Abstract
Suspicion of sepsis in neutropenic patients requires immediate antimicrobial treatment. The initial regimen in critically ill patients should cover both Gram-positive and Gram-negative pathogens, including Pseudomonas aeruginosa. However, the risk of selecting multidrug-resistant pathogens should be considered when using broad-spectrum antibiotics for a prolonged period of time. The choice of the first-line empirical drugs should take into account the underlying malignancy, local bacterial ecology, clinical presentation and severity of acute illness. This review provides an up-to-date guide that will assist physicians in choosing the best strategy regarding the use of antibiotics in neutropenic patients, with a special focus on critically ill patients, based on the above-mentioned considerations and on the most recent international guidelines and literature.
Similar content being viewed by others
Introduction
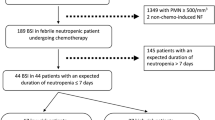
Neutropenia is defined as a neutrophil count ≤ 500/mm3 or ≤ 1000/mm3 with a predicted decrease to ≤ 500/mm3 [1, 2]. Infection remains a major complication of neutropenia, and severe sepsis and septic shock are associated with high hospital mortality [3, 4]. Fever, defined as a single oral temperature ≥38.3°C or ≥38.0°C for at least 1 hour, develops in 10-50% of patients after chemotherapy for solid tumors and in more than 80% of patients with hematological malignancies [5].
Urgent and appropriate antibiotic administration is mandatory to prevent further clinical deterioration, especially in critically ill patients with signs of respiratory distress or severe sepsis. Therefore, the first-line antibiotics should cover the pathogens deemed to be most likely based on the patient's characteristics, neutropenia, and local epidemiology. However, the changing epidemiology of infections, global increase in resistant strains, and need to contain healthcare costs require careful selection of antibiotics. Only 10-40% of episodes of febrile neutropenia are microbiologically documented in neutropenic patients, which hampers appropriate antibiotic spectrum adjustment in most cases [5]. This review provides an up-to-date guide to assist physicians in choosing the optimal antibiotic regimen in neutropenic patients, based on the above-mentioned considerations and on the most recent international guidelines and literature.
Bacterial epidemiology in neutropenic patients
During the 1990s, Gram-positive bacteria emerged as the leading agents responsible for infections in neutropenic patients worldwide. In adults with bloodstream infections and malignancies in the United States, the proportion of Gram-positive organisms increased from 62% in 1995 to 76% in 2000, whereas the proportion of Gram-negative infections decreased from 22% to 15% [6]. Factors that may increase the risk of Gram-positive sepsis in neutropenic patients include the widespread use of central venous catheters, introduction of prophylactic quinolone therapy, increased use of proton pump inhibitors, and rising prevalence of chemotherapy-induced mucositis [7]. Importantly, Gram-negative bacteria seem to be causing an increasing number of infections in neutropenic patients since the early 2000s (Table 1). The selection of empirical antimicrobials depends in part on an assessment of which pathogens are most likely to be involved. Table 2 shows a nonexhaustive list of pathogens with their possible sites of development in neutropenic patients. Although Gram-negative bacteria are usually associated with severe infections that have high mortality rates, coagulase-negative staphylococci (CNS), which are recognized as the most common causes of nosocomial bacteremia, often are associated with more indolent forms of infections and have been more prevalent among low-risk than among high-risk patients [8]. However, in the setting of sustained bacteremia, CNS is an emerging cause of nosocomial endocarditis, usually occurring as a complication of catheter-related infection [9]. Viridans group streptococcal bacteremia may be associated with fulminant infection and is common in patients with hematological malignancies and profound neutropenia [6].
A major concern is the emergence of multidrug-resistant bacteria [10, 11]. Among Gram-negative rods, Pseudomonas aeruginosa, Escherichia coli, Citrobacter freundii, Acinetobacter species, and Stenotrophomonas maltophilia are increasingly found to exhibit multidrug-resistance (i.e., resistance to three or more classes of antimicrobials), extensive drug resistance (i.e., resistance to all but one or two classes), or pandrug-resistance (i.e., resistance to all available classes) [12]. Antibiotic selection pressure promotes the induction of extended-spectrum chromosomal β-lactamases (ESBL) after the use of β-lactams [13, 14] and the selection of enterobacteria with decreased porin production after the use of carbapenems [11]. ESBL-producing Enterobacteriaceae are now commonly isolated in the community [15]. Furthermore, Enterobacteriaceae that produce Klebsiella pneumoniae carbapenemases (KPCs) are now reported worldwide, and KPCs have become the leading class A carbapenemases. KPC β-lactamases confer decreased susceptibility or resistance to virtually all β-lactams [16]. Similarly, fluoroquinolone exposure is associated with the emergence of methicillin-resistant Staphylococcus aureus (MRSA) and penicillin-resistant streptococci [17]. Widespread use of vancomycin has been described to cause outbreaks of bacteremia due to nosocomial vancomycin-resistant enterococci associated with high mortality rates [6]. Finally, other Gram-positive organisms with limited susceptibility or resistance to β-lactams have been increasingly isolated in cancer patients with febrile neutropenia; examples include Corynebacterium jeikeum, Lactobacillus, Bacillus species, and Rhodococcus species [12]. Antibiotic resistance rates vary widely across countries. For instance, the proportion of P. aeruginosa strains that exhibit carbapenem resistance is below 10% in Denmark, The Netherlands, Switzerland, Sweden, and Finland, greater than 25% in Croatia, Turkey, Germany, Italy, the Czech Republic, and as high as 45% in Greece [18].
