Abstract
Background
The diagnostic criteria for primary stabbing headache (PSH) in the 3rd beta edition of International Classification of Headache Disorders (ICDH-3 beta) were recently revised. In the ICDH-3 beta, PSH is defined as short-lasting head pain spontaneous occurring as a single stab or series of stabs without autonomic symptoms and involving all head areas (i.e., not limited to the ophthalmic branch region of the trigeminal nerve). The aim of this study was to investigate the validity of the ICHD-3 beta criteria for PSH in a clinic-based setting.
Methods
We prospectively collected data from patients with complaint of headache with stabbing pain without apparent cause at an initial visit to a secondary-care hospital from March 2009 to March 2014. Patients were followed up for 2 weeks to assess changes in clinical characteristics and secondary causes of pain.
Results
Data from 280 patients with headache with stabbing pain without apparent cause were collected, and 245 patients were followed up for 2 weeks. Secondary causes for stabbing headache were observed in 9 patients (herpes zoster in 7 patients and Bell’s palsy in 2 patients) after 2 weeks. The remaining 236 patients fulfilled the diagnostic criteria for PSH according to ICHD-3 beta. Only 22 patients met the diagnostic criteria for PSH according to ICHD-2.
Conclusions
All patients with headache with stabbing pain without cranial autonomic symptoms fulfilled the diagnostic criteria for PSH according to ICHD-3 beta at the initial visit. Secondary causes for headache with stabbing pain were revealed in a small proportion (3.7 %) of patients after 2 weeks of follow-up.
Similar content being viewed by others
Background
Stabbing pain in the head that lasts a few seconds is a common type of headache [1–4]. The second edition of the International Classification of Headache Disorders (ICHD-2) proposed diagnostic criteria for this type of headache, which is known as primary stabbing headache (PSH) (code 4.1). These criteria require that head pain occurs exclusively or predominantly in the first division of the trigeminal nerve without apparent cause [5]. Previous studies have shown, however, that PSH can occur outside the trigeminal region, including in the extracephalic regions. The third beta edition of the International Classification of Headache Disorders (ICHD-3 beta), therefore, has revised the diagnostic criteria for PSH (code 4.1) as head pain that occurs spontaneously as a single stab or series of stabs without cranial autonomic symptoms in all head regions [1–4, 6–12].
The diagnostic criteria for PSH according to ICHD-3 beta have not been validated yet. The purpose of this study was 1) to test the validity of the diagnostic criteria for PSH according to ICHD-3 beta; 2) to investigate the clinical characteristics of PSH according to pain location, which represents a criterion that changed from ICHD-2 to ICHD-3 beta; and 3) to investigate the clinical characteristics of secondary stabbing headache (SSH) at a follow-up visit among patients diagnosed with PSH at an initial visit.
Methods
Participants
We consecutively recruited patients with short-duration headache without apparent cause who visited the Department of Neurology at Kangdong Sacred Heart Hospital, a secondary-care hospital in Korea, from March 2009 to March 2014. Exclusion criteria included 1) 19 years old or younger; 2) patients with possible causes for stabbing headache; and 3) patients who refused to participate the study. After 5 years of consecutive recruitment, we analyzed data of structured interview and medical records of all the subjects in accordance with the ICHD-3 beta diagnostic criteria of PSH in the present study. This study was approved by the Institutional Review Board of Kangdong Sacred Heart Hospital. Written informed consent was obtained from all participants.
Assessment
A physician (HKS) interviewed all patients using a structured questionnaire and performed the physical examination. The information collected included age; gender; headache duration; location, intensity, frequency, and quality of pain; preceding infection; presence of allodynia; associated symptoms; and recurrence of stabbing headache. Patients were followed up for 2 weeks to investigate response to treatment, change in clinical characteristics, and secondary causes for stabbing headache.
The location of pain was recorded relative to the trigeminal and upper cervical regions. The trigeminal region was subdivided into ophthalmic (V1), maxillary (V2), and mandibular (V3) branches. The upper cervical region was subdivided into the lesser occipital nerve (LON), greater occipital nerve (GON), and greater auricular nerve.
A headache specialist (HKS) treated all patients with PSH. Patients with PSH were treated with gabapentin (300 mg bid), naproxen (275 mg bid), or amitriptyline (5 mg hs) based on the judgement of the specialist. Each patient was categorized as either a responder (cessation of stabbing pain) or non-responder (continuation of stabbing pain) in response to treatment after 2 weeks. After 2 weeks of follow up, we asked our participants to inform us if stabbing headache persisted more than 1 week or occurring other secondary causes of stabbing headache to detect persisting symptoms or late-onset SSH.
