Abstract
Background
The design of clinical immunology studies in sepsis presents several fundamental challenges to improving the translational understanding of pathologic mechanisms. We undertook a systematic review of bed-to-benchside studies to test the hypothesis that variable clinical design methodologies used to investigate immunologic function in sepsis contribute to apparently conflicting laboratory data, and identify potential alternatives that overcome various obstacles to improve experimental design.
Methods
We performed a systematic review of the design methodology employed to study neutrophil function (respiratory burst), monocyte endotoxin tolerance and lymphocyte apoptosis in the intensive care setting, over the past 15 years. We specifically focussed on how control samples were defined, taking into account age, gender, ethnicity, concomitant therapies, timing of sample collection and the criteria used to diagnose sepsis.
Results
We identified 57 eligible studies, the majority of which (74%) used case–control methodology. Healthy volunteers represented the control population selected in 83% of studies. Comprehensive demographic data on age, gender and ethnicity were provided in ≤48% of case control studies. Documentation of diseases associated with immunosuppression, malignancy and immunomodulatory therapies was rare. Less than half (44%) of studies undertook independent adjudication for the diagnosis of sepsis while 68% provided microbiological data. The timing of sample collection was defined by highly variable clinical criteria. By contrast, surgical studies avoided many such confounders, although only one study in surgical patients monitored the study group for development of sepsis.
Conclusions
We found several important and common limitations in the clinical design of translational immunologic studies in human sepsis. Major elective surgery overcame many of these methodological limitations. The failure of adequate clinical design in mechanistic studies may contribute to the lack of translational therapeutic progress in intensive care medicine.
Similar content being viewed by others
Background
Mortality from sepsis is persistently high, and may even be rising despite decades of research [1, 2]. Promising pre-clinical immunomodulatory therapies have failed in clinical practice [3–5] perhaps attributable, in part, to differences between human and rodent immunology [6]. However, an alternative explanation is that the heterogeneous etiology, presentation and progression of human sepsis generate confounding factors that distort the interpretation of clinical immunologic studies. Thus, the identification of appropriate controls, diagnostic accuracy, demographic influences and therapies with immunomodulatory off-target effects are critical considerations in interpreting translational work.
We therefore systematically reviewed the clinical experimental design of studies in three key areas of bed-to-benchside immunologic research in sepsis, focusing in particular on comparator groups and the documentation of known confounding factors. We also explored how the investigation of immune mechanisms in other clinical scenarios - trauma and major elective surgery - associated with the development of sepsis may help refine experimental design.
Methods
A Pubmed search was performed for the terms‘Neutrophil respiratory burst’ OR‘Monocyte endotoxin tolerance’ OR‘Lymphocyte apoptosis’ AND‘Sepsis’ OR‘Trauma’ OR‘Surgery’, restricted to adult human studies published between 03 January 1998 and 03 January 2013. The abstract of each paper was manually assessed for suitability. In vitro studies of healthy volunteer cells were excluded.
Clinical demographics
For all eligible manuscripts, we recorded the primary author, year of publication and clinical setting. The number, age, gender, clinical severity score of subjects and their corresponding controls, in whom the same assay of immune function was performed, were compared. The criteria used to define sepsis - complete with evidence for microbiological confirmation and independent adjudication of the sepsis diagnosis - were also recorded. Since immune cell effector function may change over the course of sepsis, we also recorded details of the timing of initial and subsequent blood samples, and the reason for blood sampling itself. Given that a recent report detected differences in genomic markers of inflammation that associate with survival within the first 24 h of intensive care admission [7], we assessed whether samples were obtained within, or beyond, this 24-h window. Since several commonly used therapies used in intensive care medicine exhibit immune modulating effects, we also recorded whether common immunomodulatory agents including antibiotics [8], glucocorticoids [9] and sedative agents [10] were documented. Reporting of pre-existing immunosuppressive or malignant disease - or their specific exclusion - was also recorded.
Study aims
The specific aims of each study were recorded with regard to the experimental context and primary conclusion. The context within which each of the three functional assays was studied was classified as: Pathophysiological - observational mechanistic studies detailing evolution of the assay response in clinical samples; Experimental - use of patient samples for more detailed experimental investigations beyond the assay itself; Clinical outcome - correlation of outcome measure with assay response; Biomarker comparison - correlation of alternative assay with functional assay.
Laboratory samples
We recorded whether an a priori power analysis had been performed to determine the number of subjects/controls needed to refute the primary hypothesis. Sample timing and key aspects of experimental technique were compared between sepsis and control subjects. Associations made between immune cell function and clinical outcome were noted.
