatory drugs (NSAIDs) are still the recommended first-line medications for the acute phase of migraine attacks [6,7,8,9]. At present, the selection strategy for NSAIDs is mainly based on the trial-and-error method, which may prolong the disease course and increase the cost of ineffectiveness. Moreover, the use of NSAIDs increases the risk of developing gastrointestinal symptoms, liver and kidney impairment, and cardiovascular accidents [10, 11]. Considering the socioeconomic influence and personal burden caused by migraine, exploring effective treatment strategies for this condition is a core area of clinical issues.
Currently, the trigeminovascular system (TVS) is widely recognized as the primary neuropathological mechanism underlying migraine [12, 13]. Multimodal magnetic resonance imaging (MRI) provides a novel approach to comprehensively gain a deeper understanding of the neuropathological mechanism and clinical treatment strategies for migraine. Disturbances in brain function and structure within the TVS contribute to the occurrence and development of migraine, and give rise to the manifestation of complicated clinical symptoms associated with migraine [14, 15]. In particular, the brain stem, thalamus, limbic system, and higher sensory cortex are the key cerebral regions involved in the TVS [13, 16]. Of note, the periaqueductal gray within the brainstem is believed to be a trigger area for migraine. This finding is strongly supported by a positron emission tomography study in which the authors observed increased cerebral blood flow in the dorsal pons during spontaneous migraine attacks [17]. On the other hand, the thalamus serves as the tertiary structure of the TVS, receiving pain signals transmitted from the dura and spinal cord trigeminocervical complex before projecting them to the high-level cortex [13]. Furthermore, migraine has been proposed as a disorder of the neurolimbic pain network [18], in which neural activity reflects the affective experience that activates our response to pain [19]. The inhibition of neural activity and a decrease in cerebral blood flow in the higher cerebral regions of the TVS may play an essential role in the neural mechanism underlying medication-induced analgesia [20, 21]. Despite these findings, the relationship between the functional and structural changes in the brain regions of the TVS and clinical treatment outcomes for migraine remains unclear.
Individualized treatment is an important trend in future medical therapy [22, 23]. The widespread use of medical imaging information for diagnosing neurological and psychiatric disorders has facilitated the development of biomarkers for migraine based on its neuropathophysiological mechanisms. These predictors can aid in disease diagnosis and classification, and help predict the outcomes and prognosis of individualized treatment [15, 24,25,26,27,28]. Neural activity in the cerebral cortex can be used to effectively classify migraine and its subtypes [24, 25]. Furthermore, prediction models for assessing acupuncture efficacy have been established based on functional and structural changes in patients with migraine, which have yielded promising results [26, 27]. However, few studies have been conducted using multimodal MRI information to predict the efficacy of NSAIDs in migraine management.
Machine learning (ML), a branch of artificial intelligence, has emerged as a powerful tool for analyzing complex data sets and making predictions based on identified patterns. By integrating multiple neuroimaging features and leveraging the power of ML algorithms, it is possible to construct models that can predict treatment outcomes with high accuracy. In this study, we hypothesized that abnormalities in the percent amplitude of fluctuation (PerAF) and gray matter volume (GMV) hold predictive value for the efficacy of NSAIDs in patients with migraine. PerAF is indicative of the magnitude of spontaneous neuronal activity and is not influenced by the scale of the original signal, showing higher reliability [29]. Concurrently, GMV offers insights into the structural integrity of brain regions. Such a model could guide clinicians in making informed decisions on NSAIDs prescriptions, aiming to optimize treatment outcomes and reduce reliance on trial-and-error methods.
Methods
Participants
Patients diagnosed with episodic migraine conforming to the International Classification of Headache Disorders (the 3rd Edition) [30] were recruited between January 2018 and December 2023. The diagnosis was made by a qualified neurologist based on a detailed medical history, clinical examination, and exclusion of other potential causes of headache. Inclusion and exclusion criteria for patients with episodic migraine and MRI scanning parameters are provided in detail in Supplementary Materials. Ethical approval was obtained through the Ethics Committee of the Affiliated Jiangning Hospital of Nanjing Medical University (20180285, 2020–03-026-K01, and 2023–03-010-K01). Informed consent was obtained from all subjects according to institutional review board–approved protocols, which were carried out in accordance with the Declaration of Helsinki.
Patients with episodic migraine have been required to complete comprehensive structured questionnaires before the scanning, including demographic data (e.g., age, sex, and education level), migraine-related features (e.g., disease duration, frequency, attack time, headache intensity, impact extent, and burden on quality of life), neuropsychiatric assessment (e.g., anxiety, depression, and sleep disorders), and sleep quality. Specifically, the intensity, extent, and burden of migraine were assessed using the Visual Analogue Scale (VAS) [31], Headache Impact Test 6-Item (HIT-6) [32], and Migraine Disability Assessment Scale (MIDAS) [33], respectively. Anxiety, depression, and sleep quality were measured using the Generalized Anxiety Disorder 7-Item (GAD-7) [34], Patient Health Questionnaire 9-Item (PHQ-9) [35], and Pittsburgh Sleep Quality Index (PSQI) [36], respectively.
Response assessment
After scanning, patients with episodic migraine were asked to record the headache diary, mainly including the date of migraine attacks, the types and doses of medications taken, and the intensity of pain experienced before and 2 h after medication administration over the following 3 months. The documentation of date allows us to quantify the frequency and number of attacks, while the recorded levels of pain serve as a critical indicator for evaluating the treatment efficacy. The criteria for evaluating efficacy were as follows: (1) no pain after 2 h; (2) improvement from moderate to severe pain to mild or no pain (or decrease in VAS score by 50%) after 2 h; (3) no recurrence or need for medications within 24 h after successful treatment; and (4) repeatable curative effects with effects in at least more than two of the three attacks.
