Abstract
Background
The paroxysmal nature of migraine is a hallmark of the disease. Some patients report increased attack frequency at certain seasons or towards the end of the week, while others experience diurnal variations of migraine attack onset. This systematic review investigates the chronobiology of migraine and its relation to the periodicity of attacks in existing literature to further understand the oscillating nature of migraine.
Main body
PubMed and Embase were systematically searched and screened for eligible articles with outcome measures relating to a circadian, weekly or seasonal distribution of migraine attacks. We found that the majority of studies reported morning hours (6 am–12 pm) as the peak time of onset for migraine attacks. More studies reported Saturday as weekly peak day of attack. There was no clear seasonal variation of migraine due to methodological differences (primarily related to location), however four out of five studies conducted in Norway reported the same yearly peak time indicating a possible seasonal periodicity phenomenon of migraine.
Conclusions
The findings of the current review suggest a possible role of chronobiologic rhythms to the periodicity of migraine attacks. Future studies are, however, still needed to provide more knowledge of the oscillating nature of migraine.
Similar content being viewed by others
Background
The paroxysmal nature of migraine is a hallmark of the disease [1]. The frequency of attacks and pain-free intervals vary from patient to patient [2]. Some patients may experience increased frequency of attacks at certain times of the year [3] or towards the end of the week [4], while others report diurnal variations of migraine attack onset [5]. The mechanisms underlying the oscillating nature of migraine are unknown.
Chronobiology is the study of biological rhythms present in most life forms that inhabit the surface of the planet. The best known is the circadian ~24-hour rhythms of behavior, metabolism and physiology. There are also biological rhythms that correspond to phases of the moon or the season, while the ultradian rhythms have periods varying from several hours to minutes. Circadian rhythms have the most pervasive influence on the many functions in the human body such as blood pressure [6], sleep-wake cycles, body temperature and hormone production [7]. Circadian dysfunction is common in shift workers (~ 21 % of workers in the European Union [8]) and has been linked to a large number of health problems either as a cause or an effect [9,10,11].
In migraine, it is well established that the menstrual cycle influences the periodicity of migraine attacks for some women [12]. Migraine patients may also experience headaches awakening from sleep possibly triggered by sleep disturbances [13]. Moreover, the prevalence of migraine increases with age and peaks at 35–39 years of age, followed by a decline, showing that migraine prevalence changes according to lifespan [14]. The question is whether chronobiology, involving circadian or infradian (> 24 h) biological rhythms, influences the periodicity of migraine attacks. This aspect of periodicity in migraine has been investigated based on data collected from headache diaries, questionnaires and emergency department visits.
Here, we conducted a systematic review of the literature to identify studies that investigated the temporal distribution of migraine attacks within a circadian, weekly and seasonal time frame.
Methods
Study identification
This review has been conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines [15]. We searched PubMed and Embase to identify all possibly relevant articles. Following search string was used: Migraine AND (periodicity OR circadian OR circannual OR life span OR chronobiology OR chronology OR rhythm OR cycle OR fluctuation OR rhythmicity OR season OR nocturnal OR equinox OR solstice OR diurnal). The search was performed August 24th, 2020.
Study selection
Investigators AHP and JT independently screened all articles by title and abstract. Possible eligible articles were retrieved for full-text screening according to the pre-defined selection criteria (Table 1). Any discrepancy between the two investigators was determined by discussion. Further disagreement between the two investigators was determined by consulting a senior investigator (SY). Subsequently, a manual reference screening of the included studies and other relevant primary articles was performed to find possible eligible studies missed by the search string.
Data extraction and analysis
Data were extracted using a pre-defined form. For each included study, data on the following parameters were extracted: study site (country), study type (questionnaire, diary, emergency department), length of follow-up period, number of patients, mean age of patients, female/male-ratio, monthly frequency of headache days, comorbidities, medication and outcome variables.
The outcome variable was categorized according to the biological rhythm. Following periods were reported: circadian (C), weekly (W) and seasonal (S) distribution of migraine attacks. The three distinct predefined study types were: diary studies, questionnaire studies (relying on patients’ retrospective view of their distribution of attacks) and emergency department studies (analyzing the admittance pattern of patients with migraine diagnosis).