Statistics
Data are presented as mean ± SD, or median (interquartile range). Age data in primary studies was used to construct 95% confidence intervals in order to assess whether differences existed between control and study populations (NCSS 8, Kaysville, UT, USA).
Results
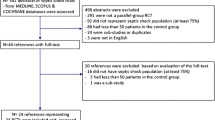
Fifty-seven eligible studies were identified, as summarised in Figure 1. Data is displayed into 3 tables for each immune assay, titled "Principal features of studies" (Tables 1, 2 and 3), "Demographic information" (Tables 4, 5 and 6) and "Experimental conduct and exclusion criteria" (Tables 7, 8 and 9).
Source of experimental control subjects
No studies reported a priori power analyses based on either preceding laboratory data or ex vivo clinical research. The majority of studies (42/57; 74%) used case–control methodology. Control samples were obtained from healthy volunteers in (35/42; 83%), with the remainder using a variety of loosely defined clinical phenotypes (Figure 2, Tables 1, 2 and 3). The exception was elective surgical patients, where preoperative samples served as appropriate controls. Cohort methodology, where samples including controls were obtained serially from the same patient, was employed in 14/57 (25%) of studies. The majority of cohort studies were conducted in elective surgical patients (12/14; 86%).
Age, gender and ethnicity
Advanced age is associated with progressively impaired innate and adaptive immunity [67]. Less than half of case control studies (20/42; 48%) reported the age distribution of both study and control populations. In studies where age was reported, the critically ill patients studied were often older than the control population. Female gender is associated with improved clinical outcomes following sepsis [68, 69] and increased longevity compared to males in general. Information on gender was provided in (26/42; 62%) of case–control studies. Significant variation in the incidence of sepsis has been reported according to ethnicity [70], which may reflect residual confounding or plausible biologic differences in susceptibility. However, only one study reported the ethnicity of patients.
Co-morbidity
Various comorbidities ranging from cardiac failure to active malignancy are associated with important deleterious alteration in effective immune function, independent of those described in sepsis [71, 72]. The majority of studies (34/57; 60%) excluded patients with overt immunosuppression while a minority (8/57; 14%) excluded those with malignancy (Figure 3).
Clinical definition of sepsis
A high proportion of studies (26/33; 79%) defined sepsis in accordance with the ACCP/SCCM [73, 74] or Surviving Sepsis Campaign (2008 update) [75] criteria. Of those studies which used standard consensus conference criteria, (15/26, 58%) included patients with‘sepsis’, (20/26; 77%) included those with‘severe sepsis’ and (24/26, 92%) included those with‘septic shock’. In a large minority of these 26 studies (11/26; 42%), sub-categories defining sepsis were not compared separately, but combined. Immunologic studies in trauma and surgical patient samples usually did not document (18/24; 75%) whether patients developed an infection during the course of the study. In these studies, the majority (5/6) used established consensus conference criteria.
Microbiological definitions of sepsis
Independent adjudication of the definition of sepsis used in studies was undertaken in 17/57 (30%) of studies. Since recent basic laboratory studies have demonstrated that the clinical signs/symptoms of sepsis are frequently mimicked by non-pathogenic molecules [76, 77], we sought to establish whether microbial evidence for sepsis was presented. Microbiological data were provided in 25/57 (44%).
Severity of critical illness
A minority of studies (19/57; 33%) provided data on organ dysfunction related to sepsis severity, such as APACHE-II or SAPS II. When a severity index was used, a wide range was reported within individual studies suggesting substantial heterogeneity. In studies where mortality was reported (4/57; 7%), severity of critical illness was not reported in those patients who survived.
Timing of experimental samples
The timing of the index blood sample obtained from septic patients was described in the majority (26/33; 79%) of cases. However, the criteria for initial sampling were not comparable between studies and was most frequently defined by the severity of sepsis (Figure 4). These triggers included hospital admission (1/26), ICU admission (5/26), proof of infection (2/26), diagnosis of sepsis (5/26), onset of sepsis (14/26; 54%), onset of organ failure (3/24) and onset of septic shock (7/26) - the remaining two samples were from autopsy studies. Multiple criteria for sampling were often used and dependent upon the severity of patient illness. Approximately half of all studies (14/26; 58%) obtained an initial sample within 24 h of hospital admission. Similar patterns of sample timing were described for trauma patients. Repeat samples were often undertaken, but over highly variable intervals that were frequently not defined a priori. By contrast, all 12 studies undertaken in the elective surgical setting obtained preoperative control samples, with subsequent samples taken on predefined postoperative days.