Data processing
The processing of functional images was performed using the Resting-state Functional MRI Data Analysis Toolkit plus (RESTplus, http://restfmri.net/forum/) [37]. The main steps were as follows: (1) The first 10 time points were discarded to avoid instability of the initial MRI signals, (2) slice-timing adjustment and realignment, (3) spatial standardization into Montreal Neurological Institute (MNI) space (resampling voxel size = 3 mm × 3 mm × 3 mm), (4) smoothing with a full-width at half-maximum (FWHM) of 6 mm and detrending, and (5) controlling head motion, white matter (WM) signal, and cerebrospinal fluid signal (CFS). Participants who exhibited head motion of less than 2.0 mm displacement or a 2.0◦ rotation in any direction were included. For PerAF calculation, bandpass filtering was performed with a frequency range of 0.01–0.08 Hz. The detailed formula calculating the PerAF value of a single voxel is referred to Jia et al. [29].
The processing of 3D T1-weighted images was performed using the Voxel-Based Morphometry toolbox (VBM8, http://dbm.neuro.uni-jena.de/vbm) based on the Statistical Parametric Mapping (SPM12, https://www.fil.ion.ucl.ac.uk/spm/). The structural images were first visually screened to exclude poor-quality images and then segmented into WM, GM, and CSF using the standard segmentation model. After affine registration of the GM concentration map to MNI space, the images were nonlinearly deformed using the DARTEL algorithm and resampled to 1.5 mm3 isotropic voxel size. The normalized and modulated tissue probability map of GM volume was obtained by multiplying the GM concentration map by the nonlinear determinant. Finally, the GM images were smoothed with a FWHM of 15 mm.
Model construction
The propensity score matching (PSM) was employed to account for any discrepancies in the baseline data between patients with response and nonresponse to NSAIDs in terms of demographic data, migraine-related features, and neuropsychiatric assessment. The final included patients with episodic migraine after PSM analysis were allocated to training and testing cohorts in a ratio of 7:3, using a stratified random sampling method. Further, the least absolute shrinkage and selection operator (LASSO) logistic regression and support vector machine recursive feature elimination (SVM-RFE) algorithms were used for feature selection.
The included neuroimaging features were used for constructing multiple ML models including logistic regression, SVM, random forest (RF), decision tree (DT), k-nearest neighbor (KNN), multilayer perceptron, elastic network, light gradient boosting machine (Lightgbm), extreme gradient boosting algorithms. The tenfold CV on the training data was conducted to prevent overfitting, followed by a calibration curve. The Brier score was applied as the calibration index wherein lower Brier scores represent a higher calibration degree. The model with the lowest root mean square (RMS) of residuals and Brier score was selected as the final model.
Seven statistical metrics were utilized to evaluate the model performance: area under the receiver operating characteristic (ROCAUC) curve, area under the precision-recall curve (PRAUC), balance accuracy (BACC), sensitivity, F1 score, positive predictive value (PPV), and negative predictive value (NPV).
Moreover, Shapley additive explanations (ie, SHAP values) [38] were calculated to further quantify the association of a variable with the outcome individually. A positive SHAP value indicates that the corresponding variable tends to response, and vice versa. The contribution of a variable toward prediction performance is represented by the magnitude of SHAP values.
External validation cohort
For external validation, we used a public database: the OpenNEURO database (https://openneuro.org/datasets/ds000208/versions/1.0.1) [39]. The external validation cohort consists of 39 patients with chronic osteoarthritis pain, with an average age of 58.36 years and a standard deviation of 7.47. The gender distribution is nearly balanced with 18 males and 21 females. Patients with chronic osteoarthritis pain were treated with either placebo or duloxetine. Ultimately, 18 patients experienced a beneficial response to treatment, while 21 did not. Among the 20 patients who received duloxetine, 8 patients reported beneficial response.
Subgroup analysis and correlation analysis
All continuous variables were grouped according to the medians. The interaction effects were assessed via subgroup analysis. Additionally, we calculated the contribution levels of features in age and sex subgroups to evaluate the potential bias of age and sex that could act as confounding factors in the association between features and outcomes.
Then, Spearman correlation analysis was performed to analyze the correlation between the included neuroimaging features and clinical characteristics of patients with episodic migraine.
Statistical analysis
Statistical analyses were performed using SPSS software (version 24.0) and R software (version 4.2.1). Continuous variables with normal distribution were presented as mean (standard deviation), whereas those with non-normal distribution were presented as median (interquartile range) and compared using Mann–Whitney U test. Categorical variables were analyzed using Chi-square or Fisher’s exact tests. Statistical significance was established at a threshold of p < 0.05. The flowchart presented in Fig. 1 describes all processes of sample selection and model construction.
The flowchart illustrates all processes of patient selection and model construction. GMV, gray matter volume; ICHD, International Classification of Headache Disorders; LASSO, least absolute shrinkage and selection operator; NSAIDs, non-steroidal anti-inflammatory drugs; PerAF, percent amplitude of fluctuation; PSM, propensity score matching; RFE, recursive feature elimination
Results
Demographic and clinical characteristics
After PSM, 118 patients with migraine (59 responders and 59 non-responders) were included in this study. No significant differences were found in the demographic data, migraine-related features, and neuropsychiatric assessment between the patients with response and nonresponse to NSAIDs (Table 1).