Principles underlying first-line antibiotic therapy
Antibiotic therapy must be initiated immediately in febrile patients with neutropenia, especially when criteria of severe sepsis are met [1, 2]. The antibiotics used for first-line therapy must be active against the most likely pathogens, as estimated based on the suspected source of infection, patient's medical history, careful clinical examination, bacteriological findings, and x-ray results. Signs and symptoms of inflammation are frequently minimal or absent in patients with neutropenia. The initial assessment of patients with febrile neutropenia should include a careful physical examination for subtle signs and symptoms of infection, with special attention to the sinuses and oropharynx, skin and skin folds, intravenous lines, genital organs, and anal area. Obtaining bacterial samples is crucial to ensure the detection and susceptibility testing of the causative pathogen. Most pathogens are isolated from blood cultures, which must be drawn both from the catheter and from a peripheral vein. Cultures of stool, urine, cerebrospinal fluid, and/or skin lesions should be performed as indicated by the clinical picture. Previous microbiological results should be considered, because carriage of multiresistant strains may last several weeks or months [19]. A chest radiograph should be obtained, and high-resolution computed tomography of the chest may be indicated if the patient has pulmonary symptoms with an uninformative chest radiograph or if an invasive mold infection is suspected [1, 2].
Choice of the first-line antibiotic regimen
Route of empirical antibiotic therapy
Although oral antibiotic administration can be an option in neutropenic patients with the lowest risk of complications, all patients with prolonged (> 7 days duration) and/or profound neutropenia (< 100 cells/mm3) and/or abdominal pain, nausea and/or vomiting diarrhea and/or criteria of severe sepsis or septic shock with signs of organ failure should be treated intravenously. Suspicion of catheter-related infection or new pulmonary infiltrates are other indications of intravenous antibiotics administration.
Antibiotic combinations
The advantages of combination therapy include coverage of a broad spectrum of pathogens and, theoretically, synergistic activity with a decrease in the emergence of resistant strains. The main downsides are ototoxicity and nephrotoxicity, most notably with aminoglycosides, and increased cost. It should be pointed out that nephrotoxicity may occur even with very short courses of aminoglycosides, particularly with multiple-dose regimens and in patients receiving or having received other toxic substances (e.g., cisplatin, ciclosporin, amphotericin B, colistin, acyclovir, or contrast media) [20, 21].
So far, no randomized study or metaanalysis has proven that adding an aminoglycoside or quinolone to a β-lactam is superior over using a broad-spectrum β-lactam alone. Results from a recent multicentric propensity matched cohort study have suggested that early combination antibiotic therapy is associated with decreased mortality in septic shock. Although not being the focus of this study, it is likely that neutropenic patients also may benefit from antibiotic combination antibiotic therapy [22]. Given that P. aeruginosa infection is rather common and associated with high mortality rates in neutropenic patients [23], the empirical antibiotic regimen should cover this pathogen. Monotherapy with ceftazidime, imipenem, or piperacillin/tazobactam seems to be as effective as β-lactam/aminoglycoside combinations, even in the subset of bacteremic patients [1, 2].
There are no studies of β-lactam/aminoglycoside combinations in critically ill neutropenic patients. According to the aforementioned guidelines, β-lactam plus aminoglycoside combinations may be justified in patients with severe sepsis or septic shock and in those with suspected resistant Gram-negative infections. The safety of cefepime has recently been put into question by a meta-analysis, suggesting an increase risk of death associated with the use of cefepime in neutropenic patients [24]. The mechanism underlying such an association could not been identified. However, the U.S. Food and Drug Administration (FDA) still approves cefepime based on a new metaanalysis performed by the Agency, including additional data, which did not find any increase in mortality in cefepime-treated compared with control patients [2].
