Abstract
Introduction
Mutations in isocitrate dehydrogenase genes IDH1 or IDH2 are frequent in glioma, and IDH mutation status is a strong diagnostic and prognostic marker. Current IDH mutation screening is performed with an immunohistochemistry (IHC) assay specific for IDH1 R132H, the most common mutation. Sequencing is recommended as a second-step test for IHC-negative or -equivocal cases. We developed and validated a new real-time quantitative polymerase chain reaction (PCR) assay for single-step detection of IDH1 R132H and 11 rare IDH1/2 mutations in formalin-fixed paraffin-embedded (FFPE) glioma samples. Performance of the IDH1/2 PCR assay was compared to IHC and Sanger sequencing.
Results
The IDH1/2 PCR assay combines PCR clamping for detection of 7 IDH1 and 5 IDH2 mutations, and Amplification Refractory Mutation System technology for specific identification of the 3 most common mutations (IDH1 R132H, IDH1 R132C, IDH2 R172K). Analytical sensitivity of the PCR assay for mutation detection was <5% for 11/12 mutations (mean: 3.3%), and sensitivity for mutation identification was very high (0.8% for IDH1 R132H; 1.2% for IDH1 R132C; 0.6% for IDH2 R172K). Assay performance was further validated on 171 clinical glioma FFPE samples; of these, 147 samples met the selection criteria and 146 DNA samples were successfully extracted. IDH1/2 status was successfully obtained in 91% of cases. All but one positive IDH1 R132H-IHC cases were concordantly detected by PCR and 3 were not detected by sequencing. Among the IHC-negative cases (n = 72), PCR detected 12 additional rare mutations (10 IDH1, 2 IDH2). All mutations detected by sequencing (n = 67) were concordantly detected by PCR and 5/66 sequencing-negative cases were PCR-positive (overall concordance: 96%). Analysis of synthetic samples representative of the 11 rare IDH1/2 mutations detected by the assay produced 100% correct results.
Conclusions
The new IDH1/2 PCR assay has a high technical success rate and is more sensitive than Sanger sequencing. Positive concordance was 98% with IHC for IDH1 R132H detection and 100% with sequencing. The PCR assay can reliably be performed on FFPE samples and has a faster turnaround time than current IDH mutation detection algorithms. The assay should facilitate implementation of a comprehensive IDH1/2 testing protocol in routine clinical practice.
Similar content being viewed by others
Introduction
Histopathological evaluation remains the gold standard for glioma classification [1] but the incorporation of emergent molecular biomarkers has been shown to improve diagnosis and prognosis of this heterogeneous disease. In addition to the established 1p/19q co-deletion and MGMT methylation, new biomarkers including IDH1/2, EGFR or BRAF mutations and FGFR gene fusions, are increasingly documented to play a role as diagnostic, prognostic or predictive markers, and should progressively be introduced in the diagnostic and treatment decision algorithm for glioma [2, 3].
IDH1/2 mutations are highly frequent (up to 80%) in diffuse glioma [4–6]. Their identification in surgical neuropathology samples increases diagnostic accuracy of World Health Organization (WHO) grade II or III astrocytoma, oligodendroglioma, oligoastrocytoma, and WHO grade IV secondary glioblastoma (GBM) [5, 7]. In addition, IDH mutations have been repeatedly shown to be associated with significantly better patient survival, thereby providing valuable prognostic information [8–12]. Based on these findings, IDH1 mutation status is becoming part of the standard diagnostic assessment of these tumors and will likely be included in the next WHO classification of diffuse gliomas [2].
In addition, IDH mutation status may predict benefit from alkylating agent when combined with MGMT promoter methylation assessment [13]. Very recently, updated data from the RTOG 9402 trial showed that the IDH mutation predicts the benefit of adjuvant chemotherapy in grade III glioma, even in absence of 1p19q co-deletion [14]. Recent data suggested that IDH1 mutation may also serve as a predictive marker to guide aggressive surgical resection of malignant astrocytomas [15].
Given the high IDH clinical relevance, stratification according to IDH mutation should be taken into account for more effective future clinical trials [2, 16]. In addition, the discovery of IDH mutations has led to the development of novel therapies targeted against IDH alterations, using selective IDH inhibitors or by reversion of mutated-IDH induced hypermethylation with the use of DNA methyltransferase inhibitors [17–19].
IDH1 R132H mutation represents the most common IDH mutation (approximately 90%). Less common are the IDH mutations within the same IDH1 codon 132 (around 7%), and in the homologous IDH2 codon 172 (approximately 3%) [20].
An algorithm for IDH mutation screening has recently been proposed [21]. It is a two-step process implying initial search for the most common IDH1 R132H mutation using immunohistochemistry (IHC)-based assay, followed by DNA-based analysis on IHC-negative or -equivocal cases. The IDH1 R132H mutation-specific antibody shows high sensitivity and specificity [7, 22], but the IHC technique can be problematic in some cases, as a result of background staining or regional heterogeneity of IDH1 R132H protein expression [23]. Regarding DNA-based analyses, Sanger sequencing still represents the gold standard for the identification of somatic mutations. However, sequencing sensitivity is low (around 15-20% mutation load) and this may lead to false negative results when analyzing tumor specimens with insufficient neoplastic cells in a background of normal cells. Moreover, this technology is also not readily available in all neuropathological centers, and its use generally leads to additional delay in providing a comprehensive IDH mutational status assessment. Here we describe a new IDH1/2 polymerase chain reaction (PCR) assay which was designed to detect the most common IDH1 R132H mutation and 11 rare IDH mutations in one single step using formalin-fixed paraffin-embedded (FFPE) samples. Analytical studies were conducted to verify its performance. This assay was further validated on a large series of FFPE glioma samples to determine the reliability of the method in a routine clinical setting, by comparing IDH1/2 mutation analysis with IHC and Sanger sequencing.
Materials and methods
IDH1/2 one-step quantitative PCR assay
PCR-clamping was used for the qualitative detection of 6 mutations within IDH1 codon 132 (the 2 major R132H and R132C mutations, and 4 “IDH1-other”: R132G, R132S, R132L, R132V), one within IDH1 codon 100 (R100Q) and 5 within IDH2 codon 172 (the major R172K and 4 “IDH2-other”: R172M, R172W, R172S, R172G). Amplification Refractory Mutation System (ARMS) PCR technology was combined to selectively identify the most frequent IDH1 R132H/R132C and IDH2 R172K mutations (Table 1).