Model performance
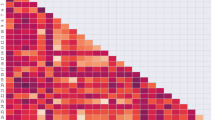
The patients with episodic migraine were randomly divided into a training group (n = 82) and a testing group (n = 36) according to a ratio of 7:3. Six features were finally included after LASSO and SVM-RFE algorithms, namely the PerAF of the left insula (INS.L) and left transverse temporal gyrus (TTG.L), and the GMV of the left postcentral gyrus (PoCG.L), right PoCG (PoCG.R), left precuneus (PCU.L), and right superior frontal gyrus (SFG.R). The RF model was selected as the best model based on its lowest RMS (Fig. 2A) and Brier score (Fig. 2B). Figure 3 displays the contribution importance of the selected features in RF model to the identification ability on the vertical axis in descending order (PoCG, INS, PCU, TTG, and SFG) and the distribution of SHAP values of a single feature in an individual. In particular, the GMV of PoCG.L plays a significantly positive role in treatment response, whereas the PerAF of INS.L exhibits an inverse effect.
Residual plots for all models to demonstrate the residual distribution. Grey dots represent root mean squares (A). Calibration curves and Brier scores of all models (B). BS, Brier score; DT, decision tree; ENet, elastic network; RF, random forest; KNN, k-nearest neighbor; Lightgbm, light gradient boosting machine; LR, logistic regression; MLP, multilayer perceptron; SVM, support vector machine; Xgboost, extreme gradient boosting
SHAP values illustrate how features contribute to the random forest model. Blue shows a negative contribution, and orange shows a positive contribution. The mean of SHAP values indicates the average contribution of the variable in the model and is provided on the vertical axis in descending order. INS, insula; PCU, precuneus; PoCG, postcentral gyrus; SHAP, SHapley Additive exPlanations; SFG, superior frontal gyrus; TTG, transverse temporal gyrus; L, left; R, right
The RF model performance metrics (ROCAUC, PRAUC, BACC, sensitivity, F1 score, PPV, and NPV) of the training and testing groups were 0.982, 0.983, 0.927, 0.976, 0.930, 0.889, and 0.973; and 0.711, 0.648, 0.639, 0.667, 0.649, 0.632, and 0.647, respectively (Table 2 and Fig. 4A, B). Moreover, these of the external group were 0.631, 0.651, 0.611, 0.808, 0.656, 0.553, and 0.706, respectively (Table 2 and Fig. 4C).
Receiver operating characteristic and precision-recall curves of the random forest model in the training, testing, and external groups (A, B). The line charts (C) of the random forest model performance metrics: area under the receiver operating characteristic (ROCAUC) curve, area under the precision-recall curve (PRAUC), balance accuracy(BACC), sensitivity (SEN), F1 score, positive predictive value (PPV), and negative predictive value (NPV)
Moreover, in the testing group, the KNN and Lightgbm models generally outperform the RF model in terms of multiple metrics. In the external validation group, the DT model achieves a higher PRAUC than the RF model. However, the RF model overall demonstrates the best performance among all external models. The detailed model metrics of all 9 models across the testing and external validation datasets were summarized in the Supplementary Materials (Figure S1 and Table S1).
Subgroup analysis and correlation analysis results
Subgroup analysis reveals no significant interactions among all subgroups, and the detailed results are summarized in Table 3. Moreover, subgroup analysis results indicate that in patients with episodic migraine, the GMV of the PoCG predominates in the model, followed by the functions of INS and TTG. Conversely, in patients with chronic osteoarthritis, the functions of INS and TTG become the primary contributors, followed by the GMV of the PoCG. The importance of PCU and SFG remains relatively stable in all subgroups. The detailed varied contribution levels of these features in age and sex subgroups of our migraine and external validation datasets are described in Fig. 5A, B.
In the non-response group, the GMV of the PCU.L was positively correlated with attack time (r = 0.310, p = 0.017) (Fig. 6). No other significant correlations were found.
Discussion
In this study, we developed a RF model for the analgesic effect of episodic migraine treatment based on the whole-brain functional and structural signatures. Although some other models exhibited superior performance than the RF model in terms of certain prediction metrics in the testing and external groups, it is essential to consider that during the model construction and selection phase, the prediction metrics for both the testing and external groups were unknown. This model also predicted an independent dataset in patients with chronic knee osteoarthritis pain [39], and showed comparable performance. The selection of this specific external validation dataset was guided by several critical factors. First, the experimental design closely resembled our study, involving multimodal magnetic resonance imaging scanning prior to a 3-month treatment period and the primary objective to predict post-treatment analgesic effects based on baseline neuroimaging data. This similarity ensures that the external validation is meaningful. Second, the patient population in the external validation cohort suffers from chronic knee osteoarthritis, a condition that, like migraine, falls under the category of chronic inflammatory diseases and shares certain overlapping pathological mechanism [40]. The existence of this overlap was critical to the selection of this dataset to evaluate the model performance beyond the specific context of migraine. Lastly, the inclusion of both responders and non-responders in the external validation dataset is invaluable. It allows us to evaluate the model performance across different treatment strategies in different pain conditions. Additionally, these datasets were heterogeneous in terms of pain conditions, scanning parameters, and participant characteristics. The heterogeneity of the samples might reduce predictive accuracy during external validation, but it helps develop a model with better robustness and generalizability. Comparisons between models for treatment efficacy in different pain conditions provided evidence that different pain conditions share common brain representations in response to pain treatment. Therefore, this study provides promising neuroimaging biomarkers for predicting the analgesic effect of migraine management with potential for clinical translation.
The observed neuroimaging features were involved in multiple cerebral networks which constitute a complex TVS [13]. These networks mainly include the default mode network (DMN), central executive network (CEN), auditory network, sensorimotor network (SMN), and salience network (SN). The SFG is part of the prefrontal cortex (PFC), and together with the parietal cortex constitutes the CEN typically associated with the cognitive and executive functions [41, 42]. The PCU is a core region of the posterior DMN (pDMN), which is highly active at rest and inhibits activity mainly involved in internally-directed cognition, such as emotional processing and self-referential activity [43, 44]. The INS is a hub in the SN, which is mainly responsible for regulating attention shifting between the exogenous and endogenous states [45,46,47]. The PoCG belongs to the primary sensory cortex (S1) and combines the premotor cortex, primary motor cortex, and posterior parietal cortex to receive and integrate motor and sensory information for planning and coordinating complex movements [48, 49]. The TTG also known as Heschl’s gyrus is the typical location of the primary auditory cortex and is the first cortical structure to process incoming auditory information [50]. However, previous research indicated that the TTG is a part of the SMN [51]. In this study, our results suggest that the functional and structural abnormalities of TVS may play a crucial role in the modulation of pain-related signals and in our model of predicting analgesic effect, although this hypothesis needs to be tested more thoroughly in the future.
