Abstract
Patients with rheumatoid arthritis (RA) are at risk of excess mortality, predominantly owing to cardiovascular (CV) events. The receptor for advanced glycation end products (RAGE) has been implicated in the perpetuation of the chronic inflammatory response in vascular disease. A Gly82→Ser polymorphism in the RAGE gene, which is associated with enhanced RAGE signaling, is present more frequently in patients with RA than the general population. To investigate whether RAGE Gly82→Ser polymorphism is associated with CV events in RA, we examined CV events, CV risk factors, features of RA and RAGE Gly82→Ser polymorphism in 232 patients with RA attending a tertiary referral hospital. CV events, the duration and severity of RA, and risk factors for CV disease were determined using patient questionnaires, chart review, laboratory analysis and radiographs. DNA was typed for HLA–DRB1 genes and RAGE Gly82→Ser polymorphism. The RAGE Ser82 allele, which is in linkage disequilibrium with the RA susceptibility allele HLA–DRB1*0401, was carried by 20% of patients. More than 20% of the cohort had suffered a vascular event; a shorter duration of RA, but not the RAGE genotype, was significantly associated with CV events. However, a history of statin use was protective. Thus, the RAGE Ser82 allele, associated with enhanced RAGE signaling, does not predispose to CV events in RA. However, treatment of hyperlipidemia with statins reduces the probability of a CV event.
Similar content being viewed by others
Introduction
The mortality of patients with rheumatoid arthritis (RA) is increased compared with the general population and most of this increase can be attributed to excess cardiovascular (CV) deaths [1]. Immune dysregulation and systemic inflammation have important roles in the accelerated atherosclerosis of RA. Serologic markers of inflammation, such as C-reactive protein (CRP) and serum amyloid A, are strongly associated with CV disease in the general population, in addition to systemic inflammatory diseases, including RA, systemic lupus erythematosus and inflammatory bowel disease [2–4]. Although the INTERHEART study showed 90% to 94% of the risk of myocardial infarction could be accounted for by conventional risk factors (abnormal lipids, smoking, hypertension, diabetes, abdominal obesity and inactivity), in addition to psychosocial factors and diet [5], the contribution of inflammation is associated with these risk factors. Inflammation might potentiate a prothrombotic inflammatory state, or promote metabolic and psychosocial factors, which affect disease [6, 7]. For example, smoking is a risk factor for both CV disease and RA and itself associated with the promotion of inflammation, characterized by elevated CRP levels [8]. For patients with inflammatory polyarthritis or RA, the baseline level of CRP or peak erythrocyte sedimentation rate (ESR) within the first year after onset has been independently associated with the risk of CV death [9, 10]. Thus, the progress of CV disease might depend on the burden of inflammation.
The receptor for advanced glycation end products (RAGE) is a multiligand member of the immunoglobulin superfamily of cell-surface receptor molecules encoded by chromosome 6 at the major histocompatability locus (MHC) class II/III junction [11]. When ligated, RAGE is implicated in atherogenesis and chronic inflammatory diseases by amplifying inflammatory events in tissues previously sensitized by lipid deposition or inflammatory triggers [12]. RAGE is expressed at low levels in normal tissues but upregulated at sites of vascular pathology or severe injury [13, 14]. RAGE ligands include the calgranulin family of S100 proteins, the cytokine amphoterin (high-mobility group box chromosomal protein (HMGB1)), β-pleated sheet fibrils of amyloid and advanced glycation end products (AGEs) [15]. AGEs are the products of nonenzymatic glycation and oxidation of proteins that form with aging, diabetes and renal failure, and at sites of inflammation (by oxidation) [16].
Levels of S100 proteins and HMGB1 are increased in both adult and juvenile RA [17], and inhibition of the RAGE has been shown to suppress inflammation in animal models of arthritis [18]. There are four polymorphisms of the RAGE, of which the Gly82→Ser functional dimorphism shows the highest prevalence [19]. Ser82 enhances receptor signaling through mitogen activated protein (MAP) kinases and nuclear factor of kappa B (NF-κB) [18]. The increased prevalence of Ser82 in RA might be accounted for by linkage disequilibrium with the RA-associated HLA–DRB1*0401 allele [11, 18, 20]. However, although RAGE has been implicated in atherosclerosis, and the vascular component of diabetes mellitus and renal disease, RAGE Gly82→Ser polymorphism showed no association with CV disease in the general population [21]. Here, we tested whether the RAGE Gly82→Ser polymorphism was associated with CV events in RA.