Predefined intervals were applied for studies reporting circadian and seasonal variations of migraine attacks to systemize the data analysis. The 24-hours of the day were categorized into 6-hour intervals: night (00:00 am–06:00 am), morning (06:00 am–12:00 pm), afternoon (12:00 pm–06:00 pm) and evening (06:00 pm–12:00 am). The seasonal distribution of attacks was categorized according to the Northern Hemisphere seasonal standards as all studies were conducted north of the Equator: winter (December–February), spring (March–May), summer (June–August) and fall (September–November).
Results
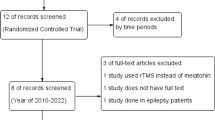
The database search resulted in 4874 articles identified through PubMed and 2867 identified through Embase (Fig. 1). Duplicates were removed and a total of 6783 unique articles were retrieved for title and abstract screening yielding 132 articles identified for full-text screening, resulting in 33 eligible articles. Additional two eligible articles were found through reference screening of the 132 full-text screened articles. In total, 35 articles met the eligibility criteria and were included for qualitative synthesis. Distribution of study type among the included articles was: 18 diary studies, 12 questionnaire studies and five emergency department studies.
Study and patient characteristics
Studies mainly included more migraine patients without aura (MO) than with aura (MA) [5, 16,17,18,19,20,21,22,23,24]. Six studies included mostly MA patients [3, 18, 25,26,27,28]. Furthermore, 12 studies only reported data from patients with episodic migraine (EM) [3, 17, 19, 22, 23, 25,26,27,28,29,30,31], while three studies reported data from both chronic migraine (CM) and EM [5, 16, 32]. One study included more patients with CM than EM [16]. All studies were conducted in the Northern Hemisphere [20, 22, 23, 29, 30, 32,33,34,35,36,37,38]. Two studies included more males than females [17, 24]. Female/male-ratio was not reported in five studies [35, 39,40,41,42]. Mean age was mostly between 30 and 50 years of age (based on 21 out of 24 studies reporting mean age), while three studies investigated a pediatric sample (4–18 years of age) [17, 24, 36] (Table 2).
Circadian distribution of migraine attacks
Fifteen studies investigated the circadian distribution of migraine onset time. Eleven of these studies reported peak time to onset of migraine attacks involving the morning hours (6 am–12 pm) (Fig. 2) [3, 5, 17, 19, 22, 26, 29, 39, 40, 42, 43]. The range of this reported peak overlapped with the nighttime/early morning time interval (3 am–5 am) in four studies [3, 19, 39, 40] and with the afternoon time interval (12 pm–6 pm) in two studies [26, 29].
Circadian (24-hour) distribution of migraine attack onset peak interval for the included studies (n = 15). One study reported migraine attack onset at any time of the day [32] and thus was not included in the figure. Horizontal black lines indicate the reported time range where most migraine attacks began as reported by the individual studies. Black dot was applied if studies reported a specific peak time. Broken lines were applied for three studies where specific time clocks were unreported [3, 23, 43]. Thus, reporting of early morning hours was estimated to 5 am–8 am [3], morning hours was estimated to 6 am–12 pm [43] and after noon was estimated to 12 pm–12 am [23]. n: total sample size
Three studies did not report peak time to onset of migraine attacks involving the morning hours (6 am – 12 pm). Hereof, one study reported peak at night time (12 am – 6 am) [44], one study reported peak after noon (12 pm – 12 am) [23], while one study calculated peak of attack onset time to 4.48 pm [24]. One study reported migraine attack onset to be at any time of the day [32].
Weekly and seasonal distribution of migraine attacks
Ten studies reported data regarding the weekly distribution of attacks, which is visualized in Fig. 3. Four of the studies reported Saturday as the day of the week where patients experienced more migraine [18, 31, 45, 46]. Twenty-one studies had outcome measures related to seasonal or yearly distribution of migraine attacks. This is visualized in Fig. 4, where studies are grouped according to geographical location. Four out of five studies, conducted in Northern Norway, showed peak of migraine attack frequency during polar light season (May 21st to July 21st [27]), while four out of six studies, in other European countries, most frequently reported peak time interval of migraine attacks during winter [24, 40, 41, 47]. North American studies (n = 5) reported peak period of migraine attacks mainly during spring and summer (n = 3) [35, 37, 38]. A Nigerian study reported peak of migraine attacks during the dry period (October–May) [34], while one Taiwanese study demonstrated peak during spring and winter [30]. Four studies reported no peak of migraine attack frequency throughout the year [18,19,20,21].