The therascreen IDH1/2 RGQ PCR kit was used following manufacturer’s instructions (Qiagen). The test consisted in 9 separate amplification reactions: (i) 3 total amplification reactions (“Total IDH1 R132”, “Total IDH2 R172” and “Total IDH1 R100”), (ii) 3 mutation amplification reactions of IDH1 codon 132 (“IDH1 R132 Mut”), IDH1 codon 100 (“IDH1 R100 Mut”) and IDH2 codon 172 (“IDH2 R172 Mut”), and (iii) 3 mutation-specific amplification reactions of IDH1 R132H (“IDH1 Mut R132H”), IDH1 R132C (“IDH1 Mut R132C”) and IDH2 R172K (“IDH1 Mut R172K”). Total reaction mixes for (i) contained primers and probes amplifying both wild-type (WT) and IDH-mutated target sequences. Mutation detection reaction mixes for (ii) combined specific primers and probes to amplify both mutated and WT target sequences, plus a WT-specific 3’P-blocked oligonucleotide preventing elongation (PCR clamping). Mutation identification for (iii) was achieved by allele-specific amplification using ARMS (Figure 1).
Principle of the IDH1/2 PCR assay. Total reaction mixes (top) The total Primers and Probe Mixes (PPM-Total) used primers and probes to amplify both mutated and wild-type (WT) target sequences. Mutation detection reaction mixes (middle) The mutation detection primers and probe mixes combined primers and probes, to amplify both mutated and WT target sequences, plus an oligonucleotide, 3'-blocked with the addition of a phosphate group (3’-Oligo-P) to prevent elongation (PCR clamping), which was specific to the WT target sequence. When the PCR template contained the WT sequence, the 3'-Oligo-P bound preferentially over the PCR primer binding due to higher affinity. There was no or low extension by the DNA polymerase and no or low amplification was observed. When a mutated sequence was present, PCR primer bound preferentially over the 3'-Oligo-P and amplification proceeded. Mutation identification reaction mixes (bottom) Allele-specific amplification was achieved by ARMS® (Amplification Refractory Mutation System), which exploits the ability of the DNA polymerase to distinguish between a match and a mismatch at the 3' end of a PCR primer. When the PCR primer fully matched, the amplification proceeded with full efficiency. When the 3' base was a mismatch, only low-level background amplification occurred. The same principle shown on the figure to detect IDH1 R132H applied for IDH1 R132C and IDH2 R172K.
PCRs were performed with 25 ng of sample or control DNA using the Rotor-Gene Q 5-plex HRM instrument (Qiagen). Run controls (positive, negative and no template control) were assessed to ensure that acceptable Ct values were met and that the reactions were performed correctly. Each sample was processed once per PCR run.
Sample ΔCt values were calculated as the difference between the mutation assay Ct and respective total assay Ct from the same sample. Samples were classified as mutation-positive if the ΔCt value was less than or equal to the ΔCt cut-off value of the respective mutation assay.
Determination of the cut-off values of the assay
Limit of Detection (LOD), defined as the lowest amount of mutant DNA in a WT DNA background, was based on the “precision profile approach” following the CLSI EP17-A2 guideline [24]. A sample set was developed by mixing synthetic IDH mutant DNA with WT genomic DNA to correspond to 5 IDH1/2 mutation positive percentages (2, 5, 10, 15 and 20%). In total, 30 to 110 measurements were made per mutation type and mutation percentage. Each sample was run in duplicate, over 5 days on 3 different instruments and with 3 different lots of IDH1/2 therascreen kits, leading to a total of 2250 ΔCt measurements.
For each mutation LOD, the associated mutation percentage was estimated by fitting a non-linear model between ∆Ct values and mutant percentage.
IDH1/2 quantitative PCR assay repeatability and reproducibility
The precision of the therascreen IDH1/2 kit was determined using a protocol based on the CLSI EP05-A2 [25]. The following deviations were estimated: within-run repeatability (Sr), between-runs reproducibility (Srun), within and between-days and precision of the assay (Stot).
Synthetic mutant samples were used for this evaluation: WT genomic DNA from clinical glioma FFPE samples was spiked in 3 mastered proportions (5, 10 and 30% mutant copies) with either R100Q, R132C, R132H or R172K plasmid mutant DNA. Corresponding WT DNA (0%) was also tested. Each sample was tested 40 times in duplicate i.e. 80 ΔCt measurements. Runs were performed by 3 operators over 10 days, on 2 RGQ instruments, with 3 different lots of IDH1/2 therascreen kits leading to a total of 2240 ΔCt measurements. A variance Component Analysis (fully nested Model II ANOVA) was performed on ΔCt values to estimate the different sources of variability for each mutation test.
Glioma clinical samples
A total of 171 FFPE clinical tumor samples were collected. In total, 121 samples were retrospectively collected from the Pitié-Salpêtrière Hospital (n = 19) and the Mayo Clinic (n = 102) tumor banks and 50 additional FFPE samples were collected from commercial tumor banks. All FFPE sections were reviewed by local neuropathologists for diagnosis of glioma and assessment of neoplastic cellularity. Samples selection criteria were based on age of the samples (<10 years old), tissue area (≥50 mm2) and neoplastic cellularity (sections with ≥40% tumor cells).
Synthetic mutant-IDH DNA samples
Synthetic samples representative of each of the 6 minor IDH1 and 5 IDH2 mutations (Table 1) were prepared at 2 dilutions (30 and 40%) by mixing mutant-IDH synthetic DNA into WT IDH genomic DNA. The samples were processed similarly to clinical samples.
Immunochemistry
The presence and extent of tumor was assessed on H&E slides. Immunohistochemical staining for mutant IDH1 was performed using the anti-human IDH1 R132H mouse monoclonal antibody DIA clone H09 (Dianova, Germany) at a dilution of 1:100. Pretreatment of slides with Cell Conditioner 1 (EDTA) MILD using the Ventana BenchMark XT stainer system was followed by incubation with the primary antibody for 32 minutes at 37°C, which was then detected using Ventana UltraView detection with Ventana DAB. Hematoxylin counterstain was performed with the Leica ST 5020 apparatus. Positive and negative controls were performed using specimens previously validated.