Statistics
Data were analyzed using SPSS Statistics for Windows, Version 21 (Armonk, New York, USA). Student’s t-tests, chi-square tests, and Mann–Whitney U tests were used for comparison as appropriate. A p-value < 0.05 was considered statistically significant
Results
Subjects
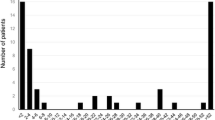
During the study period, a total of 280 patients with stabbing headache were recruited during the initial visit. Of these patients, 243 were prescribed medication for their stabbing headache at the initial visit and 245 were followed for 2 weeks (Fig. 1) Clinical characteristics at initial visit.
Distribution of participants diagnosed with primary stabbing headache at the initial visit according to ICHD-3 beta and ICHD-2 criteria. PSH: primary stabbing headache; ICHD-2: the second edition of the international classification of headache disorders; ICHD-3 beta: the third beta edition of the international classification of the headache disorders
Of the 280 patients with stabbing headache without apparent cause at the initial visit, 103 were men and 177 were women. The mean age of patients was 51.4 ± 13.3 years. The mean duration from the onset of symptoms to the initial visit was 4.0 ± 3.7 days. The mean visual analog scale (VAS) score for headache intensity was 4.6 ± 1.6. Seventy-four (26.4 %) patients reported mild pain (VAS score 1–3), 165 (58.9 %) reported moderate pain (VAS score 4–6), and 41 (14.6 %) reported severe pain (VAS score 7–10). The duration of a single stab was within 1–2 s in 262 patients (93.6 %) and 3–5 s in 18 patients (6.4 %). No patient reported autonomic symptoms during their headache attacks. There was no predominant pain lateralization (145 on the left, 133 on the right, and 2 on both the left and right). Pain was reported in the LON region in 129 patients, GON region in 80 patients, V1 region of the trigeminal nerve in 27 patients, V2 region in 28 patients, and V3 region in 8 patients. One patient had pain in both the LON and GON, and another patient had pain in both V1 and V2. No patients reported stabbing headache in both the trigeminal and upper cervical regions. A total of 243 patients (86.8 %) were treated with medication. Fifty-three patients (18.9 %) reported allodynia on the same side of the stabbing headache. Allodynia was reported in 8 patients who reported stabbing headache in the V1 region (Table 1).
Clinical characteristics at follow-up
Of the 245 patients who were followed for 2 weeks after the initial visit, 231 (94.3 %) reported improvements. Mean duration for improvement among the responder group was 3.2 ± 1.9 days. Secondary causes for stabbing headache were observed in 9 patients (3.8 %) (herpes zoster in 7 patients and Bell’s palsy in 2 patients); these patients were initially diagnosed with PSH (Table 1). Improvement at follow-up was not significantly different between those who did and did not take medication (189/199 vs. 37/37, respectively; p = 0.164). Among 10 PSH patients with persisting stabbing headache at follow-up, no patient additionally visited for their headaches. All 4 SSH patients with persisting stabbing headache at follow-up were diagnosed as having herpes zoster. Three of them improved their stabbing headache after 1 week and the remaining 1 patient improved after 2 weeks.
Validating the ICHD-3 beta criteria for PSH
All 280 patients who participated in the present study fulfilled the diagnostic criteria for PSH at the initial visit. Of the 245 patients who were followed for 2 weeks, 9 (3.2 %) did not meet the criteria for PSH at the second visit due to secondary causes for their stabbing headaches. These patients were diagnosed with SSH. Thus, at follow-up, 236 patients were diagnosed with PSH according to ICHD-3 beta. In contrast, only 28 patients (10.0 %) fulfilled the ICHD-2 criteria for PSH (Fig. 2). The remaining 252 patients were diagnosed with trigeminal neuralgia (N = 7, 2.5 %) or unclassified headache (N = 245, 87.5 %) based on ICHD-2 criteria. One patient (4.5 %) who was initially diagnosed with PSH according to ICHD-2 criteria was diagnosed with SSH due to Bell’s palsy at follow-up. The proportion of patients with PSH re-diagnosed with SSH at follow-up was not significantly different between ICHD-3 beta and ICHD-2 criteria (9/271 vs. 1/27, p = 0.919). No patient was classified as having probable stabbing headache (code 4.7.1) at initial and follow-up visit. The number of patients with PSH re-diagnosed with SSH at follow-up was not significantly different between ICHD-3 and ICHD-2 criteria.