Ciprofloxacin has good activity against Gram-negative bacteria, including Pseudomonas aeruginosa, but poor coverage of Gram-positive organisms. Levofloxacin has better activity against Gram-positive organisms but less activity against Pseudomonas aeruginosa. However, fluoroquinolones use is associated with the emergence of antibiotic-resistant pathogens, and therefore, their use in initial empirical regimens should be discouraged, particularly in patients with a history of quinolone-based prophylaxis.
In febrile neutropenic patients, efficacy seems largely equivalent with β-lactam monotherapy by cefepime, piperacillin/tazobactam, and carbapenems [1, 2, 25, 26] (Table 3). Ceftazidime monotherapy may be an effective strategy. However, the limited activity of ceftazidime against Gram-positive bacteria is of concern in high-risk neutropenic patients, because streptococcal bacteremia is associated with high complication rates [27]. Although most broad spectrum β-lactams (cefepime, piperacillin/tazobactam, and carbapenems) provide coverage against most Gram-positive bacteria, some Gram-positive organisms, such as S. mitis, methicillin-resistant S. aureus, Enterococcus faecium, and Corynebacterium species, may be resistant to β-lactams and susceptible only to glycopeptides (i.e., vancomycin and teicoplanin), quinupristin-dalfopristin, daptomycin, or linezolid. The appropriateness of adding vancomycin to a β-lactam has long been a matter of debate. Given the risk of emergence of resistant pathogens due to widespread vancomycin use and the often relatively indolent course of infections due to the most commonly isolated resistant Gram-positive organisms (i.e., CNS), routinely adding vancomycin to the first-line regimen is now strongly discouraged in stable patients [1, 2, 28]. In contrast, the vancomycin/β-lactam combination remains recommended for the first-line treatment of patients with severe sepsis or septic shock and of patients at high risk for infection by antibiotic-resistant Gram-positive cocci (i.e., those with prolonged (> 7 days) and profound (absolute neutrophil count < 100 cells/mm3) neutropenia and/or presenting with hypotension, pneumonia, new-onset abdominal pain, or neurologic changes [1, 2], Table 3).
In a randomized, controlled study of neutropenic patients with cancer, linezolid and vancomycin produced similar outcomes [29]. The limited data on linezolid and the bacteriostatic activity of this drug are of concern when treating neutropenic patients. Linezolid may finally cause marrow suppression when given for more than 14 days. Limited data exist on daptomycin in neutropenic patients, but it may represent an alternative in selected situations [30].
In all likelihood, no guidelines of universal relevance can be developed. Instead, the global epidemiology of bacterial infections should be considered in conjunction with local rates of pathogen isolation and resistance. The patient's own ecology also should be considered. Valuable information can be garnered from a review of previous anterior nasal and rectal swabs, which may have shown colonization by antibiotic-resistant bacteria (e.g., methicillin-resistant S. aureus, P. aeruginosa, multidrug-resistant Gram-negative bacilli, and vancomycin-resistant enterococci). A history of infection should raise the possibility of a recurrence and should prompt the use of antibiotics active against the pathogen involved. Finally, renal and hepatic function and the risk of allergies may influence the choice of the first-line antibiotics.
Adapting the antibiotics: treatment duration
Failure to respond to empirical therapy is defined as persistent fever and the development of serious medical complications. The median time to defervescence in hospitalized patients with cancer is 5-7 days, although low-risk patients often respond within 2 days or less [1, 2]. International guidelines recommend a reassessment of the initial antibiotic regimen after 3-5 days if the fever persists [1, 2]. Persistence of fever with clinical deterioration or infectious disease progression should be distinguished from persistence of fever in a clinically stable patient. Patients whose clinical status deteriorates require a complete reassessment, including a careful physical examination and the collection of new culture specimens to look for a second infection. Ultrasonography and high-resolution computed tomography should be performed as indicated by the clinical data, and the indwelling catheter should be removed if a catheter-related infection is proven or strongly suspected. If a resistant pathogen is isolated or suspected to be responsible for the deterioration (i.e., if present in a recent stool culture) and is not covered by initial empirical regimen, the treatment should be modified promptly. Empirical addition of a glycopeptide, if not used initially, may be warranted, and switching from piperacillin-tazobactam or a third-generation cephalosporin to a carbapenem as second-line therapy should be considered (Figure 1). Finally, empirical addition of antifungal agents deserves consideration in patients who have risk factors for fungal infection [1, 2, 28, 31]. The management of antifungal therapy is beyond the scope of this chapter, but readers can refer to specific reviews on this topic [31–33]. For clinically stable patients with persistent fever, there is no published evidence to support a change in the antibiotic regimen. Moreover, the widespread emergence of multiresistant and panresistant bacterial strains should discourage "escalating" strategies, such as switching from piperacillin-tazobactam or cefepime to a carbapenem or adding vancomycin. When a causative pathogen is identified, the antibiotic regimen should be adapted based on the antibiotic susceptibility test results. The dwindling number of drugs in the pharmaceutical pipeline and the increased incidence of multidrug-resistant bacteria have led to the increasing use of old antibiotics, such as colistin [34].