Materials and methods
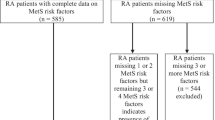
Patients
All current cases of RA, which met the American College of Rheumatology (ACR) 1987 revised criteria for the classification of RA [22], who presented for a scheduled appointment over a 5-month period (July to November 2003) at our tertiary hospital rheumatology clinic were invited to participate. Almost all RA patients regularly attending the rheumatology department, in addition to cases of recent onset, would be expected to have been captured during this timeframe. Patients completed a questionnaire detailing CV history, risk factors and their treatment, and details of RA and were clinically evaluated, with chart review for CV history, at least once. The study protocol was approved by the Princess Alexandra Hospital Research Ethics Committee (Brisbane, Australia).
Genotyping
High-resolution HLA–DRB1 genotyping was carried out on buffy-coat DNA using PCR and sequence-specific oligonucleotide probes. To delineate the RAGE Gly82→Ser polymorphism, PCR was carried out as previously described [18]. Shared epitope was considered positive if at least one DRB1 allele was one of the RA susceptibility alleles described by Gregersen and co-workers [20].
Assessment of cardiovascular events
To ascertain CV events, patients were asked for a history, dates and treatments of myocardial infarction (MI), angina, stroke, transient ischemic attack (TIA) or peripheral vascular disease (PVD), and these events were verified by reviewing the medical records. Although a number of patients had events before the diagnosis of RA, only CV events that occurred after RA diagnosis were included in the current analysis. Patients with multiple events had only one event counted per person. MI was identified if patients developed either of the following clinical signs: a typical rise and fall in the levels of biochemical markers consistent with myocardial necrosis, in addition to ischemic symptoms, development of pathologic Q waves on the electrocardiogram ECG and/or ECG changes indicative of ischemia (ST-segment elevation or depression); or either new pathologic Q waves on serial ECGs or pathologic changes of healed or healing MI [23]. Stroke or TIA was identified if patients had been admitted to the hospital with evidence of ischemic occlusion on computed tomography (CT) scanning, carotid endarterectomy, or symptoms of stroke/TIA, evidence of a significant plaque on carotid ultrasound and neurologic sequelae, with the exclusion of subarachnoid hemorrhage and space-occupying lesions. PVD was confirmed if Doppler ultrasonography showed significant large-vessel disease.
Assessment of potential cardiovascular risk factors
Cigarette smoking was assessed by questionnaire, which included details about past and present smoking habits, the number of cigarettes smoked per day and the number of years the patient had been a smoker. Diabetes mellitus was classified as present if patients had been diagnosed by a physician or were taking antidiabetic medications at the time of the assessment. A family history of CV or cerebrovascular attack before the age of 65 years in first-degree relatives and those with an average prednisone dose greater than 10 mg/day were determined by questionnaire. If stroke was deemed hemorrhagic, the history was not included. The body-mass index (BMI) was calculated as weight in kilograms divided by the square of the height in meters. Blood pressure was measured at the time of evaluation. Hypercholesterolemia and hypertension were identified if the diagnoses were recorded in medical records by a physician or patients were taking lipid-lowering or antihypertensive drugs at the time of the evaluation. The percentage risk of CV events over the next 5 years was estimated using the 'CV disease risk calculator' derived from the Framingham study [24] for patients between 30 and 74 years of age and without a history of clinical CV disease.
Laboratory data collected at the time of clinical evaluation included the fasting total cholesterol level, low-density lipoprotein (LDL) level, high-density lipoprotein (HDL) level, very-low-density lipoprotein (VLDL) level, triglyceride (TG) level, LDL: HDL cholesterol ratio, glucose level, renal and liver functions, CRP level, ESR, anti-cyclic citrullinated peptide anti-CCP antibody and rheumatoid factor (RF) status. A 12-lead ECG carried out within the previous 12 months was scored for evidence of Q waves, to ascertain possible silent coronary disease. Creatinine clearance (CrCl) was estimated for each patient on the basis of the serum creatinine (SCr) level, age (in years) and ideal body weight (in kg), using the Cockcroft and Gault method, as follows:
CrCl (ml/min) = [(140 - age) × (ideal weight)]/833 × SCr (mmol/l). For females, the formula was multiplied by 0.85 [25].
