Abstract
Introduction
Microcirculatory blood flow, and notably gut perfusion, is important in the development of multiple organ failure in septic shock. We compared the effects of dopexamine and norepinephrine (noradrenaline) with those of epinephrine (adrenaline) on gastric mucosal blood flow (GMBF) in patients with septic shock. The effects of these drugs on oxidative stress were also assessed.
Methods
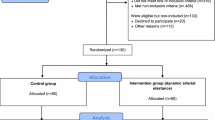
This was a prospective randomized study performed in a surgical intensive care unit among adults fulfilling usual criteria for septic shock. Systemic and pulmonary hemodynamics, GMBF (laser-Doppler) and malondialdehyde were assessed just before catecholamine infusion (T0), as soon as mean arterial pressure (MAP) reached 70 to 80 mmHg (T1), and 2 hours (T2) and 6 hours (T3) after T1. Drugs were titrated from 0.2 μg kg-1 min-1 with 0.2 μg kg-1 min-1 increments every 3 minutes for epinephrine and norepinephrine, and from 0.5 μg kg-1 min-1 with 0.5 μg kg-1 min-1 increments every 3 minutes for dopexamine.
Results
Twenty-two patients were included (10 receiving epinephrine, 12 receiving dopexamine–norepinephrine). There was no significant difference between groups on MAP at T0, T1, T2, and T3. Heart rate and cardiac output increased significantly more with epinephrine than with dopexamine–norepinephrine, whereas. GMBF increased significantly more with dopexamine–norepinephrine than with epinephrine between T1 and T3 (median values 106, 137, 133, and 165 versus 76, 91, 90, and 125 units of relative flux at T0, T1, T2 and T3, respectively). Malondialdehyde similarly increased in both groups between T1 and T3.
Conclusion
In septic shock, at doses that induced the same effect on MAP, dopexamine–norepinephrine enhanced GMBF more than epinephrine did. No difference was observed on oxidative stress.
Similar content being viewed by others
Introduction
In septic shock, when volume resuscitation fails to restore mean arterial pressure (MAP), catecholamines such as dopamine, dobutamine, epinephrine (adrenaline), or norepinephrine (noradrenaline) are used, either alone or in combination [1–3]. Their effectiveness primarily reflects their cardiac and vascular actions, but their ability to modulate the sepsis-induced production of reactive oxygen species may also participate [4]. Nonetheless, if they generally allow normalizing MAP, they can leave some regional blood flows impaired, especially hepatosplanchnic perfusion, which contributes to multiple organ failure [5, 6].
Dopexamine is a structural and synthetic analog of dopamine that exerts systemic vasodilatation through the stimulation of β2 adrenoceptors and peripheral DA1 and DA2 receptors, and weak inotropic properties through the stimulation of β1 adrenoceptors. This pharmacological profile could make the use of dopexamine interesting in combination with norepinephrine to improve both systemic hemodynamics and microcirculatory blood flow, notably gut perfusion. Moreover, in rats, dopexamine has been shown to exert a protective effect against the reactive oxygen species generated by an intravenous administration of xanthine followed by xanthine oxidase [7]. The main objective of the present study was therefore to compare the effects of the combination of dopexamine and norepinephrine with those of epinephrine alone on gastric mucosal blood flow (GMBF). The effects of these drugs on oxidative stress were also assessed.
Materials and methods
Protocol and approval
The protocol was approved by the institutional review board for human research of our hospital (Comité Consultatif de Protection des Personnes dans la Recherche Biomédicale de Rennes) on September 5th 2001 (Reference number: 01/34-355). The study was prospective, randomized, and open-labeled, and was performed on two parallel groups. It was conducted in a 21-bed surgical intensive care unit in a university hospital. Informed consent was obtained from each patient or next of kin.
Patients
Inclusion criteria
Adults aged over 18 years were included if they fulfilled the following:
(1) Evidence of infection.