DNA extraction from FFPE samples
DNA was extracted from 10 μm FFPE sections using the QIAamp DNA FFPE Tissue kit (Qiagen) following instructions for use of the therascreen IDH1/2 RGQ PCR kit (Qiagen).
IDH1 and IDH2 sequencing
Bidirectional Sanger sequencing was performed centrally (Qiagen, Hilden). Fragments of 129 base pairs (bp) for IDH1 codon 132 and 150 bp length for IDH2 codon 172 were amplified using primers previously described [21]. A fragment containing IDH1 codon 100 was amplified using the following primers: 5’-AAGGATGCTGCAGAAGCTATAA-3’ (forward) and 5’-CCATAAGCATGACGACCTATGA-3’ (reverse). Briefly, PCR was performed in a total volume of 60 μL using 15 ng of DNA and Taq Polymerase Platinium in standard PCR buffer conditions. Initial denaturation at 94°C for 2 minutes was followed by 35 cycles of 94°C for 30 secondes, 55°C for 30 secondes and 68°C for 30 secondes. PCR products were purified using the QIAquick 96 PCR Purification kit (Qiagen, Hilden). The purified PCR products (1.5 μL) were sequenced using Applied Biosystems Big Dye 3.1 dideoxy chain termination sequencing chemistry in conjunction with fluorescent-based capillary sequencers (Model 3730xl Applied Biosystems Division of Perkin Elmer, Foster City, California, USA) for electrophoresis, data collection and base calling.
Pyrosequencing for detection of IDH1 codon 132 and IDH2 codon 172 mutations was performed as previously described [26]. Locked Nucleic Acid (LNA) Sanger sequencing was performed in a separate reaction by amplifying the mutation hotspot regions using the pyrosequencing PCR primers and LNA (+T + A + G + G + T + C + G + T + C + A+/3InvdT/) at the final concentration of 70 nM. The PCR product was sequenced using BigDye Terminator v1.1 Sequencing kit (Applied Biosystems; Foster City, CA, USA).
Statistical analyses
The main objective of the clinical validation study was to calculate the Positive Percent Agreement (PPA) first, between the IDH1/2 PCR test and IDH1 R132H IHC, and secondly, between the IDH1/2 PCR test and Sanger sequencing. For both comparisons, the aim was to obtain a PPA of at least 90% with a target of 95%, with a lower boundary (Lbound) of 95% confidence interval (CI) ≥90%.
The PPA between the PCR test and the reference methods (IHC and Sanger sequencing) was calculated as the percentage of true positive (TP) i.e. the percentage of cases detected as positive by both the IDH1/2 PCR test and the reference method, according to the following formula: PPA = (100×TP)/(TP + FN), where FN were false-negative cases i.e. negative by PCR when reference method was positive.
Secondary objectives were to calculate the Negative Percent Agreement (NPA) defined as NPA = (100×TN)/(TN + FP) and overall agreement (OA) defined as OA = (TP + TN)/(TP + TN + FP + FN), where TN and FP were true negative and false positive cases, respectively.
Results
Determination of sensitivity
The IDH1/2 assay was based on a combination of PCR-clamping and ARMS technology and can detect 12 IDH1/2 mutations (Table 1). Assay sensitivity was therefore estimated for each mutation, by LOD using mixed mutant IDH DNA with WT genomic DNA at 5 mutation percentages i.e. 2, 5, 10, 15 and 20%. Sensitivity varied according to mutations, ranging from 0.6% to 15%, (Figure 2 and Additional file 1: Table S1) with a mean of 3.3%. Sensitivity results are shown as supplementary data (Additional file 2: Figure S1). Reproducible and reliable mutation detection was achieved at a concentration of mutant DNA below 5% for 11/12 mutations and ≤3% for 9 mutations. The identification of the 3 major IDH1/2 mutations showed very high sensitivity levels, respectively 0.8% for IDH1 R132H, 1.2% for IDH1 R132C and 0.6% for IDH2 R172K (Figure 2 and Additional file 1: Table S1).
Sensitivity of the IDH1/2 PCR assay for the 12 detected and 3 identified IDH1/2 mutations. The sensitivity defined as the lowest amount of mutant DNA in a background of wild-type DNA was indicated for each of the 12 IDH1/2 mutations detected with the PCR IDH1/2 kit. The cut-off values were derived from a total of 2250 ΔCt measurements. Sensitivity varied across mutations from 0.6% to 15% with a mean of 3.3% (red dotted line). Limit of Detection was <5% for 11/12 mutations and ≤3% for 9 of them.
Repeatability and reproducibility
IDH WT and mutant samples were tested at 3 different mutant allele burden (5, 10 and 30%) and precision performance of the IDH1/2 PCR assay was established on a total of 2240 measurements (see Materials and Methods). High precision was demonstrated for the 3 mutant sample levels and WT, with at least 99% correct mutation calls for all mutation assays across multiple lots, platforms and operators for both within- and between-run experiments. Estimates of variance for each tested mutant and WT samples are listed in supplementary Additional file 1: Table S2.
IDH1/2 PCR assay technical success rate
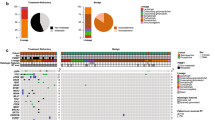
Performance of the assay was established on 171 retrospectively tested FFPE clinical glioma samples collected in 3 different sources: the Pitié-Salpêtrière Hospital, the Mayo Clinic and commercially available. Twenty-four samples did not meet the selection criteria (see Materials and Methods): for 2 cases, diagnosis of glioma was not confirmed; 17 samples were more than 10 years old and 5 samples contained less than 40% tumor cells. Histological distribution of the tumor samples reflected distribution observed in clinical routine with a predominance of glioblastomas (n = 61, 41%). The other samples were astro cytomas (n = 22, 15%), anaplastic astrocytomas (n = 25, 17%), oligodendrogliomas (n = 3, 2%), anaplastic oligodendrogliomas (n = 4, 3%), oligoastrocytomas (n = 12, 8%), and anaplastic oligoastrocytomas (n = 20, 14%) (Figure 3).