Weekly distribution of migraine attacks. The number of studies reporting migraine attack frequency peak on each day of the week. Three studies found that attacks were equally distributed throughout the week [19, 25, 42]. One study found that there were fewer migraine attacks on Sundays compared to other days of the week [25]. n: total sample size
Seasonal distribution of migraine attacks. Horizontal black lines indicate the reported time of year for peak in migraine attack frequency. Broken lines represent estimated dates based on definition of the polar light season in Tromsø (May 21st –July 21st ) [27] as exact dates were not specified by authors. Four studies on the seasonal distribution reported no peak of migraine attack frequency throughout the year [18,19,20,21]. Black dot indicates peak date. n: total sample size, N: north (latitude), E: east (longitude), W: west (longitude), MA: migraine with aura. MO: migraine without aura. CL: confidence level. *Data only obtained by those who answered yes to experiencing a seasonal variation of migraine attacks. **Results estimated from figure. Increased headache frequency in spring is more prevalent for MA compared to MO patients. *** This study followed patients for two consecutive years. In the first year, there was no pattern in regard to distribution of migraine attack frequency. In the subsequent year, there was however a monthly variation of attack frequency with a peak in March. **** Temperature sensitive patients showed migraine attack frequency peak in winter and non-temperature sensitive patients had more migraine attacks during spring
Discussion
This systematic review revealed the association between circadian, weekly and seasonal rhythms and migraine attack periodicity. The majority of studies reported morning hours as being the time of day where most migraine attacks began. Only two studies reported their entire peak of attack onset interval being between 12 pm and 12 am [23, 24]. However, this could be explained by methodological differences such as age differences [24] and study type [23]. The migraine attack onset in morning hours is further confirmed by drug intervention studies [48, 49]. These findings point towards a possible role of the circadian clock in migraine.
This review further revealed a pattern of weekly distribution of migraine attacks. It has been shown that migraine attack frequency rises towards the end of the week peaking on Saturdays [18, 31, 45, 46]. Three [19, 25, 42] out of the ten studies included in the weekly attack distribution analysis could not demonstrate a weekly periodicity phenomenon and reported that migraine attacks were distributed equally throughout the week. It is unlikely that an endogenous infradian rhythm is responsible for migraine attacks being more prevalent on Saturdays than other weekdays. Instead, environmental factors are a more plausible explanation as the transition from weekdays to weekend often is accompanied by life-style changes such as a reduction of perceived stress and changes in alcohol and caffeine consumption [50, 51]. Interestingly, one study found that only patients with a job, and not unemployed patients, experienced fewer migraine attacks on Sundays, indicating that work and work-related stress could influence the weekly pattern of migraine [25].
Seasonal variation of migraine attacks was less clear. Most studies reported that migraine attack frequency was raised during winter and spring rather than summer and fall (Fig. 4). In northern Norway, patients had more migraine attacks during the polar light season (May 21st –July 21st [27]) [3, 16, 27, 52]. Interestingly, two out of four studies only reported this periodicity phenomenon for MA patients and not for the MO patients [3, 27]. One Norwegian study reported no seasonal peak [21]. Given that studies have been conducted at different locations around the world, it is difficult to point at one certain time of the year being worse than another for migraine patients. However, the Norwegian studies suggested that there was a circannual or seasonal periodicity of migraine when comparing studies conducted in the same area with the same climate and endogenous clock settings [3, 16, 27, 52].
Limitations
The present systematic review revealed limitations of studies investigating a circadian, weekly, and seasonal biological rhythm. Therefore, caution is needed in interpreting the results of these studies. First, the studies were of three distinct study types (diary, emergency department and questionnaire studies) and thus difficult to compare. Headache diary studies may be preferable due to the prospective data collection. Self-reported questionnaire studies are subject to confirmation and recall bias since they rely on patients’ retrospective view of their migraine attack distribution. A recent study showed that patients tend to underestimate their headache frequency using retrospective questionnaire compared to headache diaries [53]. Periodicity of migraine attacks in the emergency department studies might be influenced by various factors. Patients may seek the emergency department due to a long-lasting migraine attack or status migrainosus, and exact time of onset of migraine attack is not routinely recorded. Due to the potential methodological reservations, we marked the emergency department studies separately in this review.