(2) At least three of the following criteria: temperature more than 38.0°C or less than 36.5°C, respiratory rate more than 20 breaths per minute or arterial pressure in CO2 (PaCO2) less than 32 mmHg or mechanical ventilation, heart rate more than 90 beats per minute, white blood cell count more than 12,000 per mm3 or less than 4,000 per mm3.
(3) At least two of the following criteria: plasma lactate more than 2 mmol per liter or unexplained metabolic acidosis (pH < 7.3), hypoxemia defined by arterial pressure in oxygen (PaO2) less than 70 mmHg at room air or a ratio of PaO2 to fractional inspired oxygen (FiO2) of less than 280 mmHg (or less than 200 mmHg if pneumonia was the source of sepsis) or a need for mechanical ventilation, urine output less than 30 ml per hour for at least 2 hours despite a fluid challenge of at least 500 ml, a platelet count of less than 100,000 per mm3 or a decrease of 50% from a previous value or unexplained coagulopathy (prothrombin time less than 60% and elevated fibrin degradation products more than 10 μg per ml).
(4) Systolic blood pressure less than 90 mmHg despite an optimal volume loading defined by a pulmonary capillary wedge pressure more than 14 mmHg.
Non-inclusion criteria
Pregnant women and patients who had a history of esophageal or gastric disease were not included; neither were patients with a history of esophageal or gastric surgery.
Data collection at inclusion
The following data were recorded at inclusion: general characteristics (age, weight, height, and sex); severity of illness assessed by vital signs, Simplified Acute Physiology Score II (SAPS II), and Sequential Organ Failure Assessment (SOFA) score; and interventions including administered drugs, volume of fluid infusion during the previous 24 hours, and mechanical ventilation conditions. Moreover, blood samples were drawn for hematological and biochemical analyses and blood cultures, and specimens from the site of infection were collected systematically.
Investigated variables
Systemic and pulmonary hemodynamics
All patients had an arterial catheter (Seldicath 4F 3874 13; Plastimed Laboratories, Saint-Leu-La-Forêt, France) and a pulmonary arterial catheter (ref. 831F35; Baxter Healthcare Corporation, Irvine, CA, USA) connected to a monitor (7000/SC 9000XL; Siemens-Elema AB, Solna, Sweden) allowing measurements of heart rate and arterial pressures (systolic and diastolic systemic arterial pressures, right atrial pressure, systolic and diastolic pulmonary arterial pressures, and pulmonary capillary wedge pressure). Calibration was performed with reference to the mild axillary line. Pulmonary capillary wedge pressure was measured at the end of expiration. Cardiac output was measured by thermodilution in triplicate with 10 ml of ice-cold (less than 5.0°C) 5% dextrose solution injected asynchronously with the respiratory cycle. MAP and mean pulmonary arterial pressure, stroke volume, and systemic and pulmonary vascular resistances were calculated from standard formulae.
Gastric mucosal blood flow
GMBF was assessed with a laser-Doppler flowmeter (Periflux PF3; Perimed, Stockholm, Sweden) as described previously [8, 9]. In brief, the laser light is conducted and transmitted to the tissue by an optic fiber (probe 324). Two signals are available for external recording. One signal is proportional to the number and velocity of the red blood cells moving in the measured volume (about 1 mm3) and the other allows the determination of whether the optical probe is making adequate contact with tissue surface. The flow value is expressed in units of relative flux (perfusion units). Calibration was performed against a standard latex solution before the start of measurements, as recommended by the manufacturer. Then the laser-Doppler probe was pushed through the noose into the stomach, the position being checked with X-rays. All patients had simultaneously a nasogastric tube suctioning at -60 mmHg. The laser-Doppler signal was recorded on a computer. Special care was taken to ensure persistent contact between the probe and the gastric mucosa. The ratio between GMBF and cardiac output was calculated.
Blood gases and arterial lactate
Arterial and mixed venous blood gases were determined from samples collected anaerobically in heparinized plastic syringes through the arterial and distal port of the pulmonary artery catheter, respectively. Samples were analyzed within 15 minutes by a co-oximeter (Abl 725; Radiometer, Copenhagen, Denmark) to determine arterial and mixed venous oxygen tension and saturation, as well as arterial lactate concentration (enzymatic dosage). Arterial and mixed venous oxygen content, oxygen delivery, and oxygen consumption were calculated from standard formulae.
