Abstract
Introduction
The correction of hypovolemia with acellular fluids results in acute normovolemic anemia. Whether the choice of the infusion fluid has an impact on the maintenance of oxygen (O2) supply during acute normovolemic anemia has not been investigated so far.
Methods
Thirty-six anesthetized and mechanically ventilated pigs were hemodiluted to their physiological limit of anemia tolerance, reflected by the individual critical hemoglobin concentration (Hbcrit). Hbcrit was defined as the Hb-concentration corresponding with the onset of supply-dependency of total body O2-consumption (VO2). The hemodilution protocol was randomly performed with either tetrastarch (6% HES 130/0.4, TS-group, n = 9), gelatin (3.5% urea-crosslinked polygeline, GEL-group, n = 9), hetastarch (6% HES 450/0.7, HS-group, n = 9) or Ringer's solution (RS-group, n = 9). The primary endpoint was the dimension of Hbcrit, secondary endpoints were parameters of central hemodynamics, O2 transport and tissue oxygenation.
Results
In each animal, normovolemia was maintained throughout the protocol. Hbcrit was met at 3.7 ± 0.6 g/dl (RS), 3.0 ± 0.6 g/dl (HS P < 0.05 vs. RS), 2.7 ± 0.6 g/dl (GEL, P < 0.05 vs. RS) and 2.1 ± 0.4 g/dl (TS, P < 0.05 vs. GEL, HS and RS). Hemodilution with RS resulted in a significant increase of extravascular lung water index (EVLWI) and a decrease of arterial oxygen partial pressure (paO2), and O2 extraction ratio was increased, when animals of the TS-, GEL- and HS-groups met their individual Hbcrit.
Conclusions
The choice of the intravenous fluid has an impact on the tolerance of acute normovolemic anemia induced by acellular volume replacement. Third-generation tetrastarch preparations (e.g., HES 130/0.4) appear most advantageous regarding maintenance of tissue oxygenation during progressive anemia. The underlying mechanism includes a lower degree of extravasation and favourable effects on microcirculatory function.
Similar content being viewed by others
Introduction
The correction of hypovolemia is an essential goal in the treatment of critically ill patients. However, the use of acellular fluids (that is, crystalloid or colloidal solutions) results in the dilution of the circulating cell mass (acute normovolemic anemia) with a corresponding decrease of O2 transport capacity [1–3].
Acute normovolemic anemia is initially compensated by increases of cardiac output and arterio-venous O2 extraction [4]. Moreover, O2 supply (DO2) physiologically exceeds O2 demand (reflected by total body O2 consumption (VO2) under resting conditions) by the factor three to four. When DO2 begins to decrease at lower Hb concentrations, the total body O2 demand is still met, and VO2 remains constant despite decreasing Hb concentrations (O2 supply-independency of VO2). When DO2 falls below a critical value, the amount of O2 delivered to the tissues becomes insufficient to meet their O2 demand and VO2 starts to decline (O2 supply-dependency of VO2) [5]. The corresponding critical hemoglobin concentration (Hbcrit) represents the ultimate limit of the individual anemia tolerance.
Among clinicians all over the world, infusion practice varies considerably and different intravenous (IV) fluids are used for volume replacement [6]. However, currently available IV fluids differ in their pharmacodynamic and kinetic profile (for example, molecular weight, plasma half-life, volume expansion effect) and in their effects on rheology and microcirculatory function.
We hypothesized that these properties might have an influence on the tolerance of acute normovolemic anemia. In this regard, the present study was conceived to compare potential effects of four commonly used IV fluids: low-molecular hydroxyethyl starch (HES) (tetrastarch, 6% HES 130/0.4), high-molecular HES (hetastarch, 6% HES 450/0.7), gelatin (3.5% urea-crosslinked polygeline), and crystalloid volume replacement with Ringer's solution.
Materials and methods
After approval by the local governmental review board (Regional Council Darmstadt, department for veterinary affairs/V54), experiments were performed in 36 healthy farm-bred pigs of either sex (body weight 24.0 ± 3.7 kg). All animals received good care in compliance with the Guide for the Care and Use of Laboratory Animals.
Anesthesia and ventilation
Animals were denied food 12 hours before each experiment started, but had free access to water. After intramuscular premedication with 10 mg/kg ketamine (Ketavet™, Parke-Davis, Berlin, Germany) and 1 mg/kg midazolam (Midazolam™, Ratiopharm, Ulm, Germany), anesthesia was induced by IV injection of 3 mg/kg propofol (Propofol™, Braun, Melsungen, Germany) and 30 μg/kg fentanyl (Fentanyl™, Janssen, Neuss, Germany) and maintained by continuous infusion of propofol (0.16 mg/kg/min), midazolam (0.01 mg/kg/min) and fentanyl (0.8 μg/kg/min). To facilitate ventilation, muscular paralysis was achieved with pancuronium bromide (Pancuronium™, DeltaSelect, Dreieich, Germany, bolus injection 0.2 mg/kg after induction of anesthesia, followed by continuous infusion of 0.13 mg/kg/min). Estimated fluid losses were replaced with Ringer's solution (Ringer-Infusionslösung™, Braun, Melsungen, Germany, 3 mL/kg/h).
