Abstract
Introduction
Prognosis in patients suffering out-of-hospital cardiac arrest is poor. Higher survival rates have been observed only in patients with ventricular fibrillation who were fortunate enough to have basic and advanced life support initiated soon after cardiac arrest. An ability to predict cardiac arrest outcomes would be useful for resuscitation. Changes in expired end-tidal carbon dioxide levels during cardiopulmonary resuscitation (CPR) may be a useful, noninvasive predictor of successful resuscitation and survival from cardiac arrest, and could help in determining when to cease CPR efforts.
Methods
This is a prospective, observational study of 737 cases of out-of-hospital cardiac arrest. The patients were intubated and measurements of end-tidal carbon dioxide taken. Data according to the Utstein criteria, demographic information, medical data, and partial pressure of end-tidal carbon dioxide (PetCO2) values were collected for each patient in cardiac arrest by the emergency physician. We hypothesized that an end-tidal carbon dioxide level of 1.9 kPa (14.3 mmHg) or more after 20 minutes of standard advanced cardiac life support would predict restoration of spontaneous circulation (ROSC).
Results
PetCO2 after 20 minutes of advanced life support averaged 0.92 ± 0.29 kPa (6.9 ± 2.2 mmHg) in patients who did not have ROSC and 4.36 ± 1.11 kPa (32.8 ± 9.1 mmHg) in those who did (P < 0.001). End-tidal carbon dioxide values of 1.9 kPa (14.3 mmHg) or less discriminated between the 402 patients with ROSC and 335 patients without. When a 20-minute end-tidal carbon dioxide value of 1.9 kPa (14.3 mmHg) or less was used as a screening test to predict ROSC, the sensitivity, specificity, positive predictive value, and negative predictive value were all 100%.
Conclusions
End-tidal carbon dioxide levels of more than 1.9 kPa (14.3 mmHg) after 20 minutes may be used to predict ROSC with accuracy. End-tidal carbon dioxide levels should be monitored during CPR and considered a useful prognostic value for determining the outcome of resuscitative efforts and when to cease CPR in the field.
Similar content being viewed by others
Introduction
Despite all of the progress that has been made in reanimating patients in cardiac arrest over the past half century, resuscitation attempts often fail to restore spontaneous circulation. Consistent and discouraging low survival rates mandate a reassessment of current resuscitative strategies and techniques [1–5]. Overall survival after out-of-hospital cardiac arrest is frequently under 3% [6–8], and so the most common of all decisions after initiation of cardiopulmonary resuscitation (CPR) remains the decision of when to stop. An library of research and guidelines for terminating resuscitative efforts has been developed during the past two decades, and various clinical indicators have been used to determine when CPR efforts should be terminated [8–12]. Capnography (capnometry) potentially represents a useful clinical indicator of death that could guide decisions to terminate resuscitative efforts [8, 13]. We sought to evaluate the hypothesis that partial pressure of end-tidal carbon dioxide (PetCO2) can predict nonsurvival in an independent cohort of patients suffering out-of-hospital cardiac arrest.
Materials and methods
A total of 737 patients who suffered a sudden cardiac arrest in the field and were treated by a mobile emergency team were included in the present prospective study. The data were obtained fin the field in Maribor (approximately 200,000 inhabitants). The study was approved by the Ethics Board of the Ministry of Health of the Republic of Slovenia (59/05/00), which granted a waiver of the need for informed consent. Whenever possible, patients who regained consciousness or their relatives were informed of the study after enrollment.
Consistent with the European Union recommendations, we have a single emergency number: 112. In the Centre for Emergency Medicine Maribor there are two prehospital emergency teams and two basic life support teams equipped with defibrillators. In addition, from April till October during the daytime, in Maribor there is a motorcycle rescuer with defibrillation capability; he and the prehospital emergency team are simultaneously dispatched and they rendezvous in the field.
The prehospital emergency team is an advanced life support unit including three members with an adequately equipped road vehicle. The team includes an emergency physician and two registered nurses or medical technicians.