Oxidative stress
Oxidative stress was assessed from plasma malondialdehyde levels, as an index of lipid peroxidation induced by the generation of free radicals. Malondialdehyde concentrations were estimated by a colorimetric test with thiobarbiturate [10]. After precipitation of protein with a mixture of phosphotungstic acid and sulfuric acid, the supernatant was incubated with thiobarbiturate for one hour at 90°C. Thiobarbiturate-reactive substances were then extracted with n-butanol and the absorbance was monitored at 535 nm. The concentrations were calculated from a calibration curve obtained by the acid hydrolysis of 1,1,3,3-tetramethoxypropane solution, generating standard concentrations of malondialdehyde. Standards were then treated with thiobarbiturate reagent and extracted with n-butanol in the same way as unknown samples. The normal value of malondialdehyde in healthy subjects was less than 4 μmol per liter.
Experimental protocol and treatments
As soon as inclusion criteria had been checked and informed consent had been obtained, baseline measurements were performed, including systemic and pulmonary hemodynamics and GMBF, and blood samples were drawn (T0). Ventilator settings were adapted for each patient so as to reach arterial oxygen saturation above 90% and a plateau pressure lower than 30 cmH2O. Patients were then randomized to receive either epinephrine alone or a combination of dopexamine and norepinephrine. The unpredictability of randomization was guaranteed by two specific procedures: the randomization list, generated with a computer, was equilibrated using unequal-sized blocks and the randomization of a patient was performed by an independent pharmacist. Study treatments were administered with an automatic syringe through the intermediate port of the pulmonary artery catheter. Drugs were titrated from 0.5 μg kg-1 min-1 with 0.5 μg kg-1 min-1 increments every 3 minutes for dopexamine and from 0.2 μg kg-1 min-1 with 0.2 μg kg-1 min-1 increments every 3 minutes for norepinephrine and epinephrine, until MAP reached 70 to 80 mmHg. If necessary, dopexamine and norepinephrine doses were adjusted by using cardiac output according to the algorithm in Figure 1. When MAP was above 80 mmHg, the dose of norepinephrine or epinephrine was adjusted to let MAP decrease to between 70 and 80 mmHg. Once the target MAP had been obtained, the treatment was maintained at the same doses, and the same measurements as at baseline were performed (T1). No adjustment of fluid infusion or mechanical ventilation was allowed during this first study period (namely between T0 and T1). The same variables were measured two hours (T2) and six hours (T3) later. During this second study period (that is, between T1 and T3), fluid loading and doses of catecholamines were adjusted to maintain a pulmonary capillary wedge pressure of more than 14 mmHg and MAP between 70 and 80 mmHg, respectively.
Sample size
Sample size estimation was based on GMBF data from our previous study, in which the standard deviation of GMBF was 160 units at inclusion [9]. In the actual protocol, 20 patients were planned to be included so as to detect a difference between the two groups of 240 units with a type I error of 5% and a power of 95%.
Statistical analysis
Statistical analysis was performed with SAS statistical software V8.02 (SAS Institute, Cary, NC, USA). Data are presented as means ± SD for normally distributed variables and as medians (25th – 75th centiles) for non-normally distributed variables. The homogeneity of pretreatment (T0) mean values between groups was tested with Student's t test or Wilcoxon's rank sum test when needed. Comparisons of treatment mean values between groups over the second study period (that is, between T1 and T3) were performed with a two-way (time, treatment) analysis of covariance (mixed model), the analysis being adjusted on baseline values. In case of a significant time–treatment interaction, treatment effect was assessed time by time by a one-way analysis of covariance similarly adjusted on baseline values. For non-normally distributed variables a non-parametric repeated-measures analysis, also adjusted on baseline values (mixed model), was performed on ranked data. For all analyses, p < 0.05 was considered to be significant.