Therapies as potential confounders
Commonly administered therapies in intensive care impact directly on immune function [8–10]. We assessed reporting of three of the commonest therapies with established immunomodulatory properties and found that only up to a quarter of studies documented their use (Figure 5). Specifically, these were sedative agents (4/57; 7%), antibiotics (6/57; 11%) and steroids (15/57; 26%).
Experimental conduct and outcomes
There was no apparent relationship between the experimental context of studies and the control groups that were explored (Tables 1, 2 and 3). There are, however, clear associations between the study population studied and experimental outcome (Tables 1, 7, 2, 8, 3 and 9). For example, within the respiratory burst data, there is a consistent increase in respiratory burst identified by sepsis studies. However, since none of these studies used pre-illness samples, it is unclear if the change is a feature of sepsis, or the study population in relation to healthy volunteers. The conflicting results reported by the three surgical studies are difficult to interpret since each study uses a different burst assay, and the magnitude/type of operation varies. Similar patterns are also evident across the monocyte and lymphocyte studies.
Discussion
This systematic review has revealed several important issues in the design and reporting of immunologic phenotype in intensive care/sepsis studies. The studies we selected are representative of the current literature, covering the past 15 years of work in three key areas of sepsis research. Following a preliminary Pubmed search, these three assays were chosen because they represent the most frequently investigation for each immune cell type. These limitations refer to the clinical aspects of the study methodology rather than specific laboratory techniques that we did not assess. These data suggest that the use of surgical patients to model critical illness may overcome several key limitations.
Defining what constitutes an adequate control sample for the immunologic study of sepsis is clearly highly challenging. Case–control studies are frequently used in sepsis research. Our review suggests that case-control studies cannot easily determine whether the observed differences in the experimental readout between the study and control groups is due to sepsis per se, or other differences between the groups including age, comorbidities and treatment interventions. Whereas cohort studies do allow pre-sepsis samples to be taken, the majority of studies are conducted in healthy volunteers free of important comorbidities (e.g. heart failure, cirrhosis) that influence both the development of, and survival from, sepsis [71]. Furthermore, age-, gender- and ethnicity-related differences in immune function are well documented [67–70], yet our data demonstrates that several key demographic details for study and control populations were frequently not reported. Finally, the presence of malignant disease - associated with immunosuppression [72] and disproportionately represented in the ICU population of most healthcare systems - was only documented in a minority of studies.
Sepsis is currently defined using clinical constructs that define syndromes, rather than use biologic and/or molecular criteria. It remains unclear whether there are biologically relevant differences between clinically defined subtypes of sepsis. In other words, changes in immunophenotype associated with progression of sepsis to severe sepsis/septic shock may merely reflect the consequences of clinical interventions and/or indirect effects on organ function that partly reflect pre-existing comorbidities. Furthermore, the specific detection of pathogens, or pathogen-associated molecular patterns, is likely to further impact on the robustness of immunophenotyping since the location and type of micro-organism both regulate host-immune responses [77, 78]. We identified only one study that specified infection site and/or a specific pathogen [34].
Critically ill patients are exposed to a range of therapeutic agents that have well-described immunologic effects. Although immunomodulation by the majority of these agents has been established in vitro, their role in confounding the septic immunophenotype remains unclear. Nevertheless, a myriad of off-target, immune effects have been established in pre-clinical in vivo models. Many antibiotics target mitochondria and eukaryotic protein synthesis [79]. Steroids exert potent pro- and anti-inflammatory properties - including inducing lymphocyte apoptosis [9]. Similarly, sedatives and analgesics exert profound effects on immune cell function [80, 81].
Our data suggest that surgical patients offer important potential advantages for mechanistic studies of sepsis. The incidence of sepsis - as defined by conventional clinical criteria - varies from 6.98% to 12.25%, depending upon the health care system and database interrogated [82]. No other patient population allows the collection of highly phenotyped data and individualised control samples prior to a defined traumatic insult. Since the volume of surgery is huge and large scale outcome data can be collected, potential limitations including comorbidities and concomitant therapies can be controlled for.
Conclusions
We found several important limitations in clinical design associated with translational immunologic studies of human sepsis. Clinical design in mechanistic studies exploring changes in immunophenotype may contribute to the lack of translational therapeutic progress in intensive care medicine. Major elective surgery offers a potential model to overcome many of these methodological limitations.
Take-home message
Systematic review suggests a critical re-evaluation in design of immunologic phenotyping studies conducted in intensive care.
Tweet
Immunological investigation of septic patients presents methodological challenges that are not considered by many recent studies.