Colistin exhibits rapid and concentration-dependent bactericidal activity with relatively low rates of resistance. Good rates of clinical responses have been reported in patients infected with multidrug-resistant bacteria and treated with intravenous colistin as salvage therapy. Colistin may act synergistically with rifampin or carbapenems against metallo-β-lactamase-producing (MBL) K. pneumoniae or A. baumannii strains. However, these data on colistin are chiefly from nonrandomized studies in small numbers of patients. Although the manufacturer recommends not exceeding 6 million units per day, a growing number of clinicians now routinely use daily dosages of up to 9 million IU in two to four divided doses (12,500 IU of colistin is equivalent to 1 mg of the prodrug colistin methanesulfonate). Inhalational colistin therapy has long been used in patients with cystic fibrosis and is now proposed in critically ill patients with ventilator-associated pneumonia. However, clinical data are derived from small, retrospective, nonrandomized studies. We have very little information on colistin pharmacokinetics and pharmacodynamics, especially in critically ill patients. Recently, Lu et al. reported that inhaled colistin resulted in relative higher lung tissue bioavailability in piglets compared with animals treated with intravenous colistin [35]. Nephrotoxicity associated with the use of colistin remains a matter of concern. In vitro studies have shown that the toxic effects of colistin on mammalian cells are concentration-dependent and time-dependent. Colistin nephrotoxicity seems rare in young patients with normal renal function and common in patients with underlying renal insufficiency. The risk may depend on the cumulative dose. Colistin nephrotoxicity is usually mild and almost always reversible within a few weeks or months after treatment discontinuation.
When no antibiotic-resistant Gram-positive bacteria are isolated, withdrawal of glycopeptides is warranted and may limit the emergence of vancomycin-resistant enterococci and the risk of nephrotoxicity [1, 2, 11]. Similarly, de-escalation (e.g., switching from carbapenem to cefepime or piperacillin-tazobactam) should be encouraged when no microorganism resistant to the first-line regimen is isolated.
In patients with sustained bacteremia and/or persistent fever and clinical deterioration, a portal of entry requiring specific treatment should be sought. Necrotizing cellulitis or peritonitis requires surgery. One of the commonest problems is deciding whether to remove the indwelling central venous catheter in bacteremic patients. The decision rests on the clinical presentation (septic shock, local tunnel, or port infection), pathogen, presence of intestinal colonization, and differential time to blood culture positivity of samples drawn simultaneously by phlebotomy and through the catheter. In patients with bacteremia due to Enterobacteriaceae, enterococci or Pseudomonas, with no local signs of catheter infection or septic shock, the conjunction of intestinal colonization and microbial growth in peripheral blood before or within 2 hours after growth in a sample obtained simultaneously from the catheter hub often indicates bacterial translocation from the intestine [36]. Further information regarding the management of catheter-related infections can been found in recently published guidelines [37].
Current guidelines recommend continued intravenous administration of antibiotics after 48 hours of apyrexia, for at least 2 days after neutropenia resolution or for 4-5 days if the fever persists [1]. Clinically or microbiologically documented infection may require longer treatment but with narrower-spectrum antibiotics (i.e., a neutropenic patient who has bacteremia due to multisusceptible E. coli treated with piperacillin-tazobactam should be switched to amoxicillin for a few additional days after neutropenia recovery).
International guidelines recommend that patients with persistent neutropenia remain on antibiotics for at least 2 weeks. All patients with persistent fever, with or without clinical deterioration, should be investigated for noninfectious causes of fever (Table 4). Finally, antibiotic dose adjustment based on serum concentration determination may be required, because changes in the pharmacodynamics and pharmacokinetics of antibiotics have been reported in neutropenic patients [38–40].