Clinical characteristics of PSH and SSH
We compared demographic and headache characteristics between PSH and SSH. There was no significant difference in gender, age, location of pain, preceding infection, or stressful events between patients with PSH and patients with SSH. VAS for pain was significantly higher in patients with SSH than patients with PSH. Improvement in pain at follow-up was more common in patients with PSH than patients with SSH. The duration of improvement among responders was longer in SSH than PSH (Table 1). However, further follow up of patients with SSH revealed favorable outcome within one month of onset.
Clinical characteristics of PSH involving V1 compared with other regions
Demographic and headache characteristics such as age, gender, VAS for pain, improvement after 2 weeks, duration of improvement among responders, preceding infection, stressful events, and allodynia were not significantly different between patients with PSH who reported V1 region involvement and those who reported involvement of regions other than V1 except stressful event history. Stressful event history was more common among subjects with PSH involving other than V1 region (Table 2).
Clinical characteristics of PSH involving trigeminal area and cervical area
We also compared clinical characteristics at initial visit between PSH involving trigeminal area and cervical area. Stressful event history was significantly higher among PSH subjects involving cervical area than those involving trigeminal area (Table 3).
Discussion
The key findings in the present study are as follows: 1) the diagnostic criteria for PSH in ICHD-3 beta enabled diagnosis of primary headaches with stabbing pain as PSH, most of which were not classified according to ICDH-2 criteria; 2) a small proportion (2.8 %) of new-onset stabbing headaches, which were initially diagnosed as PSH, had secondary causes that were revealed at 2-week follow-up; 3) pain intensity was more severe and pain improvement was slower among patients with SSH than that in patients with PSH.
This is the first study to field test the ICHD-3 beta diagnostic criteria for PSH. In the present study, all 280 subjects with short-lasting stabbing headache without apparent cause and without autonomic symptoms at the initial visit fulfilled the diagnostic criteria for PSH according to ICHD-3 beta. In contrast, only 9.6 % of patients met the criteria for PSH according to ICHD-2. This finding suggests that most primary stabbing headaches without cranial autonomic symptoms fulfill the diagnostic criteria for PHS.
One important change in the diagnostic criteria for PSH in ICHD-3 beta from ICHD-2 was the definition of pain location. The diagnostic criteria for PSH in ICHD-3 beta included all head regions, whereas criteria in ICHD-2 included the V1 region only [12]. To investigate the clinical characteristics of PSH according to pain location, we compared patients with PSH involving the V1 region to patients with PSH involving non-V1 regions. Age, gender, pain intensity, improvement of pain, duration of improvement among responders, preceding infection, stressful events, and allodynia were not significantly different according to pain location. These findings suggest that all clinical characteristics of PSH except pain location are similar between ICHD-3 beta and ICHD-2.
Another change in ICHD-3 beta criteria from ICHD-2 criteria was the definition of accompanying symptoms. Diagnostic criteria for PHS in ICHD-2 included as a criterion that no accompanying symptoms were present [5]. According to ICHD-2, PSH was excluded as a diagnosis if stabbing headache without apparent cause was accompanied by symptoms such as nausea, vomiting, photophobia, or phonophobia [1, 5]. In ICHD-3 beta, this criterion was revised to a lack of “cranial autonomic symptoms” [12]. However, we did not investigate accompanying symptoms except allodynia, and no patient reported cranial autonomic symptoms in the present study. This change in the definition of accompanying symptoms in ICHD-3 beta may have excluded fewer primary headaches with stabbing pain as PSH than ICHD-2.
PSH has been considered responsive to indomethacin [13–16]. Responsiveness to indomethacin was described in the “Comments” of ICHD-1 and ICHD-2 [5, 17]. However, responsiveness to indomethacin was removed from ICHD-3 beta [12]. In the present study, no patient was treated with indomethacin, and most patients with PSH improved at follow-up. Mean duration for improvement was 3.2 days among responders. In addition, improvement at follow-up was not significantly different between patients who did and did not take medication. These findings suggest that most patients with PSH have a good prognosis; specific responsiveness to indomethacin was difficult to conclude.