Animals were orotracheally intubated and ventilated with ambient air at a rate of 14 cycles/min and a positive end-expiratory pressure of 5 cmH2O (Servo 900B, SiemensElema, Solna, Sweden). Tidal volume was individually adjusted to provide arterial normocapnia and was then maintained throughout the entire protocol.
Instrumentation and monitoring
Animals were placed in the supine position and a five-lead electrocardiogram (II, V5) was installed for detection of arrhythmias and ST-segment changes. A double-lumen catheter (Arrow, Reading, PA, USA) was inserted into the cranial vena cava and a Swan-Ganz-Catheter (Baxter, Irvine, CA, USA) was floated into a branch of the pulmonary artery. Each one 6F introducer sheath (Arrow, Reading, PA, USA) was inserted into the right femoral vein and artery, respectively. For continuous measurement of arterial blood pressure and cardiac output, a thermodilution catheter was placed into the left femoral artery (Pulsion Medical Systems, Munich, Germany). Body core temperature was kept constant using a warming pad.
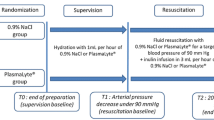
Experimental protocol
Upon completion of catheter insertion and installation of the different measuring devices, a 60 min stabilization period was allowed to elapse before the first data set was recorded (baseline). Subsequently, animals were randomized to undergo acute normovolemic hemodilution with one of the following fluids: 1) 6% HES 130/0.4 (tetrastarch, TS-group, n = 9); 2) 6% HES 450/0.7 (hetastarch, HS-group, n = 9); 3) 3.5% urea-crosslinked polygeline (gelatin, GEL-group, n = 9), or 4) Ringer's solution (RS-group, n = 9).
Acute normovolemic anemia was induced by withdrawal of blood (1mL/kg/min) and simultaneous infusion of one of the IV fluids. To maintain normovolemia during the hemodilution protocol, the following infusion rates were chosen with regard to the different plasma expansion effects of the fluids investigated (see Table 1): Ringer's solution 3 mL/kg/min, gelatin 1.2 mL/kg/min, tetrastarch and hetastarch 1 mL/kg/min, respectively. Infusion fluids were warmed in an immersion bath until IV infusion. For precise synchronization of blood withdrawal with the corresponding infusion rates, a bidirectional precision pump (Harvard Apparatus, Holliston, MA, USA) was used.
The target parameter of the hemodilution protocol was the animal's individual critical Hb concentration (Hbcrit), which was defined as the Hb concentration corresponding with a critical limitation of O2 delivery to the tissues (DO2) and the onset of O2 supply-dependency of total body O2 consumption-VO2 (see below). At the end of the hemodilution protocol, animals were killed by intracardiac injection of saturated potassium chloride solution.
Measurements
Intravascular blood volume was determined at baseline using the "whole-blood" method of the indocyanin green (ICG) indicator dilution technique, which has already been described in detail elsewhere [7]. The pressure transducers of the cardiovascular catheters were connected with a multi-channel recorder and a personal computer (Hugo-Sachs, March-Hugstetten, Germany) for continuous measurement of hemodynamic parameters. Cardiac output was continuously measured using the pulse contour analysis (PICCO classic monitor, Pulsion Medical Systems, Munich, Germany). The volumetric preload and extravasation parameters, intrathoracic blood volume (ITBV) and extravascular lung water (EVLW), were assessed after exchange of each 10% of the circulating blood volume using the transpulmonary thermodilution technique. Arterial and mixed venous blood samples were withdrawn at baseline, after exchange of each 10% of the circulating blood volume and at Hbcrit for blood gas analysis and assessment of Hb concentration (GEM-3000 and 682 CO-Oxymeter, Instrumentation Laboratory, Lexington, MA, USA).
Calculated parameters
Body surface area (BSA) was calculated according to Holt [8], from body weight (BW) and a species-dependent constant:
where k = 9 for the species pig.
The measured values of cardiac output (CO) and O2 consumption (VO2) were indexed to BSA:
Systemic and pulmonary vascular resistance indices (SVRI and PVRI) were calculated from standard formulae:
where MAP = mean arterial pressure, CVP = central venous pressure, CI = cardiac index, MPAP = mean pulmonary arterial pressure and PCWP = pulmonary capillary wedge pressure.
Arterial and mixed venous O2 content (CaO2 and CvO2), O2 delivery (DO2I) and O2 extraction ratio were calculated as follows:
Determination of Hbcrit
Hbcrit is the correlate of the critical limitation of DO2, and marks the onset of total body O2 supply-dependency. The corresponding decrease of VO2 was prospectively detected in an automated and investigator-independent manner: VO2 was measured every 60 sec with a metabolic monitor (Delta-Trac II™ MBM-200, Datex-Engstrom, Helsinki, Finland). VO2 values were simultaneously recorded and computed with specific software (Delta-Crit-System, DCS) [9]. During the stabilization period, the DCS enters VO2 values into an online regression analysis and calculates the mean and standard deviation (SD). During the subsequent hemodilution period, the VO2 value obtained every 60 secis compared to the mean value predicted by the DCS. When three consecutive VO2 values are outside the predefined range (3-fold SD of the regression line), a significant decrease of VO2 is assumed (see Figure 1) and the computer alerts visually and acoustically [9]. For determination of Hbcrit, the corresponding Hb concentration was measured in the arterial blood sample.