Pharmacodynamic and pharmacokinetic considerations
The pharmacokinetics and pharmacodynamics of many antibiotics are modified in neutropenic [38] and/or critically ill patients. The volume of distribution and clearance are increased, and therefore the half-life and plasma concentrations may be lower than in control patients. Many animal studies found decreases in the bactericidal activity of β-lactams in neutropenic animals. Given that the activity of β-lactams and glycopeptides depends on the time spent with serum drug concentrations greater than the minimum inhibitory concentration of the organism, decreasing the interval between doses or using a continuous infusion may be the best strategy for administering β-lactams and glycopeptides to neutropenic patients. In any case, therapeutic drug monitoring is valuable for guiding dosage adjustments and ensuring that therapeutic concentrations are achieved to increase the chances of eradicating the organism and to minimize the risk of selecting antibiotic-resistant bacteria [38, 41]. Serum vancomycin and teicoplanin levels should be monitored routinely [39]. In neutropenic patients who receive the recommended 2 g/day dose of imipenem, many may have serum concentrations below the therapeutic range [41]. When using carbapenems in neutropenic patients, 50-60% of the dosing interval must be spent above the minimum inhibitory concentration to achieve bactericidal activity, and success rates improve when 75-100% of the dosing interval is spent above the minimum inhibitory concentration [41–43]. Plasma carbapenem levels can be measured by using high-performance liquid chromatography in patients with persistent fever to ensure that the plasma concentrations are within the therapeutic range.
Aminoglycosides, in contrast, have a concentration-dependent bactericidal activity. Elimination of aminoglycosides is highly dependant on renal clearance, and accumulation is likely to occur in patients with renal failure. Once-daily administration of aminoglycosides often is preferred over multiple-daily dosing to reduce the risk of nephrotoxicity and is recommended in the few neutropenic patients who require an aminoglycoside in combination with a wide-spectrum β-lactam [28]. When using aminoglycosides, therapeutic drug monitoring is important to minimize the risk of renal and cochlear/vestibular toxicity [40]. A recently published review is available for readers who wish further information on antibiotic pharmacokinetics and pharmacodynamics in neutropenic patients [38].
Prophylactic antibiotics and hygiene mesures
The guidelines issued by the European Conference on Infections in Leukaemia recommend prophylactic ciprofloxacin or levofloxacin therapy from chemotherapy initiation to neutropenia resolution [28]. According to the most recent Infectous Diseases Society of America (IDSA) guidelines, such prophylaxis should only be considered [2]. In fact, many centers still do not give quinolone prophylaxis to patients with afebrile neutropenia, due to concerns about the emergence of antibiotic resistance in the long run [17]. The selection of resistant organisms by quinolones is a serious hazard, as re-emphasized recently [44]. The emergence of resistant strains should be monitored in centers where quinolone-based prophylaxis is used [2, 10, 45]. Hand hygiene remains the most effective measure to prevent hospital-acquired infections, whereas isolation into a single-patient room or use of specific protective gear (gowns, gloves, and masks) are not mandatory except for hematopoietic stem cell transplant recipients.
Conclusions
Antibiotic therapy must be initiated promptly in febrile neutropenic patients. In high-risk patients, initial empirical treatment with piperacillin-tazobatam or cefepime is recommended. In addition, the initial antibiotic strategy should be adapted based on the basis of initial clinical assessment, bacterial ecology in the hospital, and bacterial history in the patient. The use of vancomycin should be reserved for patients with suspected methicillin-resistant Gram-positive infections and/or signs of severe sepsis or septic shock. There is some evidence to support adding an aminoglycoside to the extended-spectrum β-lactams in critically ill neutropenic patients. Persistent fever requires adaptation of the initial antibiotic regimen if the clinical condition deteriorates or if a resistant pathogen is isolated. Addition of an antifungal agent must be considered. Giving the growing emergence of multidrug-resistant bacteria, the implementation of antibiotic stewardship programs is now mandatory.
References
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, Feld R, Pizzo PA, Rolston KV, Shenep JL, Young LS: 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 2002, 34: 730–751. 10.1086/339215
Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Raad II, Rolston KV, Young JA, Wingard JR, Infectious Diseases Society of America: Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer. In Clin Infect Dis. Volume 52. 2010 update of the Infectious Diseases Society of America; 2011:e56-e59. 10.1093/cid/cir073
Pene F, Percheron S, Lemiale V, Viallon V, Claessens YE, Marque S, Charpentier J, Angus DC, Cariou A, Chiche JD, Mira JP: Temporal changes in management and outcome of septic shock in patients with malignancies in the intensive care unit. Crit Care Med 2008, 36: 690–696. 10.1097/CCM.0B013E318165314B
Thiery G, Azoulay E, Darmon M, Ciroldi M, De Miranda S, Levy V, Fieux F, Moreau D, Le Gall JR, Schlemmer B: Outcome of cancer patients considered for intensive care unit admission: a hospital-wide prospective study. J Clin Oncol 2005, 23: 4406–4413. 10.1200/JCO.2005.01.487
Buchheidt D, Bohme A, Cornely OA, Fatkenheuer G, Fuhr HG, Heussel G, Junghanss C, Karthaus M, Kellner O, Kern WV, Schiel X, Sezer O, Sudhoff T, Szelenyi H: Diagnosis and treatment of documented infections in neutropenic patients--recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO). Ann Hematol 2003,82(Suppl 2):S127-S132.
Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB: Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis 2004, 39: 309–317. 10.1086/421946
Zinner SH: Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on gram-positive and resistant bacteria. Clin Infect Dis 1999, 29: 490–494. 10.1086/598620
Kamana M, Escalante C, Mullen CA, Frisbee-Hume S, Rolston KV: Bacterial infections in low-risk, febrile neutropenic patients. Cancer 2005, 104: 422–426. 10.1002/cncr.21144
Chu VH, Woods CW, Miro JM, Hoen B, Cabell CH, Pappas PA, Federspiel J, Athan E, Stryjewski ME, Nacinovich F, Marco F, Levine DP, Elliott TS, Fortes CQ, Tornos P, Gordon DL, Utili R, Delahaye F, Corey GR, Fowler VG Jr: Emergence of coagulase-negative staphylococci as a cause of native valve endocarditis. Clin Infect Dis 2008, 46: 232–242. 10.1086/524666
Ramphal R: Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin Infect Dis 2004,39(Suppl 1):S25-S31.
Irfan S, Idrees F, Mehraj V, Habib F, Adil S, Hasan R: Emergence of Carbapenem resistant Gram negative and vancomycin resistant Gram positive organisms in bacteremic isolates of febrile neutropenic patients: a descriptive study. BMC Infect Dis 2008, 8: 80. 10.1186/1471-2334-8-80
Kanamaru A, Tatsumi Y: Microbiological data for patients with febrile neutropenia. Clin Infect Dis 2004,39(Suppl 1):S7-S10.
Tumbarello M, Sanguinetti M, Montuori E, Trecarichi EM, Posteraro B, Fiori B, Citton R, D'Inzeo T, Fadda G, Cauda R, Spanu T: Predictors of mortality in patients with bloodstream infections caused by extended-spectrum-beta-lactamase-producing Enterobacteriaceae: importance of inadequate initial antimicrobial treatment. Antimicrob Agents Chemother 2007, 51: 1987–1994. 10.1128/AAC.01509-06
Moland ES, Black JA, Ourada J, Reisbig MD, Hanson ND, Thomson KS: Occurrence of newer beta-lactamases in Klebsiella pneumoniae isolates from 24 U.S. hospitals. Antimicrob Agents Chemother 2002, 46: 3837–3842. 10.1128/AAC.46.12.3837-3842.2002
Rodriguez-Bano J, Picon E, Gijon P, Hernandez JR, Ruiz M, Pena C, Almela M, Almirante B, Grill F, Colomina J, Gimenez M, Oliver A, Horcajada JP, Navarro G, Coloma A, Pascual A: Community-onset bacteremia due to extended-spectrum beta-lactamase-producing Escherichia coli: risk factors and prognosis. Clin Infect Dis 50: 40–48.
Cuzon G, Naas T, Nordmann P: KPC carbapenemases: what issue in clinical microbiology? Pathol Biol (Paris) 58: 39–45.
Cattaneo C, Quaresmini G, Casari S, Capucci MA, Micheletti M, Borlenghi E, Signorini L, Re A, Carosi G, Rossi G: Recent changes in bacterial epidemiology and the emergence of fluoroquinolone-resistant Escherichia coli among patients with haematological malignancies: results of a prospective study on 823 patients at a single institution. J Antimicrob Chemother 2008, 61: 721–728. 10.1093/jac/dkm514
European Antimicrobial Resistance surveillance System 2008 [http://www.rivm.nl/earss/database/:]
Mattner F, Biertz F, Ziesing S, Gastmeier P, Chaberny IF: Long-term persistence of MRSA in re-admitted patients. Infection 2010, 38: 363–71. 10.1007/s15010-010-0038-8
Cosgrove SE, Vigliani GA, Fowler VG Jr, Abrutyn E, Corey GR, Levine DP, Rupp ME, Chambers HF, Karchmer AW, Boucher HW: Initial low-dose gentamicin for Staphylococcus aureus bacteremia and endocarditis is nephrotoxic. Clin Infect Dis 2009, 48: 713–721. 10.1086/597031
Bayer AS, Murray BE: Initial low-dose aminoglycosides in Staphylococcus aureus bacteremia good science, urban legend, or just plain toxic? Clin Infect Dis 2009, 48: 722–724. 10.1086/597032
Kumar A, Zarychanski R, Light B, Parrillo J, Maki D, Simon D, Laporta D, Lapinsky S, Ellis P, Mirzanejad Y, Martinka G, Keenan S, Wood G, Arabi Y, Feinstein D, Kumar A, Dodek P, Kravetsky L, Doucette S: Cooperative Antimicrobial Therapy of Septic Shock (CATSS) Database Research Group. Early combination antibiotic therapy yields improved survival compared with monotherapy in septic shock: a propensity-matched analysis. Crit Care Med 2010, 38: 1773–85. 10.1097/CCM.0b013e3181eb3ccd
Picazo JJ: Management of the febrile neutropenic patient: a consensus conference. Clin Infect Dis 2004,39(Suppl 1):S1-S6.