Second, the sample size of the included studies varied widely between and within study types which challenge interpretation of data. Nevertheless, the sample size was relatively larger of studies supporting the circadian pattern of morning hours as the most common time to onset of attacks and Sundays as the potential weekday with peak attack frequency.
Third, the reviewed studies were conducted at different geographical locations and therefore only few studies were comparable regarding the ratio of light to dark hours of the day throughout the year. Melatonin production is the internal representative of the external photoperiod and hereby functions as a chronobiotic hormonal signal controlling both the circadian and circannual rhythms [54]. Thus, only studies with close proximity of geographical location should be compared regarding seasonal variation of migraine to exclude limitations due to different endogenous clock settings.
Fourth, several of the reviewed studies reported other primary outcomes such as the association of migraine to weather [18,19,20, 30, 33, 34, 40,41,42, 46] and sleep [17, 29]. Thus, these studies were not designed to mainly consider the periodicity of migraine attacks. Weather and altered sleep rhythm are both considered triggers of migraine and may potentially influence the findings [55].
Fifth, there was lack of information on the clinical characteristics of migraine (e.g., migraine phenotype, attack frequency) in several studies. Periodicity of migraine attacks might differ between patients with and without aura as shown in the reviewed studies [3, 27]. Many studies did not account for whether the attacks experienced by patients were phenotypically migraine attacks. Moreover, it is unclear how many migraine days were reported according to the headache classification, since several studies merely applied the terminology headache days per month. Attack frequency is an important aspect to consider since it would be difficult to estimate a clear pattern of periodicity in CM patients [5].
Finally, several studies failed to provide information on medication use and comorbidities. Certain drugs and diseases can influence the circadian clock system [56, 57] and consequently the periodicity of migraine. Patients using beta-blockers as preventive treatment or oral contraceptives (common treatment of menstrual migraine) had onset of migraine later in the day (4 pm and 3 pm) compared to non-drug users [26]. Furthermore, depression, a common co-morbidity to migraine [58], has been linked to a disruption of the circadian clock system and therefore might have influenced the data [59].
Lessons learned and future directions
Future research on chronobiology of migraine, including circadian and circannual periodicity, should take into consideration the limitations presented in this review. Studies with refined design aimed to specifically investigate the periodicity of migraine attacks are needed to provide further information on the chronobiology of migraine. As such, prospective diary studies are preferred for data collection following a large sample of well-characterized episodic migraine patients (without preventive treatment). By following the patients for at least one year, we would further be able to establish whether weekly and/or seasonal periodicity is a phenomenon of migraine. Investigations of MA patients separately, and comparing them to MO patients, could reveal if MA patients are more susceptible to seasonal changes. Sex should also be considered in future studies and assessed separately due to the possible influence of menstruation on the periodicity of migraine attacks [60].
Hypothalamus and the pineal gland (hereof melatonin) may be involved in the chronobiology of migraine, since these are the brain structures responsible for circadian and circannual rhythms [61, 62]. Two functional magnetic resonance imaging studies scanned episodic MO patients continuously every morning for 30 days to investigate the hypothalamic activation in migraine [63, 64]. One of the studies reported that hypothalamus was activated up to 48 h before migraine onset [63], while the case study reported increased coupling of hypothalamus to the spinal trigeminal nuclei, 24 h before attack onset, and to the dorsal rostral pons during attacks [64]. This points towards a potential role of the hypothalamus in attack initiation [65]. However, since the time to onset of migraine was not reported in the two neuroimaging studies it is unclear whether the observed hypothalamic activation plays a role in the circadian periodicity. We suggest looking further into a possible role of the hypothalamus to investigate potential underlying mechanisms.
