Abstract
Introduction
Patients with severe acute pancreatitis are at risk of candidal infectionscarrying the potential risk of an increase in mortality. Since early diagnosis isproblematic, several clinical risk scores have been developed to identify patientsat risk. Such patients may benefit from prophylactic antifungal therapy whilethose patients who have a low risk of infection may not benefit and may be harmed.The aim of this study was to assess the validity and discrimination of existingrisk scores for invasive candidal infections in patients with severe acutepancreatitis.
Methods
Patients admitted with severe acute pancreatitis to the intensive care unit wereanalysed. Outcomes and risk factors of admissions with and without candidalinfection were compared. Accuracy and discrimination of three existing risk scoresfor the development of invasive candidal infection (Candida score, CandidaColonisation Index Score and the Invasive Candidiasis Score) were assessed.
Results
A total of 101 patients were identified from 2003 to 2011 and 18 (17.8%) of thesedeveloped candidal infection. Thirty patients died, giving an overall hospitalmortality of 29.7%. Hospital mortality was significantly higher in patients withcandidal infection (55.6% compared to 24.1%, P = 0.02). Candida colonisation was associated with subsequent candidal infection onmultivariate analysis. The Candida Colonisation Index Score was the most accuratetest, with specificity of 0.79 (95% confidence interval [CI] 0.68 to 0.88),sensitivity of 0.67 (95% CI 0.41 to 0.87), negative predictive value of 0.91 (95%CI 0.82 to 0.97) and a positive likelihood ratio of 3.2 (95% CI 1.9 to 5.5). TheCandida Colonisation Index Score showed the best discrimination with area underthe receiver operating characteristic curve of 0.79 (95% CI 0.69 to 0.87).
Conclusions
In this study the Candida Colonisation Index Score was the most accurate anddiscriminative test at identifying which patients with severe acute pancreatitisare at risk of developing candidal infection. However its low sensitivity maylimit its clinical usefulness.
Similar content being viewed by others
Introduction
Infections caused by fungal pathogens have increased in the last two decades with datafrom the USA between 1979 and 2000 demonstrating a 207% increase [1]. In the Extended Prevalence of Infection in Intensive Care (EPIC II) study,candida was the fourth most common cause of infection in ICUs worldwide [2]. Infections in Europe are less frequent; however, in the Sepsis Occurrence inAcutely Ill Patients (SOAP) study, candidal organisms still accounted for 17% ofinfections [3]. Other data demonstrate that candidaemia in intensive care patients, however,has remained static or even decreased in recent years [4]. Most cases are caused by Candida albicans, but there are numerousother species, and antifungal resistance spectrums of these vary.
Numerous risk factors have been identified for the development of Candida spp bloodstream infection. These include the presence of invasive lines, for examplecentral venous catheters (CVCs), antibiotic therapy, acute kidney injury requiring renalreplacement therapy (RRT), malignancy and neutropenia, previous abdominal surgery, totalparenteral nutrition (TPN), long term hospitalisation and prior fungal colonisation [5–8].
Severe acute pancreatitis (SAP) has also been identified as a risk factor for candidalinfection [9]. Candidal infection has been identified as a cause of increased mortality inpatients post-operatively and in the critically ill [8, 10, 11] but its effect on the outcome of SAP has been disputed [12–15]. A healthy pancreas is relatively resistant to fungal infection; however,pancreatic necrosis carries a disproportionately higher risk of infection with bacterialand fungal organisms. Prior use of antibiotics has been demonstrated to increase therisk of fungal infection [5]. Prophylactic or empirical antifungal treatment has been advocated forhigh-risk surgical patients [16–19] and demonstrated to prevent fungal infection in SAP patients [12]. 'Prophylactic' antifungal treatment is defined as administration ofantifungals to patients identified as having a particular diagnosis or particularfactors that confer a high risk of subsequent fungal infection. 'Empirical' treatment isdefined as antifungal therapy given to patients with clinical features of aninflammatory response consistent with infection but without microbiologicalconfirmation. As delays in treatment are associated with increased mortality and fungalculture can take up to 72 hours, it would be desirable to identify patients at risk forinvasive infection whilst minimising unnecessary treatment and reducing the risk ofresistance through increases in non-albicans species [7, 20].