Assessment of rheumatoid arthritis radiographic severity
Hand radiographs carried out at the time of evaluation were scored for erosions and joint-space narrowing using the modified Sharp score [26].
Statistical analysis
Analyses were conducted using standard software (Excel 2003, Microsoft, Redmond, WA, USA; and Graphpad Prism 4 and SPSS version 12, SPSS Inc., Chicago, IL, USA). Correlates of the RAGE Ser82 isoform were sought in a logistic regression model. Demographic factors, CV risk factors, RA features, the RAGE Ser82 isoform and HLA–DRB1 genotype were assessed univariately as predictors of the time from RA diagnosis to a CV event, using Cox proportional hazards regression to compute hazard ratios (HRs), with Bonferroni correction for multiple comparisons. All variables that were significant at p < 0.10 on univariate analysis were added to the multivariate model. Variables significant at p < 0.05 on backwards, stepwise regression analysis were retained.
Results
Cardiovascular events experienced by rheumatoid arthritis patients within this cohort
We studied 232 patients with RA who had a mean disease duration of 15 years and mean age of 61.8 years (range, 17 to 87 years) for CV events, duration and features of RA, CV disease risk factors, and HLA–DRB1 and RAGE Gly82→Ser genotypes. The characteristics of the patients are shown in Table 1. Of the patients studied, 94% were Caucasian. The sample included nine Asian patients, three Australian aboriginals and one patient of Pacific island origin. Previously defined CV risk factors were common. Of the patients studied, 63% were positive for RF and 76% had radiographic evidence of erosive disease (Table 1). Eighteen patients who had an onset of RA within the previous 12 months were included; RA had been present for between 1 and 64 years in the remaining patients. More than 20% of patients had experienced, or developed during the course of the study, a vascular thromboembolic syndrome, including MI, an episode of angina, stroke, TIA and diagnosis of PVD. MI and angina accounted for the majority of CV morbidity, although some patients had suffered both events (Table 1). Two patients died within 12 months of consent, both from vascular causes: an extensive ischemic stroke and a massive MI. The former patient died before blood collection for RAGE genotyping.
Risk factors associated with cardiovascular events in rheumatoid arthritis
Cox regression was used to examine the association between CV events after onset of RA and CV risk factors, RA features and RAGE genotype (Table 2). Predictor variables were tested, considering the covariates as time-dependent during the period from onset of RA until the time of evaluation. A history of statin use for hyperlipidemia, a short disease duration and an average prednisone dose greater than 10 mg/day, but neither RAGE nor HLA genotype, were statistically significantly associated with CV events after RA diagnosis. Significant risk factors were further evaluated in multivariate Cox regression models (Table 3). All covariates were considered time-dependent. Significant associations persisted for disease duration and history of statin use but not prednisone dose.
Receptor for advanced glycation end products Gly82→Ser polymorphism and rheumatoid arthritis
At least one RAGE gene with the Ser82 allele was present in 20% of RA patients in the present cohort. Only one patient was homozygous for the RAGE Ser82 isoform, thus it was not possible to evaluate a gene-dose effect. To further evaluate the association between the RAGE Ser82 allele and CV events, risk factors and RA characteristics, correlates of RAGE status were sought in a logistic regression model. The only correlate was the HLA–DRB1*0401 allele. Indeed, 87% of patients with the RAGE Ser82 isoform, but only 29% of patients with the RAGE Gly82 isoform, carried the HLA–DRB1*0401 allele on at least one chromosome (p < 0.0001). The patient homozygous for the RAGE Ser82 isoform was also homozygous for HLA–DRB1*0401. Carriage of any of the 'shared epitope' DRB1 alleles associated with RA susceptibility [20] was also associated with the RAGE Ser82 isoform, although less strongly. In combination, these data confirm that the RAGE Ser82 isoform and DRB1*0401 are in linkage disequilibrium in RA.