Yahav D, Paul M, Fraser A, Sarid N, Leibovici L: Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis 2007, 7: 338–348. 10.1016/S1473-3099(07)70109-3
Harter C, Schulze B, Goldschmidt H, Benner A, Geiss HK, Hoppe-Tichy T, Ho AD, Egerer G: Piperacillin/tazobactam vs ceftazidime in the treatment of neutropenic fever in patients with acute leukemia or following autologous peripheral blood stem cell transplantation: a prospective randomized trial. Bone Marrow Transplant 2006, 37: 373–379. 10.1038/sj.bmt.1705256
Feld R, DePauw B, Berman S, Keating A, Ho W: Meropenem versus ceftazidime in the treatment of cancer patients with febrile neutropenia: a randomized, double-blind trial. J Clin Oncol 2000, 18: 3690–3698.
Han XY, Kamana M, Rolston KV: Viridans streptococci isolated by culture from blood of cancer patients: clinical and microbiologic analysis of 50 cases. J Clin Microbiol 2006, 44: 160–165. 10.1128/JCM.44.1.160-165.2006
Meunier F, Lukan C: The First European Conference on Infections in Leukaemia - ECIL1: a current perspective. Eur J Cancer 2008, 44: 2112–2117. 10.1016/j.ejca.2008.07.008
Jaksic B, Martinelli G, Perez-Oteyza J, Hartman CS, Leonard LB, Tack KJ: Efficacy and safety of linezolid compared with vancomycin in a randomized, double-blind study of febrile neutropenic patients with cancer. Clin Infect Dis 2006, 42: 597–607. 10.1086/500139
Rolston KV, McConnell SA, Brown J, Lamp KC: Daptomycin use in patients with cancer and neutropenia: data from a retrospective registry. Clin Adv Hematol Oncol 2010, 8: 249–256. 290
Almyroudis NG, Segal BH: Prevention and treatment of invasive fungal diseases in neutropenic patients. Curr Opin Infect Dis 2009, 22: 385–393. 10.1097/QCO.0b013e32832e074d
Ruping MJ, Vehreschild JJ, Cornely OA: Patients at high risk of invasive fungal infections: when and how to treat. Drugs 2008, 68: 1941–1962. 10.2165/00003495-200868140-00002
Spanakis EK, Aperis G, Mylonakis E: New agents for the treatment of fungal infections: clinical efficacy and gaps in coverage. Clin Infect Dis 2006, 43: 1060–1068. 10.1086/507891
Lim LM, Ly N, Anderson D, Yang JC, Macander L, Jarkowski A, Forrest A, Bulitta JB, Tsuji BT: Resurgence of colistin: a review of resistance, toxicity, pharmacodynamics, and dosing. Pharmacotherapy 2010, 30: 1279–1291. 10.1592/phco.30.12.1279
Lu Q, Girardi C, Zhang M, Bouhemad B, Louchahi K, Petitjean O, Wallet F, Becquemin MH, Le Naour G, Marquette CH, Rouby JJ: Nebulized and intravenous colistin in experimental pneumonia caused by Pseudomonas aeruginosa . Intensive Care Med 36: 1147–1155.