The key finding of the present study is that aberrant multimodal neuroimaging features in the TVS are pivotal factors in the neuropathological and analgesic mechanisms of migraine. The TVS is primarily composed of an ascending pain facilitatory pathway and a descending pain modulatory pathway [13]. Similar to our results, a previous study has shown that compared with HCs, individuals with migraine exhibited higher signal variation in the ascending trigeminal spinal-thalamo-cortical pathway, mainly including the spinal trigeminal nucleus, thalamus, S1, and posterior INS. Conversely, they exhibited lower signal variation in the descending pain modulatory pathway, mainly located in the dorsolateral PFC and parietal cortex [52]. Moreover, some resting-state functional MRI studies, focusing on pain conditions such as trigeminal neuralgia [53], postherpetic neuralgia [54], and chronic back pain [55], have shown reduced neural rhythms in the PFC and its associated projection pathways to the mesolimbic system, suggesting that PFC inhibition may represent a maladaptive cortical process derived from the mechanisms of persistent pain [56]. Therefore, the above findings indicated that patients with migraine showed the ability of excessive upward transmission and insufficient downward regulation of nociceptive signals. This regulatory imbalance of pain signals in the ascending descending pathways is considered the core neural mechanism underlying the occurrence, development, and analgesia of migraine.
The research has also shown that the results of the SHAP plot and subgroup analysis are similar, both indicating that the PoCG and INS play a pivotal role in the prediction models. In recent studies using resting-state functional and structural MRI, various brain networks with functional and structural changes have been reported in patients with migraine, and show notable correlations with the clinical features [57, 58]. These brain networks are consistent with the brain regions observed in this study. Moreover, there is growing evidence that neurological functional change and tissue morphology change do not synchronize, and changes in brain function are likely to be more sensitive than those in structural pathways [59,60,61]. These results implied a causal dissociation between functional impairment and structural damage. In the subgroup analysis, we observed that the younger migraine cohort showed the most significant contribution in terms of the INS function, whereas the older migraine cohort exhibited a heightened contribution degree concerning GMV within the S1, followed by the INS function. Notably, the external cohort, which consisted of individuals of advanced age in comparison to the migraine cohort, exhibited more importance of functional alterations in all subgroups. Especially, the younger subgroup of the external cohort had a relatively higher contribution proportion of function to treatment effects, similar to the episodic migraine cohort. This phenomenon may be attributed to age-related changes in brain structural integrity, which subsequently exert an influence on function.
Despite the general trend of age-related changes in cerebral cortex, such as a decrease in volume or thickness, particularly with a rate of gray matter loss in the INS that is twice the average rate across the entire brain [62], it has been observed that the structure of the INS does not significantly change with age in patients with migraine [63]. Compared to healthy female controls, female patients with migraine have thicker INS and PCU, while no such changes were found in male patients with migraine [64]. These suggested that resistance of cortical atrophy in INS is an inherent feature of migraine and functional alterations in INS render it more sensitive to the pathological mechanisms in migraine, especially in female population. Moreover, a positive correlation between larger GMV (including S1 and INS) and pain tolerance suggested that brain structure may have a neuroplastic compensatory function for recurrent stress in a general population [65]. Therefore, for the heterogeneity of the structural and functional contributions to the therapeutic response between migraine and osteoarthritis groups in the subgroup results, possible explanations include the decompensation of aging brain structure in response to long-term chronic stimulation by pain signals and physiological atrophy, leading to a more important role of function regulation in analgesic effects in older external group. Further, we speculated that individual variations in pain perception and therapeutic outcomes may be attributed to the distinct processing of pain signals and neuromodulatory mechanisms in the brain, which are characteristic of various pain conditions.
In addition, a study on the neurological mechanism of NSAIDs antinociception using arterial spin labeling found that pain condition significantly increased cerebral blood flow (CBF) in various brain regions such as the brainstem, midbrain, thalamus, INS, S1, and PFC. However, after administering ibuprofen, CBF in the INS, S1, and PFC decreased significantly [20]. An animal model has also shown that NSAIDs-evoked antinociception by injecting into the INS can significantly reduce the reaction to exogenous pain stimuli via descending endogenous opioid and cannabinoid system [66]. Moreover, the INS can predict the response to transcutaneous vagus nerve stimulation and showed a negative correlation between the decreased fractional amplitude of low frequency fluctuations (fALFF) and the relief of migraine symptoms [67]. The fALFF, which is the ratio of ALFF values at specific frequency bands (0.01 Hz to 0.08 Hz) to the overall ALFF value, can effectively reduce noise interference and improve the sensitivity and specificity of spontaneous brain activity detection. The perAF adopted is similar, reflecting fluctuation in neural activity [29]. Lower values indicate more stable neural function. We also found a negative contribution of the perAF of INS to predict NSAIDs efficacy in migraine. These results suggest that the stable functional activity observed in the INS serves as a preparation for and defense against the impact of pain signals. This stable functional activity may represent a self-protective response of the brain to painful stimuli. Such a response likely involves a range of neurobiological and physiological mechanisms aimed at maintaining internal homeostasis and balance within the body. These findings further underscore the complexity of pain processing in the brain and the significant role played by the INS in this process.