Discussion
CV disease is a frequent and serious accompaniment for RA. We show here that in our population diagnosed with RA the risk of CV events was associated with history of statin therapy for hyperlipidemia and shorter RA disease duration, suggesting that the risk of vascular events is greatest in early disease. Association of CV events with shorter disease duration is consistent with several previous studies. Goodson and colleagues recently demonstrated 10% mortality, predominantly owing to CV events, within 10 years of onset of inflammatory polyarthritis [27]. In a large study of CV mortality in RA spanning 40 years of follow-up, disease duration was found to have no influence, suggesting that the increased risk of CV death was already present at RA diagnosis. Our data also demonstrate that the RAGE Ser82 allele, which is present in one-fifth of patients, does not contribute to the risk of CV events in patients with RA.
Laboratory, clinical and epidemiologic evidence indicates that immune dysregulation, in addition to ongoing systemic inflammation, is crucial to the excess atherogenesis and CV mortality in RA compared with age-matched individuals without RA [28–30]. Thus, baseline or average ESR or CRP levels over the course of RA have been shown to predict subsequent CV death [9, 10]. However, inflammatory disease and its treatment, in turn, might affect either the prevalence or the contribution of traditional CV risk factors. Thus, cholesterol and inflammation tend to be inversely associated, owing to a disproportionate reduction of HDL and an adverse lipid profile [31, 32]. Statins are known to be anti-inflammatory and have been shown to both improve vascular function in RA patients with a normal lipid profile and have additional immunomodulatory and RA disease-modifying benefits, including reduction of CRP levels, serum TNF concentrations and indices of plasma viscosity, in addition to short-term improvements in endothelial function and arterial stiffness [33–37]. Of clinical importance, this is the first study to show that statins significantly influence the outcome of atherosclerosis in RA. Although no direct indicator of inflammatory disease, such as CRP, persisted in the multivariate model, our study was limited in its ability to discern the influence of inflammation on CV events because we examined only RA patients and not matched non-RA controls and inflammatory markers and radiographs were examined at only a single time point, which occurred at variable times after commencing a variety of antirheumatic drugs rather than at baseline.
In RA, proinflammatory ligands of the RAGE, including S100A12 and HMGB1, are reported to be expressed at high levels, levels of soluble RAGE are reduced and RAGE expression is increased by synovial macrophages [17, 38, 39]. At least one RAGE allele was present as Ser82 in 10% to 20% of RA patients in the present prospective and retrospective cohorts, figures similar to previous studies of RA patients and higher than those in unselected population-based studies or control cohorts [18, 19, 21, 40]. We confirm here that the RAGE Ser82 allele is in linkage disequilibrium with HLA–DRB1*0401 [40–42]. Because the RAGE Ser82 isoform is a functional polymorphism enhancing receptor signaling through MAP kinases and NF-κB, which activate an array of proinflammatory genes [18], we predicted an association of this polymorphism with CV events in RA, potentially through a more pronounced inflammatory response in these patients. However, the RAGE Ser82 isoform was not associated with more severe disease by any criteria in this RA cohort. Furthermore, no study has shown an independent association of the RAGE Ser82 isoform and RA. Thus, although certain RAGE ligands are highly expressed in RA and might contribute to the inflammatory process, the influence of the gain-of-function RAGE Ser82 isoform on RA expression is still unclear. Nevertheless, for similar reasons to those outlined above, the relationship between the RAGE Ser82 isoform and both inflammation and damage outcome in RA must be formally tested prospectively in RA inception cohorts.
Furthermore, in the current study of RA patients, the RAGE Ser82 isoform was not associated with CV events. This result supports the observation that the RAGE Ser82 isoform was not associated with CV disease in the general population [21], suggesting that the simple hypothesis that enhanced inflammatory signaling, mediated through the RAGE Ser82 isoform, predisposes to CV events is unlikely.
Conclusion
A Ser82 polymorphic allele of RAGE associated with enhanced RAGE signaling is present in 20% of patients with RA in linkage disequilibrium with HLA–DRB1*0401. In a cohort of established RA patients attending a tertiary referral center, a history of statin use and shorter duration of RA, but not RAGE genotype, were significantly associated with CV events. Prospective trials to determine the role of statins on CV outcome in RA patients will be of great interest.