Our study, which followed patients who were initially diagnosed with PSH, revealed that a small but significant proportion of patients were found to have SSH at follow-up. Previous studies have reported secondary causes for stabbing headache, including Bell’s palsy, herpes zoster, cerebral infarction, transient ischemic attack, post-infection, thalamic hemorrhage, autoimmune diseases, pituitary tumor, Chiari Malformation Type 1, C1-C2 subluxation, meningioma, and multiple sclerosis [2, 6, 15, 18–24]. We compared clinical characteristics of PSH and SSH and found no significant differences except in pain intensity. This finding suggests that the risk for SSH is higher for a PSH-diagnosed stabbing headache with severe pain intensity. The risk for SSH was not significantly different between ICHD-3 beta and ICHD-2 criteria in the present study.
Bell’s palsy and herpes zoster have been reported as common causes of secondary stabbing headache [6, 24]. Retroauricular stabbing pain in Bell’s palsy often presents 2–3 days before the onset of facial weakness [25, 26]. Herpes zoster is usually accompanied by short-lasting stabbing pain in the involved sites. Pain in herpes zoster often presents 4–5 days before the presentation of skin lesions [26]. Most stabbing headaches are reported to be improved within 2 weeks [1, 2]. Given these findings, we followed patients with PSH for 2 weeks. However, stabbing headache persisted in some patients, and some SSH may have been classified as PSH in the present study.
Our study has several limitations. First, we did not perform nerve block or examine tenderness in the occipital area to diagnosis occipital neuralgia (ON). According to ICHD-3 beta, ON pain is associated with tenderness over the affected nerve branch or trigger points at the emergence of the greater occipital nerve or C2 distribution [12]. Temporary relief of the pain by local anesthetic block is also required. ON in the GON and LON areas may have been diagnosed as PSH in the present study. Second, not all patients were treated, and treatment medication was not the same across patients. In the present study, a headache specialist decided which treatment to administer to each patient based on his judgement. The rate and duration of improvement was similar between patients who did and did not receive treatment. This finding is consistent with previous studies in which PSH is reported to be an easily treatable headache disorder [1, 2]. Third, we did not investigate prior history of migraine or other primary headache disorders. Though rather speculative, previous studies reported that 21 - 38 % of patients with primary stabbing headache had history of migraine [2, 16].
The strengths of this study are its large sample size, 2-week follow-up to investigate changes in clinical characteristics and secondary causes, comparisons of diagnostic criteria between ICHD-3 beta and ICHD-2, and headache diagnosis by a headache specialist, which may avoid inter-examiner bias. Future work will include a longer duration of follow-up and exclusion of ON via an examination of tenderness and performance of a nerve block.
Conclusion
In summary, the diagnostic criteria for PSH according to ICHD-3 beta are valid and enable the diagnosis of most primary headaches with stabbing pain, which were not classified according to ICDH-2. A small proportion of participants with PSH according to ICHD-3 beta criteria at the initial visit were re-diagnosed with SSH at 2-week follow-up owing to secondary causes. This information may provide a better understanding of PSH and it diagnostic criteria according to ICHD-3 beta.
Ethical standards
The study was approved by the Institutional Review Board/ethics committee of Hallym University Kangdong Sacred Heart Hospital and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consent was obtained from all participants.