Typical example of a recording of total body oxygen consumption (VO 2 ) in the course of the experimental protocol. A linear regression analysis including the calculation of SD was performed with VO2 values collected during the 60-minute stabilization period. During the subsequent hemodilution protocol, a critical limitation of oxygen delivery (DO2) was assumed, when three consecutive VO2 values fell below the lower 3σ-range.
Statistics
Statistical analysis was performed with the SAS 9.1 software package (SAS Institute, Cary, NC, USA). All data are presented as mean ± SD. Distribution of data was assessed with the Shapiro-Wilk test. In the case of normal distribution, the time effect on the different variables, and differences between groups at different time points were tested by repeated analysis of variance (ANOVA). Post hoc analysis of differences detected with ANOVA was performed with the Student Newman Keuls test. In the case of non-normal distribution, the time effect on the parameters, and the between-group differences were tested by analysis of variance on ranks (rANOVA). Post hoc analysis of differences detected with rANOVA was performed with Tukey's test. For all parameters, statistical significance was accepted at P < 0.05.
Results
Baseline characteristics
On analysis of baseline body weight, blood volume index and all investigated parameters of hemodynamics and O2 transport, there were no significant differences detected between the groups (see Tables 2 and 3).
Primary endpoint: critical Hb concentation (Hbcrit)
Depending on the plasma substitute used for hemodilution, Hbcrit was met at 2.1 ± 0.4 g/dL (TS-group), 2.7 ± 0.6 g/dL (GEL-group), 3.0 ± 0.6 g/dL (HS-group) and 3.7 ± 0.6 g/dL (RS-group). The lowest value of Hbcrit was attained in the TS-group (P < 0.05 vs. GEL, HS and RS). While Hbcrit did not differ significantly between the GEL- and HS-groups, the difference between the RS-group and the other groups (GEL-, HS- and TS- groups) was statistically significant (see Figure 2).
Critical hemoglobin concentration ( crit obtained after induction of acute anemia. Anemia was induced using tetrastarch (TS-group, Hbcrit 2.1 ± 0.4 g/dL), gelatin (GEL-group, Hbcrit 2.7 ± 0.6 g/dL), hetastarch (HS-group, Hbcrit 3.0 ± 0.6 g/dL) or Ringer's solution (RS-group, Hbcrit 3.7 ± 0.6 g/dL). *P < 0.05 vs. GEL, #P < 0.05 vs. HS, §P < 0.05 vs. RS.
The induction of critical normovolemic anemia required the exchange of 69 ± 21% of the circulating blood volume (BV) for Ringer's solution, 71 ± 19% BV for hetastarch, 93 ± 44% BV for gelatin (P < 0.05 vs. HS- and RS-groups) and 107 ± 28% BV for tetrastarch (P < 0.05 vs. HS- and RS-groups). For maintenance of normovolemia, animals received 1,812 ± 535 mL tetrastarch, 2,016 ± 898 mL gelatin, 1,369 ± 324 mL hetastarch (P < 0.05 vs. TS-group), or 3,698 ± 1320 mL Ringer's solution, respectively (P < 0.05 vs. TS- GEL- and HS-groups).
Secondary endpoints: hemodynamic and O2-derived parameters
In Tables 2 and 3, hemodynamic and O2-derived parameters are presented at the respective critical Hb concentrations, that is, after hemodilution to 3.7 g/dL, 3.0 g/dL, 2.7 g/dL and 2.1 g/dL, respectively.
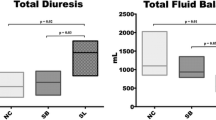
Hemodilution to Hb 3.7 g/dL (Hbcrit of the RS-group)
As compensation for hemodilution, cardiac index (CI) increased by 46 to 60% in all groups (P < 0.05 vs. baseline). Consistently, stroke volume index (SVI) and heart rate (HR) increased by 24 to 40% and 14 to 18%, respectively. While the increases in SVI were significant in the TS-group, GEL-, and RS-groups, the increase in HR was not significant in any group. Mean arterial pressure (MAP) decreased by 11 to 21% in the GEL-, HS- and RS-groups (non-significant) and systemic vascular resistance index (SVRI) decreased in all groups by 35 to 46% (P < 0.05 vs. baseline), while mean pulmonary arterial pressure (MPAP) increased by 22 to 50% (P < 0.05 vs. baseline in the GEL-, HS and RS-group). Stroke volume variation (SVV) remained unchanged in the RS-group and tended to decrease in the TS- and GEL-groups. In the HS-group, the decrease in SVV was statistically significant. Compared with baseline, ITBV index (ITBVI) increased in all groups (P < 0.05), reflecting increased venous return to the heart. The ITBVI was higher in animals hemodiluted with TS or HS than after fluid replacement with RS (P < 0.05). As a consequence of hemodilution, DO2I decreased by 14 to 30% in all groups (P < 0.05 vs. baseline). Moreover, the pH-value and base excess (BE) decreased significantly in the GEL-, HS- and RS-groups. As the protocol was terminated at the onset of the critical DO2, lactate concentration was not yet elevated at this time point (see Table 3). The EVLW index (EVLWI) was significantly increased in the RS-group (P < 0.05 vs. baseline and P < 0.05 vs. GEL-, HS- and TS-groups, see Figure 3). Consistently, arterial oxygen partial pressure (paO2) was decreased in the RS-group (P < 0.05 vs. baseline and P < 0.05 vs. GEL-, HS- and TS-groups).