Abbreviations
- ACR:
-
= American College of Rheumatology
- AGE:
-
= advanced glycation end product
- BMI:
-
= body-mass index
- CCP:
-
= cyclic citrullinated peptide
- CrCl:
-
= creatinine clearance
- CRP:
-
= C-reactive protein
- CT:
-
= computed tomography
- CV:
-
= cardiovascular
- ECG:
-
= electrocardiogram
- ESR:
-
= erythrocyte sedimentation rate
- HDL:
-
= high-density lipoprotein
- HMGB1:
-
= high-mobility group box chromosomal protein
- HR:
-
= hazard ratio
- LDL:
-
= low-density lipoprotein
- MAP:
-
= mitogen activated protein
- MHC:
-
= major histocompatability
- MI:
-
= myocardial infarction
- NF-κB:
-
= nuclear factor of kappa B
- PCR:
-
= polymerase chain reaction
- PVD:
-
= peripheral vascular disease
- RA:
-
= rheumatoid arthritis
- RF:
-
= rheumatoid factor
- RAGE:
-
= receptor for advanced glycation end products
- SCr:
-
= serum creatinine
- TG:
-
= triglyceride
- TIA:
-
= transient ischemic attack
- TNF:
-
= tumor necrosis factor
- VLDL:
-
= very-low-density lipoprotein.
References
Goodson NJ, Wiles NJ, Lunt M, Barrett EM, Silman AJ, Symmons DP: Mortality in early inflammatory polyarthritis: cardiovascular mortality is increased in seropositive patients. Arthritis Rheum. 2002, 46: 2010-2019. 10.1002/art.10419.
Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A: The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994, 331: 417-424. 10.1056/NEJM199408183310701.
Doherty NE, Siegel RJ: Cardiovascular manifestations of systemic lupus erythematosus. Am Heart J. 1985, 110: 1257-1265. 10.1016/0002-8703(85)90023-7.
Srinivas M, Basumani P, Muthusamy R, Wheeldon N: Active inflammatory bowel disease and coronary artery dissection. Postgrad Med J. 2005, 81: 68-70. 10.1136/pgmj.2004.018952.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, et al: Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004, 364: 937-952. 10.1016/S0140-6736(04)17018-9.
Dessein PH, Stanwix AE, Joffe BI: Cardiovascular risk in rheumatoid arthritis versus osteoarthritis: acute phase response related decreased insulin sensitivity and high-density lipoprotein cholesterol as well as clustering of metabolic syndrome features in rheumatoid arthritis. Arthritis Res. 2002, 4: R5-10.1186/ar428.
Hak AE, Stehouwer CD, Bots ML, Polderman KH, Schalkwijk CG, Westendorp IC, Hofman A, Witteman JC: Associations of C-reactive protein with measures of obesity, insulin resistance, and subclinical atherosclerosis in healthy, middle-aged women. Arterioscler Thromb Vasc Biol. 1999, 19: 1986-1991.
Das I: Raised C-reactive protein levels in serum from smokers. Clin Chim Acta. 1985, 153: 9-13. 10.1016/0009-8981(85)90133-0.
Goodson NJ, Symmons DP, Scott DG, Bunn D, Lunt M, Silman AJ: Baseline levels of C-reactive protein and prediction of death from cardiovascular disease in patients with inflammatory polyarthritis: a ten-year followup study of a primary care-based inception cohort. Arthritis Rheum. 2005, 52: 2293-2299. 10.1002/art.21204.
Maradit-Kremers H, Nicola PJ, Crowson CS, Ballman KV, Gabriel SE: Cardiovascular death in rheumatoid arthritis: a population-based study. Arthritis Rheum. 2005, 52: 722-732. 10.1002/art.20878.
Sugaya K, Fukagawa T, Matsumoto K, Mita K, Takahashi E, Ando A, Inoko H, Ikemura T: Three genes in the human MHC class III region near the junction with the class II: gene for receptor of advanced glycosylation end products, PBX2 homeobox gene and a notch homolog, human counterpart of mouse mammary tumor gene int-3. Genomics. 1994, 23: 408-419. 10.1006/geno.1994.1517.
Basta G, Lazzerini G, Massaro M, Simoncini T, Tanganelli P, Fu C, Kislinger T, Stern DM, Schmidt AM, De Caterina R: Advanced glycation end products activate endothelium through signal-transduction receptor RAGE: a mechanism for amplification of inflammatory responses. Circulation. 2002, 105: 816-822. 10.1161/hc0702.104183.
Sakaguchi T, Yan SF, Yan SD, Belov D, Rong LL, Sousa M, Andrassy M, Marso SP, Duda S, Arnold B, et al: Central role of RAGE-dependent neointimal expansion in arterial restenosis. J Clin Invest. 2003, 111: 959-972. 10.1172/JCI200317115.