The basic life support team includes two medical technicians or nurses and driver (paramedic). The motorcycle rescuer is a registered nurse or nurse. The prehospital emergency team is routinely dispatched to the field in emergency situations (in case of presumed cardiac arrest, heart attacks, respiratory distress, cerebrovascular incident, trauma, delivery, poisoning and so on). Basic life support and advanced life support are provided using a regional protocol that incorporates European Resuscitation Council standards and guidelines, and clinical algorithms for cardiac resuscitation. After resuscitation, the patient is transferred to the intensive care unit (ICU) of the University Clinical Center, Maribor. Data in accordance with the Utstein criteria, demographic information, medical data and PetCO2 values were collected for each patient in cardiac arrest by the emergency physician. Hospital records were used for outcome analysis, which also included assessment of cerebral performance category (CPC) by the intensive care unit specialist. A CPC score of 1 reflects good cerebral performance, CPC scores of 2 and 3 indicate moderate and severe cerebral disability, a CPC score of 4 indicates a comatose, vegetative stage, and CPC score 5 indicates brain death.
All nontraumatic out-of-hospital cardiac arrests in adults older than 18 years in the years from January 1998 to December 2006 were included in the study. Exclusion criteria were documented terminal illness and severe hypothermia (<30°C). We defined return of spontaneous circulation (ROSC) in accordance with the Utstein style ('any ROSC' – palpabile pulse on carotid artery, regardless of duration, and ROSC with admission to hospital). In our analysis and comparison, we consider only those patients with ROSC on admission to hospital (defined as having a stable blood pressure when the prehospital resuscitation team was dismissed by the ICU team).
An endotracheal tube was immediately connected to the capnometer. We measured PetCO2 continuously and recorded it during resuscitation, beginning with intial postintubation PetCO2 (first PetCO2 value obtained) and ending with the final PetCO2 value at admission to the hospital or termination of resuscitation attempts. Measurements of PetCO2 were taken using the sidestream method with the infrared capnometer integrated into the LIFEPACK 12 defibrillator monitor (Physio Control, Medtronic Inc., Redmond, WA, USA) or with BCI Capnocheck Model 20600A1 (BCi International, Waukesha, WI, USA).
Continuous data are expressed as median (range) and other data are expressed as mean ± standard deviation. Proportions were reported with 95% confidence interval. Analysis for caterogical variables were performed using χ2 test (with Yates correction, if appropriate) and exact Fisher test. Comparisons between groups were performed using t-test (normal distribution) and Mann-Whitney test (normality test failed). Sensitivity, specificity, and positive predictive value (PPV) and negative predictive value (NPV) were calaculated using standard formulae. For each value, receiver operating characteristic (ROC) curves were obtained. The ROC curve depicts the relation between true positive results (number of predicted deaths among those who actually died) and false positive results (number of predicted deaths among those who actually survived) for each score. The greater the area under the ROC curve (AUROC), the better the predictive value of PetCO2.
Analyses of independent predictors for ROSC and survival from univariate analysis were performed using multivariate logistic regression.
The null hypothesis was considered to be rejected at P values less than 0.05 in all tests. For statistical analysis we used SPSS12.01 software (SPSS Inc., Chicago, IL, USA).
Results
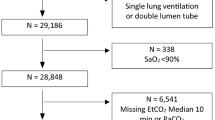
During the period of evaluation, our centre was involved in 1,086 emergency interventions in which there was absence of signs of circulation at the start of intervention. Ultimately, 737 patients were resuscitated. ROSC was achieved in 438 patients (59.4%), overall survival to hospital admission occurred in 55% (402 patients) and 170 (23%) patients were discharged alive (Figure 1).
Utstein reporting template for out-of-hospital cardiac arrest obtained over an 8-year period. CPC, cerebral performance category; CPR indicates cardiopulmonary resuscitation; EMS, emergency medicine services; PEA, pulseless electrical activity; ROSC, restoration of spontaneous circulation; VF, ventricular fibrillation; VT, ventricular tachycardia.