Abbreviations
- ACCP/SCCM:
-
American College of Chest Physicians/Society of Critical Care Medicine
- APACHE II:
-
Acute Physiology and Chronic Health Evaluation [83]
- APACHE III:
-
Acute Physiology and Chronic Health Evaluation [84]
- ASA:
-
American Society of Anesthesiologists [85]
- BC:
-
Blood culture
- CDC NNIS:
-
Centre for Disease Control National Nosocomial Infections Surveillance [86]
- ICU:
-
Intensive Care Unit
- ISS:
-
Injury Severity Score [87]
- MODS:
-
Multi Organ Dysfunction Score
- N/A:
-
not applicable
- N/S:
-
not summarised
- SAPS II:
-
Simplified Acute Physiology Score
- SSC:
-
Surviving Sepsis Campaign
- SIRS:
-
Systemic Inflammatory Response Syndrome.
References
Harrison DA, Welch CA, Eddleston JM: The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Crit Care 2006, 10: R42.
Dombrovskiy VY, Martin AA, Sunderram J, Paz HL: Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med 2007, 35: 1244–1250.
Ranieri VM, Thompson BT, Barie PS, Dhainaut J-F, Douglas IS, Finfer S, Gårdlund B, Marshall JC, Rhodes A, Artigas A, Payen D, Tenhunen J, Al-Khalidi HR, Thompson V, Janes J, Macias WL, Vangerow B, Williams MD: Drotrecogin Alfa (activated) in adults with septic shock. N Engl J Med 2012, 366: 2055–2064.
Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, Weiss YG, Benbenishty J, Kalenka A, Forst H, Laterre P-F, Reinhart K, Cuthbertson BH, Payen D, Briegel J: Hydrocortisone therapy for patients with septic shock. N Engl J Med 2008, 358: 111–124.
Finfer S, Chittock DR, Su SY-S, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hébert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ: Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009, 360: 1283–1297.
Mestas J, Hughes CCW: Of mice and not men: differences between mouse and human immunology. J Immunol 2004, 172: 2731–2738.
Xiao W, Mindrinos MN, Seok J, Cuschieri J, Cuenca AG, Gao H, Hayden DL, Hennessy L, Moore EE, Minei JP, Bankey PE, Johnson JL, Sperry J, Nathens AB, Billiar TR, West MA, Brownstein BH, Mason PH, Baker HV, Finnerty CC, Jeschke MG, López MC, Klein MB, Gamelli RL, Gibran NS, Arnoldo B, Xu W, Zhang Y, Calvano SE, McDonald-Smith GP, et al.: A genomic storm in critically injured humans. J Exp Med 2011, 208: 2581–2590.
Kanoh S, Rubin BK: Mechanisms of action and clinical application of macrolides as immunomodulatory medications. Clin Microbiol Rev 2010, 23: 590–615.
Clarke AR, Purdie CA, Harrison DJ, Morris RG, Bird CC, Hooper ML, Wyllie AH: Thymocyte apoptosis induced by p53-dependent and independent pathways. Nature 1993, 362: 849–852.
Mikawa K, Akamatsu H, Maekawa N, Nishina K, Niwa Y: Propofol inhibits human neutrophil functions. Anesth Analg 1998, 87: 695–700.
White M, Mahon V, Grealy R, Doherty DG, Stordeur P, Kelleher DP, McManus R, Ryan T: Post-operative infection and sepsis in humans is associated with deficient gene expression of γc cytokines and their apoptosis mediators. Crit Care 2011, 15: R158.
Santos SS, Brunialti MKC, Rigato O, Machado FR, Silva E, Salomao R: Generation of nitric oxide and reactive oxygen species by neutrophils and monocytes from septic patients and association with outcomes. Shock 2012, 38: 18–23.
Bruns T, Peter J, Hagel S, Herrmann A, Stallmach A: The augmented neutrophil respiratory burst in response to Escherichia coli is reduced in liver cirrhosis during infection. Clin Exp Immunol 2011, 164: 346–356.
Martins PS, Kallas EG, Neto MC, Dalboni MA, Blecher S, Salomão R: Upregulation of reactive oxygen species generation and phagocytosis, and increased apoptosis in human neutrophils during severe sepsis and septic shock. Shock 2003, 20: 208–212.
Barth E, Fischer G, Schneider EM, Moldawer LL, Georgieff M, Weiss M: Peaks of endogenous G-CSF serum concentrations are followed by an increase in respiratory burst activity of granulocytes in patients with septic shock. Cytokine 2002, 17: 275–284.
Mariano F, Tetta C, Guida G, Triolo G, Camussi G: Hemofiltration reduces the serum priming activity on neutrophil chemiluminescence in septic patients. Kidney Int 2001, 60: 1598–1605.