Out of the 147 FFPE samples which met the selection criteria, DNA extraction failed for one sample, while an IDH1/2 result was successfully obtained by the PCR test in 91% of cases (133/146). Different technical success rates were observed according to the origin of the samples with 100% technical success rate on samples from academic centers (103/103) and 70% on commercial samples (30/43) (Figure 4).
Distribution of the clinical glioma samples by tumor type (World Health Organization grade) (n = 147). The majority of the collected formalin-fixed paraffin-embedded clinical samples meeting inclusion criteria for the IDH1/2 PCR test originated from patients with diagnosed primary glioblastoma, the most frequently diagnosed glioma subtype in clinical routine. The remaining samples originated from patients diagnosed with other histological forms, mainly astrocytomas. Samples were available for each diffuse glioma subtype.
IDH1/2 PCR assay experimental flowchart: technical success rate. Out of the 147 formalin-fixed paraffin-embedded glioma clinical samples meeting the selection criteria, one DNA extraction failed. From the remaining samples, IDH1/2 PCR assay results were successfully obtained for most of the samples (91%). Successful tests were achieved on all samples (n = 103) originating from academic centers.
Clinical validation: comparison of IDH1/2 assay with IDH1 R132 immunochemistry and Sanger sequencing
To demonstrate the accuracy of the IDH1/2 PCR assay on clinical routine glioma samples, we examined the concordance between the IDH1/2 PCR results and results obtained with the current IDH1 R132H immunostaining and Sanger sequencing technologies. Out of the 133 samples successfully assessed by PCR, 61 (46%) were WT and 72 (54%) contained an IDH1/2 mutation. Out of the 72 mutated specimens, 60 (83%) carried the most common IDH1 R132H mutation, while the 12 remaining cases carried rare IDH mutations: IDH1 R132C in 3 cases, IDH1 R132-other in 7 cases, and IDH2 R172K in 1 case and IDH2 R172-other in 1 case. Using the IHC-based assay, 61 cases out of the 133 were scored as IDH1 R132H-positive. All but one IHC-positive cases were concordantly detected as IDH1 R132H by the PCR test and none of the remaining 72 IHC-negative cases were detected as IDH1 R132H-positive by PCR (Table 2), which translated into an OA of 99% [CI 95%, 95.9-99.9] between PCR and IHC (98.4% positive agreement [CI 95%, 91.3-99.7], 100% negative agreement [CI 95%, 94.9-100]).
When evaluating the 133 specimens by Sanger sequencing, the same mutations were detected by both Sanger sequencing and PCR in 67 cases (58 IDH1 R132H, 2 IDH1 R132C, 6 IDH1 R132-other and 1 IDH2 R172K), while the PCR assay detected 5 additional mutated cases (2 IDH1 R132H, 1 IDH1 R132C, 1 IDH1 R132-other and 1 IDH2 R172-other) (Tables 3 and 4), resulting in an OA of 96% [CI 95%, 91.5-98.4] between PCR and Sanger sequencing with a 100% positive agreement [CI 95%, 94.6-100] and 92% negative agreement [CI 95%, 83.5-96.7]. Predefined concordance targets for both PCR-IHC and PCR-Sanger comparisons were therefore met. Complete analysis of agreement between the IDH1/2 PCR assay and IHC or Sanger sequencing is shown in supplementary Additional file 1: Table S3.
Three IHC-positive cases were not reported positive by Sanger sequencing, including the PCR-negative case. Out of the 72 IHC-negative cases, Sanger sequencing identified 9 rare mutations (12%; 8 IDH1, 1 IDH2) while PCR identified 12 rare mutations (17%; 10 IDH1, 2 IDH2) (Table 4). The 6 cases discordant across the techniques for their identification of IDH mutation status were further investigated (Table 5). Case #1 (Figure 5), a sample of commercial origin, was IDH1 R132H IHC-positive but mutation negative by PCR and Sanger sequencing. We used 2 other techniques more sensitive than Sanger Sequencing: pyrosequencing followed by LNA-sequencing to further analyze this case. The IDH1 R132H mutation was not identified by any of these additional techniques. Consequently, based on the consistency of results obtained with PCR, Sanger sequencing, pyrosequencing and LNA-sequencing, it was likely that the mutation detected by IHC was a false-positive result.
Discordant case # 1. Case #1 stained IDH1 R132H positive by immunochemistry but was found WT for the IDH1 codon 132 (CGT) by Sanger sequencing, by pyrosequencing and with the IDH1/2 PCR assay a H&E slide. b IHC using the anti-human IDH1 R132H mouse monoclonal antibody DIA clone H09. c Sanger sequencing. d pyrogram indicating an allele frequency of 7%, thus below the cutoff for mutation ≥ 15%. e, f IDH1/2 PCR assay combining PCR-clamping (e) and ARMS (f): the red horizontal lines correspond to the threshold used to determine Ct. Total copies of IDH1 (WT ± mutated) are amplified with the total amplification reaction (red curves) but without further amplification by PCR-Clamping (blue curve) or by ARMS with specific R132H primers (green curve), indicating the absence of any mutation within IDH1 codon 132.
Cases #2 and #3 were identified as IDH1 R132H positive according to both IHC and PCR testing, and negative with Sanger sequencing. Review of the IHC R132H FFPE slide by a second pathologist confirmed the unambiguous IDH1 R132H positive IHC result. Quantitative PCR analysis revealed a low mutant allele percentage of 15% and 10% in cases #2 and #3, respectively. These percentages were below the Sanger sequencing sensitivity threshold (typically around 20% [27, 28]). Consequently this technical limit was likely to prevent mutation detection in these particular cases by Sanger sequencing.
Similarly, in case #4 identified as IDH1 R132C by PCR but WT by Sanger sequencing, a low mutant allele percentage (14%) was the probable source of conflicting results between these 2 tests as the mutation was also detected by pyrosequencing (Figure 6).