Previous brain neuroimaging studies focusing on pain have identified a pain matrix [68, 69], which consists of the S1, INS, secondary somatosensory cortex, PFC, and limbic system, representing the perceived intensity and unpleasantness elicited by nociceptive stimuli [70]. The S1, secondary sensory cortex, and posterior INS of the pain matrix were associated with the sensory component of nociception, whereas the anterior INS was associated with the affective component of nociception [13, 71]. Moreover, the S1and PFC are the initial regions of the descending pain regulation pathway, which may directly or indirectly act on the trigeminal nerve complex via the trigemino-thalamo-cortical nociceptive pathway to exhibit the regulatory function of the input nociceptive signals [13, 72]. It has been pointed out that abnormal functional connectivity patterns between the S1 and PFC may imply dysfunction in the encoding of pain sensory and affective dimensions [56, 73], which may lead to regulatory deficits in the descending pathway and cause prolonged pain states. Furthermore, recent neuroimaging studies on whole-brain functional connectivity analysis showed that the abnormal functional connectivity patterns of the pain matrix played an important role in chronic migraine progression [68, 74]. Moreover, an arterial spin labeling study showed that NSAIDs achieved analgesia by inhibiting neural activity in the brain regions of the descending pain regulatory pathway [20]. In addition, patients with migraine experience a loss of volume in the left somatosensory cortex [57], suggesting larger volume of the left S1 positively contributes to predicting therapeutic outcomes, indicating a compensatory mechanism for responding to pain signals [65]. Based on our findings, we inferred that the altered functional and structural characterizations of brain regions in the descending pain regulatory pathway were involved in the neural mechanism of migraine progression and pharmacological treatment.
The present study is of great importance because it enhanced our understanding by revealing that the multimodal neuroimaging features of the TVS possess the potential to serve as neural biomarkers for migraine treatment. Such insights deepen the current understanding of migraine-related neuropathological mechanisms and medication-related analgesic mechanisms. We believe that this study may contribute to the field forward because these findings may assist in providing precise clinical interventions to shorten the disease course and prevent further deterioration. Furthermore, with the increasing use of NSAIDs worldwide [7], the ability to predict the outcome of NSAIDs treatment would facilitate the development of individualized treatment plans and promote their wider application. In addition, previous research has suggested that the functional and structural alterations present in patients with migraine can serve as predictive indicators for the efficacy of migraine treatments [75,76,77]. Although the neuroimaging characteristics of these predictive brain regions exhibit some degree of consistency with our results, there remains a lack of a cohesive neural mechanism to effectively elucidate the combined influence of functional and structural factors on treatment efficacy. These investigations indicate that the impact of pain on the brain entails intricate interactions between functional and structural components, resulting in enduring alterations in pain perception, emotional reactivity, and cognitive processing, particularly pronounced in individuals experiencing chronic pain. As such, effective pain management strategies should acknowledge these complex cerebral changes and seek integrated approaches to mitigate pain and enhance overall quality of life.
This study has certain limitations that need to be addressed to enhance its overall validity and reliability. First, it is a single-center study with a limited amount of data. External validation was conducted with other pain disorders rather than migraine for predicting the analgesic effects. Conducting multicenter studies, including external NSAIDs-treated migraine cohorts, increasing sample sizes, and improving the stability, credibility, and generalizability of existing data are imperative in future research. Second, although the study predicted the outcome of NSAIDs based on baseline data, it could not reflect the causal relationship between changes in neuroimaging characteristics and the effects of drugs. Therefore, further longitudinal studies are needed to overcome this limitation. Third, self-reported drug consumption information and the lack of compliance may affect the effectiveness of the study. Due to the low compliance with oral analgesics, the establishment of stringent and standardized treatment protocols is challenging. This is particularly true for patients with migraine, who frequently modify their drug dosage in response to the perceived severity of pain during headache episodes. Addressing these issues is essential for the advancement of migraine treatment research. Lastly, chronic pain syndromes are often accompanied by comorbid psychological and psychiatric conditions. Despite our efforts to balance anxiety and depression scores between the two migraine groups, the quantification of participants' psychological states within a rigorous quantitative framework continues to pose a substantial challenge [78]. Computational psychophysiology, an emerging methodology, offers a novel pathway to decipher the intricate associations linking psychological and physiological parameters [79]. This approach is particularly well-suited to the advancement of personalized and precision medicine. The incorporation of computational psychophysiology to develop predictive models for treatment outcomes represents a promising frontier for future research, deserving of in-depth investigation and refinement.
Conclusions
In conclusion, this study explored potential neuroimaging biomarkers of nociceptive modulation and showed that the multimodal features of the TVS had promising prospects for predicting the efficacy of NSAIDs in individual episodic migraine management. This will help orient pharmacological strategies and optimize the distribution of medical resources, thereby achieving the ultimate goal of enhancing migraine treatment outcomes.
Availability of data and materials
The data used and analyzed in this study are available from the corresponding author upon reasonable request.