Raad I, Hanna H, Maki D: Intravascular catheter-related infections: advances in diagnosis, prevention, and management. Lancet Infect Dis 2007, 7: 645–657. 10.1016/S1473-3099(07)70235-9
Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, Raad II, Rijnders BJ, Sherertz RJ, Warren DK: Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis 2009, 49: 1–45. 10.1086/599376
Lortholary O, Lefort A, Tod M, Chomat AM, Darras-Joly C, Cordonnier C: Pharmacodynamics and pharmacokinetics of antibacterial drugs in the management of febrile neutropenia. Lancet Infect Dis 2008, 8: 612–620. 10.1016/S1473-3099(08)70228-7
Rybak MJ, Lomaestro BM, Rotscahfer JC, Moellering RC, Craig WA, Billeter M, Dalovisio JR, Levine DP: Vancomycin therapeutic guidelines: a summary of consensus recommendations from the infectious diseases Society of America, the American Society of Health-System Pharmacists, and the Society of Infectious Diseases Pharmacists. Clin Infect Dis 2009, 49: 325–327. 10.1086/600877
Bartal C, Danon A, Schlaeffer F, Reisenberg K, Alkan M, Smoliakov R, Sidi A, Almog Y: Pharmacokinetic dosing of aminoglycosides: a controlled trial. Am J Med 2003, 114: 194–198. 10.1016/S0002-9343(02)01476-6
Lamoth F, Buclin T, Pascual A, Calandra T, Marchetti O: Imipenem underdosing as a cause of persistent neutropenic fever? J Antimicrob Chemother 2009, 64: 665–667. 10.1093/jac/dkp233
Ariano RE, Nyhlen A, Donnelly JP, Sitar DS, Harding GK, Zelenitsky SA: Pharmacokinetics and pharmacodynamics of meropenem in febrile neutropenic patients with bacteremia. Ann Pharmacother 2005, 39: 32–38.
Mouton JW, Touzw DJ, Horrevorts AM, Vinks AA: Comparative pharmacokinetics of the carbapenems: clinical implications. Clin Pharmacokinet 2000, 39: 185–201. 10.2165/00003088-200039030-00002
Rangaraj G, Granwehr BP, Jiang Y, Hachem R, Raad I: Perils of quinolone exposure in cancer patients: breakthrough bacteremia with multidrug-resistant organisms. Cancer 116: 967–973.
Reuter S, Kern WV, Sigge A, Dohner H, Marre R, Kern P, von Baum H: Impact of fluoroquinolone prophylaxis on reduced infection-related mortality among patients with neutropenia and hematologic malignancies. Clin Infect Dis 2005, 40: 1087–1093. 10.1086/428732
Carratalà J, Rosón B, Fernández-Sevilla A, Alcaide F, Gudiol F: Bacteremic pneumonia in neutropenic patients with cancer: causes, empirical antibiotic therapy, and outcome. Arch Intern Med 1998, 158: 868–872. 10.1001/archinte.158.8.868
Gruson D, Hilbert G, Portel L, Boiron JM, Bebear CM, Vargas F, Bebear C, Reiffers J, Gbikpi-Benissan G, Cardinaud JP: Severe respiratory failure requiring ICU admission in bone marrow transplant recipients. Eur Respir J 1999, 13: 883–887. 10.1034/j.1399-3003.1999.13d31.x
Regazzoni CJ, Khoury M, Irrazabal C, Myburg C, Galvalisi NR, O'Flaherty M, Sarquis SG, Poderoso JJ: Neutropenia and the development of the systemic inflammatory response syndrome. Intensive Care Med 2003, 29: 135–138.
Klastersky J, Ameye L, Maertens J, Georgala A, Muanza F, Aoun M, Ferrant A, Rapoport B, Rolston K, Paesmans M: Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents 2007,30(Suppl 1):S51-S59.
Metallidis S, Kollaras P, Giannakakis T, Seitanidis B, Kordosis T, Nikolaidis J, Hatzitolios A, Nikolaidis P: A prospective, controlled, randomized, non-blind, comparative study of the efficacy and safety of a once daily high dose of ceftriaxone plus ciprofloxacin versus thrice daily ceftazidime plus amikacin in empirical therapy for febrile neutropenic patients. Eur J Intern Med 2008, 19: 619–624. 10.1016/j.ejim.2007.08.011
de la Rubia J, Montesinos P, Martino R, Jarque I, Rovira M, Vazquez L, Lopez J, Batlle M, de la Camara R, Julia A, Lahuerta JJ, Deben G, Diaz J, Garcia R, Sanz MA: Imipenem/cilastatin with or without glycopeptide as initial antibiotic therapy for recipients of autologous stem cell transplantation: results of a Spanish multicenter study. Biol Blood Marrow Transplant 2009, 15: 512–516. 10.1016/j.bbmt.2008.12.505
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
ML and AM wrote the first draft of the manuscript. BS, EA, and BG revised the manuscript. All authors read and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Legrand, M., Max, A., Schlemmer, B. et al. The strategy of antibiotic use in critically ill neutropenic patients. Ann. Intensive Care 1, 22 (2011). https://doi.org/10.1186/2110-5820-1-22
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2110-5820-1-22