The pineal gland produces melatonin, commonly known as the sleep hormone, which is regulated by the suprachiasmatic nucleus of the hypothalamus, and thus involved in modulating the internal sleep-wake cycle and endogenous biologic timekeeping [66, 67]. The regulation of circadian rhythms is complex and multifactorial [68]. Melatonin has been shown to play a role in regulating the levels of GABA, nitric oxide and CGRP as well as modulating trigeminal activation and neuroinflammation, which are factors involved in the migraine pathophysiology [54]. The question is whether a dysfunction of the retino-hypothalamic-pineal system could influence the circadian timing of migraine onset. A recent systematic review and meta-analysis reported lower levels of nocturnal serum melatonin and urine 6-sulphatoxymelatonin (melatonin metabolite discarded by the urine) in migraine patients compared to healthy controls and that melatonin may be useful as preventive treatment [69].
Interestingly, migraine patients may be less prone to a normal circadian chronotype and more sensitive to changes in their circadian rhythm compared to healthy controls [44]. In support, patients commonly report sleep disturbances as a trigger of migraine [55] and one may suspect that poor sleep quality promote the onset of migraine in the morning hours [13]. However, a recent actigraphy study, investigating patients for six consecutive weeks, reported no association between sleep disturbances and migraine the following day [70]. Further research is needed to establish whether sleep disturbance, low melatonin levels or other regulators of sleep and the circadian clock system, play a role in the periodicity of migraine attacks.
Another question is how periodicity can explain the varying attack frequency within and between patients. Attacks can be triggered by glyceryl trinitrate infusion with the same incidence and severity between patients with rare (≤ 4/year) and frequent (≥ 12/year) migraine attacks [71]. Thus, it is likely that other factors may also be at play.
Migraine patients generally report discomfort to light outside attacks as well [72]. Exposure to light (e.g. amount and intensity) may change across seasons of the year and thus play a role in the migraine periodicity phenomenon. Of note, experimental exposure to photic stimulation was not able to induce migraine attacks in patients reporting light as a common migraine trigger [73]. Nevertheless, abnormal modulation of the complex retino-thalamocortical pathway has been suggested to be involved in photophobia of migraine, which needs further research [74].
Conclusions
Migraine attacks seem to begin in the morning hours pointing towards a possible role of the circadian clock in migraine. Seasonal and weekly distributions of migraine attacks are less clear, possibly due to heterogeneity within the existing literature. Future studies are needed to further investigate and expand our understanding of the role of chronobiology in the paroxysmic nature of migraine making this an interesting topic for future migraine research.
Availability of data and materials
The data used in the present review are available from the corresponding author upon reasonable request.
Abbreviations
- C:
-
Circadian
- W:
-
Weekly
- S:
-
Seasonal
- N:
-
Number of patients
- NA:
-
Not applicable
- EM:
-
Episodic migraine
- PCOS:
-
Poly Cystic Ovary Syndrome
- OC:
-
Oral Contraceptives
- MO:
-
Migraine without aura
- MA:
-
Migraine with aura
- MX:
-
Migraine, not specified as migraine with or without aura
- NR:
-
Not reported
- ED:
-
Emergency Department
- CM:
-
Chronic Migraine
- HM:
-
Hemiplegic Migraine
- TTH:
-
Tension Type Headache
- SD:
-
Standard deviation
- CL:
-
Confidence-level
References
Ashina M (2020) Migraine. N Engl J Med 383(19):1866-1876
Dodick DW. Migraine (2018) Lancet 391(10127):1315–1330
Alstadhaug KB, Salvesen R, Bekkelund SI (2005) Seasonal variation in migraine. Cephalalgia 25(10):811–816
Torelli P, Cologno D, Manzoni GC (1999) Weekend headache: A possible role of work and life-style. Headache 39(6):398–408
de Tommaso M, Delussi M (2018) Circadian rhythms of migraine attacks in episodic and chronic patients: A cross sectional study in a headache center population. BMC Neurol 18(1):1–10
Smolensky MH, Hermida RC, Portaluppi F (2017) Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Med Rev [Internet]. 2017;33:4–16. Available from: https://doi.org/10.1016/j.smrv.2016.02.003
Loddenkemper T, Lockley SW, Kaleyias J, Kothare SV (2011) Chronobiology of epilepsy: Diagnostic and therapeutic implications of chrono-epileptology. J Clin Neurophysiol 28(2):146–153
Eurofound (2017), Sixth European Working Conditions Survey – Overview report (2017 update), Publications Office of the European Union, Luxembourg.