Results
A total of 22 patients were randomized (10 received epinephrine, and 12 received dopexamine–norepinephrine) between March 25th 2002 and March 17th 2004. Two patients (one in each group) were excluded from the analysis on the main endpoint because of inadequate location of the laser-Doppler probe, and two patients (one in each group) could not be investigated at T3 because of the need for prompt surgical management to control the source of sepsis.
General characteristics of study patients at inclusion
There was no significant difference between the groups in age, weight, height, sex ratio, SAPS II, SOFA, volume of fluid infusion during the previous 24 hours, and mechanical ventilation conditions (Table 1). The origin of sepsis was essentially peritonitis (six patients in the epinephrine group and nine patients in the dopexamine–norepinephrine group). The infection was not microbiologically documented in one patient in the epinephrine group and in two patients in the dopexamine–norepinephrine group. Mortality rates at days 28 and 90 were 3/10 (30%) and 4/10 (40%), respectively, in the epinephrine group, and 2/12 (17%) and 3/12 (25%), respectively, in the dopexamine–norepinephrine group.
The median (25th – 75th centiles) delay between randomization and stabilization of MAP at the target level was 60 minutes (50 – 80 minutes) and 70 minutes (60 – 140 minutes) in the epinephrine and dopexamine–norepinephrine groups, respectively (p = 0.078). Median catecholamine doses (μg kg-1 min-1) at the three times of investigation were 0.17 (0.14 to 0.19) at T1, 0.19 (0.14 to 0.24) at T2 and 0.19 (0.18 to 0.21) at T3 for epinephrine, 0.51 (0.48 to 0.53) at T1, 0.51 (0.49 to 0.53) at T2 and 0.51 (0.50 to 0.55) at T3 for dopexamine, and 0.20 (0.11 to 0.60) at T1, 0.20 (0.12 to 0.69) at T2 and 0.18 (0.11 to 0.74) at T3 for norepinephrine.
Effects of treatments on systemic and pulmonary hemodynamics and oxygenation parameters
At baseline, there was no significant difference between the two groups whichever variable was considered (Table 2). There was also no significant difference in MAP between the two groups at T1, T2, and T3. Heart rate and cardiac output increased significantly more with epinephrine than with dopexamine–norepinephrine between T1 and T3 (+5%, p = 0.023 for treatment effect, and +13%, p = 0.039, respectively). Similarly, oxygen delivery and oxygen consumption increased significantly more with epinephrine than with dopexamine–norepinephrine between T1 and T3 (+17%, p = 0.009 for treatment effect, and +34%, p = 0.001, respectively).
Effects of treatments on GMBF and on the ratio between GMBF and cardiac output
At baseline there was no significant difference in GMBF or in the ratio between GMBF and cardiac output between the two groups (Table 2). GMBF increased significantly more with dopexamine–norepinephrine than with epinephrine (medians 106, 137, 133, and 165 compared with 76, 91, 90, and 125 units of relative flux at T0, T1, T2, and T3, respectively; p = 0.048 for treatment effect; Figure 2, top). The ratio between GMBF and cardiac output decreased with epinephrine, whereas it did not change with dopexamine–norepinephrine between T1 and T3 (p = 0.015 for treatment effect; Figure 2, bottom).
Effects of treatments on arterial lactate concentration and oxidative stress
At baseline, there was no significant difference in arterial lactate and malondialdehyde concentrations between the two groups. Arterial lactate increased with epinephrine, whereas it did not change with dopexamine–norepinephrine between T1 and T3 (p < 0.001 for treatment effect; Figure 3, top). Malondialdehyde similarly increased in the two groups between T1 and T3 (p = 0.048 for time effect; p = 0.542 for treatment effect; Figure 3, bottom).
Discussion
The key finding of our study was that in patients with septic shock, at the same level of MAP, dopexamine–norepinephrine enhanced GMBF more than epinephrine did.