As a consequence, several risk scoring systems have been developed in an attempt to aiddiscrimination between candida colonisation and invasive candidal infection (ICI) [6, 8, 9]. These combine the identification of high-risk patients with clinical andmicrobiological data to identify those patients at risk of developing ICI. The aim ofthis study was to identify the prevalence of ICI in a population of critically illpatients with SAP, to identify risk factors for the development of ICI and to evaluateits impact on patient outcome. In addition we assessed the accuracy and discriminationof three previously described risk scores for ICI in this cohort of patients [6, 8, 9].
Materials and methods
A single centre, retrospective study was conducted at a tertiary referral centre forpatients with SAP. After discussion with the local Research Ethics Committee, the studyprotocol was approved and the requirement for written informed consent was waived, sinceinformed consent for collection and analysis of patient data recorded in the Case MixProgramme database is not required under Section 251 of the NHS Act 2006 (approvalnumber PAIG 2-10(f)/2005). All patients admitted to the ICU with a diagnosis of SAPbetween July 2003 and February 2011 were screened for inclusion in the study. Suitablecases were identified from the admissions database. Patients who were re-admitted to theICU during the same hospital stay or who were transferred from other ICUs were excludedfrom further analysis. SAP was defined as acute pancreatitis with true organ dysfunctionirrespective of local complications as per consensus guidelines in 2004 [21]. 'Significant necrosis' was defined as the presence of more than 30% necrosisseen on abdominal computed tomography scans, as reported by a radiologist. Threeindependent workers extracted data from the case notes and electronic records of eachadmission onto an Excel spreadsheet. The aetiology of SAP was classified into 'alcohol','gallstones', 'drug', or 'idiopathic'. 'Unknown' was recorded if no cause could beidentified from the case notes. Acute Physiology and Chronic Health Evaluation (APACHEII) scores were extracted from the ICU admission database. For admissions without APACHEII scores due to a unit length of stay less than eight hours, admission physiology datawere entered into a web-based calculator [22] in order to calculate an admission APACHE II score.
All patients were treated according to a routine standard of care. This includedadherence to care bundles, no prophylactic antibiotics, daily measurement of C-reactiveprotein and early enteral feeding. Naso-gastric feeding was used for nutritionalsupport, guided by the patient's ideal body weight. Prokinetics were started whenabsorption was poor and, if necessary, a post-pyloric feeding tube was inserted. TPN wasconsidered if post-pyloric feeding was unsuccessful. Abdominal computed tomography scanswere performed on admission and then every seven to ten days, and minimally invasivepancreatic necrosectomy (MIRPN), open necrosectomy or radiologically-guided drainage wasperformed, as surgically indicated.
Samples for candidal colonisation were taken routinely from tracheal aspirates and/orbronchial lavage, skin swabs and drainage fluid (if drains were in situ).Further sampling (for example, culture of blood, line tips and pancreatic tissuesamples) was performed if indicated by clinical need. Patients were classified as havingICI if they had: 1) ≥ 1 positive blood culture or 2) ≥ 1 positive pancreatictissue culture or 3) ≥ 1 pancreatic drain fluid culture positive for Candida spp. and in addition received antifungal drugs after the positive drain fluidculture. Antifungal therapy is only initiated after discussion between an intensive careconsultant and a medical microbiologist with an interest in intensive care. Patientswith Candida cultured from one or more samples from respiratory secretions,urine, line tips, or wound or skin swabs alone were classified as colonised.
For determination of risk in the scoring systems, the following were considered riskfactors: 1) severe sepsis as defined by the 2001 SCCM/ESICM/ACCP/ATS/SIS InternationalSepsis Definitions Conference criteria [23]; 2) central venous access: presence of a CVC or peripherally inserted centralvenous catheter (PICC) on days one to three post ICU admission; 3) systemic antibiotics:any intravenous antibiotics on days one to three post ICU admission (excludingprophylactic antibiotics given after surgery or to treat reduced gastric motility); 4)renal replacement therapy (RRT): any form of RRT given on day one to three post ICUadmission; 5) steroids: any dose of corticosteroids given during the seven days priorand three days after admission to ICU; 6) immunosuppressive drugs: any immunosuppressivedrugs (as listed in the British National Formulary version 59 section 8.2) given duringthe seven days prior to admission; 7) surgery: any intra-abdominal surgical procedureduring the seven days prior to admission; and 8) TPN: any TPN delivered via a CVC orPICC on days one to three post ICU admission.