Kecklund G, Axelsson J (2016) Health consequences of shift work and insufficient sleep. BMJ 355:1–13
Khan S, Nobili L, Khatami R, Loddenkemper T, Cajochen C, Dijk DJ et al. (2018) Circadian rhythm and epilepsy. Lancet Neurol 17(12):1098–108
Videnovic A, Lazar AS, Barker RA, Overeem S (2014) “The clocks that time us” - Circadian rhythms in neurodegenerative disorders. Nat Rev Neurol 10(12):683–93
Maasumi K, Tepper SJ, Kriegler JS (2017) Menstrual Migraine and Treatment Options. Review Headache 57(2):194–208
Kelman L, Rains JC (2005) Headache and sleep: Examination of sleep patterns and complaints in a large clinical sample of migraineurs. Headache 45(7):904–910
Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM et al (2018) Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17(11):954–976
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 339(7716):332–336
Bekkelund SI, Müller KI, Wilhelmsen A, Alstadhaug KB (2017) Photophobia and Seasonal Variation of Migraine in a Subarctic Population. Headache 57(8):1206–1216
Bruni O, Russo PM, Violani C, Guidetti V (2004) Sleep and migraine: an actigraphic study. Cephalalgia 24(8):134–139
Gomersall JD, Stuart A (1973) Variations in migraine attacks with changes in weather conditions. Int J Biometeorol 17(3):285–299
Hoffmann J, Lo H, Neeb L, Martus P, Reuter U (2011) Weather sensitivity in migraineurs. J Neurol 258(4):596–602
Kimoto K, Aiba S, Takashima R, Suzuki K, Takekawa H, Watanabe Y et al (2011) Influence of barometric pressure in patients with migraine headache. Intern Med 50(18):1923–1928
Lilleng H, Bekkelund S (2009) Seasonal variation of migraine in an arctic population. Headache 49(5):721–725
Park JW, Cho SJ, Park SG, Chu MK (2018) Circadian variations in the clinical presentation of headaches among migraineurs: A study using a smartphone headache diary. Chronobiol Int 35(4):546–54
Shin YW, Park HJ, Shim JY, Oh MJ, Kim M (2015) Seasonal Variation, Cranial Autonomic Symptoms, and Functional Disability in Migraine: A Questionnaire-Based Study in Tertiary Care. Headache 55(8):1112–1123
Soriani S, Fiumana E, Manfredini R, Boari B, Battistella PA, Canetta E et al (2006) Circadian and seasonal variation of migraine attacks in children. Headache 46(10):1571–1574
Alstadhaug KB, Salvesen R, Bekkelund S (2007) Weekend migraine. Cephalalgia 27(4):343–346
Alstadhaug K, Salvesen R, Bekkelund S (2008) 24-Hour distribution of migraine attacks. Headache 48(1):95–100
Alstadhaug KB, Bekkelund S, Salvesen R (2007) Circannual periodicity of migraine? Eur J Neurol 14(9):983–988
Morrison DP (1990) Occupational Stress in Migraine is Weekend Headache a Myth or Reality? Cephalalgia 10(4):189–193
Vgontzas A, Li W, Mostofsky E, Rueschman M, Mittleman MA, Bertisch SM (2020) Associations between migraine attacks and nightly sleep characteristics among adults with episodic migraine: a prospective cohort study. Sleep 43(7):zsaa001
Yang AC, Fuh JL, Huang NE, Shia BC, Wang SJ (2015) Patients with migraine are right about their perception of temperature as a trigger: time series analysis of headache diary data. J Headache Pain 16:49. Available from: https://doi.org/10.1186/s10194-015-0533-5
Drescher J, Wogenstein F, Gaul C, Kropp P, Reinel D, Siebenhaar Y et al (2019) Distribution of migraine attacks over the days of the week: Preliminary results from a web-based questionnaire. Acta Neurol Scand 139(4):340–345
Kelman L (2006) Pain characteristics of the acute migraine attack. Headache 46(6):942–953
Villeneuve PJ, Szyszkowicz M, Stieb D, Bourque DA (2006) Weather and emergency room visits for migraine headaches in Ottawa, Canada. Headache 46(1):64–72