The univariate analysis for ROSC on admission (Table 1) showed that initial PetCO2, ventricular fibrillation or pulseless ventricular tachycardia as the initial rhythm, witnessed arrest, bystander-performed CPR, female sex and response time were associated with ROSC. Using the same method, we found that bystander CPR, witnessed arrest, final PetCO2, initial PetCO2 and resposne time were associated with survival. The initial PetCO2 was higher in patients who survived and in those who achieved ROSC (values expressed as kPa [mmHg]; surviving patients: 3.17 [23.8] ± 1.42 [10.7] versus 2.34 [17.6] ± 1.95 [14.7]; ROSC patients 3.13 [23.5] ± 1.65 [12.4] versus 2.54 [19.1] ± 2.43 [18.3]; P < 0.001). The final PetCO2 (kPa [mmHg]; surviving patients: 3.89 [29.3] ± 1.12 [8.4] versus 1.99 [15.0 mmHg] ± 1.33 [10.0]; ROSC patients: 3.64 [27.4] ± 0.94 [7.1] versus 0.97 [7.3] ± 0.33 [2.5]; P < 0.001) was also considerably higher in the surviving and ROSC patients (Table 2).
The PetCO2 value after 20 minutes of advanced life support averaged 0.91 kPa (6.8 mmHg) ± 0.29 kPa (2.2 mmHg) in patients without ROSC and 4.36 kPa (32.8 mmHg) ± 1.11 kPa (8.4 mmHg) in those who achieved ROSC (P < 0.001). An end-tidal carbon dioxide value above 1.9 kPa (14.3 mmHg) discriminated between the 402 patients with ROSC and 335 patients without ROSC. When an end-tidal carbon dioxide value of 1.9 kPa (14.3 mmHg) or less was used to predict death, the sensitivity, specificity, PPV and NPV were all 100% (Table 3).
A 15-minute PetCO2 value of 1.8 kPa (13.5 mmHg) had a sensitivity and NPV of 100%, with high specificity and positive predictive value (98%).
In the patients with nonshockable initial rhythm (pulseless electrical activity), we observed significantly higher initial PetCO2 values in comparison with the patients with shockable initial rhythm. On the contrary, in the group of patients who presented with ventricular fibrillation/pulseless tachycardia arrest, there were significantly higher values of PetCO2 from the first minute of CPR to the final value (admission to hospital or termination of CPR; Table 4).
The values of PetCO2 in both groups (the group of shockable and the group of nonshockable initial rhythm) were significantly higher in patients with ROSC than in the patients without ROSC (except the PetCO2 after 1 minute of CPR in patients with asystole or pulseless electrical activity as initial rhythm). No patients with an initial, average, final, or maximum PetCO2 value of less than 1.33 kPa (10 mmHg) was resuscitated (Tables 5 and 6).
After 20 minutes of CPR, PetCO2 (regardless of initial rhythm) clearly discriminated between survivors and nonsurvivors in the field (admission to hospital; Tables 7 and 8). In the shockable group PetCO2 values above 1.5 kPa (11.3 mmHg; for a positive outcome), and in the nonshockable group values above 1.90 kPa (14.3 mmHg) had a sensitivity, specificity, PPV and NPV values of 100%, and the AUROC was 1.
After 15 minutes of CPR, PetCO2 values above 1.8 kPa (13.5 mmHg), in both shockable and nonshockable groups, had sensitivity and NPV of 100%, with acceptable specificity and PPV, and an AUROC of 1 (Tables 7 and 8).
At 20 minutes of CPR, a cut-off point for PetCO2 values of 1.5 kPa (13.5 mmHg) yielded sensitivity and NPV of 100% in terms of predicting discharge from hospital in patients with shockable intial rhythm. With a 20-minute PetCO2 cut-off of 2.1 kPa (15.8 mmHg), the sensitivity and NPV were 100% in terms of predicting discharge from hospital in patients with nonshockable initial rhythm (Table 9, Table 10).
In multivariate analysis (Table 11), initial, average, 10-minute, 15-minute, 20-minute, maximum and final values of PetCO2, shockable initial rhythm (ventricular fibrillation or tachycardia), witnessed arrest, bystander-performed CPR, female sex and arrival time were associated with improved ROSC. Using the same method we found that bystander CPR, witnessed arrest, shockable initial rhythm, initial, average, 10-minute, 15-minute, 20-minute, maximum and final PetCO2 values, and arrival time were associated with improved survival (Table 12).