Statistics
Descriptive statistics were performed on the entire cohort of admissions and onadmissions with and without ICI. Univariate analysis was performed to assessdifferences in the characteristics of patients with and without ICI. ICU and ultimatehospital mortality were compared between the two groups.
Multivariate logistic regression analysis was performed using ICI as the dependentvariable with candida colonisation, presence of necrosis and length of ICU stay asindependent variables.
'Candida score' was calculated for each admission as described previously [6] with appropriate weightings for each variable. Weightings are as follows:TPN, surgery, multifocal colonisation: 1 point; severe sepsis: 2 points. Patientswith a score >3 were defined as 'positive'. Since the Invasive Candidiasis scoreincludes SAP as a risk factor, SAP was removed for this study and a modified'Invasive Candidiasis' risk score [9] was calculated for each admission as follows: Patients who had developedICI and met the criteria of having received antibiotics and had a CVC and at leastone of: TPN, RRT, surgery, steroids or immunosuppressants were defined as truepositives. Immunosuppression was defined as described above. A Candida ColonizationIndex Score (CCIS) was calculated for each patient using the methods described [8] as follows: CCIS = ratio of the number of non-blood distinct body sitescolonised with Candida spp to the total number of body sites cultured. ACCIS ≥ 0.5 predicts Candida infection; therefore, patients who had ICIand a CCIS ≥ 0.5 were defined as true positives.
The sensitivity, specificity, positive predictive value (PPV), negative predictivevalue (NPV), positive likelihood ratio (LR+) and negative likelihood ratio (LR-) werecalculated for each score, along with 95% confidence intervals. For PPV and NPV,prevalence levels as described in the study population were used. Area under theReceiver Operating Characteristic curve (AUROC) with exact binomial confidenceintervals was calculated for each score using the method of DeLong [24]. Comparisons between groups of categorical data were made using Fisher'sexact test or χ2 test where appropriate. Continuous data werecompared using the student's t test for normally distributed data, or theMann-Whitney U test for non-normally distributed data. Results were consideredstatistically significant when P values were <0.05. MedCalc v.12.0(MedCalc Software, Belgium) was used for statistical analysis.
Results
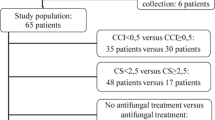
There were 213 ICU admissions with SAP during the study period. There were 32re-admissions of 26 patients during the same hospital stay. Seventy-six patients wereexcluded as they were directly transferred to the ICU from other hospitals. Fourpatients already had established candidal infection on admission to ICU and wereexcluded from further analysis (Figure 1). Therefore, 101 patientswere included of whom 58 (57%) were men. The median (IQR) age was 60 (50 to 73) years,and the most common causes of SAP were gallstones (45 (44.6%)) and alcohol (30 (29.7%)(Table 1)
There was no significant difference in APACHE II scores between the two groups. Eighteen(17.8%) patients developed ICI. Patients with ICI had a longer median length of ICU stay(16.9 versus 7.3 days, P = 0.0043). There was a significant association betweenopen necrosectomy and subsequent ICI (Table 1, P =0.0171) on univariate analysis, but this was not significant in regression analysis.Overall, 18 (17.8%) patients died in ICU with a higher mortality in patients with ICI(5/18 (27.8%) versus 13/83 (15.7%)). Overall hospital mortality was 29.7% (30/101) whichwas significantly higher in patients who developed ICI: 10/18 patients (55.6%) died,compared to 20 deaths in 83 patients without ICI (24.1%) (P = 0.0201) (Table1).
Table 2 displays the risk factors for development of ICI for thosepatients with and without ICI. There were no significant differences in incidence ofsevere sepsis, or use of CVC lines, antibiotics, RRT, steroids, immunosuppressivetherapy, previous surgery or TPN between the two groups. Of the known risk factors, onlycolonisation with Candida spp. was significantly greater in the ICI group.Sixteen (88.9%) patients with invasive candida infection were colonised with candida, asopposed to 37 (44.6%) without subsequent infection (P = 0.0006) (Table 2). Using logistic regression analysis, colonisation with candida (OR4.33) was the only factor significantly associated with invasive candidal infection(Table 3).