Abbreviations
- GON:
-
greater occipital nerve
- ICHD-2:
-
International Classification of Headache Disorders, 2nd edition
- ICHD-3 beta:
-
International Classification of Headache Disorders, 3rd edition (beta version)
- LON:
-
lesser occipital nerve
- ON:
-
occipital neuralgia
- PSH:
-
primary stabbing headache
- SSH:
-
secondary stabbing headache
References
Fuh JL, Kuo KH, Wang SJ (2007) Primary stabbing headache in a headache clinic. Cephalalgia 27(9):1005–1009
Shin JH, Song HK, Lee JH, Kim WK, Chu MK (2007) Paroxysmal stabbing headache in the multiple dermatomes of the head and neck: a variant of primary stabbing headache or occipital neuralgia? Cephalalgia 27(10):1101–1108
Sjaastad O, Pettersen H, Bakketeig LS (2001) The Vågå study; epidemiology of headache I: the prevalence of ultrashort paroxysms. Cephalalgia 21(3):207–215
Sjaastad O, Pettersen H, Bakketeig LS (2002) The Vågå study of headache epidemiology II. Jabs: clinical manifestations. Acta Neurol Scand 105(1):25–31
Headache Classification Subcommittee of the International Headache Society (IHS) (2004) The International Classification of Headache Disorders. Cephalalgia 24(suppl 1):8–160
Martins IP, Parreira E, Costa I (1995) Extratrigeminal ice‐pick status. Headache 35(2):107–110
Piovesan EJ, Kowacs PA, Lange MC, Pacheco C, Piovesan LR, Werneck LC (2001) Prevalence and semiologic aspects of the idiopathic stabbing headache in a migraine population. Arq Neuropsiquiatr 59(2-A):201–205
Raskin NH, Schwartz RK (1980) Icepick‐like pain. Neurology 30(2):203–205
Selekler HM, Budak F (2004) Idiopathic stabbing headache and experimental ice cream headache (short-lived headaches). Eur Neurol 51(1):6–9
Selekler MH, Komsuoglu SS (2004) Extracephalic stabbing pain temporally related to cephalic ones. Headache 44(7):719–721
Sjaastad O, Pettersen H, Bakketeig LS (2003) Extracephalic jabs/idiopathic stabs. Vågå study of headache epidemiology. Cephalalgia 23(1):50–54
Headache Classification Committee of the International Headache Society (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33(9):629–808
Dodick DW (2004) Indomethacin-responsive headache syndromes. Curr Pain Headache Rep 8(1):19–26
Mathew NT (1981) Indomethacin responsive headache syndromes. Headache 21(4):147–150
Rozen TD (2004) Short-lasting headache syndromes and treatment options. Curr Pain Headache Rep 8(4):268–273
Guerrero AL, Herrero S, Penas ML, Cortijo E, Rojo E, Mulero P, Fernandez R (2011) Incidence and influence on referral of primary stabbing headache in an outpatient headache clinic. J Headache Pain 12(3):311–313
Headache Classification Committee of the International Headache Society (1988) Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalalgia 8(Suppl 7):1–96
Levy MJ, Matharu MS, Meeran K, Powell M, Goadsby PJ (2005) The clinical characteristics of headache in patients with pituitary tumours. Brain 128(Pt 8):1921–1930
Piovesan EJ, Zukerman E, Kowacs PA, Werneck LC (2002) COX‐2 inhibitor for the treatment of idiopathic stabbing headache secondary to cerebrovascular diseases. Cephalalgia 22(3):197–200
Ergün U, Özer G, Sekercan S, Artan E, Kudiaki C, Üçler S, Coskun Ö, Inan L (2009) Headaches in the different phases of relapsing-remitting multiple sclerosis: a tendency for stabbing headaches during relapses. Neurologist 15(4):212–216
Mascellino AM, Lay CL, Newman LC (2001) Stabbing headache as the presenting manifestation of intracranial meningioma: a report of two patients. Headache 41(6):599–601
Rampello L, Malaguarnera M, Rampello L, Nicoletti G, Battaglia G (2012) Stabbing headache in patients with autoimmune disorders. Clin Neurol Neurosurg 114(6):751–753
Robbins MS (2011) Transient stabbing headache from an acute thalamic hemorrhage. J Headache Pain 12(3):373–375
Lewis GW (1958) Zoster sine herpete. Br Med J 2(5093):418–421
Lee G, Lee D, Seok J, Yoo J (2011) Clinical analysis of Bell’s palsy in One university hospital. J Korean Neurol Assoc 29(4):285–290
Roper A, Brown R (2005) Adams and Victor’s Principles of Neurology, 8th edn. McGraw-Hill, Columbus
Acknowledgements
The authors would like to thank Gallup Korea for providing technical support for the Korean Headache Survey.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no conflicts of interest in the research described in “Field testing primary stabbing headache criteria according to the 3rd beta edition of International Classification of Headache Disorders: a clinic-based study”.
Authors’ contributions
MWL conceived and designed the study, analysed data, and wrote the manuscript. MKC designed the study, analysed data and wrote manuscript. JL and JY collected data of this study. HKS conceived and designed the study, collected and analysed data, and wrote the manuscript. All authors read and approved the final manuscript.
Minwoo Lee and Min Kyung Chu are the first authors of this article.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Lee, M., Chu, M.K., Lee, J. et al. Field testing primary stabbing headache criteria according to the 3rd beta edition of International Classification of Headache Disorders: a clinic-based study. J Headache Pain 17, 21 (2016). https://doi.org/10.1186/s10194-016-0615-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-016-0615-z