Discordant case #4. Case #4 was IDH1 R132H negative by IHC and was identified as wild-type by Sanger sequencing for IDH1 codon 132. The IDH1/2 PCR assay identified an IDH1 R132C mutation which was confirmed by pyrosequencing. a H&E slide. b IDH1 R132H IHC positive staining. c Sanger sequencing. d the pyrogram indicates the presence of the IDH1 R132C mutation (TGT) at a low allele frequency (around 15%) suggesting that the sample contained low tumor cell content. e PCR-clamping: the difference between the IDH1 PCR-clamping mutation assay Ct (blue curve) and total assay Ct (red curve) is inferior to the cutoff value (ΔCt = 31.87 - 27.49 = 4.38 < 5.34) indicating the presence of a mutation within IDH1 codon 132. f ARMS: the difference between the total assay Ct (red curve) and the IDH1 R132C ARMS assay Ct (green curve) is inferior to the cutoff value (ΔCt = 31.20 – 27.49 = 3.71 < 7.14) indicating presence of the IDH1 R132C mutation.
Cases #5 and #6 were found to be IDH1 R132 and IDH2 R172 PCR-positive respectively, but were not detected by IHC or Sanger sequencing. Pyrosequencing and LNA sequencing confirmed the absence of mutation in both cases, thereby indicating probable false PCR-positive results. The PCR Ct values of these 2 cases were close to the cut-off values of the respective mutations (data not shown). In order to eliminate a technical issue, PCR runs were repeated twice on cases #5 and #6 and the results indicated an IDH WT status. The first PCR results could therefore be considered as false-positive.
Validation of rare IDH1/2 mutations using synthetic samples
As the likelihood of having a significant representation of rare IDH1/2 mutations in the clinical cohort was low, synthetic samples representative of all 11 rare mutations were prepared. Each rare mutation was tested at 2 mutant allele percentages (30 and 40% of mutant DNA mixed with IDH WT genomic DNA). All mutations were correctly detected by the PCR assay in the 22 samples tested.
Discussion
We developed a novel PCR assay for the detection of 12 IDH1/2 mutations in one single step. A fast and reliable IDH mutation assay easy to implement in daily practice is highly desirable, given the diagnostic and prognostic significance of IDH mutations in diffuse glioma of low and intermediate grade (WHO grade II & III) as well as in secondary GBM (WHO grade IV). Testing for the presence of an IDH1/2 mutation is now considered by international guidelines for glioma management [29, 30]. Very recently, the predictive use of IDH mutations has been confirmed in grade III glioma [14]. There is also an increasing interest in the development of IDH-targeted therapies. Newly developed mutated-IDH selective inhibitors have already demonstrated therapeutic effect in preclinical models [17] and an alternative approach whereby pathologic DNA-methylation is targeted, has led to tumor control in IDH mutant cells [18, 19]. Consolidation of these promising results in future clinical studies will imply identification of patients carrying specific IDH mutations with a reliable companion diagnostics test.
Currently, IHC covers the most prevalent IDH1 mutation, and various molecular techniques are used to assess the IHC-negative cases, leading to a two-step diagnostic algorithm with possibly long timelines to complete a full IDH profiling. With the Sanger sequencing, multiple DNA-based assays have been adapted for the detection of IDH mutations, including restriction length fragment polymorphism gel electrophoresis, PCR and endonuclease restriction, allele-specific polymerase chain reaction, pyrosequencing, high resolution melting (HRM) or cold-PCR HRM [31–36].
These methods present pros and cons in terms of ease of use, rapidity, and sensitivity performance. The majority of published assays targets the most frequent IDH1 R132 mutations but they are not designed to detect other rare ones including those within that same codon 132, the IDH1 R100 mutations or the IDH2 mutations. Therefore we developed an alternative assay for rapid (only 5 hours from DNA extraction to data acquisition) and comprehensive analysis of the 12 clinically IDH1/2 mutations reported to date, with a single-step design compatible with easy implementation in routine clinical practice. Demonstration of high analytical and clinical performance of a new test is critical before implementation in a pathology laboratory. In this study, we validated the performance of this new IDH1/2 PCR assay on a large cohort of FFPE glioma samples collected less than 10 years ago and on synthetic samples mimicking all 11 rare IDH1/2 mutations. Out of the 147 FFPE tested samples, the overall technical success rate of the PCR assay was 91%, reaching 100% on the 103 samples collected from academic centers. The technical success rate obtained on the remaining 43 commercial samples (DNA extraction failed from one sample) was lower (70%); this was probably due to a poor formalin fixation of this specific FFPE sample series, therefore impacting on the sample quality.
The assay showed a higher sensitivity than Sanger sequencing which typically detects levels as low as around 20% of mutant allele load. Without any mutant DNA enrichment before the IDH1/2-specific PCR, the test showed high analytical sensitivity with detection of mutant allele frequency, ranging from 0.6% for IDH2 R172K to below 5% for all mutations except for the rare IDH2 R172S one. Moreover, the precision study demonstrated that results for the mutation detection were highly reproducible and reliable including for mutant allele frequencies of 5%.
Out of the 133 clinical samples with a successful PCR IDH determination, IDH1/2 mutations were detected in 54% of cases. The frequency of mutations by histological subtype was similar to previous reports from large series [5] with 13% of mutations identified in primary GBMs as opposed to 83% in the other subtypes. We further examined the PCR test accuracy by comparing, in a blind manner, the results obtained from the 133 clinical FFPE samples to the ones from IDH1 R132H-IHC and Sanger sequencing, which are the 2 main clinical diagnostic technologies recommended in the current algorithms for IDH testing. Overall concordance for IDH1 R132H detection was 99% between PCR and IHC and 96% between PCR and Sanger sequencing. Positive concordances were high, with 98% between PCR and IHC and 100% between PCR and Sanger sequencing. The high concordance of the new PCR assay with the standard technologies demonstrated that the test could be used reliably for clinical diagnostics.
Regarding the agreement with IDH1 R132H-IHC, only one case was detected as negative discordant and this case was likely to be a false-positive IHC case as its analysis with 2 additional sensitive techniques confirmed its PCR and Sanger sequencing-identified IDH WT status. This highlights the need to ensure high quality in IHC testing when used for routine clinical diagnostic [37]. The number of cases (5 identified in total) with conflicting results from the IDH1/2 PCR assay and Sanger sequencing was less than 4%. Three of them could be explained by a low mutant allele content (<20%) which is below the Sanger sequencing sensitivity and therefore the mutation could not be detected using this technique. This further illustrates that if sensitivity of sequencing is generally not an issue when analyzing tumor samples with high content of neoplastic cells, it can become a limiting factor in the absence of macro-dissection for samples with a low tumor cellularity, leading to false negative results.