Extravascular lung water index (EVLWI) obtained at baseline after hemodilution to Hb 3.7 g/dL (Hbcrit of the RS-group), Hb 3.0 g/dL (Hbcrit of the HS-group), Hb 2.7 (Hbcrit of the GEL-group) and Hb 2.1 (Hbcrit of the TS-group). At Hb 3.7 g/dL, EVLWI was significantly higher in the RS-group than in the TS-, GEL-, and HS-groups. *P < 0.05 vs. GEL, #P < 0.05 vs. HS, §P < 0.05 vs. RS, +P < 0.05 vs. baseline. Hbcrit, critical haemoglobin concentration, error bars represent standard deviation of mean.
Hemodilution to Hb 3.0 g/dL (Hbcrit of the HS-group)
As the limit of anemia tolerance was already met at Hb 3.7 g/dL in the RS-group, hemodilution to 3.0 g/dL could only be performed in the HS-, GEL- and TS-groups.
A slight increase in CI, HR and SVI and a decrease in MAP and SVRI was observed in these groups, and SVV was significantly reduced compared with baseline. The ITBVI did not change further, but remained elevated above the baseline level (P < 0.05). There were no differences between the HS-, GEL and TS-groups in hemodynamic parameters at Hb 3.0 g/dL.
Consistent with progressive hemodilution, DO2I further decreased in the remaining HS-, GEL- and TS-groups. In animals hemodiluted with hetastarch, O2 extraction was significantly increased as reflected by lower partial venous oxygen pressure (pvO2) (P < 0.05 vs. baseline and vs. GEL-group) and by a higher O2 extraction ratio (P < 0.05 vs. baseline and vs. GEL- and TS-groups).
Hemodilution to Hb 2.7 g/dL (that is, Hbcrit of the GEL-group)
Hemodilution could be continued to Hb 2.7 g/dL in the GEL- and TS-groups. CI did not increase further, but was now maintained by an elevation of HR in both groups (P < 0.05 vs. baseline). The MAP and SVRI decreased slightly (non-significant vs. baseline). In both groups, the ITBVI was still higher than at baseline (P < 0.05). However, at Hb 2.7 g/dL, the ITBVI was higher and SVV was lower in the TS-group (P < 0.05 vs. GEL-group). In the GEL-group, the O2 extraction ratio (O2-ER) and EVLWI were elevated when compared with baseline (P < 0.05, see Figure 3). No further differences between the TS- and GEL-groups were observed in hemodynamic or O2-derived parameters at Hb 2.7 g/dL.
Hemodilution to Hb 2.1 g/dL (Hbcrit of the TS-group)
Hemodilution could be performed most extensively with tetrastarch. When animals of the TS-group met their individual Hbcrit at 2.1 g/dL, the following changes were significantly different to baseline: HR, CI, SVI and EVLWI increased by 30%, 90%, 36% and 38%, while SVV, SVRI, DO2I, pvO2 and BE decreased by 52%, 64%, 40%, 15% and 72%, respectively (P < 0.05). Moreover, O2-ER increased by 38% and by 40% (see Table 3).
Discussion
The main findings of the present study are that during acute normovolemic anemia, 1) the choice of the IV fluid has an impact on the maintenance of tissue oxygenation as reflected by variation in the extent of anemia tolerance; 2) anemia tolerance is higher when using colloids than when using crystalloids, and 3) among the colloids, tetrastarch (6% HES 130/0.4) provided higher anemia tolerance than did gelatin (3.5% urea-crosslinked polygeline) and hetastarch (6% HES 450/0.7). This was reflected by significantly lower values of Hbcrit and a higher allowable volume of blood exchanged for tetrastarch.
Hbcrit is the hemoglobin concentration associated with a critical limitation of O2 supply and hallmarks the ultimate tolerance limit of acute normovolemic anemia [10, 11]. In our previous experimental studies, hemodilution to Hbcrit was associated with 100% mortality, if no further treatment (such as elevation of fraction of inspired O2, transfusion of red blood cells, or infusion of artificial O2 carriers) was initiated after institution of critical normovolemic anemia [12–14]. Several authors found Hbcrit at values between 1.6 and 3.0 g/dL [10, 12, 14–21]. In detail, Hbcrit was reduced by 1) hypothermia (moderate reduction of body core temperature reduces total body O2 demand [15]); 2) hyperoxemia (bioavailability of physically dissolved O2 is excellent in profound anemia [12, 16, 17]); 3) infusion of norepinephrine (stabilization of coronary perfusion pressure during hemodilution [19]); 4) artificial O2 carriers (maintenance of arterial oxygen content despite reduced hematocrit [18, 22]), and 5) con-tinuous neuromuscular blockade (lowering skeletal muscular O2 demand [23]).