Candida infections
Eighteen patients developed ICI, giving an infection rate of 13.2 per 1,000 days(18/1,359 days). Candidaemia was present in 5 (27.8%) infected patients (3.7 per1,000 days). Five patients had only candidaemia, whereas three patients withcandidaemia also had either tissue or abdominal fluid samples that were positive forcandida spp. Candida spp. were isolated in pancreatic tissue infour patients. Ten patients had Candida in abdominal drain fluid samplesonly and received antifungal medication.
Candida species isolated
In the patients with a positive blood or tissue culture, C. albicans wasisolated in seven patients, C. glabrata and C. lusitaniae each inone patient and C. albicans and C. glabrata in one patient. In patients whohad a positive drain fluid culture and subsequent antifungal therapy, there werethree patients with C. albicans, two with C. glabrata and one eachwith C. parapsilosis and C. lusitaniae. One sample contained amixed growth of C. albicans and C. parapsilosis (Figure 2a and 2b).
Candidal species isolated. (a) The number of candidal speciesisolated from patients. The left hand bar shows the contribution of candidalspecies isolated from patients, including mixed growth; the right hand barshows single isolates only. (b) The proportion of each candidal speciescultured from all positive isolates in patients classified as infected withcandida.
Candida risk scores
Data regarding colonisation screening were not available for six patients and sothese were excluded from analysis of the performance of the CCIS. The risk predictionscores tested demonstrated low sensitivities, with values below 0.7 (Table 4). The Candida Score had the highest specificity of 0.85 and theCCIS had a specificity of 0.79. All scoring systems had high NPVs (>0.7). PPVs wereall below 0.5. The CCIS demonstrated a LR + of 3.2 and the other scores tested hadlower LR + values. No scores had LR - below 0.1.
The CCIS had the best discrimination of the scores tested, with AUROC of 0.79 (Figure3). The other two scores demonstrated poor discrimination,with AUROCs less than 0.7.
Discussion
An increase in Candida infection in non-neutropenic critically ill patients has beendemonstrated to put them at increased risk of mortality and morbidity [4, 6]. Whilst there is a concern that this is the case in patients with SAP [10, 11, 25–28], this has not been universally demonstrated [12–15]. It is, however, likely that colonisation plays an important instigating rolein these invasive infections. Patients with SAP are at particular risk of ICI. In thisstudy both colonisation with Candida spp. and a CCIS >0.5 were associated withsubsequent infection [8]. It can be difficult to distinguish colonisation from ICI. There is evidencethat delaying antifungals in ICI is associated with increased mortality [29]; however, current antimicrobial culture techniques can still take up to 72hours to grow yeasts [30]. Therefore, the unanswered question is whether critically ill patients withSAP should receive routine prophylactic antifungals with the risk of selecting outresistant strains of candida or whether treatment should be delayed until a positiveculture is obtained.
Aetiology and infection
The aetiology of SAP in this study was predominantly gallstones (44%) or alcohol(30%). In this study, as in previous studies, there was no difference in theincidence of ICI in patients with either aetiology [31].
Our data indicate that a clinically significant proportion of patients (17.8%) withSAP develop ICI during their ICU admission, giving an infection rate of 13.2 per1,000 days for ICI and 3.7 per 1,000 days for candidaemia. However, as our dataincludes infections other than candidaemias, the infection rate is higher than othershave demonstrated [7, 32, 33]. ICI was associated with both a longer ICU length of stay and higherhospital mortality. APACHE II scoring did not distinguish between the two groups(median APACHE II scores were 17 and 16 for patients with and without ICI,respectively). Other groups have identified an association in critically ill patientsbetween severity of illness and prevalence of ICI [8, 11]. It might be expected that the prevalence of candidal infection should behigher in those with a greater severity of illness. Pittet et al. found thatan APACHE II score of 20 or above was associated with increased nosocomial infections [8]. Our patients had a lower median APACHE II score than described in otherstudies that included critically ill patients with fungal infections, which maypartly explain why we did not find the same association with candidal infection.
Risk factors for invasive candidal infection
Previously identified risk factors for the development of fungal infection incritically ill patients include the presence of CVCs, the use of antibiotics andsteroids, recent abdominal surgery and TPN [5–7, 34]. In this study only colonisation with candida was identified as beingsignificantly associated with subsequent candidal infection. Although we did not findan association between abdominal surgery prior to admission and candidal infection,there was a significant association between open necrosectomy and subsequent ICI onunivariate analysis (Table 1). However, since opennecrosectomies are performed less frequently and are reserved for more complex anddifficult cases, this finding should be interpreted with caution since it may wellrepresent a confounding factor. Indeed, on logistic regression analysis, opennecrosectomy was not associated with candidal infection (Table 3). Antibiotics, steroids, CVC, TPN, RRT, immunosuppression and previousabdominal surgery were not associated with ICI in this study. In previous studies,the use of broad-spectrum antibiotics has been consistently associated with candidalinfection [8, 27, 28, 34, 35]. One explanation for this discrepancy may be that we only looked at aperiod of three days after ICU admission when antibiotics were used and not theperiod before ICU admission.