Overall, only 2 false-positive PCR results out of the 133 samples tested here were identified by comparison of IHC, Sanger sequencing, pyrosequencing and LNA-sequencing, which consistently established a WT IDH status for these 2 samples. Repeated PCR tests on these samples indicated a WT IDH status, supporting the hypothesis that the false-positive result from the first run might have come from an experimental error.
Additional synthetic samples were further analyzed in order to confirm the correct detection of all 11 rare mutations from the PCR assay and this analysis indicated 100% correct calls, further validating the performance of the assay.
Interestingly, a new dinucleotide deletion/insertion mutation has been reported since the design of this assay [38]. Since this newly identified mutation is localized within the codon 132 of the IDH1 gene, the assay design and more specifically the clamping reaction, may allow its detection. It will be of interest to confirm this on synthetic samples reproducing this mutation and then on clinical FFPE samples if available.
Conclusions
In summary, we have developed a new PCR-based assay which enables rapid and simple detection of the major IDH1 R132H mutation and of 11 rarer IDH1/2 ones in FFPE glioma samples. The test is designed as a single-step PCR procedure combining clamping and ARMS. We have established here the high sensitivity and reliability of this new assay and validated it on 171 FFPE clinical samples, indicating that the test fulfilled both analytical and clinical performance required for implementation in clinical practice. The PCR test could be used as a rapid and robust novel tool in the clinical assessment of diffuse gliomas as well as in selecting patients suitable for clinical trials.
References
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P: The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 2007, 114(2):97–109. doi:10.1007/s00401–007–0243–4 10.1007/s00401-007-0243-4
Weller M, Pfister SM, Wick W, Hegi ME, Reifenberger G, Stupp R: Molecular neuro-oncology in clinical practice: a new horizon. Lancet Oncol 2013, 14(9):e370-e379. doi:10.1016/S1470–2045(13)70168–2 10.1016/S1470-2045(13)70168-2
Thomas L, Di Stefano AL, Ducray F: Predictive biomarkers in adult gliomas: the present and the future. Curr Opin Oncol 2013, 25(6):689–694. doi:10.1097/CCO.0000000000000002 10.1097/CCO.0000000000000002
Hartmann C, Meyer J, Balss J, Capper D, Mueller W, Christians A, Felsberg J, Wolter M, Mawrin C, Wick W, Weller M, Herold-Mende C, Unterberg A, Jeuken JW, Wesseling P, Reifenberger G, von Deimling A: Type and frequency of IDH1 and IDH2 mutations are related to astrocytic and oligodendroglial differentiation and age: a study of 1,010 diffuse gliomas. Acta Neuropathol 2009, 118(4):469–474. doi:10.1007/s00401–009–0561–9 10.1007/s00401-009-0561-9
von Deimling A, Korshunov A, Hartmann C: The next generation of glioma biomarkers: MGMT methylation, BRAF fusions and IDH1 mutations. Brain Pathol 2011, 21(1):74–87. doi:10.1111/j.1750–3639.2010.00454.x 10.1111/j.1750-3639.2010.00454.x
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, Friedman H, Friedman A, Reardon D, Herndon J, Kinzler KW, Velculescu VE, Vogelstein B, Bigner DD: IDH1 and IDH2 mutations in gliomas. N Engl J Med 2009, 360(8):765–773. doi:10.1056/NEJMoa0808710 10.1056/NEJMoa0808710
Capper D, Reuss D, Schittenhelm J, Hartmann C, Bremer J, Sahm F, Harter PN, Jeibmann A, von Deimling A: Mutation-specific IDH1 antibody differentiates oligodendrogliomas and oligoastrocytomas from other brain tumors with oligodendroglioma-like morphology. Acta Neuropathol 2011, 121(2):241–252. doi:10.1007/s00401–010–0770–2 10.1007/s00401-010-0770-2
van den Bent MJ, Dubbink HJ, Marie Y, Brandes AA, Taphoorn MJ, Wesseling P, Frenay M, Tijssen CC, Lacombe D, Idbaih A, van Marion R, Kros JM, Dinjens WN, Gorlia T, Sanson M: IDH1 and IDH2 mutations are prognostic but not predictive for outcome in anaplastic oligodendroglial tumors: a report of the European Organization for Research and Treatment of Cancer Brain Tumor Group. Clin Cancer Res 2010, 16(5):1597–1604. doi:10.1158/1078–0432.CCR-09–2902 10.1158/1078-0432.CCR-09-2902
Dubbink HJ, Taal W, van Marion R, Kros JM, van Heuvel I, Bromberg JE, Zonnenberg BA, Zonnenberg CB, Postma TJ, Gijtenbeek JM, Boogerd W, Groenendijk FH, Smitt PA, Dinjens WN, van den Bent MJ: IDH1 mutations in low-grade astrocytomas predict survival but not response to temozolomide. Neurology 2009, 73(21):1792–1795. doi:10.1212/WNL.0b013e3181c34ace 10.1212/WNL.0b013e3181c34ace