Discussion
Presenting the European perspective, Scogvoll and coworkers [14] reported that the annual incidence of attempted CPR ranged from 33 to 71 per 100,000 inhabitants. Sudden cardiac death accounts for approximately 1000 lives per day in the USA [5]. In the majority of cases, CPR and other treatment efforts are unsuccessful, and the patient was eventually pronounced dead. A number of clinical indicators can be used to determine when those efforts should be terminated [15–18]. Morrison and colleagues [12] described a clinical decision rule for termination of resuscitation (TOR), which was designed to help emergency medical services to determine whether to terminate resuscitative efforts in the setting of out-of-hospital cardiac arrest. In that Canadian study, the investigators sought to validate their previously proposed prediction rule, namely that TOR should be considered if spontaneous circulation does not return before transport is initiated, if no automatic external defibrillator (AED) shocks are given before transport is initiated, and if arrest was not witnessed by emergency personnel. This simple prediction rule has 99.5% PPV and a specificity of 90.2%, and may be useful for providing supplementary guidance in the field [17]. However, a rule cannot determine, for example, how long to continue resuscitation efforts before declaring 'no ROSC'. Decisions about TOR continue to cause difficulties for health care professionals. Current guidelines provide some information on underlying principles, but they do not include a objective, clear and numerical decision rule regarding TOR.
Several animal and clinical studies suggest that the PetCO2 can be used to determine when resuscitation should be ceased. Investigators have suggested that there is a close correlation between PetCO2 and cardiac output, stroke volume, and coronary and cerebral perfusion pressure during CPR. Kalenda [19] first reported a decrease in PetCO2 in patients who could not be resuscitated, and a significant rise in PetCO2 in those patients in whom ROSC could be achieved.
Falk and coworkers [20] found that PetCO2 decreased from mean of 1.4% before arrest to 0.4% after the onset of cardiac arrest. It then increased with CPR and ROSC. Sanders and colleagues [21] found that the end-tidal carbon dioxide level predicted successful resuscitation after in hospital and out-of-hospital cardiac arrest. The average, initial, final, maximum and minimum values of PetCO2 were all higher in resuscitated patients. No patient with an average PetCO2 value of less than 1.33 kPa (10 mmHg) was resuscitated.
Callaham and Barton [22] found that the four patients who had initial and later PetCO2 values of less than 1.33 kPa (10 mmHg) were all resuscitated. These data and similar reports of ROSC after prolonged resuscitative attempts [23] with low PetCO2 values may account for the reluctance of the scientific community to incorporate PetCO2 in Utstein-style reports and resuscitation algorithms. In a landmark prospective study, Levine and colleagues [8] observed 150 patients suffering cardiac arrest and measured PetCO2 using a mainstream capnometer. They compared 20-minute PetCO2 and initial values and concluded that initial values are unreliable in predicting mortality. The 20-minute values of PetCO2 were promising and more reliable in predicting mortality. Values less then 1.33 kPa (10 mmHg) after 20 minutes of CPR were incompatible with survival, and the authors are of the opinion that this could be helpful in deciding when to stop resuscitation efforts. We established the relationship between PetCO2 and prognosis in prehospital CPR in our previous studies [5, 24]. In the second study [24], we confirmed that PetCO2 and mean arterial pressure values are prognostic for the outcome of out-of-hospital cardiac arrest. During a cardiac arrest, PetCO2 can be considered an indirect parameter for the evaluation of cardiac output in the prehospital setting, together with mean arterial pressure, when spontaneous circulation is restored.
Our study is the largest prospective study of the predictive value of PetCO2 measurement for ROSC and survival, and includes 737 victims of out-of-hospital sudden cardiac arrest. We confirmed that bystander CPR, witnessed arrest, shockable initial rhythm, initial, average, 10-minute, 15-minute, 20-minute, maximum and final values of PetCO2 and arrival time were all associated with improved ROSC and survival.
We found that PetCO2 values above 1.9 kPa (14.3 mmHg) measured after 20 minutes of resuscitation identified patients with ROSC with 100% sensitivity, specificity, PPV and NPV. No patients with initial, average, final and maximum PetCO2 values of less than 1.33 kPa (10 mmHg) was resuscitated. With a cut-off point of 20-minute PetCO2 value at 1.5 kPa (13.5 mmHg) in patients with shockable initial rhythm and a cut-off point at 2.1 kPa (15.8 mmHg) in patients with nonshockable initial rhythm, sensitivity and NPV were 100% in predicting discharge from hospital.