While different infusion fluids were used for hemodilution in the aforementioned studies, their particular impact on the limit of anemia tolerance has not been fully elucidated. In a similar hemodilution study performed in anesthetized and splenectomised dogs, van der Linden and coworkers found no differences between pentastarch (6% HES 200/0.5) and a 3% gelatin preparation in relation to the value of Hbcrit [20]. However, the typical increase of CI in compensation for dilutional anemia was absent in that study, which was explained by cardio-depressant effects of the anesthesia regimen employed [20, 21].
In the present study, gelatin provided more extensive anemia tolerance than did hetastarch. While the occasional use of hetastarch is predominantly reported by US physicians [24], European physicians rather avoid this fluid due to its adverse effects on coagulation and renal function [25]. Nevertheless, a recent clinical study found a reduction of mortality in trauma victims resuscitated with hetastarch in addition to the advanced trauma life support (ATLS)-standard of care treatment (that is, crystalloids along with blood products) [26].
Hetastarch is a hyperoncotic infusion fluid with a high viscosity in vitro (see Table 1). However, the effects of these properties in vivo are still not fully understood. While a decrease of plasma viscosity entails the increase of venous return, thereby enabling the hemodynamic compensation of acute anemia [27], recent experimental data suggest that increased plasma viscosity prevents microvascular collapse (for example, after fluid resuscitation from hemorrhagic shock) [6]. Furthermore, the effect of hetastarch on plasma viscosity is limited by its oncotic properties, as the reabsorption of interstitial fluid involves the dilution of viscogenic materials thereby lowering plasma viscosity in the long term [28].
In the present study, animals hemodiluted with hetastarch featured a significantly higher O2-ER at Hbcrit when compared with animals of the TS- or GEL-group, indicating that macro- and microhemodynamic compensation of anemia was completely exhausted. In other words, hetastarch failed to prevent microcirculatory collapse at an earlier stage of hemodilution than did tetrastarch or gelatin. Although plasma viscosity was not assessed in the present study, it may be assumed that a dilution-related fading of viscogenic potential might have contributed to this result.
Whether fluid resuscitation should be performed with crystalloids or colloids, has been a matter of controversy for decades, and the discussion is still open [29]. Although most crystalloid infusion fluids are plasma-isotonic, they cross the capillary membranes within 20 to 30 minutes of infusion, and most of the volume infused is shifted into the interstitium. To maintain normovolemia with crystalloids, it has been recom-mended to replace an acute blood loss in a ratio of at least 1:3 [30]. However, the exclusive use of crystalloids for volume replacement results in edema formation and may thereby compromise tissue oxygenation [31]. Actually, excessive tissue hydration due to pure crystalloid volume replacement in the perioperative phase was held responsible for many postoperative complications including increased incidence of anastomotic dehiscence in abdominal surgery, postoperative vomiting and orthostatic dysregulation [32, 33]. Moreover, an experimental study in pigs subjected to colon anastomosis surgery found that microcirculatory blood flow and oxygen tension in perianastomotic colon tissue were increased in animals infused with tetrastarch when compared with crystalloid fluid management [34]. This finding was explained by homogenisation of mucosal microcirculatory blood flow after infusion of tetrastarch.
In the present study, with Ringer's solution, the exchange of blood was associated with increased pulmonary edema formation (elevated EVLWI) and an impairment of pulmonary gas exchange (decreased paO2). This phenomenon was not observed in animals hemodiluted with gelatin, hetastarch or tetrastarch. Although EVLWI merely reflects the degree of tissue hydration at the site of pulmonary circulation, it may be supposed that a relevant edema formation also occurred in peripheral O2-consuming tissues: while O2 extraction increased consistently in animals hemodiluted with any of these colloids, O2 extraction was not increased when animals of the RS-group met their individual Hbcrit. As this finding may reflect a microcirculatory disorder related to excessive tissue hydration, we conclude that the comparatively early VO2-decrease in the RS-group might, in addition to the anemia-related restriction of the O2 transport capacity, also be attributable to an edema-related impairment of O2 uptake at the site of pulmonary and peripheral microcirculation.
A certain transcapillary filtration rate is also characteristic for gelatin preparations [35]. Their low molecular weight (30 to 40 kDa) entails a rapid passage into the interstitial space and a rapid clearance by glomerular filtration, finally reducing volume efficacy to 80% (that is, 20% extravasation rate). Consistently, EVLWI increased much later in the GEL-group than in the RS-group. Moreover, when hemodilution was continued below Hb 3.7 g/dL, O2 extraction could be augmented, reflecting that microcirculatory function might have been maintained more adequately than in the RS-group.
The strict maintenance of normovolemia is essential for adequate hemodynamic compensation of acute anemia, that is, for the increase in cardiac output. However, one weakness of the present protocol is the verification of normovolemia at time points characterized by extreme anemia. During extreme hemodilution, the kinetic of ICG elimination is significantly altered by dilution of albumin and increased cardiac output. Therefore, a measurement of circulating blood volume at this point would yield results not comparable with the baseline measurement [7], so normovolemia was deduced from clinically assessable parameters, for example, ITBVI and SVV.