Houillier C, Wang X, Kaloshi G, Mokhtari K, Guillevin R, Laffaire J, Paris S, Boisselier B, Idbaih A, Laigle-Donadey F, Hoang-Xuan K, Sanson M, Delattre JY: IDH1 or IDH2 mutations predict longer survival and response to temozolomide in low-grade gliomas. Neurology 2010, 75(17):1560–1566. doi:10.1212/WNL.0b013e3181f96282 10.1212/WNL.0b013e3181f96282
Weller M, Felsberg J, Hartmann C, Berger H, Steinbach JP, Schramm J, Westphal M, Schackert G, Simon M, Tonn JC, Heese O, Krex D, Nikkhah G, Pietsch T, Wiestler O, Reifenberger G, von Deimling A, Loeffler M: Molecular predictors of progression-free and overall survival in patients with newly diagnosed glioblastoma: a prospective translational study of the German Glioma Network. J Clin Oncol 2009, 27(34):5743–5750. doi:10.1200/JCO.2009.23.0805 10.1200/JCO.2009.23.0805
Wick W, Hartmann C, Engel C, Stoffels M, Felsberg J, Stockhammer F, Sabel MC, Koeppen S, Ketter R, Meyermann R, Rapp M, Meisner C, Kortmann RD, Pietsch T, Wiestler OD, Ernemann U, Bamberg M, Reifenberger G, von Deimling A, Weller M: NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. J Clin Oncol 2009, 27(35):5874–5880. doi:10.1200/JCO.2009.23.6497 10.1200/JCO.2009.23.6497
Wick W, Meisner C, Hentschel B, Platten M, Schilling A, Wiestler B, Sabel MC, Koeppen S, Ketter R, Weiler M, Tabatabai G, von Deimling A, Gramatzki D, Westphal M, Schackert G, Loeffler M, Simon M, Reifenberger G, Weller M: Prognostic or predictive value of MGMT promoter methylation in gliomas depends on IDH1 mutation. Neurology 2013, 81(17):1515–1522. doi:10.1212/WNL.0b013e3182a95680 10.1212/WNL.0b013e3182a95680
Cairncross JG, Wang M, Jenkins RB, Shaw EG, Giannini C, Brachman DG, Buckner JC, Fink KL, Souhami L, Laperriere NJ, Huse JT, Mehta MP, Curran WJ Jr: Benefit From Procarbazine, Lomustine, and Vincristine in Oligodendroglial Tumors Is Associated With Mutation of IDH. J Clin Oncol 2014, 32(8):783–790. doi:10.1200/JCO.2013.49.3726 10.1200/JCO.2013.49.3726
Beiko J, Suki D, Hess KR, Fox BD, Cheung V, Cabral M, Shonka N, Gilbert MR, Sawaya R, Prabhu SS, Weinberg J, Lang FF, Aldape KD, Sulman EP, Rao G, McCutcheon IE, Cahill DP: IDH1 mutant malignant astrocytomas are more amenable to surgical resection and have a survival benefit associated with maximal surgical resection. Neuro Oncol 2014, 16(1):81–91. doi:10.1093/neuonc/not159 10.1093/neuonc/not159
Taylor JW, Chi AS, Cahill DP: Tailored therapy in diffuse gliomas: using molecular classifiers to optimize clinical management. Oncology (Williston Park) 2013, 27(6):504–514.
Rohle D, Popovici-Muller J, Palaskas N, Turcan S, Grommes C, Campos C, Tsoi J, Clark O, Oldrini B, Komisopoulou E, Kunii K, Pedraza A, Schalm S, Silverman L, Miller A, Wang F, Yang H, Chen Y, Kernytsky A, Rosenblum MK, Liu W, Biller SA, Su SM, Brennan CW, Chan TA, Graeber TG, Yen KE, Mellinghoff IK: An inhibitor of mutant IDH1 delays growth and promotes differentiation of glioma cells. Science 2013, 340(6132):626–630. doi:10.1126/science.1236062 10.1126/science.1236062
Borodovsky A, Salmasi V, Turcan S, Fabius AW, Baia GS, Eberhart CG, Weingart JD, Gallia GL, Baylin SB, Chan TA, Riggins GJ: 5-azacytidine reduces methylation, promotes differentiation and induces tumor regression in a patient-derived IDH1 mutant glioma xenograft. Oncotarget 2013, 4(10):1737–1747.
Turcan S, Fabius AW, Borodovsky A, Pedraza A, Brennan C, Huse J, Viale A, Riggins GJ, Chan TA: Efficient induction of differentiation and growth inhibition in IDH1 mutant glioma cells by the DNMT Inhibitor Decitabine. Oncotarget 2013, 4(10):1729–1736.
The Catalogue of Somatic Mutations in Cancer (COSMIC). [http://cancer.sanger.ac.uk/cancergenome/projects/cosmic]
Preusser M, Capper D, Hartmann C: IDH testing in diagnostic neuropathology: review and practical guideline article invited by the Euro-CNS research committee. Clin Neuropathol 2011, 30(5):217–230.
Capper D, Weissert S, Balss J, Habel A, Meyer J, Jager D, Ackermann U, Tessmer C, Korshunov A, Zentgraf H, Hartmann C, von Deimling A: Characterization of R132H mutation-specific IDH1 antibody binding in brain tumors. Brain Pathol 2010, 20(1):245–254. doi:10.1111/j.1750–3639.2009.00352.x 10.1111/j.1750-3639.2009.00352.x
Preusser M, Wohrer A, Stary S, Hoftberger R, Streubel B, Hainfellner JA: Value and limitations of immunohistochemistry and gene sequencing for detection of the IDH1-R132H mutation in diffuse glioma biopsy specimens. J Neuropathol Exp Neurol 2011, 70(8):715–723. doi:10.1097/NEN.0b013e31822713f0 10.1097/NEN.0b013e31822713f0
Wayne PA: Evaluation of detection capability for clinical laboratory measurement procedures; approved guideline. CLSI document EP17-A2 2012.
Wayne PA: Evaluation of precision performance of quantitative measurement methods; approved guidelines. CLSI document EP05-A2 2004.