Timothy SY, Kwanashie HO, Nyandaiti YW, Watila M, Mava Y, Sadiq GU et al (2011) Impact of weather conditions on migraine headache in north-eastern Nigeria. Int J Pharm Pharm Sci 3(SUPPL. 3):133–136
Brewerton TD, George MS (1990) A Study of the Seasonal Variation of Migraine. Headache J Head Face Pain 30(8):511–513
Caperell K, Pitetti R (2014) Seasonal variation of presentation for headache in a pediatric emergency department. Pediatr Emerg Care 30(3):174–176
Robbins L (1994) Precipitating Factors in Migraine: A Retrospective Review of 494 Patients. Headache J Head Face Pain 34(4):214–216
Szyszkowicz M, Kaplan GG, Grafstein E, Rowe BH (2009) Emergency department visits for migraine and headache: A multi-city study. Int J Occup Med Environ Health 22(3):235–242
Gori S, Morelli N, Maestri M, Fabbrini M, Bonanni E, Murri L (2005) Sleep quality, chronotypes and preferential timing of attacks in migraine without aura. J Headache Pain 6(4):258–260
Hoffmann J, Schirra T, Lo H, Neeb L, Reuter U, Martus P (2015) The influence of weather on migraine - are migraine attacks predictable? Ann Clin Transl Neurol 2(1):22–28
Marrelli A, Marini C, Prencipe M (1988) Seasonal and Meteorological Factors in Primary Headaches. Headache J Head Face Pain 28(2):111–113
Wilkinson M, Woodrow J (1979) Migraine and Weather. Headache J Head Face Pain 19(7):375–378
Knezevic-Pogancev M (2006) Specific features of migraine syndromein children. J Headache Pain 7(4):206–210
van Oosterhout WPJ, van Someren EJW, Schoonman GG, Louter MA, Lammers GJ, Ferrari MD et al (2018) Chronotypes and circadian timing in migraine. Cephalalgia 38(4):617–625
Osterman PO, Lövstrand KG, Lundberg PO, Lundquist S, Muhr C (1981) Weekly headache periodicity and the effect of weather changes on headache. Int J Biometeorol 25(1):39–45
Yilmaz M, Gurger M, Atescelik M, Yildiz M, Gurbuz S (2015) Meteorologic parameters and migraine headache: ED study. Am J Emerg Med 33(3):409–13
Cugini P, Romit A, Di Palma L, Giacovazzo M (1990) Common migraine as a weekly and seasonal headache. Chronobiol Int 7(5–6):467–469
Solomon GD (1992) Circadian rhythms and migraine. Cleve Clin J Med 59(3):326–329
Fox AW, Davis RL (1998) Migraine chronobiology. Headache 38(6):436–441
Martin VT, Vij B (2016) Diet and Headache: Part 1. Headache 56(9):1543–1552
Lipton RB, Buse DC, Hall CB, Tennen H, DeFreitas TA, Borkowski TM et al (2014) Reduction in perceived stress as a migrain. Neurology 82(16):1395–1401
Salvesen R, Bekkelund SI (2000) Migraine, as compared to other headaches, is worse daring midnight-sun summer than during polar night. A questionnaire study in an arctic population. Headache 40(10):824–829
Miller VE, Faurot KR, Palssson OS, MacIntosh BA, Suchindran C, Honvoh G et al (2020) Comparing prospective headache diary and retrospective four-week headache questionnaire over 20 weeks: Secondary data analysis from a randomized controlled trial. Cephalalgia 40(13):1523-1531
Peres MFP, Valença MM, Amaral FG, Cipolla-Neto J (2019) Current understanding of pineal gland structure and function in headache. Cephalalgia 39(13):1700–1709
Marmura MJ (2018) Triggers, Protectors, and Predictors in Episodic Migraine. Curr Pain Headache Rep 22(12):81
Stoschitzky K, Sakotnik A, Lercher P, Zweiker R, Maier R, Liebmann P et al (1999) Influence of beta-blockers on melatonin release. Eur J Clin Pharmacol 55(2):111–115
Ohdo S, Koyanagi S, Matsunaga N (2019) Chronopharmacological strategies focused on chrono-drug discovery. Pharmacol Ther 202:72–90
Burch RC, Buse DC, Lipton RB. Migraine (2019) Epidemiology, Burden, and Comorbidity. Neurol Clin 37(4):631–649
Logan RW, McClung CA (2019) Rhythms of life: circadian disruption and brain disorders across the lifespan. Nat Rev Neurosci 20(1):49–65