With regard to systemic hemodynamics, epinephrine induced greater heart rate, cardiac output, oxygen delivery, and oxygen consumption than the combination of dopexamine and norepinephrine. These effects express the well-known strong β1-adrenergic stimulation induced by epinephrine [2] and the more balanced cardiac and vascular effects induced by the combination of dopexamine and norepinephrine. Epinephrine also induced a significant increase in arterial lactate, as has already been shown in patients with septic shock [9, 11, 12]. This effect may result from splanchnic hypoxia [12, 13]. However, epinephrine could also increase arterial lactate independently of a defect of cellular oxygenation by stimulation of the skeletal muscle cell Na+, K+-ATPase, which accelerates aerobic glycolysis and consequently the production of lactate [14].
The effect of catecholamines on the hepatosplanchnic perfusion of septic patients remains controversial, depending on the method used to evaluate perfusion, the region studied (extended versus limited area) and the severity of patients (sepsis, severe sepsis, or septic shock). Indeed, dopexamine infusion during sepsis and septic shock increased splanchnic blood flow, but the fractional contribution of the regional blood flow to cardiac output decreased or remained unchanged [15, 16]. In patients with septic shock, dopexamine alone or in combination with another catecholamine either did not change gastric mucosal pH [16, 17] or increased it [18] but did not modify the gastric mucosal–arterial pCO2 gradient [17]. When using an original method to evaluate gastrointestinal mucosal perfusion (reflectance spectrophotometry), dopexamine infusion was shown to markedly improve the hemoglobin oxygen saturation of gastric mucosa [17]. However, these results were observed in uncontrolled studies. When patients with septic shock previously treated by norepinephrine were randomized to receive either dopexamine or dobutamine, the gastric mucosal–arterial pCO2 gradient was improved similarly in the two groups [19]. Similar conflicting results exist on the effects of epinephrine on intestinal perfusion in sepsis. Epinephrine infusion was found to decrease splanchnic blood flow, decrease gastric mucosal pH, and increase the gastric mucosal–arterial pCO2 gradient [15]. However, two studies found that GMBF, assessed as in our study by laser-Doppler flowmetry, increased during epinephrine infusion in patients with septic shock [8, 9].
In the present study, both epinephrine and the combination of dopexamine and norepinephrine durably increased GMBF, but this effect was more pronounced with the combination of dopexamine and norepinephrine. The ratio between GMBF and cardiac output decreased during epinephrine infusion, whereas it did not change during dopexamine–norepinephrine infusion. Indeed, in comparison with dopexamine–norepinephrine, the increase in cardiac output allowed by epinephrine was not totally distributed to the gastric mucosa, as shown by a marked increase in estimated gastric mucosal resistance (MAP over GMBF ratio = +41% between T0 and T1). In the dopexamine–norepinephrine group, estimated gastric mucosal resistance increased only slightly (+9% between T0 and T1), supporting the hypothesis of a dopexamine-induced vasodilatation that counteracted the norepinephrine-induced vasoconstriction. These results are in agreement with those of experimental studies performed in septic rats demonstrating, by videomicroscopy, an improvement in intestinal mucosal blood flow during dopexamine infusion [20, 21]. Our results must be interpreted in the light of the limitation of the laser-Doppler technique. Indeed, this technique does not take into account the heterogeneity of microvascular blood flow (a major characteristic of sepsis-induced microcirculatory disorders), because this technique measures the average velocity of all vessels comprised in the investigated volume [22, 23]. Nevertheless, our results suggest that this technique is adapted to assess flow variations in the investigated territory under various pharmacological interventions.
The excessive production of reactive oxygen species during sepsis may be involved in cellular damage [24, 25]. A recent study performed in critically ill patients showed a significant increase in oxidative stress, as assessed by plasma concentrations of thiobarbituric acid-reactant substances, both in patients with systemic inflammatory response syndrome and multiple organ failure and in non-survivors [26]. In rats, the reactive oxygen species generated by an intravenous administration of xanthine followed by xanthine oxidase induced a circulatory failure with a survival rate of 20% [5]. When the animals were pretreated by increasing doses of dopexamine, survival was enhanced to 70%. In our study, the production of malondialdehyde similarly increased in both groups and we did not find any influence of dopexamine on the production of reactive oxygen species.