Abbreviations
- BACC:
-
Balance accuracy
- CBF:
-
Cerebral blood flow
- CEN:
-
Central executive network
- DMN:
-
Default mode network
- DT:
-
Decision tree
- ENet:
-
Elastic network
- fALFF:
-
Fractional amplitude of low frequency fluctuations
- GAD-7:
-
Generalized Anxiety Disorder 7-Item
- GMV:
-
Gray matter volume
- HIT-6:
-
Headache Impact Test 6-Item
- ICHD:
-
International Classification of Headache Disorders
- INS:
-
Insula
- KNN:
-
K-nearest neighbor
- LASSO:
-
Least absolute shrinkage and selection operator
- Lightgbm:
-
Light gradient boosting machine
- LR:
-
Logistic regression
- MIDAS:
-
Migraine Disability Assessment Scale
- ML:
-
Machine learning
- MLP:
-
Multilayer perceptron
- MNI:
-
Montreal Neurological Institute
- NPV:
-
Negative predictive value
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- PCU:
-
Precuneus; PerAF, percent amplitude of fluctuation
- PFC:
-
Prefrontal cortex
- PHQ-9:
-
Patient Health Questionnaire 9-Item
- PoCG:
-
Postcentral gyrus
- PPV:
-
Positive predictive value
- PRAUC:
-
Area under the precision-recall curve
- PSM:
-
Propensity score matching
- PSQI:
-
Pittsburgh Sleep Quality Index
- RF:
-
Random forest
- RMS:
-
Root mean square
- ROCAUC:
-
Area under the receiver operating characteristic
- S1:
-
Primary sensory cortex
- SFG:
-
Superior frontal gyrus
- SMN:
-
Sensorimotor network
- SN:
-
Salience network
- SVM-RFE:
-
Support vector machine recursive feature elimination
- TTG:
-
Transverse temporal gyrus
- TVS:
-
Trigeminovascular system
- VAS:
-
Visual Analogue Scale
- Xgboost:
-
Extreme gradient boosting
References
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1204–1222
Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z (2020) Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain 21(1):137
Patel R, Dickenson AH (2022) Neuropharmacological basis for multimodal analgesia in chronic pain. Postgrad Med 134(3):245–259
Simonetta I, Riolo R, Todaro F, Tuttolomondo A (2022) New insights on metabolic and genetic basis of migraine: novel impact on management and therapeutical approach. Int J Mol Sci 23(6):3018
Charles A (2018) The pathophysiology of migraine: implications for clinical management. Lancet Neurol 17(2):174–182
Clemow DB, Johnson KW, Hochstetler HM, Ossipov MH, Hake AM, Blumenfeld AM (2020) Lasmiditan mechanism of action-review of a selective 5-HT(1F) agonist. J Headache Pain 21(1):71
Ashina M (2020) Migraine. N Engl J Med 383(19):1866–1876
Scuteri D, Adornetto A, Rombola L, Naturale MD, Morrone LA, Bagetta G et al (2019) New trends in migraine pharmacology: targeting calcitonin gene-related peptide (CGRP) with monoclonal antibodies. Front Pharmacol 10:363
Agrawal L, Korkutata M, Vimal SK, Yadav MK, Bhattacharyya S, Shiga T (2020) Therapeutic potential of serotonin 4 receptor for chronic depression and its associated comorbidity in the gut. Neuropharmacology 166:107969
Cabassi A, Tedeschi S, Perlini S, Verzicco I, Volpi R, Gonzi G et al (2020) Non-steroidal anti-inflammatory drug effects on renal and cardiovascular function: From physiology to clinical practice. Eur J Prev Cardiol 27(8):850–867
Bindu S, Mazumder S, Bandyopadhyay U (2020) Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: a current perspective. Biochem Pharmacol 180:114147
Ashina M, Hansen JM, Do TP, Melo-Carrillo A, Burstein R, Moskowitz MA (2019) Migraine and the trigeminovascular system-40 years and counting. Lancet Neurol 18(8):795–804
Goadsby PJ, Holland PR, Martins-Oliveira M, Hoffmann J, Schankin C, Akerman S (2017) Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev 97(2):553–622
Russo A, Silvestro M, Trojsi F, Bisecco A, De Micco R, Caiazzo G et al (2020) Cognitive networks disarrangement in patients with migraine predicts cutaneous allodynia. Headache 60(7):1228–1243
Russo A, Silvestro M, Tessitore A, Tedeschi G (2019) Functional neuroimaging biomarkers in migraine: diagnostic, prognostic and therapeutic implications. Curr Med Chem 26(34):6236–6252
Kesserwani H (2021) Migraine triggers: an overview of the pharmacology, biochemistry, atmospherics, and their effects on neural networks. Cureus 13(4):e14243
Weiller C, May A, Limmroth V, Juptner M, Kaube H, Schayck RV et al (1995) Brain stem activation in spontaneous human migraine attacks. Nat Med 1(7):658–660
Maizels M, Aurora S, Heinricher M (2012) Beyond neurovascular: migraine as a dysfunctional neurolimbic pain network. Headache 52(10):1553–1565
Xiang Y, Wang Y, Gao S, Zhang X, Cui R (2018) Neural mechanisms with respect to different paradigms and relevant regulatory factors in empathy for pain. Front Neurosci 12:507
Hodkinson DJ, Khawaja N, O’Daly O, Thacker MA, Zelaya FO, Wooldridge CL et al (2015) Cerebral analgesic response to nonsteroidal anti-inflammatory drug ibuprofen. Pain 156(7):1301–1310
Hua T, Chen B, Lu D, Sakurai K, Zhao S, Han BX et al (2020) General anesthetics activate a potent central pain-suppression circuit in the amygdala. Nat Neurosci 23(7):854–868
Bumgarner JR, Becker-Krail DD, White RC, Nelson RJ (2022) Machine learning and deep learning frameworks for the automated analysis of pain and opioid withdrawal behaviors. Front Neurosci 16:953182
Khosla M, Jamison K, Ngo GH, Kuceyeski A, Sabuncu MR (2019) Machine learning in resting-state fMRI analysis. Magn Reson Imaging 64:101–121
Zhang Q, Wu Q, Zhang J, He L, Huang J, Zhang J et al (2016) Discriminative analysis of migraine without aura: Using functional and structural MRI with a multi-feature classification approach. PLoS One 11(9):e163875