In nonshockable rhythm we found higher initial values and lower values after 1 minute of CPR. In our previous study [25] we confirmed PetCO2 to be markedly elevated during the first minute of CPR in asphyxial cardiac arrest. This study therefore confirmed the findings of studies that used animal models in which cardiopulmonary arrest was induced by asphyxia. In this study the PetCO2 values during CPR were initially high, then decreasing to subnormal levels and then increasing again to near-normal levels in patients with ROSC. This pattern of PetCO2 change is different from the pattern observed in cardiac arrest caused by venticular fibrillation, because cardiac arrest from venticular fibrillation results in an abrupt cessation of cardiac output and pulmonary blood flow. We concluded that, during the period of asphyxia, continued cardiac output before cardiac arrest permits continued delivery of carbon dioxide to the lungs, which (in the absence of exhalation) results in higher alveolar carbon dioxide levels. This is reflected in increased PetCO2 when ventilation is resumed.
Our findings in patients with shockable initial rhythm confirmed the view of Levine and coworkers [8] that the data from their study (PetCO2 in patients with pulseless electrical activity) can be extended to all types of cardiac arrest. Sehra and coworkers [26], in a human model of ventricular fibrillation, confirmed that PetCO2 can predict severity of ventricular fibrillation cardiac arrest and efficacy of CPR in this type of cardiac arrest. Our findings in shockable group possible indirectly confirm the three-phase, time-dependent concept of cardiac arrest due to ventricular fibrillation [26]. PetCO2 values under 1.5 kPa (11.3 mmHg) after 20 minutes of CPR (or less that 1.8 kPa [13.5 mmHg] after 15 minutes of CPR) are incompatible with ROSC. This is time of the end of haemodynamic phase of CPR. Possibly, these values represent irreversible hemodynamic collapse, with inadequate coronary or myocardial perfusion pressure, or they may represent perfusion pressures supplied too late (after the haemodynamic phase), with consequent irreversible tissue damage [27, 28].
Our prehospital data, combined with the findings of other investigators, provide strong support for a resuscitation thresholds of PetCO2 1.33 kPa (10 mmHg) initially and 1.9 kPa (14.3 mmHg) after 20 minutes of CPR in the field. The initial values of PetCO2 are not influenced by medications used during CPR, and values at 20 minutes reflect the patient's 'response' to resuscitation efforts. We recommend initial and 20-minute (final PetCO2) to be ranked in Utstein-style reports. The objectives of this approach are to assess the initial condition of the patient in the setting of nontraumatic normothermic cardiac arrest, and to optimize the reliability of PetCO2 in predicting survival in such patients.
Our finding are potentially important, especially in emergency medical system that do not include physicians. The results of the study confirm that PetCO2 can play a pivotal role in the multifactorial decision-making process of whether to discontinue resuscitative efforts. Application of our findings could improve clinical prediction rules for TOR in the field and reduce the number of patients with cardiac arrest who undergo prolonged, futile resuscitation efforts; furthermore, they may reduce transportation of patients with refractory cardiac arrest to the hospital. For the health care system, there is less cost involved in TOR in the field than in the transfer of the patient to the hospital [12, 29, 30].
Conclusion
Measurements of PetCO2 should be used to predict nonsurvival of patients with cardiopulmonary arrest. End-tidal carbon dioxide levels should be monitored during CPR and should be regarded as having prognostic value for determining the outcome of resuscitative efforts. The results can inform decisions regarding when advanced cardiac life support can be discontinued, thus decreasing costs and dilemmas to resuscitation teams. Based on our findings, we believe that end-tidal carbon dioxide monitoring should be incorporated into advanced cardiac life support algorithms and ranked in Utstein-style reports to provide insight into the condition of patients suffering cardiac arrest.
Key messages
-
A PetCO2 level of 1.9 kPa (14.3 mmHg) or less measured 20 minutes after the initiation of advanced cardiac life support accurately predicts death in patients with nonshockable initial rhythm who are suffering cardiac arrest.
-
When a 20-minute PetCO2 value of 1.5 kPa (11.3 mmHg) or less was used as a screening test to predict death in patients with shockable rhythm, the sensitivity, specificity, PPV and NPV were all 100%.