Vetvik KG, MacGregor EA, Lundqvist C, Russell MB (2014) Prevalence of menstrual migraine: A population-based study. Cephalalgia 34(4):280–288
Eisenstein M (2013) Stepping out of time. Nature 497:S10–S12
Johnston JD (2005) Measuring seasonal time within the circadian system: Regulation of the suprachiasmatic nuclei by photoperiod. J Neuroendocrinol 17(7):459–465
Schulte LH, Mehnert J, May A (2020) Longitudinal Neuroimaging over 30 Days: Temporal Characteristics of Migraine. Ann Neurol 87(4):646–651
Schulte LH, May A (2016) The migraine generator revisited: Continuous scanning of the migraine cycle over 30 days and three spontaneous attacks. Brain 139(7):1987–1993
May A, Burstein R (2019) Hypothalamic regulation of headache and migraine. Cephalalgia 39(13):1710–1719
Pandi-Perumal SR, Srinivasan V, Maestroni GJM, Cardinali DP, Poeggeler B, Hardeland R (2006) Melatonin: Nature’s most versatile biological signal? FEBS J 273(13):2813–2838
Pandi-Perumal SR, Trakht I, Srinivasan V, Spence DW, Maestroni GJM, Zisapel N et al (2008) Physiological effects of melatonin: Role of melatonin receptors and signal transduction pathways. Prog Neurobiol 85(3):335–353
Saper CB, Scammell TE, Lu J (2005) Hypothalamic regulation of sleep and circadian rhythms. Nature 437(7063):1257–1263
Liampas I, Siokas V, Brotis A, Vikelis M, Dardiotis E (2020) Endogenous Melatonin Levels and Therapeutic Use of Exogenous Melatonin in Migraine: Systematic Review and Meta-Analysis. Headache 60(7):1273-1299.
Bertisch SM, Li W, Buettner C, Mostofsky E, Rueschman M, Kaplan ER et al (2020) Nightly sleep duration, fragmentation, and quality and daily risk of migraine. Neurology 94(5):e489–e496
Christiansen I, Daugaard D, Thomsen LL, Olesen J (2000) Glyceryl trinitrate induced headache in migraineurs - Relation to attack frequency. Eur J Neurol 7(4):405–411
Vanagaite J, Pareja J, Støren O, White L, Sanc T, Stovner LJ (1997) Light-induced discomfort and pain in migraine. Cephalalgia (7):733-41
Hougaard A, Amin FM, Hauge AW, Ashina M, Olesen J (2013) Provocation of migraine with aura using natural trigger factors. Neurology 81(23):2057
Noseda R, Copenhagen D, Burstein R (2019) Current understanding of photophobia, visual networks and headaches. Cephalalgia 39(13):1623–1634
Acknowledgements
Not applicable.
Funding
The study received financial support from Lundbeck Foundation (R310-2018-3711). The funding source played no role in the study.
Author information
Authors and Affiliations
Contributions
MA and AHP initiated the study. SY and JT contributed to the study design. AHP and JT carried out the search and data extraction. All authors contributed to interpreting the results. AHP wrote the first draft of the manuscript while SY, JT and MA contributed significantly with wording and approving the final manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no other individuals meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interest
MA is a consultant, speaker or scientific advisor for AbbVie/Allergan, Amgen, Eli Lilly, Lundbeck, Novartis, and Teva, and primary investigator for ongoing AbbVie, Amgen, Eli Lilly and Lundbeck trials. MA has no ownership interest and does not own stocks of any pharmaceutical company. MA serves as associate editor of Cephalalgia, associate editor of the Journal of Headache and Pain. MA is president of the International Headache Society.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Poulsen, A.H., Younis, S., Thuraiaiyah, J. et al. The chronobiology of migraine: a systematic review. J Headache Pain 22, 76 (2021). https://doi.org/10.1186/s10194-021-01276-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-021-01276-w