Zhu B, Coppola G, Shoaran M (2019) Migraine classification using somatosensory evoked potentials. Cephalalgia 39(9):1143–1155
Yin T, Sun G, Tian Z, Liu M, Gao Y, Dong M et al (2020) The spontaneous activity pattern of the middle occipital gyrus predicts the clinical efficacy of acupuncture treatment for migraine without aura. Front Neurol 11:588207
Cheng S, Zhang X, Zheng H, Jiang N, Zhou J, Li X et al (2022) Efficacy prediction of acupuncture treatment for migraine without aura based on multimodal MRI: a study protocol. Front Neurol 13:953921
Liu J, Mu J, Chen T, Zhang M, Tian J (2019) White matter tract microstructure of the mPFC-amygdala predicts interindividual differences in placebo response related to treatment in migraine patients. Hum Brain Mapp 40(1):284–292
Jia XZ, Sun JW, Ji GJ, Liao W, Lv YT, Wang J et al (2020) Percent amplitude of fluctuation: a simple measure for resting-state fMRI signal at single voxel level. PLoS One 15(1):e227021
Headache Classification Committee of the International Headache Society (IHS) (2013) The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 33(9):629–808
Pointer JS (2004) A novel visual analogue scale (VAS) device: an instrument based on the VAS designed to quantify the subjective visual experience. Ophthal Physl Opt 24(3):181–185
Shin HE, Park JW, Kim YI, Lee KS (2008) Headache Impact Test-6 (HIT-6) scores for migraine patients: their relation to disability as measured from a headache diary. J Clin Neurol 4(4):507
Rodriguez-Almagro D, Achalandabaso A, Rus A, Obrero-Gaitan E, Zagalaz-Anula N, Lomas-Vega R (2020) Validation of the Spanish version of the migraine disability assessment questionnaire (MIDAS) in university students with migraine. Bmc Neurol 20(1):67
Seo J, Park S (2015) Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain 16(1):1–7
Seo J, Park S (2015) Validation of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with migraine. J Headache Pain 16(1):1–7
Larche CL, Plante I, Roy M, Ingelmo PM, Ferland CE (2021) The Pittsburgh Sleep Quality Index: reliability, factor structure, and related clinical factors among children, adolescents, and young adults with chronic pain. Sleep Disord 2021:1–8
Jia XZ, Wang J, Sun HY, Zhang H, Liao W, Wang Z et al (2019) RESTplus: an improved toolkit for resting-state functional magnetic resonance imaging data processing. Sci Bull (Beijing) 64(14):953–954
Ning Y, Ong M, Chakraborty B, Goldstein BA, Ting D, Vaughan R et al (2022) Shapley variable importance cloud for interpretable machine learning. Patterns (N Y) 3(4):100452
Tetreault P, Mansour A, Vachon-Presseau E, Schnitzer TJ, Apkarian AV, Baliki MN (2016) Brain connectivity predicts placebo response across chronic pain clinical trials. Plos Biol 14(10):e1002570
Kelkar S, Nailwal N, Bhatia NY, Doshi G, Sathaye S, Godad AP (2022) An update on proficiency of voltage-gated ion channel blockers in the treatment of inflammation-associated diseases. Curr Drug Targets 23(14):1290–1303
Shiers S, Price TJ (2020) Molecular, circuit, and anatomical changes in the prefrontal cortex in chronic pain. Pain 161(8):1726–1729
De Ridder D, Vanneste S, Smith M, Adhia D (2022) Pain and the triple network model. Front Neurol 13:757241
Dadario NB, Sughrue ME (2023) The functional role of the precuneus. Brain 146(9):3598–3607
Mohan A, Roberto AJ, Mohan A, Lorenzo A, Jones K, Carney MJ et al (2016) The significance of the default mode network (DMN) in neurological and neuropsychiatric disorders: a review. Yale J Biol Med 89(1):49–57
Benarroch EE (2019) Insular cortex: functional complexity and clinical correlations. Neurology 93(21):932–938
Labrakakis C (2023) The role of the insular cortex in pain. Int J Mol Sci 24(6):5736
Menon B (2019) Towards a new model of understanding - the triple network, psychopathology and the structure of the mind. Med Hypotheses 133:109385
Mastria G, Scaliti E, Mehring C, Burdet E, Becchio C, Serino A et al (2023) Morphology, connectivity, and encoding features of tactile and motor representations of the fingers in the human precentral and postcentral gyrus. J Neurosci 43(9):1572–1589
Diguiseppi J, Tadi P (2024) Neuroanatomy, postcentral gyrus
Morosan P, Rademacher J, Schleicher A, Amunts K, Schormann T, Zilles K (2001) Human primary auditory cortex: cytoarchitectonic subdivisions and mapping into a spatial reference system. Neuroimage 13(4):684–701
Wei J, Wang X, Cui X, Wang B, Xue J, Niu Y et al (2022) Functional integration and segregation in a multilayer network model of patients with Schizophrenia. Brain Sci 12(3):368
Lim M, Jassar H, Kim DJ, Nascimento TD, Dasilva AF (2021) Differential alteration of fMRI signal variability in the ascending trigeminal somatosensory and pain modulatory pathways in migraine. J Headache Pain 22(1):4
Tsai YH, Liang X, Yang JT, Hsu LM (2019) Modular organization of brain resting state networks in patients with classical trigeminal neuralgia. Neuroimage Clin 24:102027
Liu J, Hao Y, Du M, Wang X, Zhang J, Manor B et al (2013) Quantitative cerebral blood flow mapping and functional connectivity of postherpetic neuralgia pain: a perfusion fMRI study. Pain 154(1):110–118
Liu J, Zhang F, Liu X, Zhuo Z, Wei J, Du M et al (2018) Altered small-world, functional brain networks in patients with lower back pain. Sci China Life Sci 61(11):1420–1424