Our data differ from those of other groups who have consistently demonstratedsurgery, TPN and severe sepsis to be predictors of candidal infection in anunselected group of critically ill patients [6, 34]; however, the number of patients who developed ICI in this study wassmall. More than 90% of our cohort of patients had central venous access and,therefore, it is perhaps not surprising that this did not discriminate betweenpatients with and without ICI.
Colonisation
Leon et al. demonstrated that multifocal colonisation (two or morenon-contiguous sites) was a predictor of ICI [6]. The results of this study support the finding that colonisation is a riskfactor for later infection with an odds ratio of 4.49 (Table 3). Simple numerical number of colonisation sites has been disputed as atechnique sophisticated enough to predict invasive infection; and Pittet etal. developed a 'corrected colonisation index' that expressed the intensityof colonisation rather than just the number of sites [8]. A threshold index of 0.5 (positive/sites tested) was able to identifypatients who went on to develop invasive bloodstream or other sterile site infection [8]. Our data demonstrated a significant association between candidacolonisation and development of ICI, when compared to patients without ICI (88.9%versus 44.6% P = 0.006).
The CCIS had a NPV of 0.91 (Table 4) and specificity of 0.79,that is, patients with a CCIS <0.5 are unlikely to have invasive infection,although the negative LR was 0.4, above the value of 0.1 that has been suggested asbeing useful at the bedside [36]. The CCIS may be the most useful test to identify those patients who areunlikely to benefit from antifungal therapy. In these patients, the risks ofadministering prophylactic antifungals may outweigh the benefits. Using this rule inthis cohort of patients, 28 (27.7%) would have received prophylactic antifungals, 16of whom were 'false positives', and six patients would not have received prophylacticantifungals when they actually had an invasive candidal infection.
Performance and discrimination of risk scores for invasive candidal infection
The AUROC is a measure of discriminative power with values above 0.8 suggestingexcellent discrimination [37]. The CCIS was the most discriminating test between patients with invasiveinfection and those without, as assessed by the AUROC, with an AUROC of 0.79 (95% CI0.69-0.87) (Figure 3). The other two scores did not show gooddiscrimination in this cohort of patients (Table 4).
Although the PPV (0.43) and LR+ (3.2) were greatest for the CCIS among the threescores tested, they are not high enough to be clinically useful [36]. In agreement with other studies [37], the existing scoring systems are good at identifying those at lower riskof developing invasive candidal disease, since all scores showed reasonablespecificities and NPV (Table 4).
Limitations
This study is limited in its retrospective nature with the risk of missing data. TrueICI is also difficult to identify. Our definition of ICI in those patients who hadcandida in abdominal fluid and received antifungal treatment could be disputed, as itmay not be a completely accurate indicator of invasive disease. However, given theretrospective nature of this study, it is an appropriate assumption that patients whoreceived antifungal therapy after a positive fluid culture represented trueinfection.
Another weakness in this study is that routine surveillance swabs of patients withSAP are not taken, so it could be argued that the association between colonisationand infection is not causative, since patients without signs of infection are lesslikely to have been screened. However, there was no significant difference in theproportion of patients with ICI who were screened (100%) and those without ICI whowere screened (92.8%, P = 0.587). Patients known to be colonised withcandida who then cultured candida in abdominal fluid may have been more likely toreceive antifungal treatment, representing a confounding factor, despite the inputfrom a medical microbiologist. The data may also be skewed by our hospital being atertiary referral centre and receiving patients at varying stages of their disease.Finally, the study was conducted at a single-centre, and so our results may not beapplicable to other health-care settings.