-
Values of PetCO2 less than 1.5 kPa (11.3 mmHg) after 20 minutes of CPR (or <1.8 kPa [<13.5 mmHg] after 15 minutes of CPR) are incompatible with ROSC.
-
End-tidal carbon dioxide levels should be monitored during CPR, and should be regarded as having prognostic value in predicting the outcome of resuscitative efforts and informing decisions regarding TOR.
Abbreviations
- AUROC:
-
area under the ROC curve
- CPC:
-
cerebral performance category
- CPR:
-
cardiopulmonary resuscitation
- ICU:
-
intensive care unit
- NPV:
-
negative predictive value
- PetCO2:
-
partial pressure of end-tidal carbon dioxide
- PPV:
-
positive predictive value
- ROC:
-
receiver operating characteristic
- ROSC:
-
return of spontaneous circulation
- TOR:
-
termination of resuscitation.
References
Larkin GL: Termination of resuscitation:the art of clinical decision making. Curr Opin Crit Care 2002, 8: 224-229. 10.1097/00075198-200206000-00005
Rudner R, Jalowiecki P, Karpel E, Dziurdzik P, Alberski B, Kawecki P: Survival after out-of-hospital cardiac arrests in Katowice (Poland): outcome report according to the Utstein style. Resuscitation 2004, 61: 315-325. 10.1016/j.resuscitation.2004.01.020
Fredriksson M, Herlitz J, Engdahl J: Nineteen years experience of out-of-hospital cardiac arrest in Gothenburg-reported in Utstein style. Resuscitation 2003, 58: 37-47. 10.1016/S0300-9572(03)00115-1
Bunch TJ, White RD, Gersh BJ, Meverden RA, Hodge DO, Ballman KV, Hammill SC, Shen WK, Packer DL: Long-term outcomes of out-of-hospital cardiac arrest after successful early defibrilation. N Engl J Med 2003, 348: 2626-2633. 10.1056/NEJMoa023053
Grmec Š, Križmarič M, Mally Š, Koželj A, Špindler M, Lesnik B: Utstein style analysis of out-of-hospital cardiac arrest--bystander CPR and end expired carbon dioxide. Resuscitation 2007, 72: 404-414. 10.1016/j.resuscitation.2006.07.012
Becker LB, Ostrander MP, Barrett J, Kondos GT: Outcome of CPR in a large metropolitan area: where are the survivors? Ann Emerg Med 1991, 20: 355-361. 10.1016/S0196-0644(05)81654-3
Lombardi G, Gallagher J, Gennis P: Outcome out-of-hospital cardiac arrest in New York City: the Pre-Hospital Arrest Survival Evaluation (PHASE) Study. JAMA 1994, 271: 678-683. 10.1001/jama.271.9.678
Levine RL, Wayne MA, Miller CC: End-tidal carbon dioxide and outcome out-of-hospital cardiac arrest. N Engl J Med 1997, 337: 301-306. 10.1056/NEJM199707313370503
Marwick TH, Case CC, Siskind V, Woodhouse SP: Prediction of survival from resuscitation: a prognosis index derived from multivariate logistic model analysis. Resuscitation 1991, 22: 129-137. 10.1016/0300-9572(91)90003-H
Cooper S, Duncan F: Reliability testing and update of the Resuscitation Predictor Scoring (RPS) Scale. Resuscitation 2007, 74: 253-258. 10.1016/j.resuscitation.2006.12.010
Bonin MJ, Pepe PE, Kimball KT, Clark PS: Distinct criteria for termination of resuscitation in the out of hospital setting. JAMA 1993, 270: 1457-1462. 10.1001/jama.270.12.1457
Morrison LJ, Visentin LM, Kiss A, Theriault R, Eby D, Vermeulen M, Sherbino J, Verbeek R: Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2006, 355: 478-487. 10.1056/NEJMoa052620
Karl BK, Arthur BS, William DV, Charles FB, Willis AT, Gordon AE: Changes in expired end-tidal carbon dioxide during cardiopulmonary resuscitation in dogs: a prognostic guide for resuscitation efforts. J Am Coll Cardiol 1989, 13: 1184-1189.
Skogvoll E, Sangolt GK, Isern E, Gisvold SE: Out-of-hospital cardiopulmonary resuscitation: a population-based Norwegian study of incidence and survival. Eur J Emerg Med 1999, 6: 323-330.