While ITBVI represents LV preload, decreases in SVV reflect adequate volume responsiveness. After hemodilution with either fluid, ITBVI increased above the baseline level, indicating that volume replacement was adequate to achieve macro-hemodynamic compensation of acute anemia (increase of venous return to the heart, augmentation of LV preload). However, the increase of ITBVI was more pronounced in the TS- and HS-groups. In the course of hemodilution, SVV decreased in the TS-, GEL-, and HS-groups. In the RS-group, SVV remained unchanged and at Hbcrit, it was significantly lower than in the HS-group. Both findings reflect that volume responsiveness was most strongly expressed in the starch groups. In the RS-group, however, volume responsiveness and volume efficacy were limited by partial extravasation despite infusion of 3 mL RS per mL blood withdrawn.
Although this procedure provided adequate LV preload for hemodynamic compensation of acute anemia, it may be argued that the infusion of higher volumes of RS (4 or 5 mL per mL blood withdrawn) might have elevated intravascular volume and might have improved volume responsiveness. On the other hand, extravasation and tissue hydration would have exacerbated and might have further impaired O2 uptake and tissue oxygenation.
Likewise, the volume effect of gelatin appeared to be limited by its short intravascular half-life and its extravasation tendency. No differences between the colloid groups were observed in LV preload or volume responsiveness until hemodilution to Hb 3.0 g/dL. However, after continuation of hemodilution to 2.7 g/dL, ITBVI tended to decrease and SVV to increase in the GEL-group, and both parameters differed significantly from the TS-group. Nevertheless, animals of the GEL-group still featured sufficient hemodynamic compensation of acute anemia (CI, SVI and ITBVI remained increased vs. baseline), which precludes that they were actually hypovolemic.
These findings indicate that 1) the infusion of 1.2 mL gelatin per mL blood withdrawn was adequate to maintain LV preload and volume responsiveness over a wide range of the hemodilution protocol; 2) in spite of this, the volume effect of gelatin could not be sustained until the end of the protocol, and 3) that extravasation and fading volume responsiveness might have compromised microvascular perfusion, which finally caused animals of the GEL-group to earlier achieve Hbcrit than the TS-group.
We chose Hbcrit as the primary endpoint of the hemodilution protocol. In our previous studies, lactate concentrations began to increase 60 to 90 minutes after institution of Hbcrit [12–14, 19]. Of note, we employed the identical hemodilution protocol in the present study but animals were killed immediately after achievement of Hbcrit, so that elevated lactate concentrations could not yet be expected.
In the present experimental model, the effects of the investigated infusion fluids became apparent when the O2 transport capacity was driven to its critical limit. Whether differences between the groups existed already at less severe degrees of anemia, is difficult to conclude.
However, a clinical investigation in healthy volunteers undergoing moderate hemodilution with different HES preparations (HES 130/0.4, HES 70/0.5 or HES 200/0.5) demonstrated that tetrastarch provided the most sustained increase of tissue O2 partial pressure (tpO2) [36].
In summary, our data suggest that the choice of the IV infusion fluid used for acellular volume replacement has an impact on the maintenance of O2 supply. Among the fluids investigated in the present study, tetrastarch (HES 130/0.4) provided the most extensive anemia tolerance when compared with gelatin, hetastarch or Ringer's solution. While the exact underlying mechanism remains to be elucidated, extravasation and formation of interstitial edema were associated with decreased anemia tolerance, indicating that the microcirculatory effects of the fluids investigated had a major impact on tissue oxygenation.
Conclusions
During acellular treatment of an acute blood loss in lieu of allogeneic blood transfusions (for example, correction of hypovolemia, bridging an unexpected massive blood loss, or declining of transfusion for religious reasons), modern low-molecular tetrastarch preparations (such as HES 130/0.4) appear most suitable to maintain O2 supply over a wide range of levels of acute normovolemic anemia.
Key messages
-
The correction of hypovolemia with acellular fluids implies the dilution of the cell mass remaining in the vasculature (acute normovolemic anemia).
-
Sustainment of normovolemia and nutritive microcirculatory blood flow has a major impact on the maintenance of tissue oxygenation and thereby on the tolerance of acute anemia.
-
The fluids investigated in the present study (tetrastarch, gelatin, hetastarch and Ringer's Solution) differed in their volume effects and their extravasation rate and might thereby have influenced microcirculatory function.
-
In profound anemia, modern low-molecular tetrastarch preparations were most advantageous to maintain normovolemia as well as tissue oxygenation.
Abbreviations
- ANOVA:
-
analysis of variance
- BE:
-
base excess
- BSA:
-
body surface area
- BVI:
-
circulating blood volume (indexed to BSA)
- CaO2:
-
arterial oxygen content
- CI:
-
cardiac index (cardiac output indexed to BSA)
- DO2:
-
oxygen delivery
- EVLWI:
-
extravascular lung water (indexed to BSA)
- Hbcrit:
-
critical hemoglobin concentration
- HES:
-
hydroxyethyl starch
- HR:
-
heart rate
- IV:
-
intravenous
- ICG:
-
indocyaningreen
- ITBVI:
-
intrathoracic blood volume (indexed to BSA)
- MAP:
-
mean arterial pressure
- MPAP:
-
mean pulmonary arterial pressure
- O2-ER:
-
oxygen extraction ratio
- paO2:
-
arterial oxygen partial pressure
- PCWP:
-
pulmonary capillary wedge pressure
- pvO2:
-
mixed-venous oxygen partial pressure
- SVI:
-
stroke volume (indexed to BSA)
- SVRI:
-
systemic vascular resistance (indexed to BSA)
- SVV:
-
stroke volume variation
- VO2:
-
total body oxygen consumption.