Peng K, Karunakaran KD, Labadie R, Veliu M, Cheung C, Lee A et al (2021) Suppressed prefrontal cortex oscillations associate with clinical pain in fibrodysplasia ossificans progressiva. Orphanet J Rare Dis 16(1):54
Bonanno L, Lo BV, De Salvo S, Ruvolo C, Torre V, Bramanti V et al (2020) Brain morphologic abnormalities in migraine patients: an observational study
Wei HL, Chen J, Chen YC, Yu YS, Guo X, Zhou GP et al (2020) Impaired effective functional connectivity of the sensorimotor network in interictal episodic migraineurs without aura. J Headache Pain 21(1):111
Huang J, Duan Y, Liu S, Liang P, Ren Z, Gao Y et al (2018) Altered brain structure and functional connectivity of primary visual cortex in optic neuritis
Jimenez-Marin A, Rivera D, Boado V, Diez I, Labayen F, Garrido I et al (2020) Brain connectivity and cognitive functioning in individuals six months after multiorgan failure. Neuroimage Clin 25:102137
Herold F, Torpel A, Schega L, Muller NG (2019) Functional and/or structural brain changes in response to resistance exercises and resistance training lead to cognitive improvements: a systematic review. Eur Rev Aging Phys Act 16:10
Grieve SM, Clark CR, Williams LM, Peduto AJ, Gordon E (2005) Preservation of limbic and paralimbic structures in aging. Hum Brain Mapp 25(4):391–401
Maleki N, Barmettler G, Moulton EA, Scrivani S, Veggeberg R, Spierings E et al (2015) Female migraineurs show lack of insular thinning with age. Pain 156(7):1232–1239
Maleki N, Linnman C, Brawn J, Burstein R, Becerra L, Borsook D (2012) Her versus his migraine: multiple sex differences in brain function and structure
Melum TA, Vangberg TR, Johnsen LH, Steingrimsdottir OA, Stubhaug A, Mathiesen EB et al (2023) Gray matter volume and pain tolerance in a general population: the Tromso study. Pain 164(8):1750–1758
Tsagareli N, Tsiklauri N, Kvachadze I, Tsagareli MG (2020) Endogenous opioid and cannabinoid systems contribute to antinociception produced by administration of NSAIDs into the insular cortex of rats. Biomed Pharmacother 131:110722
Fu C, Zhang Y, Ye Y, Hou X, Wen Z, Yan Z et al (2022) Predicting response to tVNS in patients with migraine using functional MRI: a voxels-based machine learning analysis. Front Neurosci 16:937453
Lee MJ, Park BY, Cho S, Kim ST, Park H, Chung CS (2019) Increased connectivity of pain matrix in chronic migraine: a resting-state functional MRI study. J Headache Pain 20(1):29
Salomons TV, Iannetti GD, Liang M, Wood JN (2016) The, “pain matrix” in pain-free individuals. Jama Neurol 73(6):755–756
Legrain V, Iannetti GD, Plaghki L, Mouraux A (2011) The pain matrix reloaded: a salience detection system for the body. Prog Neurobiol 93(1):111–124
Eisenberger NI (2015) Social pain and the brain: controversies, questions, and where to go from here. Annu Rev Psychol 66:601–629
Lorenz J, Minoshima S, Casey KL (2003) Keeping pain out of mind: the role of the dorsolateral prefrontal cortex in pain modulation. Brain 126(Pt 5):1079–1091
Kim J, Mawla I, Kong J, Lee J, Gerber J, Ortiz A et al (2019) Somatotopically specific primary somatosensory connectivity to salience and default mode networks encodes clinical pain. Pain 160(7):1594–1605
Coppola G, Di Renzo A, Petolicchio B, Tinelli E, Di Lorenzo C, Parisi V et al (2019) Aberrant interactions of cortical networks in chronic migraine: a resting-state fMRI study. Neurology 92(22):e2550–e2558
Yang XJ, Liu L, Xu ZL, Zhang YJ, Liu DP, Fishers M et al (2020) Baseline brain gray matter volume as a predictor of acupuncture outcome in treating migraine
Hong J, Sun J, Zhang L, Tan Z, Chen Y, Chen Q et al (2022) Neurological mechanism and treatment effects prediction of acupuncture on migraine without aura: study protocol for a randomized controlled trial
Wu J, Lai PY, Chen YL, Wang YF, Lirng JF, Chen ST et al (2022) The use of neuroimaging for predicting Sumatriptan treatment response in patients with migraine
Eronen MI, Bringmann LF (2021) The theory crisis in psychology: how to move forward. Perspect Psychol Sci 16(4):779–788
Hu B, Qian K, Zhang Y, Shen J, Schuller BW (2022) The inverse problems for computational psychophysiology: opinions and insights. Cyborg Bionic Syst 2022:9850248
Acknowledgements
The authors thank all participants for their participation.
Funding
This work was supported by the Science and Technology Development Project of Nanjing (YKK23220) and the Medical Imaging Artificial Intelligence Special Research Fund Project, Nanjing Medical Association Radiology Branch (NMARB202312).
Author information
Authors and Affiliations
Contributions
HLW and YSY: conception and design of the work. HLW, MYW, and GPZ: acquisition and analysis of data. HLW, YSY, and ZZ: interpretation of results. JL, HZ, and ZZ: quality control and substantive revision. HLW and YSY: manuscript writing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained through the Ethics Committee of the Affiliated Jiangning Hospital of Nanjing Medical University (20180285, 2020–03-026-K01, and 2023–03-010-K01). Informed consent was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wei, HL., Yu, YS., Wang, MY. et al. Exploring potential neuroimaging biomarkers for the response to non-steroidal anti-inflammatory drugs in episodic migraine. J Headache Pain 25, 104 (2024). https://doi.org/10.1186/s10194-024-01812-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-024-01812-4