Ahmed NA, McGill S, Yee J, Hu F, Michel RP, Christou NV: Mechanisms for the diminished neutrophil exudation to secondary inflammatory sites in infected patients with a systemic inflammatory response (sepsis). Crit Care Med 1999, 27: 2459–2468.
Pascual C, Bredle D, Karzai W, Meier-Hellmann A, Oberhoffer M, Reinhart K: Effect of plasma and LPS on respiratory burst of neutrophils in septic patients. Intensive Care Med 1998, 24: 1181–1186.
Paunel-Görgülü A, Lögters T, Flohé S, Cinatl J, Altrichter J, Windolf J, Scholz M: Stimulation of Fas signaling down-regulates activity of neutrophils from major trauma patients with SIRS. Immunobiology 2011, 216: 334–342.
Shih H-C, Huang M-S, Lee C-H: Polymorphonuclear cell priming associated with NF-kB activation in patients with severe injury is partially dependent on macrophage migration inhibitory factor. J Am Coll Surg 2010, 211: 791–797.
Kasten KR, Goetzman HS, Reid MR, Rasper AM, Adediran SG, Robinson CT, Cave CM, Solomkin JS, Lentsch AB, Johannigman JA, Caldwell CC: Divergent adaptive and innate immunological responses are observed in humans following blunt trauma. BMC Immunol 2010, 11: 4.
Valente SA, Fallon WF, Alexander TS, Tomas ER, Evancho-Chapman MM, Schmidt SP, Gorski R, Pizov O, DeFine L, Clark AJ: Immunologic function in the elderly after injury–the neutrophil and innate immunity. J Trauma 2009, 67: 968–974.
Quaid G, Cave C, Williams MA, Hennigan RF, Bokoch G, Solomkin JS: Mechanisms of human neutrophil oxidant production after severe injury. Surgery 2001, 130: 669–675. discussion 675–6
Ertel W, Keel M, Buergi U, Hartung T, Imhof HG, Trentz O: Granulocyte colony-stimulating factor inhibits neutrophil apoptosis at the local site after severe head and thoracic injury. J Trauma 1999, 46: 784–792. discussion 792–3
Ogura H, Tanaka H, Koh T, Hashiguchi N, Kuwagata Y, Hosotsubo H, Shimazu T, Sugimoto H: Priming, second-hit priming, and apoptosis in leukocytes from trauma patients. J Trauma 1999, 46: 774–781. discussion 781–3
Kawasaki T, Ogata M, Kawasaki C, Okamoto K, Sata T: Effects of epidural anaesthesia on surgical stress-induced immunosuppression during upper abdominal surgery. Br J Anaesth 2007, 98: 196–203.
Fröhlich D, Trabold B, Rothe G, Hoerauf K, Wittmann S: Inhibition of the neutrophil oxidative response by propofol: preserved in vivo function despite in vitro inhibition. Eur J Anaesthesiol 2006, 23: 948–953.
Wiezer MJ, Meijer C, Sietses C, Prins HA, Cuesta MA, Beelen RH, Meijer S, van Leeuwen PA: Bactericidal/permeability-increasing protein preserves leukocyte functions after major liver resection. Ann Surg 2000, 232: 208–215.
Shih HC, Su CH, Lee CH: Superoxide production of neutrophils after severe injury: impact of subsequent surgery and sepsis. Am J Emerg Med 1999, 17: 15–18.
Liu TF, Yoza BK, El Gazzar M, Vachharajani VT, McCall CE: NAD + -dependent SIRT1 deacetylase participates in epigenetic reprogramming during endotoxin tolerance. J Biol Chem 2011, 286: 9856–9864.
Pachot A, Cazalis M-A, Venet F, Turrel F, Faudot C, Voirin N, Diasparra J, Bourgoin N, Poitevin F, Mougin B, Lepape A, Monneret G: Decreased expression of the fractalkine receptor CX3CR1 on circulating monocytes as new feature of sepsis-induced immunosuppression. J Immunol 2008, 180: 6421–6429.
West MA, Koons A, Crandall M, Skinner R, Worley M, Shapiro MB: Whole blood leukocyte mitogen activated protein kinases activation differentiates intensive care unit patients with systemic inflammatory response syndrome and sepsis. J Trauma 2007, 62: 805–811.
Härter L, Mica L, Stocker R, Trentz O, Keel M: Increased expression of toll-like receptor-2 and -4 on leukocytes from patients with sepsis. Shock 2004, 22: 403–409.