Conclusions
Patients with SAP are known to be at high risk for ICI. We have demonstrated that ICI inSAP patients is associated with increased hospital mortality and longer duration of ICUstay. We have also shown that one of the existing risk scoring systems (CCIS [8]) in a population of critically ill patients with SAP has good discriminationto identify patients who are at low risk of developing ICI. Patients who have a CCIS of<0.5 are unlikely to go on to develop invasive candida infections. Further studiesinvestigating the benefit of prophylactic antifungal treatment in patients with SAP anda CCIS of ≥ 0.5 are needed.
Key messages
-
Patients with pancreatitis and invasive fungal infection havesignificantly greater hospital mortality.
-
Existing scoring systems are good at discriminating patients at lowrisk of developing invasive candidal infection.
-
Colonisation significantly increases the risk of invasiveinfection.
-
Patients with a CCIS of <0.5 are unlikely to develop invasiveinfection.
Abbreviations
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- CCIS:
-
Candida Colonisation IndexScore
- CVC:
-
central venous catheter
- ICI:
-
invasive candidal infection
- LR:
-
likelihoodratio
- MIRPN:
-
minimally invasive pancreatic necrosectomy
- NPV:
-
negative predictivevalue
- PICC:
-
peripherally inserted central catheter
- PPV:
-
positive predictive value
- RRT:
-
renal replacement therapy
- SAP:
-
severe acute pancreatitis
- TPN:
-
total parenteralnutrition
- 95% CI:
-
95% confidence interval.
References
Martin GS, Mannino DM, Eaton S, Moss M: The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003, 348: 1546-1554. 10.1056/NEJMoa022139
Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K, EPIC II Group of Investigators: International study of the prevalence and outcomes of infection in intensive careunits. JAMA 2009, 302: 2323-2329. 10.1001/jama.2009.1754
Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D, Sepsis Occurrence in Acutely Ill Patients Investigators: Sepsis in European intensive care units: results of the SOAP study. Crit Care Med 2006, 34: 344-353. 10.1097/01.CCM.0000194725.48928.3A
Trick WE, Fridkin SK, Edwards JR, Hajjeh RA, Gaynes RP, National Nosocomial Infections Surveillance System Hospitals: Secular trend of hospital-acquired candidemia among intensive care unit patientsin the United States during 1989-1999. Clin Infect Dis 2002, 35: 627-630. 10.1086/342300
Blumberg HM, Jarvis WR, Soucie JM, Edwards JE, Patterson JE, Pfaller MA, Rangel-Frausto MS, Rinaldi MG, Saiman L, Wiblin RT, Wenzel RP, National Epidemiology of Mycoses Survey (NEMIS) Study Group: Risk factors for candidal bloodstream infections in surgical intensive care unitpatients: the NEMIS prospective multicenter study. The National Epidemiology ofMycosis Survey. Clin Infect Dis 2001, 33: 177-186. 10.1086/321811
Leon C, Ruiz-Santana S, Saavedra P, Almirante B, Nolla-Salas J, Alvarez-Lerma F, Garnacho-Montero J, Leon MA: A bedside scoring system ("Candida score") for early antifungal treatment innonneutropenic critically ill patients with Candida colonization. Crit Care Med 2006, 34: 730-737. 10.1097/01.CCM.0000202208.37364.7D
Leroy O, Gangneux JP, Montravers P, Mira JP, Gouin F, Sollet JP, Carlet J, Reynes J, Rosenheim M, Regnier B, Lortholary O, AmarCand Study Group: Epidemiology, management, and risk factors for death of invasive Candidainfections in critical care: a multicenter, prospective, observational study inFrance (2005-2006). Crit Care Med 2009, 37: 1612-1618. 10.1097/CCM.0b013e31819efac0
Pittet D, Monod M, Suter PM, Frenk E, Auckenthaler R: Candida colonization and subsequent infections in critically ill surgicalpatients. Ann Surg 1994, 220: 751-758. 10.1097/00000658-199412000-00008
Ostrosky-Zeichner L, Sable C, Sobel J, Alexander BD, Donowitz G, Kan V, Kauffman CA, Kett D, Larsen RA, Morrison V, Nucci M, Pappas PG, Bradley ME, Major S, Zimmer L, Wallace D, Dismukes WE, Rex JH: Multicenter retrospective development and validation of a clinical prediction rulefor nosocomial invasive candidiasis in the intensive care setting. Eur J Clin Microbiol Infect Dis 2007, 26: 271-276. 10.1007/s10096-007-0270-z