References
Messmer KF: Acceptable hematocrit levels in surgical patients. World J Surg 1987, 11: 41-46. 10.1007/BF01658458
Madjdpour C, Spahn DR, Weiskopf RB: Anemia and perioperative red blood cell transfusion: a matter of tolerance. Crit Care Med 2006, 34: S102-S108. 10.1097/01.CCM.0000214317.26717.73
Pape A, Habler O: Alternatives to allogeneic blood transfusions. Best Pract Res Clin Anaesthesiol 2007, 21: 221-239. 10.1016/j.bpa.2007.02.004
Habler OP, Messmer KF: The physiology of oxygen transport. Transfus Sci 1997, 18: 425-435. 10.1016/S0955-3886(97)00041-6
Schumacker PT, Cain SM: The concept of a critical oxygen delivery. Intensive Care Med 1987, 13: 223-229. 10.1007/BF00265110
Cabrales P, Tsai AG, Intaglietta M: Increased plasma viscosity prolongs microhemodynamic conditions during small volume resuscitation from hemorrhagic shock. Resuscitation 2008, 77: 379-386. 10.1016/j.resuscitation.2008.01.008
Haller M, Akbulut C, Brechtelsbauer H, Fett W, Briegel J, Finsterer U, Peter K: Determination of plasma volume with indocyanine green in man. Life Sci 1993, 53: 1597-1604. 10.1016/0024-3205(93)90183-4
Holt JP, Rhode EA, Kines H: Ventricular volumes and body weight in mammals. Am J Physiol 1968, 215: 704-715.
Meier JM, Woelkhammer S, Habler OP: The Deltacrit-System (DCS) - a new method for online-determination of critical VO 2 -decline. Comput Biol Med 2003, 33: 395-405. 10.1016/S0010-4825(03)00015-5
Cain SM: Oxygen delivery and uptake in dogs during anemic and hypoxic hypoxia. J Appl Physiol 1977, 42: 228-234.
De Backer D: VO2/DO2 relationship: how to get rid of methodological pitfalls? Intensive Care Med 2000, 26: 1719-1722. 10.1007/s001340000713
Meier JM, Kemming GI, Kisch-Wedel H, Wolkhammer S, Habler OP: Hyperoxic ventilation reduces 6-hour mortality at the critical hemoglobin concentration. Anesthesiology 2004, 100: 70-76. 10.1097/00000542-200401000-00014
Meier JM, Pape A, Lauscher P, Zwissler B, Habler OP: Hyperoxia in lethal methemoglobinemia - effects on O 2 transport, tissue oxygenation and survival in pigs. Crit Care Med 2005, 33: 1582-1588. 10.1097/01.CCM.0000170187.39166.FF
Pape A, Kertscho H, Meier J, Horn O, Laout M, Steche M, Lossen M, Theisen A, Zwissler B, Habler O: Improved short-term survival with polyethylene glycol modified hemoglobin liposomes in critical normovolemic anemia. Intensive Care Med 2008, 34: 1534-1543. 10.1007/s00134-008-1082-z
Perez-de-Sa V, Roscher R, Cunha-Goncalves D, Larsson A, Werner O: Mild hypothermia has minimal effects on the tolerance to severe progressive normovolemic anemia in Swine. Anesthesiology 2002, 97: 1189-1197. 10.1097/00000542-200211000-00024
Pape A, Meier J, Kertscho H, Steche M, Laout M, Schwerdel F, Wedel M, Zwissler B, Habler OP: Hyperoxic ventilation increases the tolerance of acute normovolemic anemia in anesthetized pigs. Crit Care Med 2006, 34: 1475-1482. 10.1097/01.CCM.0000215826.45839.36
Kemming GI, Meisner FG, Kleen MS, Meier JM, Tillmanns JH, Hutter JW, Wojtczyk CJ, Packert KB, Bottino DA, Habler OP: Hyperoxic ventilation at the critical haematocrit. Resuscitation 2003, 56: 289-297. 10.1016/S0300-9572(02)00408-2
Meisner FG, Kemming GI, Habler OP, Kleen MS, Tillmanns JH, Hutter JW, Bottino DA, Thein E, Meier JM, Wojtczyk CJ, Pape A, Messmer K: Diaspirin crosslinked hemoglobin enables extreme hemodilution beyond the critical hematocrit. Crit Care Med 2001, 29: 829-838. 10.1097/00003246-200104000-00030
Meier J, Pape A, Loniewska D, Lauscher P, Kertscho H, Zwissler B, Habler O: Norepinephrine increases tolerance to acute anemia. Crit Care Med 2007, 35: 1484-1492. 10.1097/01.CCM.0000265740.62130.1C
van der Linden P, Schmartz D, De Groote F, Mathieu N, Willaert P, Rausin I, Vincent JL: Critical haemoglobin concentration in anaesthetized dogs: comparison of two plasma substitutes. Br J Anaesth 1998, 81: 556-562. 10.1093/bja/81.4.556
van der Linden P, De Hert S, Mathieu N, Degroote F, Schmartz D, Zhang H, Vincent JL: Tolerance to acute isovolemic hemodilution. Effect of anesthetic depth. Anesthesiology 2003, 99: 97-104. 10.1097/00000542-200307000-00018
Habler OP, Kleen MS, Hutter JW, Podtschaske AH, Tiede M, Kemming GI, Welte MV, Corso CO, Batra S, Keipert PE, Faithfull NS, Messmer KF: Hemodilution and intravenous perflubron emulsion as an alternative to blood transfusion: effects on tissue oxygenation during profound hemodilution in anesthetized dogs. Transfusion 1998, 38: 145-155. 10.1046/j.1537-2995.1998.38298193096.x
Pape A, Kertscho H, Stein P, Lossen M, Horn O, Kutschker S, Zwissler B, Habler O: Neuromuscular blockade with rocuronium bromide increases the tolerance of acute normovolemic anemia in anesthetized pigs. Eur Surg Res 2011, 48: 16-25.