Escoll P, del Fresno C, García L, Vallés G, Lendínez MJ, Arnalich F, López-Collazo E: Rapid up-regulation of IRAK-M expression following a second endotoxin challenge in human monocytes and in monocytes isolated from septic patients. Biochem Biophys Res Commun 2003, 311: 465–472.
Calvano JE, Agnese DM, Um JY, Goshima M, Singhal R, Coyle SM, Reddell MT, Kumar A, Calvano SE, Lowry SF: Modulation of the lipopolysaccharide receptor complex (CD14, TLR4, MD-2) and toll-like receptor 2 in systemic inflammatory response syndrome-positive patients with and without infection: relationship to tolerance. Shock 2003, 20: 415–419.
Sfeir T, Saha DC, Astiz M, Rackow EC: Role of interleukin-10 in monocyte hyporesponsiveness associated with septic shock. Crit Care Med 2001, 29: 129–133.
Heagy W, Hansen C, Nieman K, Cohen M, Richardson C, Rodriguez JL, West MA: Impaired ex vivo lipopolysaccharide-stimulated whole blood tumor necrosis factor production may identify “septic” intensive care unit patients. Shock 2000, 14: 271–276. discussion 276–7
Bergmann M, Gornikiewicz A, Sautner T, Waldmann E, Weber T, Mittlböck M, Roth E, Függer R: Attenuation of catecholamine-induced immunosuppression in whole blood from patients with sepsis. Shock 1999, 12: 421–427.
Heagy W, Nieman K, Hansen C, Cohen M, Danielson D, West MA: Lower levels of whole blood LPS-stimulated cytokine release are associated with poorer clinical outcomes in surgical ICU patients. Surg Infect (Larchmt) 2003, 4: 171–180.
Flohé S, Lendemans S, Schade F-U, Kreuzfelder E, Waydhas C: Influence of surgical intervention in the immune response of severely injured patients. Intensive Care Med 2004, 30: 96–102.
Buttenschoen K, Schneider ME, Utz K, Kornmann M, Beger HG, Carli Buttenschoen D: Effect of major abdominal surgery on endotoxin release and expression of Toll-like receptors 2/4. Langenbecks Arch Surg 2009, 394: 293–302.
Kawasaki T, Ogata M, Kawasaki C, Tomihisa T, Okamoto K, Shigematsu A: Surgical stress induces endotoxin hyporesponsiveness and an early decrease of monocyte mCD14 and HLA-DR expression during surgery. Anesth Analg 2001, 92: 1322–1326.
Roger P-M, Hyvernat H, Ticchioni M, Kumar G, Dellamonica J, Bernardin G: The early phase of human sepsis is characterized by a combination of apoptosis and proliferation of T cells. J Crit Care 2012, 27: 384–393.
Zhang Y, Li J, Lou J, Zhou Y, Bo L, Zhu J, Zhu K, Wan X, Cai Z, Deng X: Upregulation of programmed death-1 on T cells and programmed death ligand-1 on monocytes in septic shock patients. Crit Care 2011, 15: R70.
Guignant C, Lepape A, Huang X, Kherouf H, Denis L, Poitevin F, Malcus C, Chéron A, Allaouchiche B, Gueyffier F, Ayala A, Monneret G, Venet F: Programmed death-1 levels correlate with increased mortality, nosocomial infection and immune dysfunctions in septic shock patients. Crit Care 2011, 15: R99.
Vaki I, Kranidioti H, Karagianni V, Spyridaki A, Kotsaki A, Routsi C, Giamarellos-Bourboulis EJ: An early circulating factor in severe sepsis modulates apoptosis of monocytes and lymphocytes. J Leukoc Biol 2011, 89: 343–349.
Gogos C, Kotsaki A, Pelekanou A, Giannikopoulos G, Vaki I, Maravitsa P, Adamis S, Alexiou Z, Andrianopoulos G, Antonopoulou A, Athanassia S, Baziaka F, Charalambous A, Christodoulou S, Dimopoulou I, Floros I, Giannitsioti E, Gkanas P, Ioakeimidou A, Kanellakopoulou K, Karabela N, Karagianni V, Katsarolis I, Kontopithari G, Kopterides P, Koutelidakis I, Koutoukas P, Kranidioti H, Lignos M, Louis K, et al.: Early alterations of the innate and adaptive immune statuses in sepsis according to the type of underlying infection. Crit Care 2010, 14: R96.
Hoogerwerf JJ, van Zoelen MA, Wiersinga WJ, van’t Veer C, de Vos AF, de Boer A, Schultz MJ, Hooibrink B, de Jonge E, van derPoll T: Gene expression profiling of apoptosis regulators in patients with sepsis. J Innate Immun 2010, 2: 461–468.