Conclusion
In septic shock, at doses that induced the same effect on MAP, dopexamine–norepinephrine enhanced GMBF more than epinephrine did. No difference was observed on oxidative stress. Our findings suggest that the combination of dopexamine and norepinephrine could be an interesting alternative in the treatment of the hemodynamic disturbances observed in septic shock.
Key messages
-
In septic shock, at doses that induced the same effect on mean arterial pressure, dopexamine–norepinephrine enhanced gastric mucosal blood flow more than epinephrine did.
-
The combination of dopexamine and norepinephrine could be an interesting alternative in the treatment of the hemodynamic disturbances observed in septic shock.
Abbreviations
- GMBF:
-
GMBF = gastric mucosal blood flow
- MAP:
-
MAP = mean arterial pressure
- SAPS II:
-
SAPS II = Simplified Acute Physiology Score II
- SOFA:
-
SOFA = Sequential Organ Failure Assessment
References
Hotchkiss RS, Karl IE: The pathophysiology and treatment of sepsis. N Engl J Med 2003, 348: 138-150.
Dellinger RP: Cardiovascular management of septic shock. Crit Care Med 2003, 31: 946-955.
Hollenberg SM, Ahrens TS, Annane D, Astiz ME, Chalfin DB, Dasta JF, Heard SO, Martin C, Napolitano LM, Susla GM, et al.: Practice parameters for hemodynamic support of sepsis in adult patients: 2004 update. Crit Care Med 2004, 32: 1928-1948.
Collins JL, Vodovotz Y, Yoneyama T, Hatakeyama K, Green AM, Billiar TR: Catecholamines decrease nitric oxide production by cytokine-stimulated hepatocytes. Surgery 2001, 130: 256-264.
Koike K, Moore FA, Moore EE, Poggetti RS, Tuder RM, Banerjee A: Endotoxin after gut ischemia/reperfusion causes irreversible lung injury. J Surg Res 1992, 52: 656-662.
Asfar P, De Backer D, Meier-Hellmann A, Radermacher P, Sakka SG: Clinical review: influence of vasoactive and other therapies on intestinal and hepatic circulations in patients with septic shock. Crit Care 2004, 8: 170-179.
Jacinto SM, Chintala MS, Lokhandwala MF, Jandhyala BS: Efficacy and mechanisms of dopexamine in the prevention of ischemia-reperfusion induced organ damage: role of oxygen free radicals. Clin Exp Hypertens 1997, 19: 181-190.
Duranteau J, Sitbon P, Teboul JL, Vicaut E, Anguel N, Richard C, Samii K: Effects of epinephrine, norepinephrine, or the combination of norepinephrine and dobutamine on gastric mucosa in septic shock. Crit Care Med 1999, 27: 893-900.
Seguin P, Bellissant E, Le Tulzo Y, Laviolle B, Lessard Y, Thomas R, Malledant Y: Effects of epinephrine compared with the combination of dobutamine and norepinephrine on gastric perfusion in septic shock. Clin Pharmacol Ther 2002, 71: 381-388.
Yagi K: Simple assay for the level of total lipid peroxides in serum or plasma. In Methods in Molecular Biology: Free Radicals and Antioxidant Protocols. Edited by: Armstrong D. Totowa, NJ: Humana Press Inc; 1998:101-106.
Bollaert PE, Bauer P, Audibert G, Lambert H, Larcan A: Effects of epinephrine on hemodynamics and oxygen metabolism in dopamine-resistant septic shock. Chest 1990, 98: 949-953.
Levy B, Bollaert PE, Charpentier C, Nace L, Audibert G, Bauer P, Nabet P, Larcan A: Comparison of norepinephrine and dobutamine to epinephrine for hemodynamics, lactate metabolism, and gastric tonometric variables in septic shock: a prospective, randomized study. Intensive Care Med 1997, 23: 282-287.