Cooper S, Janghorbani M, Cooper G: A decade of in-hospital resuscitation: outcomes and prediction of survival? Resuscitation 2006, 68: 231-237. 10.1016/j.resuscitation.2005.06.012
Bialecky L, Woodward RS: Predicting death after CPR. Experience at a non-teaching community hospital with a full-time critical care staff. J Emerg Med 1995, 108: 1009-1017.
Richman PB, Vadeboncoeur TF, Chikani V, Clark L, Bobrow BJ: Independent evaluation of an out-of-hospital termination of resuscitation (TOR) clinical decision rule. Acad Emerg Med 2008, 15: 517-521. 10.1111/j.1553-2712.2008.00110.x
Eckstein M, Stratton SJ, Chan LS: Termination of resuscitative efforts for out-of-hospital cardiac arrests. Acad Emerg Med 2005, 12: 65-70. 10.1111/j.1553-2712.2005.tb01481.x
Kalenda Z: The capnogram as a guide to the efficacy of cardiac massage. Resuscitation 1978, 6: 259-263. 10.1016/0300-9572(78)90006-0
Falk JL, Rackow EC, Weil MH: End-tidal carbon dioxide concentration during cardiopulmonary resuscitation. N Engl J Med 1988, 318: 607-611.
Sanders AB, Kern KB, Otto CW, Milander MM, Ewy GA: End-tidal carbon dioxide during cardiopulmonary resuscitation: a prognostic indicator for survival. JAMA 1989, 262: 1347-1351. 10.1001/jama.262.10.1347
Callaham M, Barton C: Prediction of outcome of cardiopulmonary resuscitation from end-tidal carbon dioxide concentration. Crit Care Med 1990, 18: 358-362. 10.1097/00003246-199004000-00002
Cantineau JP, Merckx P, Lambert Y, Sorkine M, Betrand C, Duvaldestin P: Effect of epinephrine on end-tidal carbon dioxide pressure during prehospital cardiopulmonary resuscitation. Am J Emerg Med 1994, 12: 267-270. 10.1016/0735-6757(94)90136-8
Mally S, Jelatancev A, Grmec Š: Effects of epinephrine and vasopressin on end-tidal carbon dioxide tension and mean arterial blood pressure in out-of-hospital cardiopulmonary resuscitation: an observational study. Crit Care 2007, 11: R39. 10.1186/cc5726
Grmec Š, Lah K, Tusek-Bunc K: Difference in end-tidal CO2 between asphyxia cardiac arrest and ventricular fibrillation/pulseless ventricular tachycardia cardiac arrest in the prehospital setting. Crit Care 2003, 7: R139-R144. 10.1186/cc2369
Sehra R, Underwood K, Checcchia P: End tidal CO 2 is a quantitative measure of cardiac arrest. Pacing Clin Electrophysiol 2003, 26: 515-517. 10.1046/j.1460-9592.2003.00085.x
Ewy GA: Cardiocerebral resuscitation: the new cardiopulmonary resuscitation. Circulation 2005, 111: 2134-2142. 10.1161/01.CIR.0000162503.57657.FA
Ewy GA: Cardiac resuscitation: when is enough enough? N Engl J Med 2006, 355: 510-512. 10.1056/NEJMe068090
Gordon AE: Cardiac resuscitation: when is enough enough? N Engl J Med 2006, 355: 510-512. 10.1056/NEJMc061678
Cone DC, Bailey ED, Spackman AB: The safety of a field termination-of-resuscitation protocol. Prehosp Emerg Care 2005, 9: 276-281. 10.1080/10903120590961996
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MK participated in designing the study, collection and analysis of data, and helped to draft the manuscript. MK participated in designing the study, and collection and statistical analysis of data. PK participated in designing the study and helped to draft the manuscript. ŠG participated in designing the study, collection and analysis of data, revised the manuscript for important intellectual content and helped to draft the manuscript. All authors read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kolar, M., Križmarić, M., Klemen, P. et al. Partial pressure of end-tidal carbon dioxide successful predicts cardiopulmonary resuscitation in the field: a prospective observational study. Crit Care 12, R115 (2008). https://doi.org/10.1186/cc7009
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc7009