Yousef AA, Suliman GA, Mabrouk MM: The value of correlation of serum 20S proteasome concentration and percentage of lymphocytic apoptosis in critically ill patients: a prospective observational study. Crit Care 2010, 14: R215.
Turrel-Davin F, Guignant C, Lepape A, Mougin B, Monneret G, Venet F: Upregulation of the pro-apoptotic genes BID and FAS in septic shock patients. Crit Care 2010, 14: R133.
Pelekanou A, Tsangaris I, Kotsaki A, Karagianni V, Giamarellou H, Armaganidis A, Giamarellos-Bourboulis EJ: Decrease of CD4-lymphocytes and apoptosis of CD14-monocytes are characteristic alterations in sepsis caused by ventilator-associated pneumonia: results from an observational study. Crit Care 2009, 13: R172.
Delogu G, Famularo G, Tellan G, Marandola M, Antonucci A, Signore M, Marcellini S, Moretti S: Lymphocyte apoptosis, caspase activation and inflammatory response in septic shock. Infection 2008, 36: 485–487.
Weber SU, Schewe J, Lehmann LE, Müller S, Book M, Klaschik S, Hoeft A, Stüber F: Induction of Bim and Bid gene expression during accelerated apoptosis in severe sepsis. 12:1–10. Crit Care 2008, 12(5):R128.
Roth G, Moser B, Krenn C, Brunner M, Haisjackl M, Almer G, Gerlitz S, Wolner E, Boltz-Nitulescu G, Ankersmit HJ: Susceptibility to programmed cell death in T-lymphocytes from septic patients: a mechanism for lymphopenia and Th2 predominance. Biochem Biophys Res Commun 2003, 308: 840–846.
Le Tulzo Y, Pangault C, Gacouin A, Guilloux V, Tribut O, Amiot L, Tattevin P, Thomas R, Fauchet R, Drénou B: Early circulating lymphocyte apoptosis in human septic shock is associated with poor outcome. Shock 2002, 18: 487–494.
Hotchkiss RS, Tinsley KW, Swanson PE, Schmieg RE, Hui JJ, Chang KC, Osborne DF, Freeman BD, Cobb JP, Buchman TG, Karl IE: Sepsis-induced apoptosis causes progressive profound depletion of B and CD4+ T lymphocytes in humans. J Immunol 2001, 166: 6952–6963.
Hotchkiss RS, Swanson PE, Freeman BD, Tinsley KW, Cobb JP, Matuschak GM, Buchman TG, Karl IE: Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Crit Care Med 1999, 27: 1230–1251.
Bandyopadhyay G, Bankey PE, Miller-Graziano CL: Trauma patients’ elevated tumor necrosis related apoptosis inducing ligand (TRAIL) contributes to increased T cell apoptosis. Clin Immunol 2012, 145: 44–54.
Pellegrini JD, De AK, Kodys K, Puyana JC, Furse RK, Miller-Graziano C: Relationships between T lymphocyte apoptosis and anergy following trauma. J Surg Res 2000, 88: 200–206.
Hotchkiss RS, Schmieg RE, Swanson PE, Freeman BD, Tinsley KW, Cobb JP, Karl IE, Buchman TG: Rapid onset of intestinal epithelial and lymphocyte apoptotic cell death in patients with trauma and shock. Crit Care Med 2000, 28: 3207–3217.
Papadima A, Boutsikou M, Lagoudianakis EE, Kataki A, Konstadoulakis M, Georgiou L, Katergiannakis V, Manouras A: Lymphocyte apoptosis after major abdominal surgery is not influenced by anesthetic technique: a comparative study of general anesthesia versus combined general and epidural analgesia. J Clin Anesth 2009, 21: 414–421.
Słotwiński R, Olszewski W, Słodkowski M, Lech G, Zaleska M, Kędziora S, Włuka A, Domaszewska A, Słotwińska S, Krasnodębski W, Wójcik Z: Apoptosis in lymphocytes of pancreatic cancer patients: influence of preoperative enteral immunonutrition and extensive surgery. Arch Immunol Ther Exp (Warsz) 2011, 59: 385–397.
Delogu G, Famularo G, Moretti S, De Luca A, Tellan G, Antonucci A, Marandola M, Signore L: Interleukin-10 and apoptotic death of circulating lymphocytes in surgical/anesthesia trauma. J Trauma 2001, 51: 92–97.
Delogu G, Moretti S, Antonucci A, Marcellini S, Masciangelo R, Famularo G, Signore L, De Simone C: Apoptosis and surgical trauma: dysregulated expression of death and survival factors on peripheral lymphocytes. Arch Surg 2000, 135: 1141–1147.