Connor S, Alexakis N, Neal T, Raraty M, Ghaneh P, Evans J, Hughes M, Rowlands P, Garvey CJ, Sutton R, Neoptolemos JP: Fungal infection but not type of bacterial infection is associated with a highmortality in primary and secondary infected pancreatic necrosis. Dig Surg 2004, 21: 297-304. 10.1159/000080884
Gotzinger P, Wamser P, Barlan M, Sautner T, Jakesz R, Fugger R: Candida infection of local necrosis in severe acute pancreatitis is associatedwith increased mortality. Shock 2000, 14: 320-323. discussion 323-324 10.1097/00024382-200014030-00014
De Waele JJ, Vogelaers D, Blot S, Colardyn F: Fungal infections in patients with severe acute pancreatitis and the use ofprophylactic therapy. Clin Infect Dis 2003, 37: 208-213. 10.1086/375603
Gloor B, Muller CA, Worni M, Stahel PF, Redaelli C, Uhl W, Buchler MW: Pancreatic infection in severe pancreatitis: the role of fungus and multiresistantorganisms. Arch Surg 2001, 136: 592-596. 10.1001/archsurg.136.5.592
King NK, Siriwardana HP, Wood B, Siriwardena AK: Trends in fungal colonization of pancreatic necrosis in patients undergoingnecrosectomy for acute pancreatitis. HPB (Oxford) 2005, 7: 120-123. 10.1080/13651820510028837
Vege SS, Gardner TB, Chari ST, Baron TH, Clain JE, Pearson RK, Petersen BT, Farnell MB, Sarr MG: Outcomes of intra-abdominal fungal vs. bacterial infections in severe acutepancreatitis. Am J Gastroenterol 2009, 104: 2065-2070. 10.1038/ajg.2009.280
Eggimann P, Francioli P, Bille J, Schneider R, Wu MM, Chapuis G, Chiolero R, Pannatier A, Schilling J, Geroulanos S, Glauser MP, Calandra T: Fluconazole prophylaxis prevents intra-abdominal candidiasis in high-risk surgicalpatients. Crit Care Med 1999, 27: 1066-1072. 10.1097/00003246-199906000-00019
Faiz S, Neale B, Rios E, Campos T, Parsley E, Patel B, Ostrosky-Zeichner L: Risk-based fluconazole prophylaxis of Candida bloodstream infection in a medicalintensive care unit. Eur J Clin Microbiol Infect Dis 2009, 28: 689-692. 10.1007/s10096-008-0666-4
Garbino J, Lew DP, Romand JA, Hugonnet S, Auckenthaler R, Pittet D: Prevention of severe Candida infections in nonneutropenic, high-risk, criticallyill patients: a randomized, double-blind, placebo-controlled trial in patientstreated by selective digestive decontamination. Intensive Care Med 2002, 28: 1708-1717. 10.1007/s00134-002-1540-y
Pelz RK, Hendrix CW, Swoboda SM, Diener-West M, Merz WG, Hammond J, Lipsett PA: Double-blind placebo-controlled trial of fluconazole to prevent candidalinfections in critically ill surgical patients. Ann Surg 2001, 233: 542-548. 10.1097/00000658-200104000-00010
Mean M, Marchetti O, Calandra T: Bench-to-bedside review: Candida infections in the intensive care unit. Crit Care 2008, 12: 204. 10.1186/cc6212
Nathens AB, Curtis JR, Beale RJ, Cook DJ, Moreno RP, Romand JA, Skerrett SJ, Stapleton RD, Ware LB, Waldmann CS: Management of the critically ill patient with severe acute pancreatitis. Crit Care Med 2004, 32: 2524-2536. 10.1097/01.CCM.0000148222.09869.92
Scoring systems for ICU and surgical patients: APACHE II[http://www.sfar.org/score2/apache22.html]
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003, 31: 1250-1256. 10.1097/01.CCM.0000050454.01978.3B
DeLong ER, DeLong DM, Clarke-Pearson DL: Comparing the areas under two or more correlated receiver operating characteristiccurves: a nonparametric approach. Biometrics 1988, 44: 837-845. 10.2307/2531595
Grewe M, Tsiotos GG, Luque de-Leon E, Sarr MG: Fungal infection in acute necrotizing pancreatitis. J Am Coll Surg 1999, 188: 408-414. 10.1016/S1072-7515(98)00334-2
Hoerauf A, Hammer S, Muller-Myhsok B, Rupprecht H: Intra-abdominal Candida infection during acute necrotizing pancreatitis has a highprevalence and is associated with increased mortality. Crit Care Med 1998, 26: 2010-2015. 10.1097/00003246-199812000-00031