Ida CM, Lambert SR, Rodriguez FJ, Voss JS, Mc Cann BE, Seys AR, Halling KC, Collins VP, Giannini C: BRAF alterations are frequent in cerebellar low-grade astrocytomas with diffuse growth pattern. J Neuropathol Exp Neurol 2012, 71(7):631–639. doi:10.1097/NEN.0b013e31825c448a 10.1097/NEN.0b013e31825c448a
Tsiatis AC, Norris Kirby A, Rich RG, Hafez MJ, Gocke CD, Eshleman JR, Murphy KM: Comparison of Sanger sequencing, pyrosequencing, and melting curve analysis for the detection of KRAS mutations: diagnostic and clinical implications. J Mol Diagn 2010, 12(4):425–432. doi:10.2353/jmoldx.2010.090188S1525–1578(10)60082–7 10.2353/jmoldx.2010.090188
Angulo B, Garcia Garcia E, Martinez R, Suarez Gauthier A, Conde E, Hidalgo M, Lopez Rios F: Commercial real-time PCR kit provides greater sensitivity than direct sequencing to detect KRAS mutations: a morphology-based approach in colorectal carcinoma. J Mol Diagn 2010, 12(3):292–299. doi:10.2353/jmoldx.2010.090139S1525–1578(10)60063–3 10.2353/jmoldx.2010.090139
Soffietti R, Baumert BG, Bello L, von Deimling A, Duffau H, Frenay M, Grisold W, Grant R, Graus F, Hoang-Xuan K, Klein M, Melin B, Rees J, Siegal T, Smits A, Stupp R, Wick W: Guidelines on management of low-grade gliomas: report of an EFNS-EANO Task Force. Eur J Neurol 2010, 17(9):1124–1133. doi:10.1111/j.1468–1331.2010.03151.x 10.1111/j.1468-1331.2010.03151.x
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines): Central Nervous System Cancers. 2014., 1: Available via . Accessed 14 Mar 2014 http://www.nccn.org
Bujko M, Kober P, Matyja E, Nauman P, Dyttus-Cebulok K, Czeremszynska B, Bonicki W, Siedlecki JA: Prognostic value of IDH1 mutations identified with PCR-RFLP assay in glioblastoma patients. Mol Diagn Ther 2010, 14(3):163–169. doi:10.2165/11537170–000000000–00000 10.1007/BF03256369
Boisselier B, Marie Y, Labussiere M, Ciccarino P, Desestret V, Wang X, Capelle L, Delattre JY, Sanson M: COLD PCR HRM: a highly sensitive detection method for IDH1 mutations. Hum Mutat 2010, 31(12):1360–1365. doi:10.1002/humu.21365 10.1002/humu.21365
Horbinski C, Kelly L, Nikiforov YE, Durso MB, Nikiforova MN: Detection of IDH1 and IDH2 mutations by fluorescence melting curve analysis as a diagnostic tool for brain biopsies. J Mol Diagn 2010, 12(4):487–492. 10.2353/jmoldx.2010.090228 10.2353/jmoldx.2010.090228
Loussouarn D, Le Loupp AG, Frenel JS, Leclair F, Von Deimling A, Aumont M, Martin S, Campone M, Denis MG: Comparison of immunohistochemistry, DNA sequencing and allele-specific PCR for the detection of IDH1 mutations in gliomas. Int J Oncol 2012, 40(6):2058–2062. doi:10.3892/ijo.2012.1404
Setty P, Hammes J, Rothamel T, Vladimirova V, Kramm CM, Pietsch T, Waha A: A pyrosequencing-based assay for the rapid detection of IDH1 mutations in clinical samples. J Mol Diagn 2010, 12(6):750–756. doi:10.2353/jmoldx.2010.090237 10.2353/jmoldx.2010.090237
Meyer J, Pusch S, Balss J, Capper D, Mueller W, Christians A, Hartmann C, Von Deimling A: PCR- and restriction endonuclease-based detection of IDH1 mutations. Brain Pathol 2010, 20(2):298–300. doi:10.1111/j.1750–3639.2009.00327.xBPA327 10.1111/j.1750-3639.2009.00327.x
van den Bent MJ, Hartmann C, Preusser M, Strobel T, Dubbink HJ, Kros JM, von Deimling A, Boisselier B, Sanson M, Halling KC, Diefes KL, Aldape K, Giannini C: Interlaboratory comparison of IDH mutation detection. J Neurooncol 2013, 112(2):173–178. doi:10.1007/s11060–013–1056-z 10.1007/s11060-013-1056-z
Gupta R, Flanagan S, Li CC, Lee M, Shivalingham B, Maleki S, Wheeler HR, Buckland ME: Expanding the spectrum of IDH1 mutations in gliomas. Mod Pathol 2013, 26(5):619–625. doi:10.1038/modpathol.2012.210 10.1038/modpathol.2012.210
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
AC, HG, FM, CP, SC, VF and HPSP are Qiagen employees. Qiagen financed the project and article-processing charge. JV, RF, BB, KM, MS and CG declare they have no competing interests.
Authors’ contributions
AC and HPSP participated in the conception of the study, in the interpretation of data, and wrote the manuscript. HG coordinated the study, participated in its design, and participated in the analysis and interpretation of the data. FM, CP and VF participated in the design of the study, carried out the molecular tests and participated in the analysis and interpretation of the data. SC performed the statistical analysis and participated in the analysis and interpretation of the data. KM, MS and BB selected the clinical samples from La Pitié-Salpétrière Hospital. KM performed the IDH1R132H immunohistochemistry tests on the clinical samples from La Pitié-Salpêtrière Hospital. BB performed IDH1 Sanger sequencing on the clinical samples from La Pitié-Salpêtrière Hospital. MS and KM revised the paper critically. JV, RBJ and CG selected the clinical samples from Mayo Clinic and participated in the analysis and interpretation of the Mayo data. JV and CG revised the paper critically. JV carried out pyrosequencing and LNA tests. CG performed the IDH1R132H immunohistochemistry tests on the clinical samples from Mayo Clinic. All authors read and approved the final manuscript.
Electronic supplementary material
40478_2014_132_MOESM1_ESM.pdf
Additional file 1: Table S1: Sensitivity of the IDH1/2 PCR assay for the 12 detected and 3 identified IDH1/2 mutations. Table S2. Precision results. Table S3. Analysis of Agreement between the IDH1/2 PCR assay and IDH1 R132H-IHC and Sanger sequencing. (PDF 350 KB)
40478_2014_132_MOESM2_ESM.pdf
Additional file 2: Figure S1: Sensitivity of the PCR 1DH1/2 assay for each mutation. Box plots depict the ΔCt values obtained at five mutant allele percentages (2, 5, 10, 15 and 20%) in a WT DNA background for the 12 mutations detected by PCR-clamping (A, C, E) and the 3 mutations identified by ARMS (B, D). Data were obtained from repeated and independent measurements as described in materials and methods. The red lines denote the determined LOD. (PDF 17 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Catteau, A., Girardi, H., Monville, F. et al. A new sensitive PCR assay for one-step detection of 12 IDH1/2 mutations in glioma. acta neuropathol commun 2, 58 (2014). https://doi.org/10.1186/2051-5960-2-58
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2051-5960-2-58