Meier-Hellmann A, Reinhart K, Bredle DL, Specht M, Spies CD, Hannemann L: Epinephrine impairs splanchnic perfusion in septic shock. Crit Care Med 1997, 25: 399-404.
Levy B, Gibot S, Franck P, Cravoisy A, Bollaert PE: Relation between muscle Na+K+ATPase activity and raised lactate concentrations in septic shock: a prospective study. Lancet 2005, 365: 871-875.
Meier-Hellmann A, Bredle DL, Specht M, Hannemann L, Reinhart K: Dopexamine increases splanchnic blood flow but decreases gastric mucosal pH in severe septic patients treated with dobutamine. Crit Care Med 1999, 27: 2166-2171.
Kiefer P, Tugtekin I, Wiedeck H, Bracht H, Geldner G, Georgieff M, Radermacher P: Effect of a dopexamine-induced increase in cardiac index on splanchnic hemodynamics in septic shock. Am J Respir Crit Care Med 2000, 161: 775-779.
Temmesfeld-Wollbruck B, Szalay A, Mayer K, Olschewski H, Seeger W, Grimminger F: Abnormalities of gastric mucosal oxygenation in septic shock: partial responsiveness to dopexamine. Am J Respir Crit Care Med 1998, 157: 1586-1592.
Smithies M, Yee TH, Jackson L, Beale R, Bihari D: Protecting the gut and the liver in the critically ill: effects of dopexamine. Crit Care Med 1994, 22: 789-795.
Levy B, Nace L, Bollaert PE, Dousset B, Mallie JP, Larcan A: Comparison of systemic and regional effects of dobutamine and dopexamine in norepinephrine-treated septic shock. Intensive Care Med 1999, 25: 942-948.
Schmidt H, Secchi A, Wellmann R, Bach A, Bhrer H, Martin E: Dopexamine maintains intestinal villus blood flow during endotoxemia in rats. Crit Care Med 1996, 24: 1233-1237.
Madorin WS, Martin CM, Sibbald WJ: Dopexamine attenuates flow motion in ileal mucosal arterioles in normotensive sepsis. Crit Care Med 1999, 27: 394-400.
Tenhunen JJ, Uusaro A, Karja V, Oksala N, Jakob SM, Ruokonen E: Apparent heterogeneity of regional blood flow and metabolic changes within splanchnic tissues during experimental endotoxin shock. Anesth Analg 2003, 97: 555-563.
Hiltebrand LB, Krejci V, Banic A, Erni D, Wheatley AM, Sigurdsson GH: Dynamic study of the distribution of microcirculatory blood flow in multiple splanchnic organs in septic shock. Crit Care Med 2000, 28: 3233-3241.
Goode HF, Webster NR: Free radicals and antioxidants in sepsis. Crit Care Med 1993, 21: 1770-1776.
Cadenas S, Cadenas AM: Fighting the stranger – antioxidant protection against endotoxin toxicity. Toxicology 2002, 180: 45-63.
Motoyama T, Okamoto K, Kukita I, Hamaguchi M, Kinoshita Y, Ogawa H: Possible role of increased oxidant stress in multiple organ failure after systemic inflammatory response syndrome. Crit Care Med 2003, 31: 1048-1052.
Acknowledgements
We thank Valérie Turmel and Alain Renault (CIC Inserm 0203) for their contribution to the data analysis. This study was supported by Grant from Rennes University Hospital and Rennes 1 University, 2001 Clinical Research Program, Rennes, France.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
PS conceived the study, participated in the design and execution of the study, the analysis of data and wrote the manuscript. BL participated in the execution of the study, the analysis of data and co-wrote the manuscript. PG and IM participated in the execution of the study and interpretation of the data. YM and EB supervised study planning, design, execution and analysis and co-wrote the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Seguin, P., Laviolle, B., Guinet, P. et al. Dopexamine and norepinephrine versus epinephrine on gastric perfusion in patients with septic shock: a randomized study [NCT00134212]. Crit Care 10, R32 (2006). https://doi.org/10.1186/cc4827
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc4827