Treib J, Baron JF, Grauer MT, Strauss RG: An international view of hydroxyethyl starches. Intensive Care Med 1999, 25: 258-268. 10.1007/s001340050833
Ertmer C, Rehberg S, Van AH, Westphal M: Relevance of non-albumin colloids in intensive care medicine. Best Pract Res Clin Anaesthesiol 2009, 23: 193-212. 10.1016/j.bpa.2008.11.001
Ogilvie MP, Pereira BM, McKenney MG, McMahon PJ, Manning RJ, Namias N, Livingstone AS, Schulman CI, Proctor KG: First report on safety and efficacy of hetastarch solution for initial fluid resuscitation at a level 1 trauma center. J Am Coll Surg 2010, 210: 870-872. 10.1016/j.jamcollsurg.2010.01.010
Messmer K, Sunder-Plassmann L: Hemodilution. Prog Surg 1974, 13: 208-245.
Villela N, Salazar Vasquez B, Intaglietta M: Microcirculatory effects of intravenous fluids in critical illness: plasma expansion beyond cystalloids and colloids. Curr Opin Anaesthesiol 2009, 22: 163-167. 10.1097/ACO.0b013e328328d304
Ertmer C, Kampmeier T, Rehberg S, Lange M: Fluid resuscitation in multiple trauma patients. Curr Opin Anaesthesiol 2011, 24: 202-208. 10.1097/ACO.0b013e3283445326
Spahn DR, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Gordini G, Stahel PF, Hunt BJ, Komadina R, Neugebauer E, Ozier Y, Riddez L, Schultz A, Vincent JL, Rossaint R, Task Force for Advanced Bleeding Care in Trauma: Management of bleeding following major trauma: a European guideline. Crit Care 2007, 11: 412. 10.1186/cc5738
Tollofsrud S, Svennevig JL, Breivik H, Kongsgaard U, Ozer M, Hysing E, Mohr B, Seem E, Geiran O, Abdelnour M: Fluid balance and pulmonary functions during and after coronary artery bypass surgery: Ringer's acetate compared with dextran, polygeline, or albumin. Acta Anaesthesiol Scand 1995, 39: 671-677. 10.1111/j.1399-6576.1995.tb04146.x
Moretti EW, Robertson KM, El Moalem H, Gan TJ: Intraoperative colloid administration reduces postoperative nausea and vomiting and improves postoperative outcomes compared with crystalloid administration. Anesth Analg 2003, 96: 611-7.
Grocott MP, Mythen MG, Gan TJ: Perioperative fluid management and clinical outcomes in adults. Anesth Analg 2005, 100: 1093-1106. 10.1213/01.ANE.0000148691.33690.AC
Kimberger O, Arnberger M, Brandt S, Plock J, Sigurdsson GH, Kurz A, Hiltebrand L: Goal-directed colloid administration improves the microcirculation of healthy and perianastomotic colon. Anesthesiology 2009, 110: 496-504. 10.1097/ALN.0b013e31819841f6
Holbeck S, Grande PO: Effects on capillary fluid permeability and fluid exchange of albumin, dextran, gelatin, and hydroxyethyl starch in cat skeletal muscle. Crit Care Med 2000, 28: 1089-1095. 10.1097/00003246-200004000-00030
Standl T, Burmeister MA, Schroeder F, Currlin E, Schulte am EJ, Freitag M, Schulte am EJ: Hydroxyethyl starch (HES) 130/0.4 provides larger and faster increases in tissue oxygen tension in comparison with prehemodilution values than HES 70/0.5 or HES 200/0.5 in volunteers undergoing acute normovolemic hemodilution. Anesth Analg 2003, 96: 936-943.
Acknowledgements
The authors would like to thank Mr W Daut and his team for their excellent performance in animal care and Mr H Winkelmeier for his valuable technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The study was sponsored by a research grant from the Else Kröner-Fresenius-Foundation, Bad Homburg, Germany. The authors declare that they have no further competing interests.
Authors' contributions
AP, SK, HK, OH and ML carried out the experiments. SK coordinated data acquisition during the experiments and built up the database. PS performed the statistical analysis. AP, BZ and OH conceived the study and participated in its design. BZ and OH helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Pape, A., Kutschker, S., Kertscho, H. et al. The choice of the intravenous fluid influences the tolerance of acute normovolemic anemia in anesthetized domestic pigs. Crit Care 16, R69 (2012). https://doi.org/10.1186/cc11324
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11324