Sunahori K, Yamamura M, Yamana J, Takasugi K, Kawashima M, Makino H: Increased expression of receptor for advanced glycation end products by synovial tissue macrophages in rheumatoid arthritis. Arthritis Rheum. 2006, 54: 97-104. 10.1002/art.21524.
Hofmann MA, Drury S, Fu C, Qu W, Taguchi A, Lu Y, Avila C, Kambham N, Bierhaus A, Nawroth P, et al: RAGE mediates a novel proinflammatory axis: a central cell surface receptor for S100/calgranulin polypeptides. Cell. 1999, 97: 889-901. 10.1016/S0092-8674(00)80801-6.
Yan SD, Schmidt AM, Anderson GM, Zhang J, Brett J, Zou YS, Pinsky D, Stern D: Enhanced cellular oxidant stress by the interaction of advanced glycation end products with their receptors/binding proteins. J Biol Chem. 1994, 269: 9889-9897.
Taniguchi N, Kawahara K, Yone K, Hashiguchi T, Yamakuchi M, Goto M, Inoue K, Yamada S, Ijiri K, Matsunaga S, et al: High mobility group box chromosomal protein 1 plays a role in the pathogenesis of rheumatoid arthritis as a novel cytokine. Arthritis Rheum. 2003, 48: 971-981. 10.1002/art.10859.
Hofmann MA, Drury S, Hudson BI, Gleason MR, Qu W, Lu Y, Lalla E, Chitnis S, Monteiro J, Stickland MH, et al: RAGE and arthritis: the G82S polymorphism amplifies the inflammatory response. Genes Immun. 2002, 3: 123-135. 10.1038/sj.gene.6363861.
Hudson BI, Stickland MH, Grant PJ: Identification of polymorphisms in the receptor for advanced glycation end products (RAGE) gene: prevalence in type 2 diabetes and ethnic groups. Diabetes. 1998, 47: 1155-1157. 10.2337/diabetes.47.7.1155.
Gregersen PK, Silver J, Winchester RJ: The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheum. 1987, 30: 1205-1213. 10.1002/art.1780301102.
Hofmann MA, Yang Q, Harja E, Kedia P, Gregersen PK, Cupples LA, Schmidt AM, Hudson BI: The RAGE Gly82Ser polymorphism is not associated with cardiovascular disease in the Framingham offspring study. Atherosclerosis. 2005, 182: 301-305. 10.1016/j.atherosclerosis.2005.02.006.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS, et al: The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988, 31: 315-324. 10.1002/art.1780310302.
Alpert JS, Thygesen K, Antman E, Bassand JP: Myocardial infarction redefined – a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000, 36: 959-969. 10.1016/S0735-1097(00)00804-4.
Anderson KM, Odell PM, Wilson PW, Kannel WB: Cardiovascular disease risk profiles. Am Heart J. 1991, 121: 293-298. 10.1016/0002-8703(91)90861-B.
Cockcroft DW, Gault MH: Prediction of creatinine clearance from serum creatinine. Nephron. 1976, 16: 31-41.
van der Heijde D: How to read radiographs according to the Sharp/van der Heijde method. J Rheumatol. 2000, 27: 261-263.
Goodson N, Marks J, Lunt M, Symmons D: Cardiovascular admissions and mortality in an inception cohort of patients with rheumatoid arthritis with an onset in the 1980's and 1990's. Ann Rheum Dis. 2005, 64: 1595-1601. 10.1136/ard.2004.034777.
Wang L, Feng G: Rheumatoid arthritis increases the risk of coronary heart disease via vascular endothelial injuries. Med Hypotheses. 2004, 63: 442-445. 10.1016/j.mehy.2003.11.040.
del Rincon ID, Williams K, Stern MP, Freeman GL, Escalante A: High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001, 44: 2737-2745. 10.1002/1529-0131(200112)44:12<2737::AID-ART460>3.0.CO;2-#.
Solomon DH, Curhan GC, Rimm EB, Cannuscio CC, Karlson EW: Cardiovascular risk factors in women with and without rheumatoid arthritis. Arthritis Rheum. 2004, 50: 3444-3449. 10.1002/art.20636.