Sasajima K, Inokuchi K, Onda M, Miyashita M, Okawa KI, Matsutani T, Takubo K: Detection of T cell apoptosis after major operations. Eur J Surg 1999, 165: 1020–1023.
Sugimoto M, Shimaoka M, Hosotsubo K, Tanigami H, Taenaka N, Kiyono H, Yoshiya I: Up-regulation of Fas ligand (FasL) mRNA expression in peripheral blood mononuclear cells (PBMC) after major surgery. Clin Exp Immunol 1998, 112: 120–125.
Montecino-Rodriguez E, Berent-Maoz B, Dorshkind K: Causes, consequences, and reversal of immune system aging. J Clin Invest 2013, 123: 958–965.
Frink M, Pape H-C, van Griensven M, Krettek C, Chaudry IH, Hildebrand F: Influence of sex and age on mods and cytokines after multiple injuries. Shock 2007, 27: 151–156.
Sakr Y, Elia C, Mascia L, Barberis B, Cardellino S, Livigni S, Fiore G, Filippini C, Ranieri V: The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care 2013, 17: R50.
Mayr FB, Yende S, Linde-Zwirble WT, Peck-Palmer OM, Barnato AE, Weissfeld LA, Angus DC: Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. JAMA 2010, 303: 2495–2503.
Fildes JE, Shaw SM, Yonan N, Williams SG: The immune system and chronic heart failure: is the heart in control? J Am Coll Cardiol 2009, 53: 1013–1020.
Schreiber RD, Old LJ, Smyth MJ: Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science 2011, 331: 1565–1570.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992, 101: 1644–1655.
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent J-L, Ramsay G: 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med 2003, 31: 1250–1256.
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, Calandra T, Dhainaut J-F, Gerlach H, Harvey M, Marini JJ, Marshall J, Ranieri M, Ramsay G, Sevransky J, Thompson BT, Townsend S, Vender JS, Zimmerman JL, Vincent J-L: Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 2008, 34: 17–60.
Zhang Q, Raoof M, Chen Y, Sumi Y, Sursal T, Junger W, Brohi K, Itagaki K, Hauser CJ: Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature 2010, 464: 104–107.
Menu P, Vince JE: The NLRP3 inflammasome in health and disease: the good, the bad and the ugly. Clin Exp Immunol 2011, 166: 1–15.
Vandenesch F, Lina G, Henry T: Staphylococcus aureus hemolysins, bi-component leukocidins, and cytolytic peptides: a redundant arsenal of membrane-damaging virulence factors? Front Cell Infect Microbiol 2012, 2: 12.
Kanoh S, Rubin BK: Mechanisms of action and clinical application of macrolides as immunomodulatory medications. Clin Microbiol Rev 2010, 23: 590–615.
Mikawa K, Akamatsu H, Maekawa N, Nishina K, Niwa Y: Propofol inhibits human neutrophil. Anesth Analg 1998, 87: 695–700.
Vallejo R, de Leon-Casasola O, Benyamin R: Opioid therapy and immunosuppression: a review. Am J Ther 2004, 11: 354–365.
Lawson EH, Louie R, Zingmond DS, Brook RH, Hall BL, Han L, Rapp M, Ko CY: A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg 2012, 256: 973–981.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE: APACHE II: a severity of disease classification system. Crit Care Med 1985, 13: 818–829.
Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, Sirio CA, Murphy DJ, Lotring T, Damiano A: The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 1991, 100: 1619–1636.
ASA Physical Status Classification System. . Accessed 27 Jun 2013 http://www.asahq.org/For-Members/Clinical-Information/ASA-Physical-Status-Classification-System.aspx
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM: CDC definitions for nosocomial infections, 1988. Am Rev Respir Dis 1989, 139: 1058–1059.
Baker SP, O’Neill B, Haddon W, Long WB: The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974, 14: 187–196.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
GLA is supported by an Academy of Medical Science/Health Foundation Clinician Scientist Award. This work was undertaken at UCLH/UCL which received a proportion of funding from the Department of Health's NIHR Biomedical Research Centres funding scheme.
Authors’ contributions
DC performed literature search, compiled data tables plus results and drafted the manuscript. AGDA designed the study and drafted/revised manuscript. GLA designed the study and drafted/revised manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Cain, D.J., del Arroyo, A.G. & Ackland, G.L. Uncontrolled sepsis: a systematic review of translational immunology studies in intensive care medicine. ICMx 2, 6 (2014). https://doi.org/10.1186/2197-425X-2-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2197-425X-2-6