Isenmann R, Schwarz M, Rau B, Trautmann M, Schober W, Beger HG: Characteristics of infection with Candida species in patients with necrotizingpancreatitis. World J Surg 2002, 26: 372-376. 10.1007/s00268-001-0146-9
Kochhar R, Ahammed SK, Chakrabarti A, Ray P, Sinha SK, Dutta U, Wig JD, Singh K: Prevalence and outcome of fungal infection in patients with severe acutepancreatitis. J Gastroenterol Hepatol 2009, 24: 743-747. 10.1111/j.1440-1746.2008.05712.x
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, Gurka D, Kumar A, Cheang M: Duration of hypotension before initiation of effective antimicrobial therapy isthe critical determinant of survival in human septic shock. Crit Care Med 2006, 34: 1589-1596. 10.1097/01.CCM.0000217961.75225.E9
Playford EG, Lipman J, Kabir M, McBryde ES, Nimmo GR, Lau A, Sorrell TC: Assessment of clinical risk predictive rules for invasive candidiasis in aprospective multicentre cohort of ICU patients. Intensive Care Med 2009, 35: 2141-2145. 10.1007/s00134-009-1619-9
Chakrabarti A, Rao P, Tarai B, Shivaprakash MR, Wig J: Candida in acute pancreatitis. Surg Today 2007, 37: 207-211. 10.1007/s00595-006-3371-x
Gudlaugsson O, Gillespie S, Lee K, Vande Berg J, Hu J, Messer S, Herwaldt L, Pfaller M, Diekema D: Attributable mortality of nosocomial candidemia, revisited. Clin Infect Dis 2003, 37: 1172-1177. 10.1086/378745
Marchetti O, Bille J, Fluckiger U, Eggimann P, Ruef C, Garbino J, Calandra T, Glauser MP, Täuber MG, Pittet D, Fungal Infection Network of Switzerland: Epidemiology of candidemia in Swiss tertiary care hospitals: secular trends,1991-2000. Clin Infect Dis 2004, 38: 311-320. 10.1086/380637
León C, Ruiz-Santana S, Saavedra P, Galván B, Blanco A, Castro C, Balasini C, Utande-Vázquez A, González de Molina FJ, Blasco-Navalproto MA, López MJ, Charles PE, Martín E, Hernández-Viera MA, Cava Study Group: Usefulness of the "Candida score" for discriminating between Candida colonizationand invasive candidiasis in non-neutropenic critically ill patients: a prospectivemulticenter study. Crit Care Med 2009, 37: 1624-1633. 10.1097/CCM.0b013e31819daa14
Sobel JD: Candida infections in the intensive care unit. Crit Care Clin 1988, 4: 325-344.
Ridley S: Cardiac scoring systems--what is their value? Anaesthesia 2003, 58: 985-991. 10.1046/j.1365-2044.2003.03342.x
Hermsen ED, Zapapas MK, Maiefski M, Rupp ME, Freifeld AG, Kalil AC: Validation and comparison of clinical prediction rules for invasive candidiasis inintensive care unit patients: a matched case-control study. Crit Care 2011, 15: R198. 10.1186/cc10366
Acknowledgements
We would like to acknowledge the Hepatopancreatobiliary Surgeons at the RoyalLiverpool University Hospital (Professor John Neoptolomos, Professor Paula Ghaneh,Professor Robert Sutton and Mr Michael Raraty) and the departmental Clinical NurseSpecialists (Jo Garry and Faye Hughes).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AH carried out the data collection, statistical analysis and manuscript drafting. LPparticipated in the study design, data collection and manuscript drafting. BRparticipated in the study design and data collection. AW carried out data collection. MFcarried out the microbiological results collection and data collection. TN participatedin study design and microbiological results collection. CH contributed to the discussionand statistical analysis and critically reviewed the manuscript. TC provided statisticaladvice. PH conceived the study and participated in its design, data collection,statistical analysis and manuscript drafting. All authors read and approved the finalmanuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Hall, A.M., Poole, L.A., Renton, B. et al. Prediction of invasive candidal infection in critically ill patients with severeacute pancreatitis. Crit Care 17, R49 (2013). https://doi.org/10.1186/cc12569
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc12569