Situnayake RD, Kitas G: Dyslipidemia and rheumatoid arthritis. Ann Rheum Dis. 1997, 56: 341-342.
Park YB, Lee SK, Lee WK, Suh CH, Lee CW, Lee CH, Song CH, Lee J: Lipid profiles in untreated patients with rheumatoid arthritis. J Rheumatol. 1999, 26: 1701-1704.
Hermann F, Forster A, Chenevard R, Enseleit F, Hurlimann D, Corti R, Spieker LE, Frey D, Hermann M, Riesen W, et al: Simvastatin improves endothelial function in patients with rheumatoid arthritis. J Am Coll Cardiol. 2005, 45: 461-464. 10.1016/j.jacc.2004.11.006.
Tikiz C, Utuk O, Pirildar T, Bayturan O, Bayindir P, Taneli F, Tikiz H, Tuzun C: Effects of Angiotensin-converting enzyme inhibition and statin treatment on inflammatory markers and endothelial functions in patients with longterm rheumatoid arthritis. J Rheumatol. 2005, 32: 2095-2101.
McCarey DW, McInnes IB, Madhok R, Hampson R, Scherbakov O, Ford I, Capell HA, Sattar N: Trial of Atorvastatin in Rheumatoid Arthritis (TARA): double-blind, randomised placebo-controlled trial. Lancet. 2004, 363: 2015-2021. 10.1016/S0140-6736(04)16449-0.
McCarey DW, Sattar N, McInnes IB: Do the pleiotropic effects of statins in the vasculature predict a role in inflammatory diseases?. Arthritis Res Ther. 2005, 7: 55-61. 10.1186/ar1496.
Van Doornum S, McColl G, Wicks IP: Atorvastatin reduces arterial stiffness in patients with rheumatoid arthritis. Ann Rheum Dis. 2004, 63: 1571-1575. 10.1136/ard.2003.018333.
Pullerits R, Bokarewa M, Dahlberg L, Tarkowski A: Decreased levels of soluble receptor for advanced glycation end products in patients with rheumatoid arthritis indicating deficient inflammatory control. Arthritis Res Ther. 2005, 7: R817-R824. 10.1186/ar1749.
Foell D, Kane D, Bresnihan B, Vogl T, Nacken W, Sorg C, Fitzgerald O, Roth J: Expression of the pro-inflammatory protein S100A12 (EN-RAGE) in rheumatoid and psoriatic arthritis. Rheumatology (Oxford). 2003, 42: 1383-1389. 10.1093/rheumatology/keg385.
Steenvoorden MM, van der Helm-van Mil AH, Stoeken G, Bank RA, Devries RR, Huizinga TW, Degroot J, Toes RE: The RAGE G82S polymorphism is not associated with rheumatoid arthritis independently of HLA-DRB1*0401. Rheumatology (Oxford). 2006, 45: 488-490. 10.1093/rheumatology/kel011.
Prevost G, Fajardy I, Fontaine P, Danze PM, Besmond C: Human RAGE GLY82SER dimorphism and HLA class II DRB1-DQA1-DQB1 haplotypes in type 1 diabetes. Eur J Immunogenet. 1999, 26: 343-348. 10.1046/j.1365-2370.1999.00168.x.
de Vries N, Tijssen H, van Riel PL, van de Putte LB: Reshaping the shared epitope hypothesis: HLA-associated risk for rheumatoid arthritis is encoded by amino acid substitutions at positions 67–74 of the HLA-DRB1 molecule. Arthritis Rheum. 2002, 46: 921-928. 10.1002/art.10210.
Acknowledgements
Supported by grants from the Australian Rotary Health Fund, Princess Alexandra Hospital Foundation (Brisbane, Australia) and National Health and Medical Research Council of Australia. RT is supported by Arthritis Queensland (Australia). These funding bodies were independent of the data collection and preparation for publication. We thank Chris Downey, Phillip Vecchio and Martin Devereaux for clinical support during data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LC, IF, MT, TM and RT were involved in conception, design, acquisition, analysis and interpretation of data. LC, IF, TM and RT drafted and revised the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Carroll, L., Frazer, I.H., Turner, M. et al. Receptor for advanced glycation end products Glycine 82 Serine polymorphism and risk of cardiovascular events in rheumatoid arthritis . Arthritis Res Ther 9, R39 (2007). https://doi.org/10.1186/ar2175
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar2175